Differential Effects of Antiseptic Mouth Rinses on SARS-CoV-2 Infectivity In Vitro
et al., Pathogens, doi:10.3390/pathogens10030272, Mar 2021
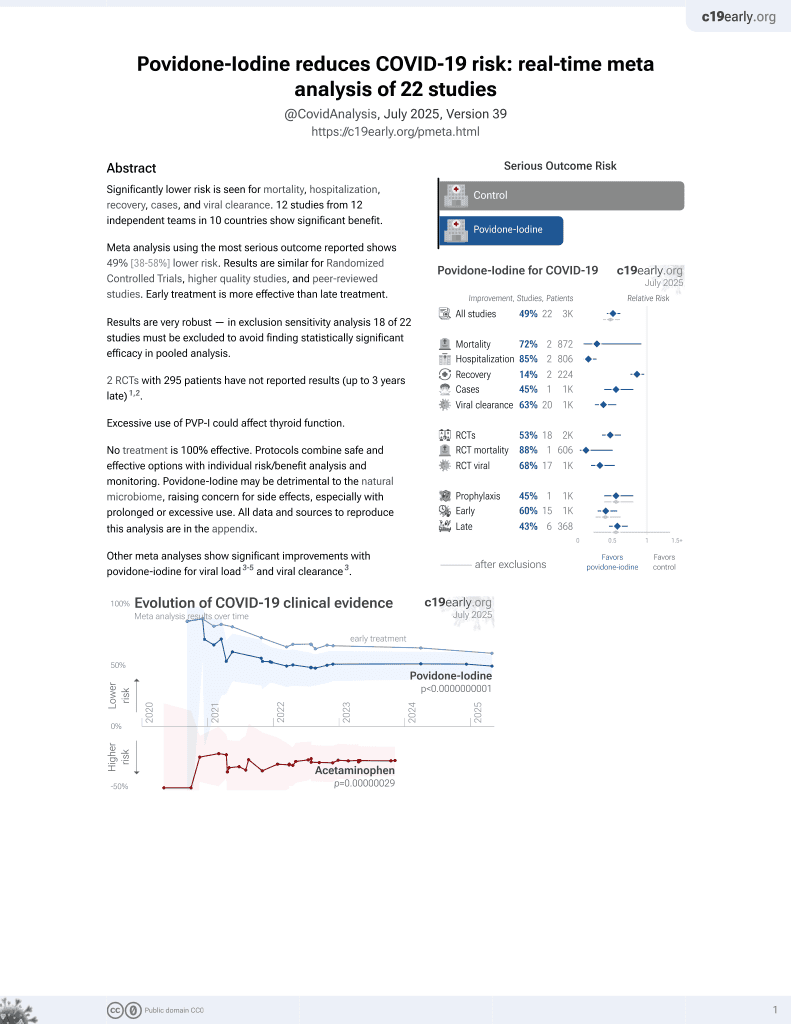
PVP-I for COVID-19
15th treatment shown to reduce risk in
February 2021, now with p = 0.000000000016 from 22 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
In vitro study showing that PVP-I and other mouthwashes inactivated replication-competent SARS-CoV-2.
9 preclinical studies support the efficacy of povidone-iodine for COVID-19:
1.
Xu et al., Differential Effects of Antiseptic Mouth Rinses on SARS-CoV-2 Infectivity In Vitro, Pathogens, doi:10.3390/pathogens10030272.
2.
Tucker et al., In vitro inactivation of SARS-CoV-2 with 0.5% povidone iodine nasal spray (Nasodine) at clinically relevant concentrations and timeframes using tissue culture and PCR based assays, bioRxiv, doi:10.1101/2021.01.31.426979.
3.
Pelletier et al., Efficacy of Povidone-Iodine Nasal and Oral Antiseptic Preparations Against Severe Acute Respiratory Syndrome-Coronavirus 2 (SARS-CoV-2), Ear, Nose & Throat Journal, doi:10.1177/0145561320957237.
4.
Frank et al., In Vitro Efficacy of a Povidone-Iodine Nasal Antiseptic for Rapid Inactivation of SARS-CoV-2, JAMA Otolaryngol Head Neck Surg, doi:10.1001/jamaoto.2020.3053.
5.
Meister et al., Virucidal Efficacy of Different Oral Rinses Against Severe Acute Respiratory Syndrome Coronavirus 2, The Journal of Infectious Diseases, doi:10.1093/infdis/jiaa471.
6.
Anderson et al., Povidone-Iodine Demonstrates Rapid In Vitro Virucidal Activity Against SARS-CoV-2, The Virus Causing COVID-19 Disease, Infectious Diseases and Therapy, doi:10.1007/s40121-020-00316-3.
7.
Hassandarvish et al., Povidone iodine gargle and mouthwash, British Dental Journal volume, doi:10.1038/s41415-020-1794-1.
Xu et al., 1 Mar 2021, peer-reviewed, 7 authors.
In vitro studies are an important part of preclinical research, however results may be very different in vivo.
Differential Effects of Antiseptic Mouth Rinses on SARS-CoV-2 Infectivity In Vitro
Pathogens, doi:10.3390/pathogens10030272
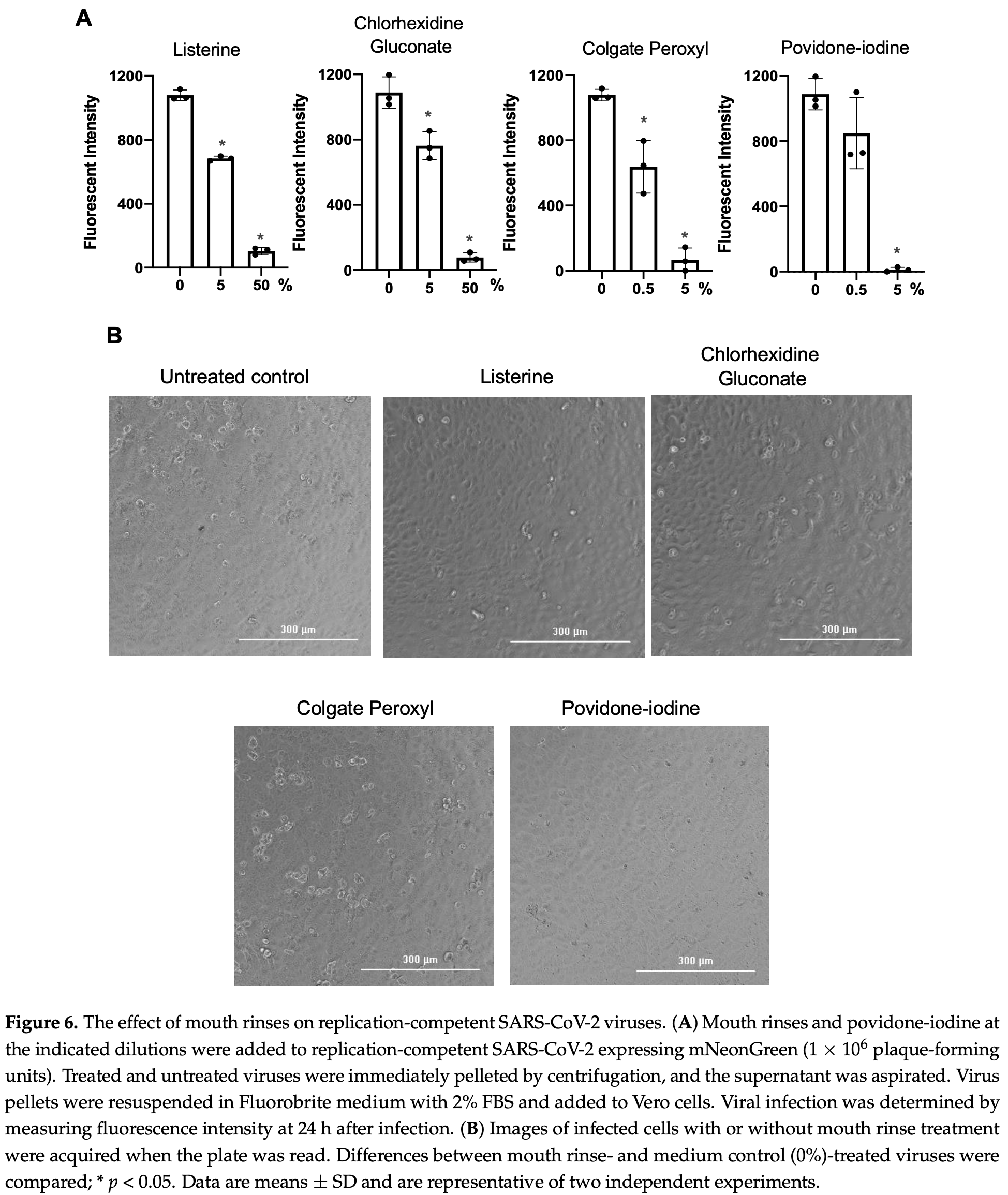
Severe acute respiratory syndrome-related coronavirus (SARS-CoV-2) is detectable in saliva from asymptomatic individuals, suggesting a potential benefit from the use of mouth rinses to suppress viral load and reduce virus spread. Published studies on the reduction of SARS-CoV-2-induced cytotoxic effects by mouth rinses do not exclude antiseptic mouth rinse-associated cytotoxicity. Here, we determined the effect of commercially available mouth rinses and antiseptic povidone-iodine on the infectivity of replication-competent SARS-CoV-2 viruses and of pseudotyped SARS-CoV-2 viruses. We first determined the effect of mouth rinses on cell viability to ensure that antiviral activity was not a consequence of mouth rinse-induced cytotoxicity. Colgate Peroxyl (hydrogen peroxide) exhibited the most cytotoxicity, followed by povidone-iodine, chlorhexidine gluconate (CHG), and Listerine (essential oils and alcohol). The potent antiviral activities of Colgate Peroxyl mouth rinse and povidone-iodine were the consequence of rinse-mediated cellular damage when the products were present during infection. The potency of CHG was greater when the product was not washed off after virus attachment, suggesting that the prolonged effect of mouth rinses on cells impacts the antiviral outcome. To minimalize mouth rinse-associated cytotoxicity, mouth rinse was largely removed from treated viruses by centrifugation prior to infection of cells. A 5% (v/v) dilution of Colgate Peroxyl or povidone-iodine completely blocked viral infectivity. A similar 5% (v/v) dilution of Listerine or CHG had a moderate suppressive effect on the virus, but a 50% (v/v) dilution of Listerine or CHG blocked viral infectivity completely. Mouth rinses inactivated the virus without prolonged incubation. The new infectivity assay, with limited impacts of mouth rinse-associated cytotoxicity, showed the differential effects of mouth rinses on SARS-CoV-2 infection. Our results indicate that mouth rinses can significantly reduce virus infectivity, suggesting a potential benefit for reducing SARS-CoV-2 spread.
In conclusion, all mouth rinses tested inactivated replication-competent SARS-CoV-2 viruses and pseudotyped viruses expressing spike proteins. The cytotoxic effects of mouth rinses should be considered when assessing their antiviral activities. Since diluted Listerine and CHG exhibited no cytotoxic effects, these products may be good candidates to reduce virus spread. Studies of the antiviral effects of mouth rinses are needed for determining their clinical efficacy in reducing virus spread, particularly in asymptomatic individuals.
Supplementary Materials: The following are available online at https://www.mdpi.com/2076-081 7/10/3/272/s1. Figure S1
References
Anderson, Sivalingam, Kang, Ananthanarayanan, Arumugam et al., Povidone-Iodine Demonstrates Rapid In Vitro Virucidal Activity Against SARS-CoV-2, The Virus Causing COVID-19 Disease, Infect. Dis, doi:10.1007/s40121-020-00316-3
Baqui, Kelley, Jabra-Rizk, Depaola, Falkler et al., In vitro effect of oral antiseptics on human immunodeficiency virus-1 and Herpes simplex virus type 1, J. Clin. Periodontol, doi:10.1034/j.1600-051x.2001.028007610.x
Bidra, Pelletier, Westover, Frank, Brown et al., Rapid In-Vitro Inactivation of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Using Povidone-Iodine Oral Antiseptic Rinse, J. Prosthodont, doi:10.1111/jopr.13209
Carrouel, Conte, Fisher, Gonçalves, Dussart et al., COVID-19: A Recommendation to Examine the Effect of Mouthrinses with β-Cyclodextrin Combined with Citrox in Preventing Infection and Progression, J. Clin. Med, doi:10.3390/jcm9041126
Carrouel, Gonçalves, Conte, Campus, Fisher et al., Antiviral Activity of Reagents in Mouth Rinses against SARS-CoV-2, J. Dent. Res, doi:10.1177/0022034520967933
Eggers, Koburger-Janssen, Eickmann, Zorn, In Vitro Bactericidal and Virucidal Efficacy of Povidone-Iodine Gargle/Mouthwash Against Respiratory and Oral Tract Pathogens, Infect. Dis, doi:10.1007/s40121-018-0200-7
Fine, Furgang, Korik, Olshan, Barnett et al., Reduction of viable bacteria in dental aerosols by preprocedural rinsing with an antiseptic mouthrinse, Am. J. Dent
Fine, Korik, Furgang, Myers, Olshan et al., Assessing pre-procedural subgingival irrigation and rinsing with an antiseptic mouthrinse to reduce bacteremia, J. Am. Dent. Assoc, doi:10.14219/jada.archive.1996.0276
Holmes, Zhang, Bieniasz, Single-Cell and Single-Cycle Analysis of HIV-1 Replication, PLoS Pathog, doi:10.1371/journal.ppat.1004961
Koletsi, Belibasakis, Eliades, Interventions to Reduce Aerosolized Microbes in Dental Practice: A Systematic Review with Network Meta-analysis of Randomized Controlled Trials, J. Dent. Res, doi:10.1177/0022034520943574
Lee, Kim, Lee, Lee, Kim et al., Clinical Course and Molecular Viral Shedding Among Asymptomatic and Symptomatic Patients With SARS-CoV-2 Infection in a Community Treatment Center in the Republic of Korea, JAMA Intern. Med, doi:10.1001/jamainternmed.2020.3862
Meiller, Silva, Ferreira, Jabra-Rizk, Kelley et al., Efficacy of Listerine Antiseptic in reducing viral contamination of saliva, J. Clin. Periodontol, doi:10.1111/j.1600-051X.2005.00673.x
Meister, Bruggemann, Todt, Conzelmann, Muller et al., Virucidal efficacy of different oral rinses against SARS-CoV-2, J. Infect. Dis, doi:10.1093/infdis/jiaa471
Mittal, Manjunath, Ranjan, Kaushik, Kumar et al., COVID-19 pandemic: Insights into structure, function, and hACE2 receptor recognition by SARS-CoV-2, PLoS Pathog, doi:10.1371/journal.ppat.1008762
O'donnell, Thomas, Stanton, Maillard, Murphy et al., Potential role of oral rinses targeting the viral lipid envelope in SARS-CoV-2 infection, Function
Park, Park, Effect of chlorhexidine on the in vitro and in vivo herpes simplex virus infection, Oral. Surg. Oral. Med. Oral. Pathol, doi:10.1016/0030-4220(89)90320-4
Petersen, Koopmans, Go, Hamer, Petrosillo et al., Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics, Lancet Infect. Dis, doi:10.1016/S1473-3099(20)30484-9
Rogers, Zhao, Huang, Beutler, Burns et al., Isolation of potent SARS-CoV-2 neutralizing antibodies and protection from disease in a small animal model, Science
Sriwilaijaroen, Hiramatsu, Takahashi, Suzuki, Ito et al., Mechanisms of the action of povidone-iodine against human and avian influenza A viruses: Its effects on hemagglutination and sialidase activities, Virol. J, doi:10.1186/1743-422X-6-124
Thomson, The Effect of Hydrogen Peroxide on the Permeability of the Cell, J. Exp. Biol
To, Tsang, Leung, Tam, Wu et al., Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: An observational cohort study, Lancet Infect. Dis, doi:10.1016/S1473-3099(20)30196-1
To, Tsang, Yip, Chan, Wu et al., Consistent Detection of 2019 Novel Coronavirus in Saliva, Clin. Infect. Dis, doi:10.1093/cid/ciaa149
Ward, Blakely, Joner, Mammalian cells are not killed by DNA single-strand breaks caused by hydroxyl radicals from hydrogen peroxide, Radiat Res, doi:10.2307/3576760
Wei, Lin, Duan, Huang, Lu et al., Asymptomatic COVID-19 Patients Can Contaminate Their Surroundings: An Environment Sampling Study, mSphere, doi:10.1128/mSphere.00442-20
Who, None
Who, Transmission of SARS-CoV-2: Implication for Infection Prevention Precautions
Wu, Zhao, Yu, Chen, Wang et al., A new coronavirus associated with human respiratory disease in China, Nature, doi:10.1038/s41586-020-2008-3
Xie, Muruato, Lokugamage, Narayanan, Zhang et al., An Infectious cDNA Clone of SARS-CoV-2, Cell Host Microbe, doi:10.1016/j.chom.2020.04.004
Zeidler, Karpinski, SARS-CoV, MERS-CoV, SARS-CoV-2 Comparison of Three Emerging Coronaviruses, Jundishapur. J. Microbiol, doi:10.5812/jjm.103744
Zhu, Zhang, Wang, Li, Yang et al., A Novel Coronavirus from Patients with Pneumonia in China, N. Engl. J. Med, doi:10.1056/NEJMoa2001017
DOI record:
{
"DOI": "10.3390/pathogens10030272",
"ISSN": [
"2076-0817"
],
"URL": "http://dx.doi.org/10.3390/pathogens10030272",
"abstract": "<jats:p>Severe acute respiratory syndrome-related coronavirus (SARS-CoV-2) is detectable in saliva from asymptomatic individuals, suggesting a potential benefit from the use of mouth rinses to suppress viral load and reduce virus spread. Published studies on the reduction of SARS-CoV-2-induced cytotoxic effects by mouth rinses do not exclude antiseptic mouth rinse-associated cytotoxicity. Here, we determined the effect of commercially available mouth rinses and antiseptic povidone-iodine on the infectivity of replication-competent SARS-CoV-2 viruses and of pseudotyped SARS-CoV-2 viruses. We first determined the effect of mouth rinses on cell viability to ensure that antiviral activity was not a consequence of mouth rinse-induced cytotoxicity. Colgate Peroxyl (hydrogen peroxide) exhibited the most cytotoxicity, followed by povidone-iodine, chlorhexidine gluconate (CHG), and Listerine (essential oils and alcohol). The potent antiviral activities of Colgate Peroxyl mouth rinse and povidone-iodine were the consequence of rinse-mediated cellular damage when the products were present during infection. The potency of CHG was greater when the product was not washed off after virus attachment, suggesting that the prolonged effect of mouth rinses on cells impacts the antiviral outcome. To minimalize mouth rinse-associated cytotoxicity, mouth rinse was largely removed from treated viruses by centrifugation prior to infection of cells. A 5% (v/v) dilution of Colgate Peroxyl or povidone-iodine completely blocked viral infectivity. A similar 5% (v/v) dilution of Listerine or CHG had a moderate suppressive effect on the virus, but a 50% (v/v) dilution of Listerine or CHG blocked viral infectivity completely. Mouth rinses inactivated the virus without prolonged incubation. The new infectivity assay, with limited impacts of mouth rinse-associated cytotoxicity, showed the differential effects of mouth rinses on SARS-CoV-2 infection. Our results indicate that mouth rinses can significantly reduce virus infectivity, suggesting a potential benefit for reducing SARS-CoV-2 spread.</jats:p>",
"alternative-id": [
"pathogens10030272"
],
"author": [
{
"affiliation": [],
"family": "Xu",
"given": "Chuan",
"sequence": "first"
},
{
"affiliation": [],
"family": "Wang",
"given": "Annie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hoskin",
"given": "Eileen R.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5321-0608",
"affiliation": [],
"authenticated-orcid": false,
"family": "Cugini",
"given": "Carla",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Markowitz",
"given": "Kenneth",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chang",
"given": "Theresa L.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fine",
"given": "Daniel H.",
"sequence": "additional"
}
],
"container-title": "Pathogens",
"container-title-short": "Pathogens",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
3,
1
]
],
"date-time": "2021-03-01T06:26:33Z",
"timestamp": 1614579993000
},
"deposited": {
"date-parts": [
[
2021,
4,
27
]
],
"date-time": "2021-04-27T03:25:14Z",
"timestamp": 1619493914000
},
"funder": [
{
"DOI": "10.13039/100000002",
"award": [
"R01AI36948"
],
"doi-asserted-by": "publisher",
"name": "National Institutes of Health"
}
],
"indexed": {
"date-parts": [
[
2024,
4,
30
]
],
"date-time": "2024-04-30T13:52:12Z",
"timestamp": 1714485132587
},
"is-referenced-by-count": 41,
"issue": "3",
"issued": {
"date-parts": [
[
2021,
3,
1
]
]
},
"journal-issue": {
"issue": "3",
"published-online": {
"date-parts": [
[
2021,
3
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
3,
1
]
],
"date-time": "2021-03-01T00:00:00Z",
"timestamp": 1614556800000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2076-0817/10/3/272/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "272",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2021,
3,
1
]
]
},
"published-online": {
"date-parts": [
[
2021,
3,
1
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"key": "ref1",
"unstructured": "WHOhttps://covid19.who.int/"
},
{
"key": "ref2"
},
{
"DOI": "10.1056/NEJMoa2001017",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1371/journal.ppat.1008762",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.5812/jjm.103744",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"key": "ref6",
"unstructured": "Transmission of SARS-CoV-2: Implication for Infection Prevention Precautions. World Health Organizationhttps://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions"
},
{
"DOI": "10.1016/S1473-3099(20)30196-1",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1128/mSphere.00442-20",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.1001/jamainternmed.2020.3862",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.14219/jada.archive.1996.0276",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"article-title": "Reduction of viable bacteria in dental aerosols by preprocedural rinsing with an antiseptic mouthrinse",
"author": "Fine",
"first-page": "219",
"journal-title": "Am. J. Dent.",
"key": "ref11",
"volume": "6",
"year": "1993"
},
{
"DOI": "10.1177/0022034520943574",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.1111/j.1600-051X.2005.00673.x",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.1016/0030-4220(89)90320-4",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1093/function/zqaa002",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.3390/jcm9041126",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.1177/0022034520967933",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1111/jopr.13209",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1093/infdis/jiaa471",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1007/s40121-020-00316-3",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1016/j.chom.2020.04.004",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1038/s41586-020-2008-3",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1126/science.abc7520",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1371/journal.ppat.1004961",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1016/S1473-3099(20)30484-9",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1093/cid/ciaa149",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1007/s40121-018-0200-7",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.2307/3576760",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1242/jeb.5.3.252",
"article-title": "The Effect of Hydrogen Peroxide on the Permeability of the Cell",
"author": "THOMSON",
"doi-asserted-by": "crossref",
"first-page": "252",
"journal-title": "J. Exp. Biol.",
"key": "ref29",
"volume": "5",
"year": "1928"
},
{
"DOI": "10.1186/1743-422X-6-124",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"key": "ref31",
"unstructured": "WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care is Safer Carehttps://www.paho.org/col/index.php?option=com_docman&view=download&alias=264-who-guidelines-on-hand-hygiene&category_slug=publicaciones-ops-oms-colombia&Itemid=688"
},
{
"DOI": "10.1034/j.1600-051x.2001.028007610.x",
"doi-asserted-by": "publisher",
"key": "ref32"
}
],
"reference-count": 32,
"references-count": 32,
"relation": {
"has-preprint": [
{
"asserted-by": "object",
"id": "10.1101/2020.12.01.405662",
"id-type": "doi"
}
]
},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2076-0817/10/3/272"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Differential Effects of Antiseptic Mouth Rinses on SARS-CoV-2 Infectivity In Vitro",
"type": "journal-article",
"volume": "10"
}