Efficacy of Mouth Rinses and Nasal Spray in the Inactivation of SARS-CoV-2: A Systematic Review and Meta-Analysis of In Vitro and In Vivo Studies
et al., International Journal of Environmental Research and Public Health, doi:10.3390/ijerph191912148, Sep 2022
PVP-I for COVID-19
15th treatment shown to reduce risk in
February 2021, now with p = 0.000000000016 from 22 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
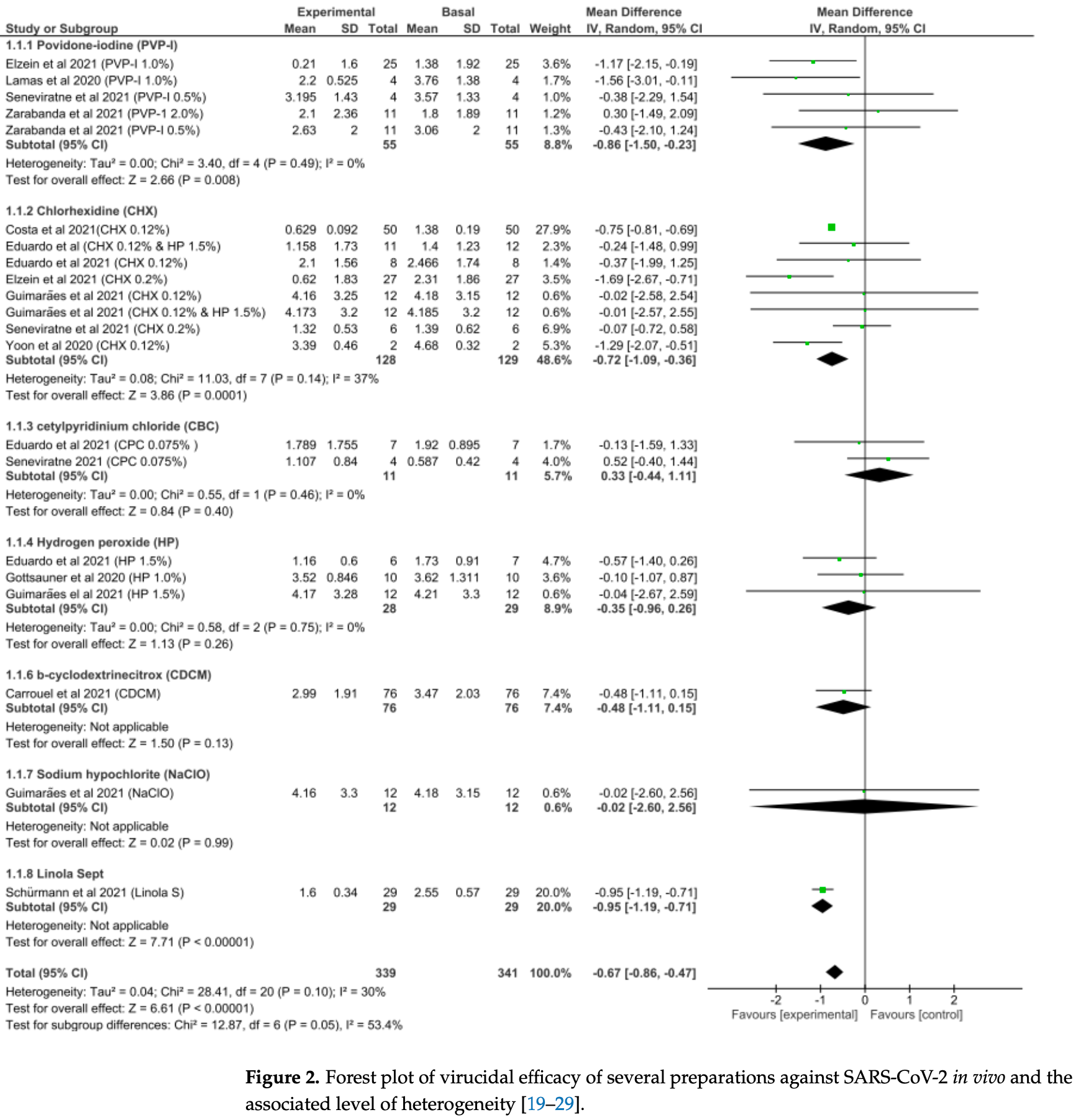
Systematic review and meta analysis showing significant reduction in SARS-CoV-2 salivary viral load with povidone-iodine and chlorhexidine.
3 meta-analyses show significant improvements with povidone-iodine for viral load1-3 and
viral clearance1.
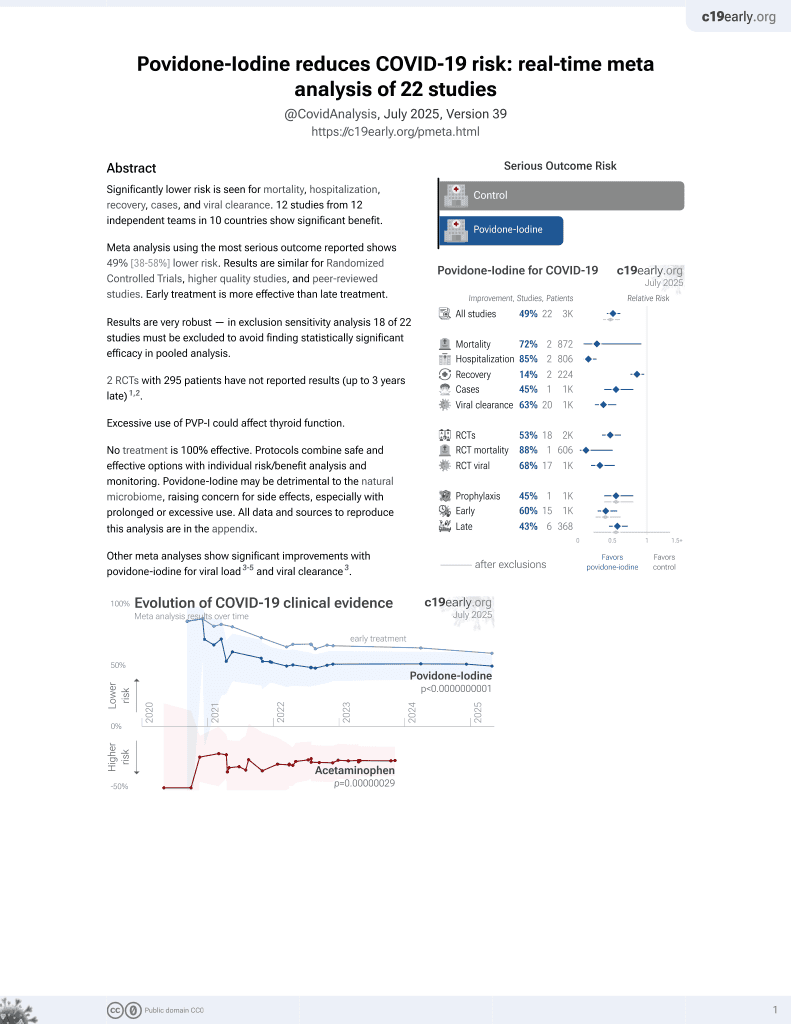
Currently there are 22 povidone-iodine for COVID-19 studies, showing 72% lower mortality [8‑92%], 85% lower hospitalization [73‑91%], and 45% fewer cases [20‑62%].
1.
Hasan et al., Effects of Chlorhexidine and Povidone-Iodine on the SARS-CoV-2 Load: A Systematic Review and Meta-analysis, European Journal of Dentistry, doi:10.1055/s-0042-1753470.
Idrees et al., 25 Sep 2022, peer-reviewed, 6 authors.
Contact: omar.kujan@uwa.edu.au (corresponding author).
Efficacy of Mouth Rinses and Nasal Spray in the Inactivation of SARS-CoV-2: A Systematic Review and Meta-Analysis of In Vitro and In Vivo Studies
International Journal of Environmental Research and Public Health, doi:10.3390/ijerph191912148
Severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) is a global and evolving pandemic associated with heavy health and financial burdens. Considering the oral cavity as the major reservoir for SARS-CoV-2, a systematic review and meta-analysis were conducted to assess the efficacy of mouth rinses and nasal sprays in reducing the salivary viral load of SARS-CoV-2. All in vivo and in vitro studies that assessed the virucidal efficacy of mouth rinses and nasal sprays against SARS-CoV-2 and were published in the English language from December 2019 to April 2022 were considered for analyses. Special Medical Subject Headings terms were used to search Pubmed, Scopus, Embase Ovid, and Web of Science databases. The toxicological data reliability assessment tool (ToxRToool) was used to assess the quality of the included studies. Thirty-three studies (11 in vivo and 22 in vitro) were deemed eligible for inclusion in this analysis. Results of the pooled data showed that povidone-iodine is the most efficacious intervention in vivo in terms of reducing the SARS-CoV-2 salivary viral load, followed by chlorhexidine. The mean difference in the viral load was 86% and 72%, respectively. Similarly, povidone-iodine was associated with the highest log 10 reduction value (LRV) in vitro, followed by cetylpyridinium chloride, (LRV = 2.938 (p < 0.0005) and LRV = 2.907 (p = 0.009), respectively). Povidone-iodine-based oral and nasal preparations showed favourable results in terms of reducing SARS-CoV-2 viral loads both in vivo and in vitro. Considering the limited number of patients in vivo, further studies among larger cohorts are recommended.
References
Abdelalim, Mohamady, Elsayed, Elawady, Ghallab, Corticosteroid nasal spray for recovery of smell sensation in COVID-19 patients: A randomized controlled trial, Am. J. Otolaryngol, doi:10.1016/j.amjoto.2020.102884
Almanza-Reyes, Moreno, Plascencia-Lopez, Alvarado-Vera, Patron-Romero et al., Evaluation of silver nanoparticles for the prevention of SARS-CoV-2 infection in health workers: In vitro and in vivo, PLoS ONE, doi:10.1371/journal.pone.0256401
Amber, Abhishek, Nikita, Efficacy of Mouth Rinses against SARS-CoV-2: A Scoping Review, Front. Dent. Med
Anderson, Patterson, Richards, Pitol, Edwards et al., CPC-containing oral rinses inactivate SARS-CoV-2 variants and are active in the presence of human saliva, J. Med. Microbiol, doi:10.1099/jmm.0.001508
Anderson, Sivalingam, Kang, Ananthanarayanan, Arumugam et al., Povidone-Iodine Demonstrates Rapid In Vitro Virucidal Activity against SARS-CoV-2, the Virus Causing COVID-19 Disease, Infect. Dis. Ther, doi:10.1007/s40121-020-00316-3
Aref, Bazeed, Hassan, Hassan, Rashad et al., Biochemical and Molecular Evaluations of Ivermectin Mucoadhesive Nanosuspension Nasal Spray in Reducing Upper Respiratory Symptoms of Mild COVID-19, Int. J. Nanomed, doi:10.2147/IJN.S313093
Arefin, Rumi, Uddin, Banu, Khan et al., Virucidal effect of povidone iodine on COVID-19 in the nasopharynx: An open-label randomized clinical trial, Indian J. Otolaryngol. Head Neck Surg, doi:10.1007/s12070-021-02616-7
Avhad, Bhanushali, Sachdev, Save, Kalra et al., Comparison of effectiveness of chlorine dioxide mouthwash and chlorhexidine gluconate mouthwash in reduction of oral viral load in patients with COVID-19, Indian J. Public Health Res. Dev
Balouch, Vontela, Yeakel, Alnouri, Sataloff, Role of Famotidine and Other Acid Reflux Medications for SARS-CoV-2: A Pilot Study, J. Voice, doi:10.1016/j.jvoice.2021.01.007
Bano-Polo, Martinez-Gil, Sanchez Del Pino, Massoli, Mingarro et al., Cetylpyridinium chloride promotes disaggregation of SARS-CoV-2 virus-like particles, J. Oral Microbiol, doi:10.1080/20002297.2022.2030094
Bansal, Jonsson, Taylor, Figueroa, Dugour et al., Iota-carrageenan and xylitol inhibit SARS-CoV-2 in Vero cell culture, PLoS ONE, doi:10.1371/journal.pone.0259943
Bentley, Stanton, Hydroxypropyl Methylcellulose-Based Nasal Sprays Effectively Inhibit In Vitro SARS-CoV-2 Infection and Spread, Viruses, doi:10.3390/v13122345
Bidra, Pelletier, Westover, Frank, Brown et al., Comparison of In Vitro Inactivation of SARS CoV-2 with Hydrogen Peroxide and Povidone-Iodine Oral Antiseptic Rinses, J. Prosthodont, doi:10.1111/jopr.13220
Bidra, Pelletier, Westover, Frank, Brown et al., Rapid In-Vitro Inactivation of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Using Povidone-Iodine Oral Antiseptic Rinse, J. Prosthodont, doi:10.1111/jopr.13209
Bovard, Van Der Toorn, Schlage, Constant, Renggli et al., Iota-carrageenan extracted from red algae is a potent inhibitor of SARS-CoV-2 infection in reconstituted human airway epithelia, Biochem. Biophys. Rep, doi:10.1016/j.bbrep.2021.101187
Buonavoglia, Camero, Lanave, Catella, Trombetta et al., Virucidal activity in vitro of mouthwashes against a feline coronavirus type II, Oral Dis, doi:10.1111/odi.14067
Burgos-Ramos, Urbieta, Rodriguez, Is hydrogen peroxide an effective mouthwash for reducing the viral load of SARS-CoV-2 in dental clinics? Saudi, Dent. J, doi:10.1016/j.sdentj.2022.01.005
Burton, Clarkson, Goulao, Glenny, Mcbain et al., Antimicrobial mouthwashes (gargling) and nasal sprays to protect healthcare workers when undertaking aerosol-generating procedures (AGPs) on patients without suspected or confirmed COVID-19 infection, Cochrane Database Syst. Rev
Cannon, Westover, Bleher, Sanchez-Gonzalez, Ferrer, In Vitro Analysis of the Anti-viral Potential of nasal spray constituents against SARS-CoV-2, bioRxiv, doi:10.1101/2020.12.02.408575
Carrouel, Conte, Fisher, Goncalves, Dussart et al., COVID-19: A Recommendation to Examine the Effect of Mouthrinses with beta-Cyclodextrin Combined with Citrox in Preventing Infection and Progression, J. Clin. Med, doi:10.3390/jcm9041126
Carrouel, Valette, Gadea, Esparcieux, Illes et al., Use of an antiviral mouthwash as a barrier measure in the SARS-CoV-2 transmission in adults with asymptomatic to mild COVID-19: A multicentre, randomized, double-blind controlled trial, Clin. Microbiol. Infect, doi:10.1016/j.cmi.2021.05.028
Cavalcante-Leao, De Araujo, Basso, Schroder, Guariza-Filho et al., Is there scientific evidence of the mouthwashes effectiveness in reducing viral load in COVID-19? A systematic review, J. Clin. Exp. Dent, doi:10.4317/jced.57406
Chaudhary, Melkonyan, Meethil, Saraswat, Hall et al., Estimating salivary carriage of severe acute respiratory syndrome coronavirus 2 in nonsymptomatic people and efficacy of mouthrinse in reducing viral load: A randomized controlled trial, J. Am. Dent. Assoc, doi:10.1016/j.adaj.2021.05.021
Costa, Brites, Vaz, De Santana, Dos Santos et al., Chlorhexidine mouthwash reduces the salivary viral load of SARS-CoV-2: A randomized clinical trial, Oral Dis, doi:10.1111/odi.14086
Da Fonseca Orcina, Vilhena, Cardoso De Oliveira, Marques Da Costa Alves, Araki et al., A Phthalocyanine Derivate Mouthwash to Gargling/Rinsing as an Option to Reduce Clinical Symptoms of COVID-19: Case Series, Clin. Cosmet. Investig. Dent, doi:10.2147/CCIDE.S295423
Davies, Buczkowski, Welch, Green, Mawer et al., Effective in vitro inactivation of SARS-CoV-2 by commercially available mouthwashes, J. Gen. Virol
De Toledo Telles-Araujo, Caminha, Kallas, Sipahi, Da Silva Santos, Potential mouth rinses and nasal sprays that reduce SARS-CoV-2 viral load: What we know so far?, Clinics, doi:10.6061/clinics/2020/e2328
Domenico, Collares, Santos, Lenz, Antunes et al., Hydrogen peroxide as an auxiliary treatment for COVID-19 in Brazil: A randomized double-blind clinical trial, Epidemiol. Health, doi:10.4178/epih.e2021051
Eduardo, Correa, Heller, Daep, Benitez et al., Salivary SARS-CoV-2 load reduction with mouthwash use: A randomized pilot clinical trial, Heliyon, doi:10.1016/j.heliyon.2021.e07346
Elzein, Abdel-Sater, Fakhreddine, Hanna, Feghali et al., In vivo evaluation of the virucidal efficacy of chlorhexidine and povidone-iodine mouthwashes against salivary SARS-CoV-2. A randomized-controlled clinical trial, J. Evid. Based Dent. Pract, doi:10.1016/j.jebdp.2021.101584
Errecalde, Lifschitz, Vecchioli, Ceballos, Errecalde et al., Safety and Pharmacokinetic Assessments of a Novel Ivermectin Nasal Spray Formulation in a Pig Model, J. Pharm. Sci, doi:10.1016/j.xphs.2021.01.017
Fallahi, Keyhan, Zandian, Kim, Cheshmi, Being a front-line dentist during the COVID-19 pandemic: A literature review, Maxillofac. Plast. Reconstr. Surg, doi:10.1186/s40902-020-00256-5
Fears, Klimstra, Duprex, Hartman, Weaver et al., Persistence of Severe Acute Respiratory Syndrome Coronavirus 2 in Aerosol Suspensions, Emerg. Infect. Dis, doi:10.3201/eid2609.201806
Figueroa, Lombardo, Dogliotti, Flynn, Giugliano et al., Efficacy of a Nasal Spray Containing Iota-Carrageenan in the Postexposure Prophylaxis of COVID-19 in Hospital Personnel Dedicated to Patients Care with COVID-19 Disease, Int. J. Gen. Med, doi:10.2147/IJGM.S328486
Frank, Brown, Capriotti, Westover, Pelletier et al., In Vitro Efficacy of a Povidone-Iodine Nasal Antiseptic for Rapid Inactivation of SARS-CoV-2, JAMA Otolaryngol. Head Neck Surg, doi:10.1001/jamaoto.2020.3053
Frank, Capriotti, Brown, Tessema, Povidone-Iodine Use in Sinonasal and Oral Cavities: A Review of Safety in the COVID-19 Era, Ear Nose Throat J, doi:10.1177/0145561320932318
Funnell, Afrough, Baczenas, Berry, Bewley et al., A cautionary perspective regarding the isolation and serial propagation of SARS-CoV-2 in Vero cells, NPJ Vaccines
Garcia-Sanchez, Pena-Cardelles, Ruiz, Robles, Ordonez-Fernandez et al., Efficacy of Pre-Procedural Mouthwashes against SARS-CoV-2: A Systematic Review of Randomized Controlled Trials, J. Clin. Med, doi:10.3390/jcm11061692
Gentilini, Turba, Taddei, Gritti, Fantini et al., Modelling RT-qPCR cycle-threshold using digital PCR data for implementing SARS-CoV-2 viral load studies, PLoS ONE, doi:10.1371/journal.pone.0260884
Gerlach, Wolff, Ludwig, Schafer, Keiner et al., Rapid SARS-CoV-2 inactivation by commonly available chemicals on inanimate surfaces, J. Hosp. Infect, doi:10.1016/j.jhin.2020.09.001
Gottsauner, Michaelides, Schmidt, Scholz, Buchalla et al., A prospective clinical pilot study on the effects of a hydrogen peroxide mouthrinse on the intraoral viral load of SARS-CoV-2, Clin. Oral Investig, doi:10.1007/s00784-020-03549-1
Green, Roberts, Tobery, Vincent, Barili et al., In vitro assessment of the virucidal activity of four mouthwashes containing Cetylpyridinium Chloride, ethanol, zinc and a mix of enzyme and proteins against a human coronavirus, bioRxiv
Gudmundsdottir, Scheving, Lindberg, Stefansson, Inactivation of SARS-CoV-2 and HCoV-229E in vitro by ColdZyme(R) a medical device mouth spray against the common cold, J. Med. Virol, doi:10.1002/jmv.26554
Guenezan, Garcia, Strasters, Jousselin, Leveque et al., Povidone Iodine Mouthwash, Gargle, and Nasal Spray to Reduce Nasopharyngeal Viral Load in Patients With COVID-19: A Randomized Clinical Trial, JAMA Otolaryngol. Head Neck Surg, doi:10.1001/jamaoto.2020.5490
Guimaraes, Marques, Castro, Secco, Porto et al., Reducing the viral load of SARS-CoV-2 in the saliva of patients with COVID-19, Oral Dis, doi:10.1111/odi.14118
Haridas, Sasidhar, Nath, Abhithaj, Sabu et al., Compounds of Citrus medica and Zingiber officinale for COVID-19 inhibition: In silico evidence for cues from Ayurveda, Future J. Pharm. Sci, doi:10.1186/s43094-020-00171-6
Harrel, Molinari, Aerosols and splatter in dentistry: A brief review of the literature and infection control implications, J. Am. Dent. Assoc, doi:10.14219/jada.archive.2004.0207
Hasanoglu, Korukluoglu, Asilturk, Cosgun, Kalem et al., Higher viral loads in asymptomatic COVID-19 patients might be the invisible part of the iceberg, Infection
Hassandarvish, Tiong, Mohamed, Arumugam, Ananthanarayanan et al., In vitro virucidal activity of povidone iodine gargle and mouthwash against SARS-CoV-2: Implications for dental practice, Br. Dent. J, doi:10.1038/s41415-020-2402-0
Hoffmann, Kleine-Weber, Schroeder, Kruger, Herrler et al., SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor, Cell, doi:10.1016/j.cell.2020.02.052
Huang, Huang, Use of chlorhexidine to eradicate oropharyngeal SARS-CoV-2 in COVID-19 patients, J. Med. Virol, doi:10.1002/jmv.26954
Jain, Grover, Singh, Sharma, Das et al., Chlorhexidine: An effective anticovid mouth rinse, J. Indian Soc. Periodontol, doi:10.4103/jisp.jisp_824_20
Kariwa, Sawa, Kobayashi, Inactivation of SARS-CoV-2 by povidone-iodine products: Implications for effective mouth rinsing and gargling, Jpn. J. Vet. Res
Kasiri, Rouhani, Salehifar, Ghazaeian, Fallah, Mometasone furoate nasal spray in the treatment of patients with COVID-19 olfactory dysfunction: A randomized, double blind clinical trial, Int. Immunopharmacol, doi:10.1016/j.intimp.2021.107871
Khan, Parab, Paranjape, Repurposing 0.5% povidone iodine solution in otorhinolaryngology practice in COVID-19 pandemic, Am. J. Otolaryngol, doi:10.1016/j.amjoto.2020.102618
Klimisch, Andreae, Tillmann, A systematic approach for evaluating the quality of experimental toxicological and ecotoxicological data, Regul. Toxicol. Pharmacol, doi:10.1006/rtph.1996.1076
Koch-Heier, Hoffmann, Schindler, Lussi, Planz, Inactivation of SARS-CoV-2 through Treatment with the Mouth Rinsing Solutions ViruProX((R)) and BacterX((R)) Pro, Microorganisms, doi:10.3390/microorganisms9030521
Komine, Yamaguchi, Okamoto, Yamamoto, Virucidal activity of oral care products against SARS-CoV-2 in vitro, J. Oral Maxillofac. Surg. Med. Pathol, doi:10.1016/j.ajoms.2021.02.002
Kontos, Efficacy of "Essential Iodine Drops" against Severe Acute Respiratory Syndrome-Coronavirus 2 (SARS-CoV-2), PLoS ONE, doi:10.1371/journal.pone.0254341
Laferl, Seitz, Baier-Grabner, Kelani, Scholz et al., Evaluation of RT-qPCR of mouthwash and buccal swabs for detection of SARS-CoV-2 in children and adults, Am. J. Infect. Control, doi:10.1016/j.ajic.2021.10.019
Liang, Yuan, Wei, Wang, Zhang et al., In-Vivo Toxicity Studies and In-Vitro Inactivation of SARS-CoV-2 by Povidone-iodine In-situ Gel Forming Formulations, bioRxiv
Martinez Lamas, Diz Dios, Perez Rodriguez, Del Campo Perez, Cabrera Alvargonzalez et al., Is povidone iodine mouthwash effective against SARS-CoV-2? First in vivo tests, Oral Dis, doi:10.1111/odi.13526
Meister, Todt, Bruggemann, Steinmann, Banava et al., Virucidal activity of nasal sprays against severe acute respiratory syndrome coronavirus-2, J. Hosp. Infect, doi:10.1016/j.jhin.2021.10.019
Michel, Farber, Dilas, Heuft, Tammer et al., A combined oro-nasopharyngeal swab is more sensitive than mouthwash in detecting SARS-CoV-2 by a high-throughput PCR assay, Infection, doi:10.1007/s15010-021-01600-1
Moakes, Davies, Stamataki, Grover, Formulation of a Composite Nasal Spray Enabling Enhanced Surface Coverage and Prophylaxis of SARS-COV-2, Adv. Mater, doi:10.1002/adma.202008304
Mohamed, Baharom, Sulaiman, Rashid, Ken et al., Early viral clearance among COVID-19 patients when gargling with povidone-iodine and essential oils-A clinical trial, medRvix, doi:10.1101/2020.09.07.20180448
Mora-Aguilera, Martinez-Bustamante, Acevedo-Sanchez, Coria-Contreras, Guzman-Hernandez et al., Surveillance Web System and Mouthwash-Saliva qPCR for Labor Ambulatory SARS-CoV-2 Detection and Prevention, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph19031271
Morokutti-Kurz, Froba, Graf, Grosse, Grassauer et al., Iota-carrageenan neutralizes SARS-CoV-2 and inhibits viral replication in vitro, PLoS ONE, doi:10.1371/journal.pone.0237480
Munoz-Basagoiti, Perez-Zsolt, Leon, Blanc, Raich-Regue et al., Mouthwashes with CPC Reduce the Infectivity of SARS-CoV-2 Variants In Vitro, J. Dent. Res
Page, Mckenzie, Bossuyt, Boutron, Hoffmann et al., The PRISMA 2020 statement: An updated guideline for reporting systematic reviews, BMJ, doi:10.1136/bmj.n71
Paolacci, Ergoren, De Forni, Manara, Poddesu et al., In vitro and clinical studies on the efficacy of alpha-cyclodextrin and hydroxytyrosol against SARS-CoV-2 infection, Eur. Rev. Med. Pharmacol. Sci, doi:10.26355/eurrev_202112_27337
Pattanshetty, Narayana, Radhakrishnan, Povidone-iodine gargle as a prophylactic intervention to interrupt the transmission of SARS-CoV-2, Oral Dis, doi:10.1111/odi.13378
Paull, Luscombe, Castellarnau, Heery, Bobardt et al., Protective Effects of Astodrimer Sodium 1% Nasal Spray Formulation against SARS-CoV-2 Nasal Challenge in K18-hACE2 Mice, Viruses, doi:10.3390/v13081656
Pelletier, Tessema, Frank, Westover, Brown et al., Efficacy of Povidone-Iodine Nasal and Oral Antiseptic Preparations Against Severe Acute Respiratory Syndrome-Coronavirus 2 (SARS-CoV-2), Ear Nose Throat J, doi:10.1177/0145561320957237
Peng, Xu, Li, Cheng, Zhou et al., Transmission routes of 2019-nCoV and controls in dental practice, Int. J. Oral Sci, doi:10.1038/s41368-020-0075-9
Pyrc, Milewska, Duran, Botwina, Dabrowska et al., SARS-CoV-2 inhibition using a mucoadhesive, amphiphilic chitosan that may serve as an anti-viral nasal spray, Sci. Rep, doi:10.1038/s41598-021-99404-8
Robinson, Moakes, Grover, Low Acyl Gellan as an Excipient to Improve the Sprayability and Mucoadhesion of Iota Carrageenan in a Nasal Spray to Prevent Infection With SARS-CoV-2, Front. Med. Technol, doi:10.3389/fmedt.2021.687681
Rodriguez, Saunier, Rigaill, Audoux, Botelho-Nevers et al., Evaluation of in vitro activity of copper gluconate against SARS-CoV-2 using confocal microscopy-based high content screening, J. Trace Elem. Med. Biol, doi:10.1016/j.jtemb.2021.126818
Rodriguez-Casanovas, La Rosa, Bello-Lemus, Rasperini, Acosta-Hoyos, Virucidal Activity of Different Mouthwashes Using a Novel Biochemical Assay, Healthcare, doi:10.3390/healthcare10010063
Santos, Da Fonseca Orcina, Brito Reia, Ribeiro, Grotto et al., Virucidal Activity of the Antiseptic Mouthwash and Dental Gel Containing Anionic Phthalocyanine Derivative: In vitro Study, Clin. Cosmet. Investig. Dent, doi:10.2147/CCIDE.S315419
Saud, Tyrrell, Zaragkoulias, Protty, Statkute et al., The SARS-CoV2 envelope differs from host cells, exposes procoagulant lipids, and is disrupted in vivo by oral rinses, J. Lipid Res, doi:10.1016/j.jlr.2022.100208
Schneider, Schwarz, Burkholder, Kopp-Schneider, Edler et al., ToxRTool", a new tool to assess the reliability of toxicological data, Toxicol. Lett, doi:10.1016/j.toxlet.2009.05.013
Schurmann, Aljubeh, Tiemann, Sudhoff, Mouthrinses against SARS-CoV-2: Anti-inflammatory effectivity and a clinical pilot study, Eur. Arch. Otorhinolaryngol, doi:10.1007/s00405-021-06873-8
Seneviratne, Balan, Ko, Udawatte, Lai et al., Efficacy of commercial mouth-rinses on SARS-CoV-2 viral load in saliva: Randomized control trial in Singapore, Infection, doi:10.1007/s15010-020-01563-9
Sharad, Kapur, Indian Herb-Derived Phytoconstituent-Based Antiviral, Antimicrobial and Antifungal Formulation: An Oral Rinse Candidate for Oral Hygiene and the Potential Prevention of COVID-19 Outbreaks, Pathogens, doi:10.3390/pathogens10091130
Shet, Hong, Igo, Cataldo, Bhaskar, In Vitro Evaluation of the Virucidal Activity of Different Povidone-Iodine Formulations against Murine and Human Coronaviruses, Infect. Dis. Ther, doi:10.1007/s40121-021-00536-1
Shet, Westover, Hong, Igo, Cataldo et al., In vitro inactivation of SARS-CoV-2 using a povidone-iodine oral rinse, BMC Oral Health, doi:10.1186/s12903-022-02082-9
Shewale, Gelhaus, Ratcliff, Hernandez-Kapila, In vitro antiviral activity of stabilized chlorine dioxide containing oral care products, Oral Dis, doi:10.1111/odi.14044
Statkute, Rubina, O'donnell, Thomas, Stanton, Brief Report: The Virucidal Efficacy of Oral Rinse Components against SARS-CoV-2 In Vitro, bioRxiv, doi:10.1101/2020.11.13.381079
Steinhauer, Meister, Todt, Krawczyk, Passvogel et al., Comparison of the in-vitro efficacy of different mouthwash solutions targeting SARS-CoV-2 based on the European Standard EN 14476, J. Hosp. Infect, doi:10.1016/j.jhin.2021.01.031
Tateyama-Makino, Abe-Yutori, Iwamoto, Tsutsumi, Tsuji et al., The inhibitory effects of toothpaste and mouthwash ingredients on the interaction between the SARS-CoV-2 spike protein and ACE2, and the protease activity of TMPRSS2 in vitro, PLoS ONE, doi:10.1371/journal.pone.0257705
Teagle, Clem, Yoon, Virucidal Properties of Molecular Iodine Oral Rinse Against SARS-CoV-2, Compend. Contin. Educ. Dent
Tiong, Hassandarvish, Bakar, Mohamed, Wan Sulaiman et al., The effectiveness of various gargle formulations and salt water against SARS-CoV-2, Sci. Rep, doi:10.1038/s41598-021-99866-w
Van Doremalen, Bushmaker, Morris, Holbrook, Gamble et al., Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1, N. Engl. J. Med, doi:10.1056/NEJMc2004973
Vergara-Buenaventura, Castro-Ruiz, Use of mouthwashes against COVID-19 in dentistry, Br. J. Oral Maxillofac. Surg, doi:10.1016/j.bjoms.2020.08.016
Wang, Zhao, Gao, Gao, Wang et al., SARS-CoV-2: Structure, Biology, and Structure-Based Therapeutics Development, Front. Cell. Infect. Microbiol, doi:10.3389/fcimb.2020.587269
Westover, Ferrer, Vazquez, Bethencourt-Mirabal, Go, In Vitro Virucidal Effect of Intranasally Delivered Chlorpheniramine Maleate Compound against Severe Acute Respiratory Syndrome Coronavirus 2, Cureus
Xu, Wang, Hoskin, Cugini, Markowitz et al., Differential effects of antiseptic mouth rinses on SARS-CoV-2 infectivity in vitro, bioRxiv, doi:10.3390/pathogens10030272
Yadalam, Varatharajan, Rajapandian, Chopra, Arumuganainar et al., Antiviral Essential Oil Components against SARS-CoV-2 in Pre-procedural Mouth Rinses for Dental Settings during COVID-19: A Computational Study, Front. Chem, doi:10.3389/fchem.2021.642026
Yoon, Yoon, Song, Yoon, Lim et al., Clinical Significance of a High SARS-CoV-2 Viral Load in the Saliva, J. Korean Med. Sci, doi:10.3346/jkms.2020.35.e195
Yuki, Fujiogi, Koutsogiannaki, COVID-19 pathophysiology: A review, Clin. Immunol, doi:10.1016/j.clim.2020.108427
Zarabanda, Vukkadala, Phillips, Qian, Mfuh et al., The Effect of Povidone-Iodine Nasal Spray on Nasopharyngeal SARS-CoV-2 Viral Load: A Randomized Control Trial, doi:10.1002/lary.29935
DOI record:
{
"DOI": "10.3390/ijerph191912148",
"ISSN": [
"1660-4601"
],
"URL": "http://dx.doi.org/10.3390/ijerph191912148",
"abstract": "<jats:p>Severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) is a global and evolving pandemic associated with heavy health and financial burdens. Considering the oral cavity as the major reservoir for SARS-CoV-2, a systematic review and meta-analysis were conducted to assess the efficacy of mouth rinses and nasal sprays in reducing the salivary viral load of SARS-CoV-2. All in vivo and in vitro studies that assessed the virucidal efficacy of mouth rinses and nasal sprays against SARS-CoV-2 and were published in the English language from December 2019 to April 2022 were considered for analyses. Special Medical Subject Headings terms were used to search Pubmed, Scopus, Embase Ovid, and Web of Science databases. The toxicological data reliability assessment tool (ToxRToool) was used to assess the quality of the included studies. Thirty-three studies (11 in vivo and 22 in vitro) were deemed eligible for inclusion in this analysis. Results of the pooled data showed that povidone-iodine is the most efficacious intervention in vivo in terms of reducing the SARS-CoV-2 salivary viral load, followed by chlorhexidine. The mean difference in the viral load was 86% and 72%, respectively. Similarly, povidone-iodine was associated with the highest log10 reduction value (LRV) in vitro, followed by cetylpyridinium chloride, (LRV = 2.938 (p < 0.0005) and LRV = 2.907 (p = 0.009), respectively). Povidone-iodine-based oral and nasal preparations showed favourable results in terms of reducing SARS-CoV-2 viral loads both in vivo and in vitro. Considering the limited number of patients in vivo, further studies among larger cohorts are recommended.</jats:p>",
"alternative-id": [
"ijerph191912148"
],
"author": [
{
"affiliation": [],
"family": "Idrees",
"given": "Majdy",
"sequence": "first"
},
{
"affiliation": [],
"family": "McGowan",
"given": "Bridget",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6357-0535",
"affiliation": [],
"authenticated-orcid": false,
"family": "Fawzy",
"given": "Amr",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Abuderman",
"given": "Abdulwahab Ali",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Balasubramaniam",
"given": "Ramesh",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5951-8280",
"affiliation": [],
"authenticated-orcid": false,
"family": "Kujan",
"given": "Omar",
"sequence": "additional"
}
],
"container-title": "International Journal of Environmental Research and Public Health",
"container-title-short": "IJERPH",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
9,
26
]
],
"date-time": "2022-09-26T03:13:27Z",
"timestamp": 1664162007000
},
"deposited": {
"date-parts": [
[
2022,
9,
27
]
],
"date-time": "2022-09-27T07:59:56Z",
"timestamp": 1664265596000
},
"indexed": {
"date-parts": [
[
2022,
9,
28
]
],
"date-time": "2022-09-28T05:41:35Z",
"timestamp": 1664343695115
},
"is-referenced-by-count": 0,
"issue": "19",
"issued": {
"date-parts": [
[
2022,
9,
25
]
]
},
"journal-issue": {
"issue": "19",
"published-online": {
"date-parts": [
[
2022,
10
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
9,
25
]
],
"date-time": "2022-09-25T00:00:00Z",
"timestamp": 1664064000000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/1660-4601/19/19/12148/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "12148",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
9,
25
]
]
},
"published-online": {
"date-parts": [
[
2022,
9,
25
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1016/j.clim.2020.108427",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.3389/fcimb.2020.587269",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.14219/jada.archive.2004.0207",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1007/s15010-020-01548-8",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1186/s40902-020-00256-5",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1056/NEJMc2004973",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.3201/eid2609.201806",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"key": "ref8",
"unstructured": "Australian Dental Association: Risk Management Principles for Dentistry during the COVID-19 Pandemichttps://www.ada.org.au/getdoc/d3eecaba-d0aa-4803-a7ea-89facae6f274/Risk-Management-Principles-for-Dentistry-(1).aspx"
},
{
"key": "ref9",
"unstructured": "American Dental Association: ADA Interim Guidance for Minimizing Risk of COVID-19 Transmissionhttps://snlg.iss.it/wp-content/uploads/2020/04/ADA_COVID_Int_Guidance_Treat_Pts.pdf"
},
{
"article-title": "Antimicrobial mouthwashes (gargling) and nasal sprays to protect healthcare workers when undertaking aerosol-generating procedures (AGPs) on patients without suspected or confirmed COVID-19 infection",
"author": "Burton",
"first-page": "CD013628",
"journal-title": "Cochrane Database Syst. Rev.",
"key": "ref10",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.3389/fdmed.2021.648547",
"article-title": "Efficacy of Mouth Rinses against SARS-CoV-2: A Scoping Review",
"author": "Amber",
"doi-asserted-by": "crossref",
"first-page": "648547",
"journal-title": "Front. Dent. Med.",
"key": "ref11",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.4317/jced.57406",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.3390/jcm11061692",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.1136/bmj.n71",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"key": "ref15",
"unstructured": "European Standard: EN14476:2013+A1:2015, Chemical Disinfectants and Antiseptics—Quantitative Suspension Test for the Evaluation of Virucidal Activity in the Medical Area—Test Method and Requirements (Phase 2/Step 1)https://standards.iteh.ai/catalog/standards/cen/5e78911a-aedf-4456-90b7-39e1649f8acf/en-14476-2013a1-2015"
},
{
"DOI": "10.1371/journal.pone.0260884",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.1016/j.toxlet.2009.05.013",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1006/rtph.1996.1076",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1016/j.cmi.2021.05.028",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1111/odi.14086",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1016/j.heliyon.2021.e07346",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1016/j.jebdp.2021.101584",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1007/s00784-020-03549-1",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1111/odi.14118",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1111/odi.13526",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1007/s15010-020-01563-9",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1007/s00405-021-06873-8",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.3346/jkms.2020.35.e195",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1002/lary.29935",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1099/jmm.0.001508",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1111/jopr.13209",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.1111/jopr.13220",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1001/jamaoto.2020.3053",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.1002/jmv.26554",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1371/journal.pone.0254341",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1101/2020.05.18.103184",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.1177/0145561320957237",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.1186/s12903-022-02082-9",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.1111/odi.14044",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"article-title": "Virucidal Properties of Molecular Iodine Oral Rinse Against SARS-CoV-2",
"author": "Teagle",
"first-page": "e13",
"journal-title": "Compend. Contin. Educ. Dent.",
"key": "ref40",
"volume": "43",
"year": "2022"
},
{
"DOI": "10.1007/s40121-020-00316-3",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.1099/jgv.0.001578",
"doi-asserted-by": "publisher",
"key": "ref42"
},
{
"DOI": "10.1038/s41415-020-2402-0",
"doi-asserted-by": "publisher",
"key": "ref43"
},
{
"DOI": "10.1016/j.ajoms.2021.02.002",
"doi-asserted-by": "publisher",
"key": "ref44"
},
{
"article-title": "Inactivation of SARS-CoV-2 by povidone-iodine products: Implications for effective mouth rinsing and gargling",
"author": "Kariwa",
"first-page": "183",
"journal-title": "Jpn. J. Vet. Res.",
"key": "ref45",
"volume": "69",
"year": "2021"
},
{
"DOI": "10.3390/microorganisms9030521",
"doi-asserted-by": "publisher",
"key": "ref46"
},
{
"DOI": "10.1016/j.jhin.2021.10.019",
"doi-asserted-by": "publisher",
"key": "ref47"
},
{
"DOI": "10.1038/s41598-021-99404-8",
"doi-asserted-by": "publisher",
"key": "ref48"
},
{
"DOI": "10.2147/CCIDE.S315419",
"doi-asserted-by": "publisher",
"key": "ref49"
},
{
"DOI": "10.1038/s41598-021-99866-w",
"doi-asserted-by": "publisher",
"key": "ref50"
},
{
"DOI": "10.1016/j.jhin.2021.01.031",
"doi-asserted-by": "publisher",
"key": "ref51"
},
{
"DOI": "10.1016/j.cell.2020.02.052",
"doi-asserted-by": "publisher",
"key": "ref52"
},
{
"DOI": "10.1038/s41541-021-00346-z",
"doi-asserted-by": "publisher",
"key": "ref53"
},
{
"DOI": "10.1016/j.amjoto.2020.102884",
"doi-asserted-by": "publisher",
"key": "ref54"
},
{
"DOI": "10.1016/j.adaj.2021.05.021",
"doi-asserted-by": "publisher",
"key": "ref55"
},
{
"DOI": "10.1016/j.sdentj.2022.01.005",
"doi-asserted-by": "publisher",
"key": "ref56"
},
{
"DOI": "10.2147/CCIDE.S295423",
"doi-asserted-by": "publisher",
"key": "ref57"
},
{
"DOI": "10.4178/epih.e2021051",
"doi-asserted-by": "publisher",
"key": "ref58"
},
{
"DOI": "10.2147/IJGM.S328486",
"doi-asserted-by": "publisher",
"key": "ref59"
},
{
"DOI": "10.1001/jamaoto.2020.5490",
"doi-asserted-by": "publisher",
"key": "ref60"
},
{
"DOI": "10.1002/jmv.26954",
"doi-asserted-by": "publisher",
"key": "ref61"
},
{
"DOI": "10.1016/j.intimp.2021.107871",
"doi-asserted-by": "publisher",
"key": "ref62"
},
{
"DOI": "10.1007/s12070-021-02616-7",
"doi-asserted-by": "publisher",
"key": "ref63"
},
{
"DOI": "10.1016/j.amjoto.2020.102618",
"doi-asserted-by": "publisher",
"key": "ref64"
},
{
"DOI": "10.1016/j.jlr.2022.100208",
"doi-asserted-by": "publisher",
"key": "ref65"
},
{
"article-title": "Comparison of effectiveness of chlorine dioxide mouthwash and chlorhexidine gluconate mouthwash in reduction of oral viral load in patients with COVID-19",
"author": "Avhad",
"first-page": "27",
"journal-title": "Indian J. Public Health Res. Dev.",
"key": "ref66",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0256401",
"doi-asserted-by": "publisher",
"key": "ref67"
},
{
"DOI": "10.2147/IJN.S313093",
"doi-asserted-by": "publisher",
"key": "ref68"
},
{
"DOI": "10.1016/j.ajic.2021.10.019",
"doi-asserted-by": "publisher",
"key": "ref69"
},
{
"DOI": "10.1007/s15010-021-01600-1",
"doi-asserted-by": "publisher",
"key": "ref70"
},
{
"DOI": "10.3390/ijerph19031271",
"doi-asserted-by": "publisher",
"key": "ref71"
},
{
"DOI": "10.3390/v13081656",
"doi-asserted-by": "publisher",
"key": "ref72"
},
{
"DOI": "10.1016/j.xphs.2021.01.017",
"doi-asserted-by": "publisher",
"key": "ref73"
},
{
"DOI": "10.4103/jisp.jisp_824_20",
"doi-asserted-by": "publisher",
"key": "ref74"
},
{
"DOI": "10.1080/20002297.2022.2030094",
"doi-asserted-by": "publisher",
"key": "ref75"
},
{
"DOI": "10.1371/journal.pone.0259943",
"doi-asserted-by": "publisher",
"key": "ref76"
},
{
"DOI": "10.3390/v13122345",
"doi-asserted-by": "publisher",
"key": "ref77"
},
{
"DOI": "10.1016/j.bbrep.2021.101187",
"doi-asserted-by": "publisher",
"key": "ref78"
},
{
"DOI": "10.1186/s43094-020-00171-6",
"doi-asserted-by": "publisher",
"key": "ref79"
},
{
"DOI": "10.1002/adma.202008304",
"doi-asserted-by": "publisher",
"key": "ref80"
},
{
"DOI": "10.1371/journal.pone.0237480",
"doi-asserted-by": "publisher",
"key": "ref81"
},
{
"DOI": "10.1177/00220345211029269",
"doi-asserted-by": "publisher",
"key": "ref82"
},
{
"DOI": "10.26355/eurrev_202112_27337",
"doi-asserted-by": "publisher",
"key": "ref83"
},
{
"DOI": "10.1016/j.jtemb.2021.126818",
"doi-asserted-by": "publisher",
"key": "ref84"
},
{
"DOI": "10.3390/pathogens10091130",
"doi-asserted-by": "publisher",
"key": "ref85"
},
{
"DOI": "10.1371/journal.pone.0257705",
"doi-asserted-by": "publisher",
"key": "ref86"
},
{
"DOI": "10.3389/fchem.2021.642026",
"doi-asserted-by": "publisher",
"key": "ref87"
},
{
"DOI": "10.3390/healthcare10010063",
"doi-asserted-by": "publisher",
"key": "ref88"
},
{
"DOI": "10.3389/fmedt.2021.687681",
"doi-asserted-by": "publisher",
"key": "ref89"
},
{
"DOI": "10.7759/cureus.10501",
"doi-asserted-by": "publisher",
"key": "ref90"
},
{
"DOI": "10.1101/2020.12.02.408575",
"doi-asserted-by": "publisher",
"key": "ref91"
},
{
"DOI": "10.1101/2020.09.07.20180448",
"doi-asserted-by": "publisher",
"key": "ref92"
},
{
"DOI": "10.1101/2020.11.13.381079",
"doi-asserted-by": "publisher",
"key": "ref93"
},
{
"DOI": "10.3390/pathogens10030272",
"doi-asserted-by": "publisher",
"key": "ref94"
},
{
"DOI": "10.1111/odi.14067",
"doi-asserted-by": "publisher",
"key": "ref95"
},
{
"DOI": "10.1101/2020.10.28.359257",
"doi-asserted-by": "publisher",
"key": "ref96"
},
{
"DOI": "10.1007/s40121-021-00536-1",
"doi-asserted-by": "publisher",
"key": "ref97"
},
{
"DOI": "10.1016/j.jvoice.2021.01.007",
"doi-asserted-by": "publisher",
"key": "ref98"
},
{
"DOI": "10.1177/0145561320932318",
"doi-asserted-by": "publisher",
"key": "ref99"
},
{
"DOI": "10.1016/j.bjoms.2020.08.016",
"doi-asserted-by": "publisher",
"key": "ref100"
},
{
"DOI": "10.6061/clinics/2020/e2328",
"doi-asserted-by": "publisher",
"key": "ref101"
},
{
"DOI": "10.1016/j.jhin.2020.09.001",
"doi-asserted-by": "publisher",
"key": "ref102"
},
{
"DOI": "10.3390/jcm9041126",
"doi-asserted-by": "publisher",
"key": "ref103"
},
{
"DOI": "10.1038/s41368-020-0075-9",
"doi-asserted-by": "publisher",
"key": "ref104"
},
{
"DOI": "10.1111/odi.13378",
"doi-asserted-by": "publisher",
"key": "ref105"
}
],
"reference-count": 105,
"references-count": 105,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/1660-4601/19/19/12148"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Health, Toxicology and Mutagenesis",
"Public Health, Environmental and Occupational Health"
],
"subtitle": [],
"title": "Efficacy of Mouth Rinses and Nasal Spray in the Inactivation of SARS-CoV-2: A Systematic Review and Meta-Analysis of In Vitro and In Vivo Studies",
"type": "journal-article",
"volume": "19"
}