Preprocedural Viral Load Effects of Oral Antiseptics on SARS-CoV-2 in Patients with COVID-19: A Systematic Review
et al., Biomedicines, doi:10.3390/biomedicines11061694, Jun 2023
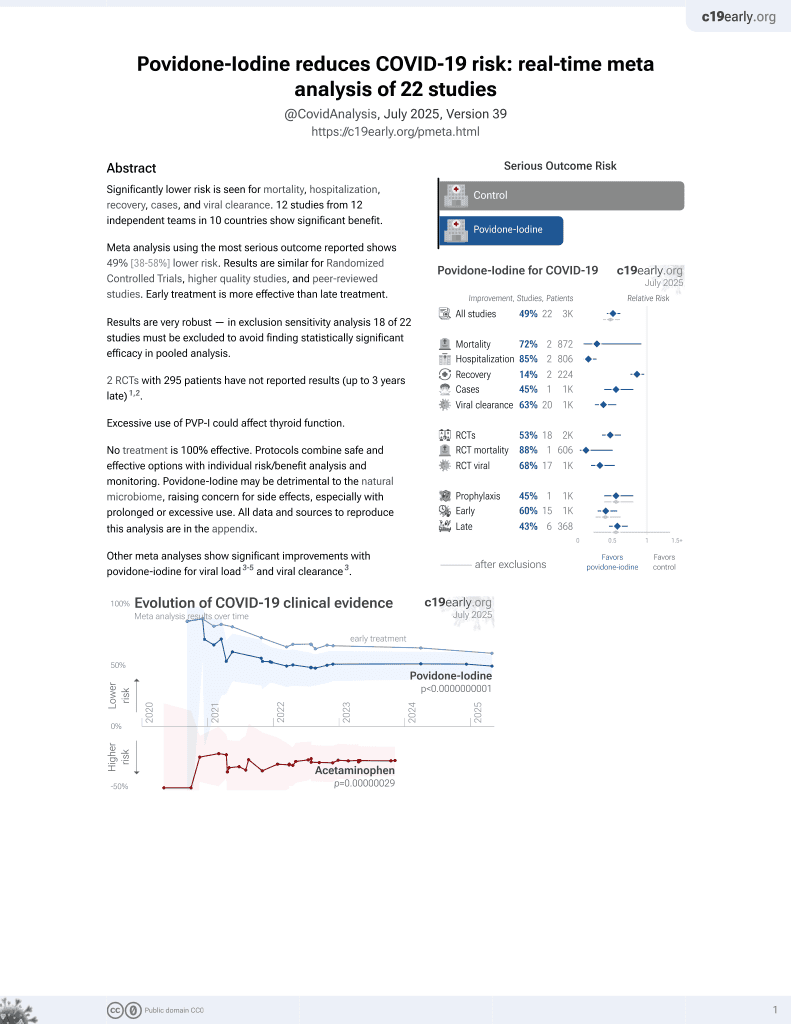
PVP-I for COVID-19
15th treatment shown to reduce risk in
February 2021, now with p = 0.000000000016 from 22 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
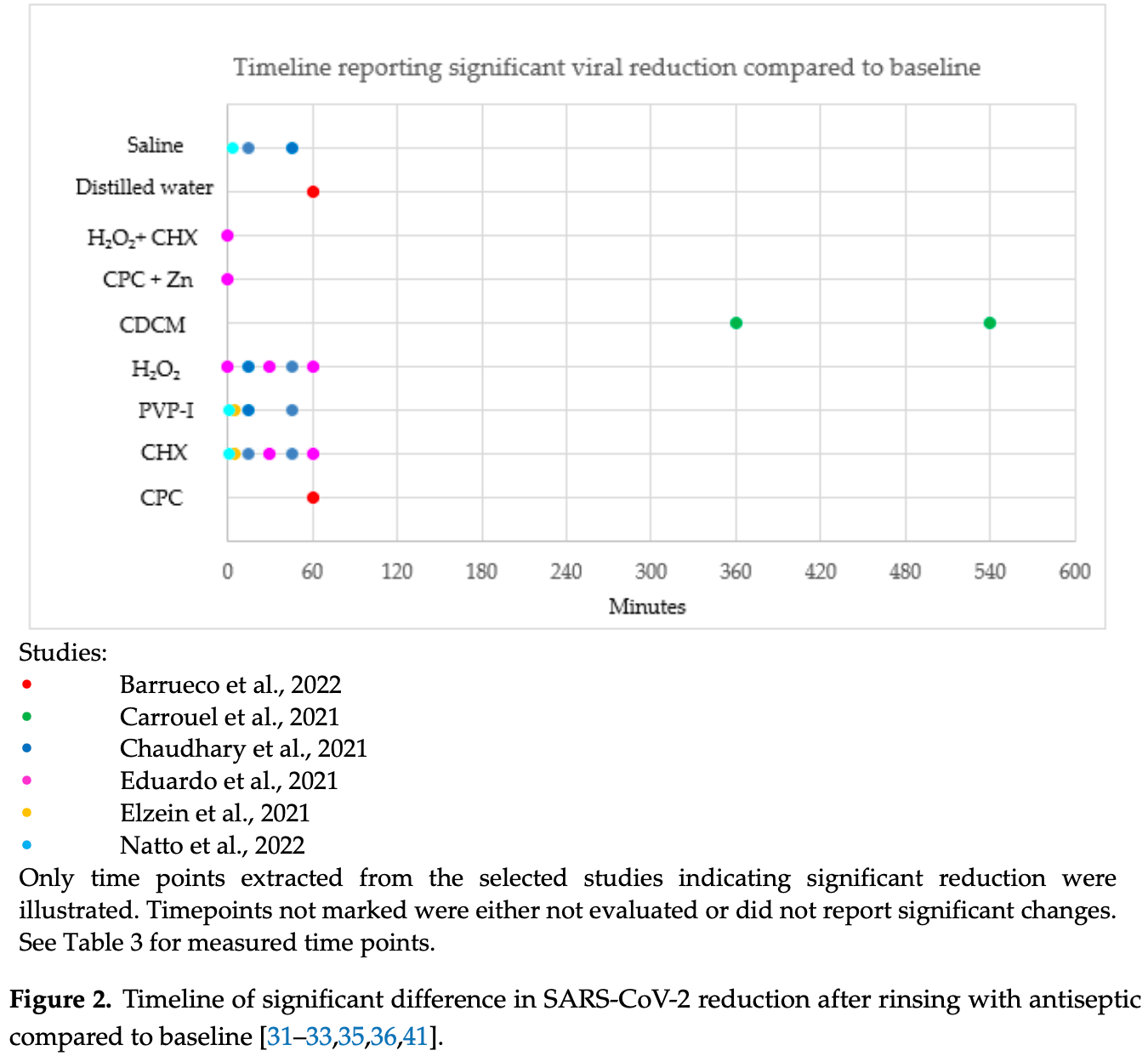
Systematic review of 14 RCTs, showing significant reductions in short-term viral load with mouth rinses cetylpyridinium chloride, β-cyclodextrin and citrox, hydrogen peroxide, chlorhexidine, povidone-iodine, hypochlorous acid, saline, and water.
3 meta-analyses show significant improvements with povidone-iodine for viral load1-3 and
viral clearance1.
Currently there are 22 povidone-iodine for COVID-19 studies, showing 72% lower mortality [8‑92%], 85% lower hospitalization [73‑91%], and 45% fewer cases [20‑62%].
Study covers povidone-iodine, cetylpyridinium chloride, chlorhexidine, hydrogen peroxide, and hypochlorous acid.
1.
Hasan et al., Effects of Chlorhexidine and Povidone-Iodine on the SARS-CoV-2 Load: A Systematic Review and Meta-analysis, European Journal of Dentistry, doi:10.1055/s-0042-1753470.
Ting et al., 12 Jun 2023, peer-reviewed, 5 authors.
Contact: thinkdentallearninginstitute@gmail.com (corresponding author), abdahlkemper@gmail.com, schwartzjj1@gmail.com, manzel.woodfork@jefferson.edu, jon.suzuki@temple.edu.
Preprocedural Viral Load Effects of Oral Antiseptics on SARS-CoV-2 in Patients with COVID-19: A Systematic Review
Biomedicines, doi:10.3390/biomedicines11061694
1) There are limited clinical trials to support the effectiveness of mouth rinses when used as a preprocedural rinse against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This systematic review aims to evaluate the efficacy of antiseptic mouth rinses as a preprocedural rinse in reducing SARS-CoV-2 oral viral load in-vivo. (2) Methods: A literature search was conducted through November 2022 for the following databases: PubMed, Web of Science, Cochrane Library, and Google Scholar. The evaluated outcomes were quantitative changes in viral load and the statistical significance of that change after using antiseptic mouth rinses. (3) Results: 14 randomized controlled trials (RCT) were selected for risk of bias assessment and data extraction. (4) Conclusion: Within the limits of this systematic review, preprocedural mouth rinses may significantly reduce SARS-CoV-2 in the mouth, thus, reducing the viral particles available for airborne dispersion. Preprocedural mouth rinses may be an effective strategy for reducing airborne SARS-CoV-2 dispersion in the environment. Their use may be a preventive strategy to reduce the spread of COVID-19 in selected medical and healthcare facilities, including dental clinics. Potential preprocedural mouth rinses are identified for use as an integral part of safe practice for healthcare protocols.
Author Contributions: Conceptualization, M.T. and J.B.S.; resources, A.D., J.J.S., M.W., M.T. and J.B.S.; data curation, M.T.; writing-original draft preparation, A.D., J.J.S. and M.T.; writing-review and editing, A.D., J.J.S., M.W., M.T. and J.B.S.; visualization, M.W. and M.T.; supervision, J.B.S. and M.T.; project administration, M.T. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest: The authors declare no conflict of interest.
References
Aguilera, Viñas, Sierra, Vinuesa, De Henestrosa et al., Substantivity of mouth-rinse formulations containing cetylpyridinium chloride and O-cymen-5-ol: A randomizedcrossover trial, BMC Oral Health, doi:10.1186/s12903-022-02688-z
Alemany, Millat-Martinez, Ouchi, Corbacho-Monné, Bordoy et al., Self-collected mid-nasal swabs and saliva specimens, compared with nasopharyngeal swabs, for SARS-CoV-2 detection in mild COVID-19 patients, J. Infect, doi:10.1016/j.jinf.2021.09.012
Alemany, Perez-Zsolt, Raich-Regue, Munoz-Basagoiti, Ouchi et al., Cetylpyridinium Chloride Mouthwash to Reduce Shedding of Infectious SARS-CoV-2: A Double-Blind Randomized Clinical Trial, J. Dent. Res, doi:10.1177/00220345221102310
Almanza-Reyes, Moreno, Plascencia-López, Alvarado-Vera, Patrón-Romero et al., Evaluation of silver nanoparticles for the prevention of SARS-CoV-2 infection in health workers: In vitro and in vivo, doi:10.1371/journal.pone.0256401
Alshaeri, Natto, A contemporary look at COVID-19 medications: Available and potentially effective drugs, Eur. Rev. Med. Pharmacol. Sci
Anderson, Patterson, Richards, Pitol, Edwards et al., CPC-containing oral rinses inactivate SARS-CoV-2 variants and are active in the presence of human saliva, J. Med. Microbiol, doi:10.1099/jmm.0.001508
Anderson, Sivalingam, Kang, Ananthanarayanan, Arumugam et al., Povidone-Iodine Demonstrates Rapid In Vitro Virucidal Activity Against SARS-CoV-2, The Virus Causing COVID-19 Disease, Infect. Dis. Ther, doi:10.1007/s40121-020-00316-3
Arefin, Rumi, Uddin, Banu, Khan et al., Virucidal effect of povidone iodine on COVID-19 in the nasopharynx: An open-label randomized clinical trial, Indian J. Otolaryngol. Head Neck Surg. Off. Publ. Assoc. Otolaryngol. India, doi:10.1007/s12070-021-02616-7
Avhad, Bhanushali, Sachdev, Save, Kalra et al., Comparison of Effectiveness of Chlorine Dioxide Mouthwash and Chlorhexidine Gluconate Mouthwash in Reduction of Oral Viral Load in Patients with COVID-19, Indian J. Public Health Res. Dev, doi:10.37506/ijphrd.v11i11.11343
Barkvoll, Rølla, Svendsen, Interaction between chlorhexidine digluconate and sodium lauryl sulfate in vivo, J. Clin. Periodontol, doi:10.1111/j.1600-051X.1989.tb02143.x
Belcaro, Corsi, Agus, Cesarone, Cornelli et al., Thrombo-prophylaxis prevents thrombotic events in home-managed COVID patients. A registry study, Minerva Med, doi:10.23736/S0026-4806.20.06688-4
Berchier, Slot, Van Der Weijden, The efficacy of 0.12% chlorhexidine mouthrinse compared with 0.2% on plaque accumulation and periodontal parameters: A systematic review, J. Clin. Periodontol, doi:10.1111/j.1600-051X.2010.01575.x
Biber, Lev, Mandelboim, Lustig, Harmelin et al., The role of mouthwash sampling in SARS-CoV-2 diagnosis, Eur. J. Clin. Microbiol. Infect. Dis, doi:10.1007/s10096-021-04320-4
Bidra, Pelletier, Westover, Frank, Brown et al., Rapid In-Vitro Inactivation of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Using Povidone-Iodine Oral Antiseptic Rinse, J. Prosthodont, doi:10.1111/jopr.13209
Bonesvoll, Lokken, Rolla, Influence of concentration, time, temperature and pH on the retention of chlorhexidine in the human oral cavity after mouth rinses, Arch. Oral Biol, doi:10.1016/0003-9969(74)90089-2
Brito-Reia, Da Silva Bastos, Vilhena, Honório, Da Costa Alves et al., Populationbased virucidal phthalocyanine gargling/rinsing protocol to reduce the risk of coronavirus disease-2019: A community trial, Infect. Control
Buttenheim, SARS-CoV-2 Vaccine Acceptance: We May Need to Choose Our Battles, Ann. Intern. Med
Carrouel, Valette, Gadea, Esparcieux, Illes et al., Use of an antiviral mouthwash as a barrier measure in the SARS-CoV-2 transmission in adults with asymptomatic to mild COVID-19: A multicentre, randomized, double-blind controlled trial, Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis, doi:10.1016/j.cmi.2021.05.028
Challacombe, Kirk-Bayley, Sunkaraneni, Combes, None, J. Povidone iodine. Br. Dent. J, doi:10.1038/s41415-020-1589-4
Chaudhary, Melkonyan, Meethil, Saraswat, Hall et al., Estimating salivary carriage of severe acute respiratory syndrome coronavirus 2 in nonsymptomatic people and efficacy of mouthrinse in reducing viral load: A randomized controlled trial, J. Am. Dent. Assoc, doi:10.1016/j.adaj.2021.05.021
Choudhury, Shabnam, Ahsan, Kabir, Md Khan et al., Effect of 1% Povidone Iodine Mouthwash/Gargle, Nasal and Eye Drop in COVID-19 patient, Bioresearch Commun, doi:10.3329/brc.v7i1.54245
Chumpitaz-Cerrate, Chávez-Rimache, Ruiz-Ramirez, Franco-Quino, Erazo-Paredes, Evaluation of Current Evidence on the Use of Oral Antiseptics Against SARS-CoV-2: A Narrative Review, J. Int. Soc. Prev. Community Dent, doi:10.4103/jispcd.JISPCD_65_22
Cieplik, Jakubovics, Buchalla, Maisch, Hellwig et al., Resistance Toward Chlorhexidine in Oral. Bacteria-Is There Cause for Concern?, Front. Microbiol, doi:10.3389/fmicb.2019.00587
Costa, Brites, Vaz, De Santana, Dos Santos et al., Chlorhexidine mouthwash reduces the salivary viral load of SARS-CoV-2: A randomized clinical trial, Oral Dis, doi:10.1111/odi.14086
Cousido, Tomas Carmona, Garcia-Caballero, Limeres, Alvarez et al., In vivo substantivity of 0.12% and 0.2% chlorhexidine mouthrinses on salivary bacteria, Clin. Oral Investig, doi:10.1007/s00784-009-0320-2
Davis, Assaf, Mccorkell, Wei, Low et al., Characterizing long COVID in an international cohort: 7 months of symptoms and their impact, EClinicalMedicine, doi:10.1016/j.eclinm.2021.101019
Dawes, Circadian rhythms in human salivary flow rate and composition, J. Physiol, doi:10.1113/jphysiol.1972.sp009721
Deana, Seiffert, Aravena-Rivas, Alonso-Coello, Munoz-Millan et al., Recommendations for Safe Dental Care: A Systematic Review of Clinical Practice Guidelines in the First Year of the COVID-19 Pandemic, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph181910059
Di Domênico, Cesca, Ponciano, Santos, Lenz et al., Effectiveness of hydrogen peroxide as auxiliary treatment for hospitalized COVID-19 patients in Brazil: Preliminary results of a randomized double-blind clinical trial, Epidemiol. Health, doi:10.4178/epih.e2021032
Di Domênico, Collares, Dos Santos, Lenz, Antunes et al., Hydrogen peroxide as an auxiliary treatment for COVID-19 in Brazil: A randomized double-blind clinical trial, Epidemiol. Health, doi:10.4178/epih.e2021051
Eduardo, Correa, Heller, Daep, Benitez et al., Salivary SARS-CoV-2 load reduction with mouthwash use: A randomized pilot clinical trial, doi:10.1016/j.heliyon.2021.e07346
Eggers, Infectious Disease Management and Control with Povidone Iodine, Infect. Dis. Ther, doi:10.1007/s40121-019-00260-x
Eggers, Koburger-Janssen, Eickmann, Zorn, In Vitro Bactericidal and Virucidal Efficacy of Povidone-Iodine Gargle/Mouthwash Against Respiratory and Oral Tract Pathogens, Infect. Dis. Ther, doi:10.1007/s40121-018-0200-7
Elworthy, Greenman, Doherty, Newcombe, Addy, The substantivity of a number of oral hygiene products determined by the duration of effects on salivary bacteria, J. Periodontol, doi:10.1902/jop.1996.67.6.572
Elzein, Abdel-Sater, Fakhreddine, Hanna, Feghali et al., In vivo evaluation of the virucidal efficacy of chlorhexidine and povidone-iodine mouthwashes against salivary SARS-CoV-2. A randomized-controlled clinical trial, J. Evid. Based Dent. Pract, doi:10.1016/j.jebdp.2021.101584
Emilson, Fornell, Effect of toothbrushing with chlorhexidine gel on salivary microflora, oral hygiene, and caries. Scand, J. Dent. Res, doi:10.1111/j.1600-0722.1976.tb00495.x
Fantozzi, Pampena, Pierangeli, Oliveto, Sorrentino et al., Efficacy of antiseptic mouthrinses against SARS-CoV-2: A prospective randomized placebo-controlled pilot study, Am. J. Otolaryngol, doi:10.1016/j.amjoto.2022.103549
Ferrer, Barrueco, Martinez-Beneyto, Mateos-Moreno, Ausina-Márquez et al., Clinical evaluation of antiseptic mouth rinses to reduce salivary load of SARS-CoV-2, doi:10.1038/s41598-021-03461-y
Friedland, Tucker, Goodall, Julander, Mendenhall et al., In vivo (human) and in vitro inactivation of SARS-CoV-2 with 0.5% povidone-iodine nasal spray, Aust. J. Otolaryngol, doi:10.21037/ajo-21-40
Garcia-Caballero, Quintas, Prada-Lopez, Seoane, Donos et al., Chlorhexidine substantivity on salivary flora and plaque-like biofilm: An in situ model, PLoS ONE, doi:10.1371/journal.pone.0083522
Garcia-Sanchez, Peña-Cardelles, Ordonez-Fernandez, Montero-Alonso, Kewalramani et al., Povidone-Iodine as a Pre-Procedural Mouthwash to Reduce the Salivary Viral Load of SARS-CoV-2: A Systematic Review of Randomized Controlled Trials, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph19052877
Gjermo, Bonesvoll, Rolla, Relationship between plaque-inhibiting effect and retention of chlorhexidine in the human oral cavity, Arch. Oral Biol, doi:10.1016/0003-9969(74)90090-9
Goldfarb, Tilley, Al-Rawahi, Srigley, Ford et al., Self-Collected Saline Gargle Samples as an Alternative to Health Care Worker-Collected Nasopharyngeal Swabs for COVID-19 Diagnosis in Outpatients, J. Clin. Microbiol, doi:10.1128/JCM.02427-20
Gorbalenya, Baker, Baric, De Groot, Drosten et al., The species Severe acute respiratory syndrome-related coronavirus: Classifying 2019-nCoV and naming it SARS-CoV-2
Gottsauner, Michaelides, Schmidt, Scholz, Buchalla et al., A prospective clinical pilot study on the effects of a hydrogen peroxide mouthrinse on the intraoral viral load of SARS-CoV-2, Clin. Oral Investig, doi:10.1007/s00784-020-03549-1
Guenezan, Garcia, Strasters, Jousselin, Lévêque et al., Povidone Iodine Mouthwash, Gargle, and Nasal Spray to Reduce Nasopharyngeal Viral Load in Patients with COVID-19: A Randomized Clinical Trial, JAMA Otolaryngol. Head Neck Surg, doi:10.1001/jamaoto.2020.5490
Guerrero Bernal, Reyes Uribe, Salazar Flores, Varela Hernández, Gómez-Sandoval et al., Oral Antiseptics against SARS-CoV-2: A Literature Review, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph19148768
Hasan, Rumi, Banu, Uddin, Islam et al., Virucidal effect of povidone iodine on COVID-19 in the nasopharynx: A structured summary of a study protocol for an open-label randomized clinical trial, Trials, doi:10.1186/s13063-020-04963-2
He, Lau, Wu, Deng, Wang et al., Temporal dynamics in viral shedding and transmissibility of COVID-19, Nat. Med, doi:10.1038/s41591-020-0869-5
Hsieh, Goldsmith, Schaub, Divenere, Kuo et al., Structure-based design of prefusion-stabilized SARS-CoV-2 spikes, Science, doi:10.1126/science.abd0826
Huang, Huang, Use of chlorhexidine to eradicate oropharyngeal SARS-CoV-2 in COVID-19 patients, J. Med. Virol, doi:10.1002/jmv.26954
Johansson, Quandelacy, Kada, Prasad, Steele et al., SARS-CoV-2 Transmission From People Without COVID-19 Symptoms, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2020.35057
Joynt, Wu, Understanding COVID-19: What does viral RNA load really mean?, Lancet Infect. Dis
Kampf, Acquired resistance to chlorhexidine-Is it time to establish an 'antiseptic stewardship' initiative?, J. Hosp. Infect, doi:10.1016/j.jhin.2016.08.018
Kampf, Biocidal Agents Used for Disinfection Can Enhance Antibiotic Resistance in Gram-Negative Species, Antibiotics, doi:10.3390/antibiotics7040110
Kampf, Todt, Pfaender, Steinmann, Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents, J. Hosp. Infect, doi:10.1016/j.jhin.2020.01.022
Kariwa, Fujii, Takashima, Inactivation of SARS coronavirus by means of povidone-iodine, physical conditions and chemical reagents, Dermatology, doi:10.1159/000089211
Keitel, Jensen, Feldt, Fischer, Bode et al., Reconvalescent plasma/camostat mesylate in early SARS-CoV-2 Q-PCR positive high-risk individuals (RES-Q-HR): A structured summary of a study protocol for a randomized controlled trial, Trials, doi:10.1186/s13063-021-05181-0
Khan, Kazmi, Iqbal, Iqbal, Ali et al., A quadruple blind, randomised controlled trial of gargling agents in reducing intraoral viral load among hospitalised COVID-19 patients: A structured summary of a study protocol for a randomised controlled trial, Trials, doi:10.1186/s13063-020-04634-2
Khan, Parab, Paranjape, Repurposing 0.5% povidone iodine solution in otorhinolaryngology practice in COVID-19 pandemic, Am. J. Otolaryngol, doi:10.1016/j.amjoto.2020.102618
Koch-Heier, Hoffmann, Schindler, Lussi, Planz, Inactivation of SARS-CoV-2 through Treatment with the Mouth Rinsing Solutions ViruProX((R)) and BacterX((R)) Pro. Microorganisms 2021, doi:10.3390/microorganisms9030521
Koletsi, Belibasakis, Eliades, Interventions to Reduce Aerosolized Microbes in Dental Practice: A Systematic Review with Network Meta-analysis of Randomized Controlled Trials, J. Dent. Res, doi:10.1177/0022034520943574
Komine, Yamaguchi, Okamoto, Yamamoto, Virucidal activity of oral care products against SARS-CoV-2 in vitro, J. Oral Maxillofac. Surg. Med. Pathol, doi:10.1016/j.ajoms.2021.02.002
Kowalski, Sanabria, Ridge, Ng, Bree et al., COVID-19 pandemic: Effects and evidence-based recommendations for otolaryngology and head and neck surgery practice, Head Neck, doi:10.1002/hed.26164
Lee, Lee, Lee, Park, Suh et al., The antiplaque and bleeding control effects of a cetylpyridinium chloride and tranexamic acid mouth rinse in patients with gingivitis, J. Periodontal Implant. Sci
Linley, Denyer, Mcdonnell, Simons, Maillard, Use of hydrogen peroxide as a biocide: New consideration of its mechanisms of biocidal action, J. Antimicrob. Chemother, doi:10.1093/jac/dks129
Loe, Schiott, The effect of mouthrinses and topical application of chlorhexidine on the development of dental plaque and gingivitis in man, J. Periodontal Res, doi:10.1111/j.1600-0765.1970.tb00696.x
Martínez Lamas, Diz Dios, Pérez Rodríguez, Del Campo Pérez, Cabrera Alvargonzalez et al., Is povidone iodine mouthwash effective against SARS-CoV-2? First in vivo tests, Oral Dis, doi:10.1111/odi.13526
Maynard, Jenkins, Moran, Addy, Newcombe et al., A 6-month home usage trial of a 1% chlorhexidine toothpaste (II). Effects on the oral microflora, J. Clin. Periodontol, doi:10.1111/j.1600-051X.1993.tb00345.x
Mccoy, Wehler, Rich, Garcia, Miller et al., Adverse events associated with chlorhexidine use: Results from the Department of Veterans Affairs Dental Diabetes Study, J. Am. Dent. Assoc, doi:10.14219/jada.archive.2008.0134
Meister, Bruggemann, Todt, Conzelmann, Muller et al., Virucidal Efficacy of Different Oral Rinses Against Severe Acute Respiratory Syndrome Coronavirus 2, J. Infect. Dis, doi:10.1093/infdis/jiaa471
Meister, Gottsauner, Schmidt, Heinen, Todt et al., Mouthrinses against SARS-CoV-2-High antiviral effectivity by membrane disruption in vitro translates to mild effects in a randomized placebo-controlled clinical trial, Virus Res, doi:10.1016/j.virusres.2022.198791
Mendoza, Ubillús, Bolívar, Palacios, Lopez et al., Antiviral effect of mouthwashes against SARS-CoV-2: A systematic review, Saudi Dent. J, doi:10.1016/j.sdentj.2022.01.006
Meng, Hua, Bian, Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine, J. Dent. Res, doi:10.1177/0022034520914246
Meselson, Droplets and Aerosols in the Transmission of SARS-CoV-2, N. Engl. J. Med, doi:10.1056/NEJMc2009324
Meyers, Robison, Milici, Alam, Quillen et al., Lowering the transmission and spread of human coronavirus, J. Med. Virol, doi:10.1002/jmv.26514
Mohamed, Baharom, Sulaiman, Rashid, Ken et al., Early viral clearance among COVID-19 patients when gargling with povidone-iodine and essential oils-A clinical trial
Mukherjee, Esper, Buchheit, Arters, Adkins et al., Randomized, double-blind, placebo-controlled clinical trial to assess the safety and effectiveness of a novel dual-action oral topical formulation against upper respiratory infections, BMC Infect. Dis, doi:10.1186/s12879-016-2177-8
Mukhtar, Qassim, Al Qahtani, Danjuma, Mohamedali et al., A randomized trial on the regular use of potent mouthwash in COVID-19 treatment, MedRxiv
Munoz-Basagoiti, Perez-Zsolt, Leon, Blanc, Raich-Regue et al., Mouthwashes with CPC Reduce the Infectivity of SARS-CoV-2 Variants In Vitro, J. Dent. Res, doi:10.1177/00220345211029269
Natto, Alshaeri, Characteristics of First Cases of Coronavirus Disease 2019 and the Effort to Prevent the Early Spread of COVID-19 in Saudi Arabia, Risk Manag. Healthc. Policy, doi:10.2147/RMHP.S278394
Natto, Alshehri, Alghamdi, Infection Control Practices at the Dental Clinics in Jeddah, Saudi Arabia, J. Multidiscip. Healthc, doi:10.2147/JMDH.S330567
Natto, Bakhrebah, Afeef, Al-Harbi, Nassar et al., The short-term effect of different chlorhexidine forms versus povidone iodine mouth rinse in minimizing the oral SARS-CoV-2 viral load: An open label randomized controlled clinical trial study, Medicine, doi:10.1097/MD.0000000000028925
O'donnell, Thomas, Stanton, Maillard, Murphy et al., Potential Role of Oral Rinses Targeting the Viral Lipid Envelope in SARS-CoV-2 Infection, doi:10.1093/function/zqaa002
Ogun, Erinoso, Aina, Ojo, Adejumo et al., Efficacy of Hexetidine, Thymol and Hydrogen Peroxide-Containing Oral Antiseptics in Reducing SARS-CoV-2 Virus in the Oral Cavity: A Pilot Study, West Afr. J. Med, doi:10.55891/wajm.v39i1.98
Otten, Busscher, Van Der Mei, Abbas, Van Hoogmoed, Retention of antimicrobial activity in plaque and saliva following mouthrinse use in vivo, Caries Res, doi:10.1159/000320267
Ozduman, Oglakci, Dogan, Deger, Eliguzeloglu Dalkilic, How does antiseptic mouthwashes against SARS-COV-2 affect the bond strength of universal adhesive to enamel?, Microsc. Res. Tech, doi:10.1002/jemt.24028
Page, Mckenzie, Bossuyt, Boutron, Hoffmann et al., The PRISMA 2020 statement: An updated guideline for reporting systematic reviews, PLoS Med
Park, Li, Yu, Brinkman, Wong, Characterization of RNA in saliva, Clin. Chem, doi:10.1373/clinchem.2005.063206
Pelletier, Tessema, Frank, Westover, Brown et al., Efficacy of Povidone-Iodine Nasal and Oral Antiseptic Preparations Against Severe Acute Respiratory Syndrome-Coronavirus 2 (SARS-CoV-2), Ear Nose Throat J, doi:10.1177/0145561320957237
Peng, Xu, Li, Cheng, Zhou et al., Transmission routes of 2019-nCoV and controls in dental practice, Int. J. Oral Sci, doi:10.1038/s41368-020-0075-9
Poleti, Gregório, Bistaffa, Fernandes, Vilhena et al., Use of mouthwash and dentifrice containing an antimicrobial phthalocyanine derivative for the reduction of clinical symptoms of COVID-19: A randomized triple-blind clinical trial, J. Evid. Based Dent. Pract
Popkin, Zilka, Dimaano, Fujioka, Rackley et al., Cetylpyridinium Chloride (CPC) Exhibits Potent, Rapid Activity Against Influenza Viruses in vitro and in vivo, Pathog. Immun, doi:10.20411/pai.v2i2.200
Pullano, Di Domenico, Sabbatini, Valdano, Turbelin et al., Underdetection of cases of COVID-19 in France threatens epidemic control, Nature, doi:10.1038/s41586-020-03095-6
Radford, Beighton, Nugent, Jackson, Effect of use of 0.05% cetylpyridinium chloride mouthwash on normal oral flora, J. Dent, doi:10.1016/S0300-5712(95)00116-6
Redmond, Li, Ghaddara, Haq, Jones et al., A pilot randomized trial to evaluate the efficacy of oral and nasal povidone iodine in reducing the burden of severe acute respiratory syndrome coronavirus 2 RNA in patients with coronavirus disease, Infect. Control. Hosp. Epidemiol, doi:10.1017/ice.2022.257
Roberts, Addy, Comparison of the bisbiguanide antiseptics alexidine and chlorhexidine. I. Effect on plaque accumulation and salivary bacteria, J. Clin. Periodontol, doi:10.1111/j.1600-051X.1981.tb02032.x
Russell, Biocide use and antibiotic resistance: The relevance of laboratory findings to clinical and environmental situations, Lancet Infect. Dis, doi:10.1016/S1473-3099(03)00833-8
Sabino-Silva, Jardim, Siqueira, Coronavirus COVID-19 impacts to dentistry and potential salivary diagnosis, Clin. Oral Investig, doi:10.1007/s00784-020-03248-x
Saito, Adachi, Yamayoshi, Koga, Iwatsuki-Horimoto et al., Gargle Lavage as a Safe and Sensitive Alternative to Swab Samples to Diagnose COVID-19: A Case Report in Japan, Clin. Infect. Dis
Sanchez Barrueco, Mateos-Moreno, Martinez-Beneyto, Garcia-Vazquez, Campos Gonzalez et al., Effect of oral antiseptics in reducing SARS-CoV-2 infectivity: Evidence from a randomized double-blind clinical trial, Emerg. Microbes Infect, doi:10.1080/22221751.2022.2098059
Sanidad, Wang, Panigrahy, Zhang, Triclosan and triclocarban as potential risk factors of colitis and colon cancer: Roles of gut microbiota involved, Sci. Total Environ, doi:10.1016/j.scitotenv.2022.156776
Santos, Orcina, Machado, Vilhena, Alves et al., Beneficial effects of a mouthwash containing an antiviral phthalocyanine derivative on the length of hospital stay for COVID-19: Randomised trial, Sci. Rep, doi:10.1038/s41598-021-99013-5
Saraswathi, Chalageri, Bhushan, Ranganath, Rani et al., Impact of Steam Inhalation, Saline Gargling, and Povidone-Iodine Gargling on Clinical Outcome of COVID-19 Patients in Bengaluru, Karnataka: A Randomized Control Trial, Indian. J. Community Med, doi:10.4103/ijcm.ijcm_804_21
Saud, Tyrrell, Zaragkoulias, Protty, Statkute et al., The SARS-CoV2 envelope differs from host cells, exposes procoagulant lipids, and is disrupted in vivo by oral rinses, J. Lipid Res, doi:10.1016/j.jlr.2022.100208
Schiott, Löe, Jensen, Kilian, Davies et al., The effect of chlorhexidine mouthrinses on the human oral flora, J. Periodontal Res, doi:10.1111/j.1600-0765.1970.tb00697.x
Schutz, Conzelmann, Fois, Gross, Weil et al., Carrageenan-containing over-the-counter nasal and oral sprays inhibit SARS-CoV-2 infection of airway epithelial cultures, Am. J. Physiol. Lung Cell. Mol. Physiol, doi:10.1152/ajplung.00552.2020
Schürmann, Aljubeh, Tiemann, Sudhoff, Mouthrinses against SARS-CoV-2: Anti-inflammatory effectivity and a clinical pilot study, Eur. Arch. Oto-Rhino-Laryngol, doi:10.1007/s00405-021-06873-8
Seet, Quek, Ooi, Sengupta, Lakshminarasappa et al., Positive impact of oral hydroxychloroquine and povidone-iodine throat spray for COVID-19 prophylaxis: An open-label randomized trial, Int. J. Infect. Dis, doi:10.1016/j.ijid.2021.04.035
Seneviratne, Balan, Ko, Udawatte, Lai et al., Efficacy of commercial mouth-rinses on SARS-CoV-2 viral load in saliva: Randomized control trial in Singapore, Infection, doi:10.1007/s15010-020-01563-9
Sevinc Gul, Dilsiz, Saglik, Aydin, Effect of oral antiseptics on the viral load of SARS-CoV-2: A randomized controlled trial, Dent. Med. Probl, doi:10.17219/dmp/150831
Shankar, Saha, Jamir, Kakkar, Protection at Portal of Entry (PPE) with Povidone Iodine for COVID-19, Int. J. Med. Public Health, doi:10.5530/ijmedph.2020.4.36
Siami, Aghajanian, Mansouri, Mokhames, Pakzad et al., Effect of Ammonium Chloride in addition to standard of care in outpatients and hospitalized COVID-19 patients: A randomized clinical trial, Int. J. Infect. Dis, doi:10.1016/j.ijid.2021.04.043
Smeets, Pfefferle, Buttner, Knobloch, Lutgehetmann, Impact of Oral Rinsing with Octenidine Based Solution on SARS-CoV-2 Loads in Saliva of Infected Patients an Exploratory Study, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph19095582
Sreebny, Saliva in health and disease: An appraisal and update, Int. Dent. J, doi:10.1111/j.1875-595X.2000.tb00554.x
Steinhauer, Meister, Todt, Krawczyk, Passvogel et al., Comparison of the in-vitro efficacy of different mouthwash solutions targeting SARS-CoV-2 based on the European Standard EN 14476, J. Hosp. Infect, doi:10.1016/j.jhin.2021.01.031
Sterne, Savović, Page, Elbers, Blencowe et al., RoB 2: A revised tool for assessing risk of bias in randomised trials, BMJ, doi:10.1136/bmj.l4898
Supranoto, Slot, Addy, Van Der Weijden, The effect of chlorhexidine dentifrice or gel versus chlorhexidine mouthwash on plaque, gingivitis, bleeding and tooth discoloration: A systematic review, Int. J. Dent. Hyg
Suresh, Sharma, Aggarwal, Preanesthetic Povidone-Iodine gargles for patients with COVID-19, J. Clin. Anesth, doi:10.1016/j.jclinane.2020.110035
Tadakamadla, Boccalari, Rathore, Dolci, Tartaglia et al., In vitro studies evaluating the efficacy of mouth rinses on SARS-CoV-2: A systematic review, J. Infect. Public Health, doi:10.1016/j.jiph.2021.07.020
Tartaglia, Tadakamadla, Connelly, Sforza, Martín, Adverse events associated with home use of mouthrinses: A systematic review, Ther. Adv. Drug Saf, doi:10.1177/2042098619854881
Ting, Molinari, Suzuki, Current SARS-CoV-2 Protective Strategies for Healthcare Professionals, Biomedicines, doi:10.3390/biomedicines11030808
Ting, Suzuki, COVID-19: Current Overview on SARS-CoV-2 and the Dental Implications. Oral Health 2022
Ting, Suzuki, Is the COVID-19 Pandemic Over? The Current Status of Boosters, Immunosenescence, Long Haul COVID, and Systemic Complications, Int. J. Transl. Med, doi:10.3390/ijtm2020021
Ting, Suzuki, SARS-CoV-2: Overview and Its Impact on Oral Health. Biomedicines 2021, doi:10.3390/biomedicines9111690
Ting, Suzuki, The In Vitro Virucidal Effects of Mouthwashes on SARS-CoV-2, Int. J. Transl. Med
To, Tsang, Leung, Tam, Wu et al., Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: An observational cohort study, Lancet Infect. Dis, doi:10.1016/S1473-3099(20)30196-1
To, Tsang, Yip, Chan, Wu et al., Consistent Detection of 2019 Novel Coronavirus in Saliva, Clin. Infect. Dis, doi:10.1093/cid/ciaa149
Tomas, Cousido, Tomas, Limeres, Garcia-Caballero et al., In vivo bactericidal effect of 0.2% chlorhexidine but not 0.12% on salivary obligate anaerobes, Arch. Oral Biol, doi:10.1016/j.archoralbio.2008.07.009
Tomas, Garcia-Caballero, Lopez-Alvar, Suarez-Cunqueiro, Diz et al., In situ chlorhexidine substantivity on saliva and plaque-like biofilm: Influence of circadian rhythm, J. Periodontol, doi:10.1902/jop.2013.120475
Torres, Collins, Corbit, Ramirez, Winters et al., Comparison of saliva and nasopharyngeal swab SARS-CoV-2 RT-qPCR testing in a community setting, J. Infect, doi:10.1016/j.jinf.2020.11.015
Vitug, Santiaguel, Angelica Exconde, Ma Teresa Tricia, Oral Gargle of Ethanol-Based Mouthwash Solution and Its Effects on Adult Patients with Mild COVID-19 Infection: An Open Label-Randomized Controlled Trial
Wang, Wu, Wang, Zhu, Shi et al., Virucidal effect of povidone-iodine against SARS-CoV-2 in vitro, J. Int. Med. Res, doi:10.1177/03000605211063695
Wang, Xu, Gao, Lu, Han et al., Detection of SARS-CoV-2 in Different Types of Clinical Specimens, JAMA, doi:10.1001/jama.2020.3786
Warabi, Tobisawa, Kawazoe, Murayama, Norioka et al., Effects of oral care on prolonged viral shedding in coronavirus disease 2019 (COVID-19), Spec. Care Dent, doi:10.1111/scd.12498
Weber, Bonn, Auer, Kirschneck, Buchalla et al., Preprocedural mouthwashes for infection control in dentistry-an update, Clin. Oral Investig, doi:10.1007/s00784-023-04953-z
Wood, Payne, The action of three antiseptics/disinfectants against enveloped and non-enveloped viruses, J. Hosp. Infect, doi:10.1016/S0195-6701(98)90077-9
Wright, Tan, Walmsley, Hulme, O'connor et al., Protecting Frontline Health Care Workers from COVID-19 with Hydroxychloroquine Pre-exposure Prophylaxis: A structured summary of a study protocol for a randomised placebo-controlled multisite trial in Toronto, Canada. Trials, doi:10.1186/s13063-020-04577-8
Wyllie, Fournier, Casanovas-Massana, Campbell, Tokuyama et al., Saliva or Nasopharyngeal Swab Specimens for Detection of SARS-CoV-2, N. Engl. J. Med, doi:10.1056/NEJMc2016359
Wölfel, Corman, Guggemos, Seilmaier, Zange et al., Virological assessment of hospitalized patients with COVID-2019, Nature, doi:10.1038/s41586-020-2196-x
Xu, Li, Gan, Du, Yao et al., Potential Reservoirs for COVID-19 Asymptomatic Infection, J. Dent. Res, doi:10.1177/0022034520918518
Xu, Wang, Hoskin, Cugini, Markowitz et al., Differential Effects of Antiseptic Mouth Rinses on SARS-CoV-2 Infectivity In Vitro. Pathogens 2021, doi:10.3390/pathogens10030272
Yoon, Yoon, Song, Yoon, Lim et al., Clinical Significance of a High SARS-CoV-2 Viral Load in the Saliva, J. Korean Med. Sci, doi:10.3346/jkms.2020.35.e195
Zou, Ruan, Huang, Liang, Huang et al., SARS-CoV-2 Viral Load in Upper Respiratory Specimens of Infected Patients, N. Engl. J. Med, doi:10.1056/NEJMc2001737
DOI record:
{
"DOI": "10.3390/biomedicines11061694",
"ISSN": [
"2227-9059"
],
"URL": "http://dx.doi.org/10.3390/biomedicines11061694",
"abstract": "<jats:p>(1) There are limited clinical trials to support the effectiveness of mouth rinses when used as a preprocedural rinse against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This systematic review aims to evaluate the efficacy of antiseptic mouth rinses as a preprocedural rinse in reducing SARS-CoV-2 oral viral load in-vivo. (2) Methods: A literature search was conducted through November 2022 for the following databases: PubMed, Web of Science, Cochrane Library, and Google Scholar. The evaluated outcomes were quantitative changes in viral load and the statistical significance of that change after using antiseptic mouth rinses. (3) Results: 14 randomized controlled trials (RCT) were selected for risk of bias assessment and data extraction. (4) Conclusion: Within the limits of this systematic review, preprocedural mouth rinses may significantly reduce SARS-CoV-2 in the mouth, thus, reducing the viral particles available for airborne dispersion. Preprocedural mouth rinses may be an effective strategy for reducing airborne SARS-CoV-2 dispersion in the environment. Their use may be a preventive strategy to reduce the spread of COVID-19 in selected medical and healthcare facilities, including dental clinics. Potential preprocedural mouth rinses are identified for use as an integral part of safe practice for healthcare protocols. This systematic review was registered with the National Institute for Health Research, international prospective register of systematic reviews (PROSPERO): CRD42022315177.</jats:p>",
"alternative-id": [
"biomedicines11061694"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-8503-2279",
"affiliation": [
{
"name": "Department of Periodontics, University of Pennsylvania, Philadelphia, PA 19104, USA"
},
{
"name": "General Practice Residency, Albert Einstein Medical Center, Philadelphia, PA 19141, USA"
},
{
"name": "Think Dental Learning Institute, Paoli, PA 19301, USA"
}
],
"authenticated-orcid": false,
"family": "Ting",
"given": "Miriam",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0003-1009-244X",
"affiliation": [
{
"name": "General Practice Residency, Albert Einstein Medical Center, Philadelphia, PA 19141, USA"
}
],
"authenticated-orcid": false,
"family": "Dahlkemper",
"given": "Alex",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "General Practice Residency, Albert Einstein Medical Center, Philadelphia, PA 19141, USA"
}
],
"family": "Schwartz",
"given": "Jeremy J.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "General Practice Residency, Albert Einstein Medical Center, Philadelphia, PA 19141, USA"
}
],
"family": "Woodfork",
"given": "Manzel",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3348-8893",
"affiliation": [
{
"name": "Department of Graduate Periodontics, University of Maryland, Baltimore, MD 21201, USA"
},
{
"name": "Department of Graduate Prosthodontics, University of Washington, Seattle, WA 98015, USA"
},
{
"name": "Department of Graduate Periodontics, Nova Southeastern University, Ft. Lauderdale, FL 33314, USA"
}
],
"authenticated-orcid": false,
"family": "Suzuki",
"given": "Jon B.",
"sequence": "additional"
}
],
"container-title": "Biomedicines",
"container-title-short": "Biomedicines",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
6,
13
]
],
"date-time": "2023-06-13T05:35:30Z",
"timestamp": 1686634530000
},
"deposited": {
"date-parts": [
[
2023,
6,
13
]
],
"date-time": "2023-06-13T09:03:37Z",
"timestamp": 1686647017000
},
"indexed": {
"date-parts": [
[
2023,
6,
14
]
],
"date-time": "2023-06-14T04:20:28Z",
"timestamp": 1686716428194
},
"is-referenced-by-count": 0,
"issue": "6",
"issued": {
"date-parts": [
[
2023,
6,
12
]
]
},
"journal-issue": {
"issue": "6",
"published-online": {
"date-parts": [
[
2023,
6
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
6,
12
]
],
"date-time": "2023-06-12T00:00:00Z",
"timestamp": 1686528000000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2227-9059/11/6/1694/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1694",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
6,
12
]
]
},
"published-online": {
"date-parts": [
[
2023,
6,
12
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1056/NEJMc2009324",
"article-title": "Droplets and Aerosols in the Transmission of SARS-CoV-2",
"author": "Meselson",
"doi-asserted-by": "crossref",
"first-page": "2063",
"journal-title": "N. Engl. J. Med.",
"key": "ref_1",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1056/NEJMc2001737",
"article-title": "SARS-CoV-2 Viral Load in Upper Respiratory Specimens of Infected Patients",
"author": "Zou",
"doi-asserted-by": "crossref",
"first-page": "1177",
"journal-title": "N. Engl. J. Med.",
"key": "ref_2",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.3390/biomedicines9111690",
"doi-asserted-by": "crossref",
"key": "ref_3",
"unstructured": "Ting, M., and Suzuki, J.B. (2021). SARS-CoV-2: Overview and Its Impact on Oral Health. Biomedicines, 9."
},
{
"key": "ref_4",
"unstructured": "Ting, M., and Suzuki, J.B. (2022). COVID-19: Current Overview on SARS-CoV-2 and the Dental Implications. Oral Health, Available online: https://www.oralhealthgroup.com/features/covid-19-current-overview-on-sars-cov-2-and-the-dental-implications/."
},
{
"DOI": "10.3390/biomedicines11030808",
"doi-asserted-by": "crossref",
"key": "ref_5",
"unstructured": "Ting, M., Molinari, J.A., and Suzuki, J.B. (2023). Current SARS-CoV-2 Protective Strategies for Healthcare Professionals. Biomedicines, 11."
},
{
"article-title": "Is the COVID-19 Pandemic Over? The Current Status of Boosters, Immunosenescence, Long Haul COVID, and Systemic Complications",
"author": "Ting",
"first-page": "230",
"journal-title": "Int. J. Transl. Med.",
"key": "ref_6",
"volume": "2",
"year": "2022"
},
{
"DOI": "10.7326/M20-6206",
"article-title": "SARS-CoV-2 Vaccine Acceptance: We May Need to Choose Our Battles",
"author": "Buttenheim",
"doi-asserted-by": "crossref",
"first-page": "1018",
"journal-title": "Ann. Intern. Med.",
"key": "ref_7",
"volume": "173",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciaa149",
"article-title": "Consistent Detection of 2019 Novel Coronavirus in Saliva",
"author": "To",
"doi-asserted-by": "crossref",
"first-page": "841",
"journal-title": "Clin. Infect. Dis.",
"key": "ref_8",
"volume": "71",
"year": "2020"
},
{
"DOI": "10.1016/S1473-3099(20)30196-1",
"article-title": "Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: An observational cohort study",
"author": "To",
"doi-asserted-by": "crossref",
"first-page": "565",
"journal-title": "Lancet Infect. Dis.",
"key": "ref_9",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.3390/ijerph181910059",
"doi-asserted-by": "crossref",
"key": "ref_10",
"unstructured": "Deana, N.F., Seiffert, A., Aravena-Rivas, Y., Alonso-Coello, P., Munoz-Millan, P., Espinoza-Espinoza, G., Pineda, P., and Zaror, C. (2021). Recommendations for Safe Dental Care: A Systematic Review of Clinical Practice Guidelines in the First Year of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health, 18."
},
{
"DOI": "10.1177/0022034520918518",
"article-title": "Salivary Glands: Potential Reservoirs for COVID-19 Asymptomatic Infection",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "989",
"journal-title": "J. Dent. Res.",
"key": "ref_11",
"volume": "99",
"year": "2020"
},
{
"DOI": "10.1177/00220345221102310",
"article-title": "Cetylpyridinium Chloride Mouthwash to Reduce Shedding of Infectious SARS-CoV-2: A Double-Blind Randomized Clinical Trial",
"author": "Alemany",
"doi-asserted-by": "crossref",
"first-page": "1450",
"journal-title": "J. Dent. Res.",
"key": "ref_12",
"volume": "101",
"year": "2022"
},
{
"DOI": "10.3390/ijerph19148768",
"doi-asserted-by": "crossref",
"key": "ref_13",
"unstructured": "Guerrero Bernal, C.G., Reyes Uribe, E., Salazar Flores, J., Varela Hernández, J.J., Gómez-Sandoval, J.R., Martínez Salazar, S.Y., Gutiérrez Maldonado, A.F., Aguilar Martínez, J., and Lomelí Martínez, S.M. (2022). Oral Antiseptics against SARS-CoV-2: A Literature Review. Int. J. Environ. Res. Public Health, 19."
},
{
"DOI": "10.4103/jispcd.JISPCD_65_22",
"article-title": "Evaluation of Current Evidence on the Use of Oral Antiseptics Against SARS-CoV-2: A Narrative Review",
"doi-asserted-by": "crossref",
"first-page": "488",
"journal-title": "J. Int. Soc. Prev. Community Dent.",
"key": "ref_14",
"volume": "12",
"year": "2022"
},
{
"article-title": "Preprocedural mouthwashes for infection control in dentistry-an update",
"author": "Weber",
"first-page": "2",
"journal-title": "Clin. Oral Investig.",
"key": "ref_15",
"volume": "20",
"year": "2023"
},
{
"DOI": "10.1007/s00784-020-03248-x",
"article-title": "Coronavirus COVID-19 impacts to dentistry and potential salivary diagnosis",
"author": "Jardim",
"doi-asserted-by": "crossref",
"first-page": "1619",
"journal-title": "Clin. Oral Investig.",
"key": "ref_16",
"volume": "24",
"year": "2020"
},
{
"article-title": "Cetylpyridinium Chloride (CPC) Exhibits Potent, Rapid Activity Against Influenza Viruses in vitro and in vivo",
"author": "Popkin",
"first-page": "252",
"journal-title": "Pathog. Immun.",
"key": "ref_17",
"volume": "2",
"year": "2017"
},
{
"DOI": "10.1159/000089211",
"article-title": "Inactivation of SARS coronavirus by means of povidone-iodine, physical conditions and chemical reagents",
"author": "Kariwa",
"doi-asserted-by": "crossref",
"first-page": "119",
"journal-title": "Dermatology",
"key": "ref_18",
"volume": "212",
"year": "2006"
},
{
"DOI": "10.1002/jmv.26514",
"article-title": "Lowering the transmission and spread of human coronavirus",
"author": "Meyers",
"doi-asserted-by": "crossref",
"first-page": "1605",
"journal-title": "J. Med. Virol.",
"key": "ref_19",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1016/j.jhin.2021.01.031",
"article-title": "Comparison of the in-vitro efficacy of different mouthwash solutions targeting SARS-CoV-2 based on the European Standard EN 14476",
"author": "Steinhauer",
"doi-asserted-by": "crossref",
"first-page": "180",
"journal-title": "J. Hosp. Infect.",
"key": "ref_20",
"volume": "111",
"year": "2021"
},
{
"DOI": "10.1016/S0195-6701(98)90077-9",
"article-title": "The action of three antiseptics/disinfectants against enveloped and non-enveloped viruses",
"author": "Wood",
"doi-asserted-by": "crossref",
"first-page": "283",
"journal-title": "J. Hosp. Infect.",
"key": "ref_21",
"volume": "38",
"year": "1998"
},
{
"DOI": "10.1007/s40121-018-0200-7",
"article-title": "In Vitro Bactericidal and Virucidal Efficacy of Povidone-Iodine Gargle/Mouthwash Against Respiratory and Oral Tract Pathogens",
"author": "Eggers",
"doi-asserted-by": "crossref",
"first-page": "249",
"journal-title": "Infect. Dis. Ther.",
"key": "ref_22",
"volume": "7",
"year": "2018"
},
{
"DOI": "10.1177/00220345211029269",
"article-title": "Mouthwashes with CPC Reduce the Infectivity of SARS-CoV-2 Variants In Vitro",
"author": "Leon",
"doi-asserted-by": "crossref",
"first-page": "1265",
"journal-title": "J. Dent. Res.",
"key": "ref_23",
"volume": "100",
"year": "2021"
},
{
"DOI": "10.1016/j.jhin.2020.01.022",
"article-title": "Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents",
"author": "Kampf",
"doi-asserted-by": "crossref",
"first-page": "246",
"journal-title": "J. Hosp. Infect.",
"key": "ref_24",
"volume": "104",
"year": "2020"
},
{
"DOI": "10.1093/infdis/jiaa471",
"article-title": "Virucidal Efficacy of Different Oral Rinses Against Severe Acute Respiratory Syndrome Coronavirus 2",
"author": "Meister",
"doi-asserted-by": "crossref",
"first-page": "1289",
"journal-title": "J. Infect. Dis.",
"key": "ref_25",
"volume": "222",
"year": "2020"
},
{
"DOI": "10.1007/s40121-020-00316-3",
"article-title": "Povidone-Iodine Demonstrates Rapid In Vitro Virucidal Activity Against SARS-CoV-2, The Virus Causing COVID-19 Disease",
"author": "Anderson",
"doi-asserted-by": "crossref",
"first-page": "669",
"journal-title": "Infect. Dis. Ther.",
"key": "ref_26",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1038/s41368-020-0075-9",
"article-title": "Transmission routes of 2019-nCoV and controls in dental practice",
"author": "Peng",
"doi-asserted-by": "crossref",
"first-page": "9",
"journal-title": "Int. J. Oral Sci.",
"key": "ref_27",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1002/hed.26164",
"article-title": "COVID-19 pandemic: Effects and evidence-based recommendations for otolaryngology and head and neck surgery practice",
"author": "Kowalski",
"doi-asserted-by": "crossref",
"first-page": "1259",
"journal-title": "Head Neck",
"key": "ref_28",
"volume": "42",
"year": "2020"
},
{
"DOI": "10.31222/osf.io/v7gm2",
"doi-asserted-by": "crossref",
"key": "ref_29",
"unstructured": "Page, M.J., McKenzie, J.E., Bossuyt, P.M., Boutron, I., Hoffmann, T.C., Mulrow, C.D., Shamseer, L., Tetzlaff, J.M., Akl, E.A., and Brennan, S.E. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. PLoS Med., 88."
},
{
"DOI": "10.1136/bmj.l4898",
"article-title": "RoB 2: A revised tool for assessing risk of bias in randomised trials",
"author": "Sterne",
"doi-asserted-by": "crossref",
"first-page": "l4898",
"journal-title": "BMJ",
"key": "ref_30",
"volume": "366",
"year": "2019"
},
{
"DOI": "10.1080/22221751.2022.2098059",
"article-title": "Effect of oral antiseptics in reducing SARS-CoV-2 infectivity: Evidence from a randomized double-blind clinical trial",
"author": "Rueda",
"doi-asserted-by": "crossref",
"first-page": "1833",
"journal-title": "Emerg. Microbes Infect.",
"key": "ref_31",
"volume": "11",
"year": "2022"
},
{
"article-title": "Use of an antiviral mouthwash as a barrier measure in the SARS-CoV-2 transmission in adults with asymptomatic to mild COVID-19: A multicentre, randomized, double-blind controlled trial",
"author": "Carrouel",
"first-page": "1494",
"journal-title": "Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis.",
"key": "ref_32",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1016/j.adaj.2021.05.021",
"article-title": "Estimating salivary carriage of severe acute respiratory syndrome coronavirus 2 in nonsymptomatic people and efficacy of mouthrinse in reducing viral load: A randomized controlled trial",
"author": "Chaudhary",
"doi-asserted-by": "crossref",
"first-page": "903",
"journal-title": "J. Am. Dent. Assoc.",
"key": "ref_33",
"volume": "152",
"year": "2021"
},
{
"DOI": "10.1111/odi.14086",
"article-title": "Chlorhexidine mouthwash reduces the salivary viral load of SARS-CoV-2: A randomized clinical trial",
"author": "Costa",
"doi-asserted-by": "crossref",
"first-page": "2500",
"journal-title": "Oral Dis.",
"key": "ref_34",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1016/j.heliyon.2021.e07346",
"article-title": "Salivary SARS-CoV-2 load reduction with mouthwash use: A randomized pilot clinical trial",
"author": "Eduardo",
"doi-asserted-by": "crossref",
"first-page": "e07346",
"journal-title": "Heliyon",
"key": "ref_35",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1016/j.jebdp.2021.101584",
"article-title": "In vivo evaluation of the virucidal efficacy of chlorhexidine and povidone-iodine mouthwashes against salivary SARS-CoV-2. A randomized-controlled clinical trial",
"author": "Elzein",
"doi-asserted-by": "crossref",
"first-page": "101584",
"journal-title": "J. Evid. Based Dent. Pract.",
"key": "ref_36",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1016/j.amjoto.2022.103549",
"article-title": "Efficacy of antiseptic mouthrinses against SARS-CoV-2: A prospective randomized placebo-controlled pilot study",
"author": "Fantozzi",
"doi-asserted-by": "crossref",
"first-page": "103549",
"journal-title": "Am. J. Otolaryngol.",
"key": "ref_37",
"volume": "43",
"year": "2022"
},
{
"DOI": "10.1038/s41598-021-03461-y",
"article-title": "Clinical evaluation of antiseptic mouth rinses to reduce salivary load of SARS-CoV-2",
"author": "Ferrer",
"doi-asserted-by": "crossref",
"first-page": "24392",
"journal-title": "Sci. Rep.",
"key": "ref_38",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.17219/dmp/150831",
"article-title": "Effect of oral antiseptics on the viral load of SARS-CoV-2: A randomized controlled trial",
"author": "Dilsiz",
"doi-asserted-by": "crossref",
"first-page": "357",
"journal-title": "Dent. Med. Probl.",
"key": "ref_39",
"volume": "59",
"year": "2022"
},
{
"DOI": "10.1016/j.virusres.2022.198791",
"article-title": "Mouthrinses against SARS-CoV-2—High antiviral effectivity by membrane disruption in vitro translates to mild effects in a randomized placebo-controlled clinical trial",
"author": "Meister",
"doi-asserted-by": "crossref",
"first-page": "198791",
"journal-title": "Virus Res.",
"key": "ref_40",
"volume": "316",
"year": "2022"
},
{
"DOI": "10.1097/MD.0000000000028925",
"article-title": "The short-term effect of different chlorhexidine forms versus povidone iodine mouth rinse in minimizing the oral SARS-CoV-2 viral load: An open label randomized controlled clinical trial study",
"author": "Natto",
"doi-asserted-by": "crossref",
"first-page": "e28925",
"journal-title": "Medicine",
"key": "ref_41",
"volume": "101",
"year": "2022"
},
{
"DOI": "10.1017/ice.2022.257",
"article-title": "A pilot randomized trial to evaluate the efficacy of oral and nasal povidone iodine in reducing the burden of severe acute respiratory syndrome coronavirus 2 RNA in patients with coronavirus disease 2019",
"author": "Redmond",
"doi-asserted-by": "crossref",
"first-page": "679",
"journal-title": "Infect. Control. Hosp. Epidemiol.",
"key": "ref_42",
"volume": "44",
"year": "2023"
},
{
"DOI": "10.1007/s15010-020-01563-9",
"article-title": "Efficacy of commercial mouth-rinses on SARS-CoV-2 viral load in saliva: Randomized control trial in Singapore",
"author": "Seneviratne",
"doi-asserted-by": "crossref",
"first-page": "305",
"journal-title": "Infection",
"key": "ref_43",
"volume": "49",
"year": "2021"
},
{
"DOI": "10.1111/odi.13526",
"article-title": "Is povidone iodine mouthwash effective against SARS-CoV-2? First in vivo tests",
"author": "Feijoo",
"doi-asserted-by": "crossref",
"first-page": "908",
"journal-title": "Oral Dis.",
"key": "ref_44",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.3390/ijerph19095582",
"doi-asserted-by": "crossref",
"key": "ref_45",
"unstructured": "Smeets, R., Pfefferle, S., Buttner, H., Knobloch, J.K., and Lutgehetmann, M. (2022). Impact of Oral Rinsing with Octenidine Based Solution on SARS-CoV-2 Loads in Saliva of Infected Patients an Exploratory Study. Int. J. Environ. Res. Public Health, 19."
},
{
"DOI": "10.1007/s10096-021-04320-4",
"article-title": "The role of mouthwash sampling in SARS-CoV-2 diagnosis",
"author": "Biber",
"doi-asserted-by": "crossref",
"first-page": "2199",
"journal-title": "Eur. J. Clin. Microbiol. Infect. Dis.",
"key": "ref_46",
"volume": "40",
"year": "2021"
},
{
"article-title": "In vivo (human) and in vitro inactivation of SARS-CoV-2 with 0.5% povidone-iodine nasal spray",
"author": "Friedland",
"first-page": "5",
"journal-title": "Aust. J. Otolaryngol.",
"key": "ref_47",
"volume": "2022",
"year": "2022"
},
{
"DOI": "10.1016/j.jlr.2022.100208",
"article-title": "The SARS-CoV2 envelope differs from host cells, exposes procoagulant lipids, and is disrupted in vivo by oral rinses",
"author": "Saud",
"doi-asserted-by": "crossref",
"first-page": "100208",
"journal-title": "J. Lipid Res.",
"key": "ref_48",
"volume": "63",
"year": "2022"
},
{
"DOI": "10.1007/s00405-021-06873-8",
"article-title": "Mouthrinses against SARS-CoV-2: Anti-inflammatory effectivity and a clinical pilot study",
"author": "Aljubeh",
"doi-asserted-by": "crossref",
"first-page": "5059",
"journal-title": "Eur. Arch. Oto-Rhino-Laryngol.",
"key": "ref_49",
"volume": "278",
"year": "2021"
},
{
"DOI": "10.1002/jemt.24028",
"article-title": "How does antiseptic mouthwashes against SARS-COV-2 affect the bond strength of universal adhesive to enamel?",
"author": "Ozduman",
"doi-asserted-by": "crossref",
"first-page": "1199",
"journal-title": "Microsc. Res. Tech.",
"key": "ref_50",
"volume": "85",
"year": "2022"
},
{
"article-title": "Comparison of Effectiveness of Chlorine Dioxide Mouthwash and Chlorhexidine Gluconate Mouthwash in Reduction of Oral Viral Load in Patients with COVID-19",
"author": "Avhad",
"first-page": "27",
"journal-title": "Indian J. Public Health Res. Dev.",
"key": "ref_51",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.23736/S0026-4806.20.06688-4",
"article-title": "Thrombo-prophylaxis prevents thrombotic events in home-managed COVID patients. A registry study",
"author": "Belcaro",
"doi-asserted-by": "crossref",
"first-page": "366",
"journal-title": "Minerva Med.",
"key": "ref_52",
"volume": "111",
"year": "2020"
},
{
"DOI": "10.4178/epih.e2021032",
"article-title": "Effectiveness of hydrogen peroxide as auxiliary treatment for hospitalized COVID-19 patients in Brazil: Preliminary results of a randomized double-blind clinical trial",
"author": "Cesca",
"doi-asserted-by": "crossref",
"first-page": "e2021032",
"journal-title": "Epidemiol. Health",
"key": "ref_53",
"volume": "43",
"year": "2021"
},
{
"DOI": "10.4178/epih.e2021051",
"article-title": "Hydrogen peroxide as an auxiliary treatment for COVID-19 in Brazil: A randomized double-blind clinical trial",
"author": "Collares",
"doi-asserted-by": "crossref",
"first-page": "e2021051",
"journal-title": "Epidemiol. Health",
"key": "ref_54",
"volume": "43",
"year": "2021"
},
{
"DOI": "10.1002/jmv.26954",
"article-title": "Use of chlorhexidine to eradicate oropharyngeal SARS-CoV-2 in COVID-19 patients",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "4370",
"journal-title": "J. Med. Virol.",
"key": "ref_55",
"volume": "93",
"year": "2021"
},
{
"article-title": "Early viral clearance among COVID-19 patients when gargling with povidone-iodine and essential oils—A clinical trial",
"author": "Mohamed",
"first-page": "20180448",
"journal-title": "medRxiv",
"key": "ref_56",
"volume": "2020",
"year": "2020"
},
{
"article-title": "A randomized trial on the regular use of potent mouthwash in COVID-19 treatment",
"author": "Mukhtar",
"first-page": "20234997",
"journal-title": "MedRxiv",
"key": "ref_57",
"volume": "2020",
"year": "2021"
},
{
"DOI": "10.55891/wajm.v39i1.98",
"article-title": "Efficacy of Hexetidine, Thymol and Hydrogen Peroxide-Containing Oral Antiseptics in Reducing SARS-CoV-2 Virus in the Oral Cavity: A Pilot Study",
"author": "Ogun",
"doi-asserted-by": "crossref",
"first-page": "83",
"journal-title": "West Afr. J. Med.",
"key": "ref_58",
"volume": "39",
"year": "2022"
},
{
"DOI": "10.1016/j.jebdp.2022.101777",
"article-title": "Use of mouthwash and dentifrice containing an antimicrobial phthalocyanine derivative for the reduction of clinical symptoms of COVID-19: A randomized triple-blind clinical trial",
"author": "Poleti",
"doi-asserted-by": "crossref",
"first-page": "101777",
"journal-title": "J. Evid. Based Dent. Pract.",
"key": "ref_59",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.1101/2021.05.20.21256197",
"doi-asserted-by": "crossref",
"key": "ref_60",
"unstructured": "Almanza-Reyes, H., Moreno, S., Plascencia-López, I., Alvarado-Vera, M., Patrón-Romero, L., Borrego, B., Reyes-Escamilla, A., Valencia-Manzo, D., Brun, A., and Pestryakov, A. (2021). Evaluation of silver nanoparticles for the prevention of SARS-CoV-2 infection in health workers: In vitro and in vivo. PLoS ONE, 16."
},
{
"DOI": "10.1016/j.chest.2021.08.014",
"article-title": "Oral Gargle of Ethanol-Based Mouthwash Solution and Its Effects on Adult Patients with Mild COVID-19 Infection: An Open Label-Randomized Controlled Trial",
"author": "Santiaguel",
"doi-asserted-by": "crossref",
"first-page": "A2504",
"journal-title": "Chest",
"key": "ref_61",
"volume": "160",
"year": "2021"
},
{
"DOI": "10.1038/s41598-021-99013-5",
"article-title": "Beneficial effects of a mouthwash containing an antiviral phthalocyanine derivative on the length of hospital stay for COVID-19: Randomised trial",
"author": "Santos",
"doi-asserted-by": "crossref",
"first-page": "19937",
"journal-title": "Sci. Rep.",
"key": "ref_62",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.5530/ijmedph.2020.4.36",
"article-title": "Protection at Portal of Entry (PPE) with Povidone Iodine for COVID-19",
"author": "Shankar",
"doi-asserted-by": "crossref",
"first-page": "166",
"journal-title": "Int. J. Med. Public Health",
"key": "ref_63",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1111/scd.12498",
"article-title": "Effects of oral care on prolonged viral shedding in coronavirus disease 2019 (COVID-19)",
"author": "Warabi",
"doi-asserted-by": "crossref",
"first-page": "470",
"journal-title": "Spec. Care Dent.",
"key": "ref_64",
"volume": "40",
"year": "2020"
},
{
"DOI": "10.4103/ijcm.ijcm_804_21",
"article-title": "Impact of Steam Inhalation, Saline Gargling, and Povidone-Iodine Gargling on Clinical Outcome of COVID-19 Patients in Bengaluru, Karnataka: A Randomized Control Trial",
"author": "Saraswathi",
"doi-asserted-by": "crossref",
"first-page": "207",
"journal-title": "Indian. J. Community Med.",
"key": "ref_65",
"volume": "47",
"year": "2022"
},
{
"DOI": "10.3329/brc.v7i1.54245",
"article-title": "Effect of 1% Povidone Iodine Mouthwash/Gargle, Nasal and Eye Drop in COVID-19 patient",
"author": "Shabnam",
"doi-asserted-by": "crossref",
"first-page": "919",
"journal-title": "Bioresearch Commun.",
"key": "ref_66",
"volume": "7",
"year": "2021"
},
{
"article-title": "Population-based virucidal phthalocyanine gargling/rinsing protocol to reduce the risk of coronavirus disease-2019: A community trial",
"author": "Vilhena",
"first-page": "Doc23",
"journal-title": "GMS Hyg. Infect. Control",
"key": "ref_67",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.1001/jamaoto.2020.5490",
"article-title": "Povidone Iodine Mouthwash, Gargle, and Nasal Spray to Reduce Nasopharyngeal Viral Load in Patients with COVID-19: A Randomized Clinical Trial",
"author": "Guenezan",
"doi-asserted-by": "crossref",
"first-page": "400",
"journal-title": "JAMA Otolaryngol. Head Neck Surg.",
"key": "ref_68",
"volume": "147",
"year": "2021"
},
{
"DOI": "10.1186/s13063-021-05181-0",
"article-title": "Reconvalescent plasma/camostat mesylate in early SARS-CoV-2 Q-PCR positive high-risk individuals (RES-Q-HR): A structured summary of a study protocol for a randomized controlled trial",
"author": "Keitel",
"doi-asserted-by": "crossref",
"first-page": "343",
"journal-title": "Trials",
"key": "ref_69",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1016/j.amjoto.2020.102618",
"article-title": "Repurposing 0.5% povidone iodine solution in otorhinolaryngology practice in COVID-19 pandemic",
"author": "Khan",
"doi-asserted-by": "crossref",
"first-page": "102618",
"journal-title": "Am. J. Otolaryngol.",
"key": "ref_70",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.1007/s12070-021-02616-7",
"article-title": "Virucidal effect of povidone iodine on COVID-19 in the nasopharynx: An open-label randomized clinical trial",
"author": "Arefin",
"doi-asserted-by": "crossref",
"first-page": "2963",
"journal-title": "Indian J. Otolaryngol. Head Neck Surg. Off. Publ. Assoc. Otolaryngol. India",
"key": "ref_71",
"volume": "74",
"year": "2022"
},
{
"DOI": "10.1186/s12879-016-2177-8",
"doi-asserted-by": "crossref",
"key": "ref_72",
"unstructured": "Mukherjee, P.K., Esper, F., Buchheit, K., Arters, K., Adkins, I., Ghannoum, M.A., and Salata, R.A. (2017). Randomized, double-blind, placebo-controlled clinical trial to assess the safety and effectiveness of a novel dual-action oral topical formulation against upper respiratory infections. BMC Infect. Dis., 17."
},
{
"DOI": "10.1016/j.ijid.2021.04.035",
"article-title": "Positive impact of oral hydroxychloroquine and povidone-iodine throat spray for COVID-19 prophylaxis: An open-label randomized trial",
"author": "Seet",
"doi-asserted-by": "crossref",
"first-page": "314",
"journal-title": "Int. J. Infect. Dis.",
"key": "ref_73",
"volume": "106",
"year": "2021"
},
{
"DOI": "10.1016/j.ijid.2021.04.043",
"article-title": "Effect of Ammonium Chloride in addition to standard of care in outpatients and hospitalized COVID-19 patients: A randomized clinical trial",
"author": "Siami",
"doi-asserted-by": "crossref",
"first-page": "306",
"journal-title": "Int. J. Infect. Dis.",
"key": "ref_74",
"volume": "108",
"year": "2021"
},
{
"DOI": "10.1186/s13063-020-04577-8",
"article-title": "Protecting Frontline Health Care Workers from COVID-19 with Hydroxychloroquine Pre-exposure Prophylaxis: A structured summary of a study protocol for a randomised placebo-controlled multisite trial in Toronto, Canada",
"author": "Wright",
"doi-asserted-by": "crossref",
"first-page": "647",
"journal-title": "Trials",
"key": "ref_75",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1186/s13063-020-04963-2",
"article-title": "Virucidal effect of povidone iodine on COVID-19 in the nasopharynx: A structured summary of a study protocol for an open-label randomized clinical trial",
"author": "Hasan",
"doi-asserted-by": "crossref",
"first-page": "2",
"journal-title": "Trials",
"key": "ref_76",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1186/s13063-020-04634-2",
"article-title": "A quadruple blind, randomised controlled trial of gargling agents in reducing intraoral viral load among hospitalised COVID-19 patients: A structured summary of a study protocol for a randomised controlled trial",
"author": "Khan",
"doi-asserted-by": "crossref",
"first-page": "785",
"journal-title": "Trials",
"key": "ref_77",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1177/0022034520943574",
"article-title": "Interventions to Reduce Aerosolized Microbes in Dental Practice: A Systematic Review with Network Meta-analysis of Randomized Controlled Trials",
"author": "Koletsi",
"doi-asserted-by": "crossref",
"first-page": "1228",
"journal-title": "J. Dent. Res.",
"key": "ref_78",
"volume": "99",
"year": "2020"
},
{
"DOI": "10.1007/s40121-019-00260-x",
"article-title": "Infectious Disease Management and Control with Povidone Iodine",
"author": "Eggers",
"doi-asserted-by": "crossref",
"first-page": "581",
"journal-title": "Infect. Dis. Ther.",
"key": "ref_79",
"volume": "8",
"year": "2019"
},
{
"DOI": "10.1038/s41564-020-0695-z",
"article-title": "The species Severe acute respiratory syndrome-related coronavirus: Classifying 2019-nCoV and naming it SARS-CoV-2",
"author": "Gorbalenya",
"doi-asserted-by": "crossref",
"first-page": "536",
"journal-title": "Nat. Microbiol.",
"key": "ref_80",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1093/function/zqaa002",
"article-title": "Potential Role of Oral Rinses Targeting the Viral Lipid Envelope in SARS-CoV-2 Infection",
"author": "Thomas",
"doi-asserted-by": "crossref",
"first-page": "zqaa002",
"journal-title": "Function",
"key": "ref_81",
"volume": "1",
"year": "2020"
},
{
"DOI": "10.1111/j.1875-595X.2000.tb00554.x",
"article-title": "Saliva in health and disease: An appraisal and update",
"author": "Sreebny",
"doi-asserted-by": "crossref",
"first-page": "140",
"journal-title": "Int. Dent. J.",
"key": "ref_82",
"volume": "50",
"year": "2000"
},
{
"DOI": "10.1016/j.jclinane.2020.110035",
"article-title": "Preanesthetic Povidone-Iodine gargles for patients with COVID-19",
"author": "Suresh",
"doi-asserted-by": "crossref",
"first-page": "110035",
"journal-title": "J. Clin. Anesth.",
"key": "ref_83",
"volume": "67",
"year": "2020"
},
{
"DOI": "10.3390/ijerph19052877",
"doi-asserted-by": "crossref",
"key": "ref_84",
"unstructured": "Garcia-Sanchez, A., Peña-Cardelles, J.F., Ordonez-Fernandez, E., Montero-Alonso, M., Kewalramani, N., Salgado-Peralvo, A.O., Végh, D., Gargano, A., Parra, G., and Guerra-Guajardo, L.I. (2022). Povidone-Iodine as a Pre-Procedural Mouthwash to Reduce the Salivary Viral Load of SARS-CoV-2: A Systematic Review of Randomized Controlled Trials. Int. J. Environ. Res. Public Health, 19."
},
{
"DOI": "10.1111/jopr.13209",
"article-title": "Rapid In-Vitro Inactivation of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Using Povidone-Iodine Oral Antiseptic Rinse",
"author": "Bidra",
"doi-asserted-by": "crossref",
"first-page": "529",
"journal-title": "J. Prosthodont.",
"key": "ref_85",
"volume": "29",
"year": "2020"
},
{
"DOI": "10.1038/s41415-020-1589-4",
"article-title": "Povidone iodine",
"author": "Challacombe",
"doi-asserted-by": "crossref",
"first-page": "656",
"journal-title": "Br. Dent. J.",
"key": "ref_86",
"volume": "228",
"year": "2020"
},
{
"article-title": "A contemporary look at COVID-19 medications: Available and potentially effective drugs",
"author": "Alshaeri",
"first-page": "9188",
"journal-title": "Eur. Rev. Med. Pharmacol. Sci.",
"key": "ref_87",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.2147/RMHP.S278394",
"article-title": "Characteristics of First Cases of Coronavirus Disease 2019 and the Effort to Prevent the Early Spread of COVID-19 in Saudi Arabia",
"author": "Natto",
"doi-asserted-by": "crossref",
"first-page": "315",
"journal-title": "Risk Manag. Healthc. Policy",
"key": "ref_88",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.2147/JMDH.S330567",
"article-title": "Infection Control Practices at the Dental Clinics in Jeddah, Saudi Arabia",
"author": "Natto",
"doi-asserted-by": "crossref",
"first-page": "2951",
"journal-title": "J. Multidiscip. Healthc.",
"key": "ref_89",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1126/science.abd0826",
"article-title": "Structure-based design of prefusion-stabilized SARS-CoV-2 spikes",
"author": "Hsieh",
"doi-asserted-by": "crossref",
"first-page": "1501",
"journal-title": "Science",
"key": "ref_90",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1111/j.1600-051X.1981.tb02032.x",
"article-title": "Comparison of the bisbiguanide antiseptics alexidine and chlorhexidine. I. Effect on plaque accumulation and salivary bacteria",
"author": "Roberts",
"doi-asserted-by": "crossref",
"first-page": "213",
"journal-title": "J. Clin. Periodontol.",
"key": "ref_91",
"volume": "8",
"year": "1981"
},
{
"DOI": "10.1902/jop.1996.67.6.572",
"article-title": "The substantivity of a number of oral hygiene products determined by the duration of effects on salivary bacteria",
"author": "Elworthy",
"doi-asserted-by": "crossref",
"first-page": "572",
"journal-title": "J. Periodontol.",
"key": "ref_92",
"volume": "67",
"year": "1996"
},
{
"DOI": "10.1099/jmm.0.001508",
"article-title": "CPC-containing oral rinses inactivate SARS-CoV-2 variants and are active in the presence of human saliva",
"author": "Anderson",
"doi-asserted-by": "crossref",
"first-page": "001508",
"journal-title": "J. Med. Microbiol.",
"key": "ref_93",
"volume": "71",
"year": "2022"
},
{
"DOI": "10.1016/j.scitotenv.2022.156776",
"article-title": "Triclosan and triclocarban as potential risk factors of colitis and colon cancer: Roles of gut microbiota involved",
"author": "Sanidad",
"doi-asserted-by": "crossref",
"first-page": "156776",
"journal-title": "Sci. Total Environ.",
"key": "ref_94",
"volume": "842",
"year": "2022"
},
{
"DOI": "10.1177/2042098619854881",
"article-title": "Adverse events associated with home use of mouthrinses: A systematic review",
"author": "Tartaglia",
"doi-asserted-by": "crossref",
"first-page": "2042098619854881",
"journal-title": "Ther. Adv. Drug Saf.",
"key": "ref_95",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1186/s12903-022-02688-z",
"doi-asserted-by": "crossref",
"key": "ref_96",
"unstructured": "Aguilera, F.-R., Viñas, M., Sierra, J.M., Vinuesa, T., de Henestrosa, A.R.F., Furmanczyk, M., Trullàs, C., Jourdan, E., López-López, J., and Jorba, M. (2022). Substantivity of mouth-rinse formulations containing cetylpyridinium chloride and O-cymen-5-ol: A randomized-crossover trial. BMC Oral Health, 22."
},
{
"DOI": "10.14219/jada.archive.2008.0134",
"article-title": "Adverse events associated with chlorhexidine use: Results from the Department of Veterans Affairs Dental Diabetes Study",
"author": "McCoy",
"doi-asserted-by": "crossref",
"first-page": "178",
"journal-title": "J. Am. Dent. Assoc.",
"key": "ref_97",
"volume": "139",
"year": "2008"
},
{
"DOI": "10.5051/jpis.2017.47.3.134",
"article-title": "The antiplaque and bleeding control effects of a cetylpyridinium chloride and tranexamic acid mouth rinse in patients with gingivitis",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "134",
"journal-title": "J. Periodontal Implant. Sci.",
"key": "ref_98",
"volume": "47",
"year": "2017"
},
{
"DOI": "10.3346/jkms.2020.35.e195",
"article-title": "Clinical Significance of a High SARS-CoV-2 Viral Load in the Saliva",
"author": "Yoon",
"doi-asserted-by": "crossref",
"first-page": "e195",
"journal-title": "J. Korean Med. Sci.",
"key": "ref_99",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.1016/0003-9969(74)90089-2",
"article-title": "Influence of concentration, time, temperature and pH on the retention of chlorhexidine in the human oral cavity after mouth rinses",
"author": "Bonesvoll",
"doi-asserted-by": "crossref",
"first-page": "1025",
"journal-title": "Arch. Oral Biol.",
"key": "ref_100",
"volume": "19",
"year": "1974"
},
{
"DOI": "10.1016/0003-9969(74)90090-9",
"article-title": "Relationship between plaque-inhibiting effect and retention of chlorhexidine in the human oral cavity",
"author": "Gjermo",
"doi-asserted-by": "crossref",
"first-page": "1031",
"journal-title": "Arch. Oral Biol.",
"key": "ref_101",
"volume": "19",
"year": "1974"
},
{
"DOI": "10.1159/000320267",
"article-title": "Retention of antimicrobial activity in plaque and saliva following mouthrinse use in vivo",
"author": "Otten",
"doi-asserted-by": "crossref",
"first-page": "459",
"journal-title": "Caries Res.",
"key": "ref_102",
"volume": "44",
"year": "2010"
},
{
"article-title": "In situ chlorhexidine substantivity on saliva and plaque-like biofilm: Influence of circadian rhythm",
"author": "Tomas",
"first-page": "1662",
"journal-title": "J. Periodontol.",
"key": "ref_103",
"volume": "84",
"year": "2013"
},
{
"DOI": "10.1371/journal.pone.0083522",
"doi-asserted-by": "crossref",
"key": "ref_104",
"unstructured": "Garcia-Caballero, L., Quintas, V., Prada-Lopez, I., Seoane, J., Donos, N., and Tomas, I. (2013). Chlorhexidine substantivity on salivary flora and plaque-like biofilm: An in situ model. PLoS ONE, 8."
},
{
"DOI": "10.1007/s00784-009-0320-2",
"article-title": "In vivo substantivity of 0.12% and 0.2% chlorhexidine mouthrinses on salivary bacteria",
"author": "Cousido",
"doi-asserted-by": "crossref",
"first-page": "397",
"journal-title": "Clin. Oral Investig.",
"key": "ref_105",
"volume": "14",
"year": "2010"
},
{
"DOI": "10.1016/j.archoralbio.2008.07.009",
"article-title": "In vivo bactericidal effect of 0.2% chlorhexidine but not 0.12% on salivary obligate anaerobes",
"author": "Tomas",
"doi-asserted-by": "crossref",
"first-page": "1186",
"journal-title": "Arch. Oral Biol.",
"key": "ref_106",
"volume": "53",
"year": "2008"
},
{
"DOI": "10.1111/j.1600-051X.2010.01575.x",
"article-title": "The efficacy of 0.12% chlorhexidine mouthrinse compared with 0.2% on plaque accumulation and periodontal parameters: A systematic review",
"author": "Berchier",
"doi-asserted-by": "crossref",
"first-page": "829",
"journal-title": "J. Clin. Periodontol.",
"key": "ref_107",
"volume": "37",
"year": "2010"
},
{
"DOI": "10.1111/idh.12078",
"article-title": "The effect of chlorhexidine dentifrice or gel versus chlorhexidine mouthwash on plaque, gingivitis, bleeding and tooth discoloration: A systematic review",
"author": "Supranoto",
"doi-asserted-by": "crossref",
"first-page": "83",
"journal-title": "Int. J. Dent. Hyg.",
"key": "ref_108",
"volume": "13",
"year": "2015"
},
{
"DOI": "10.1093/jac/dks129",
"article-title": "Use of hydrogen peroxide as a biocide: New consideration of its mechanisms of biocidal action",
"author": "Linley",
"doi-asserted-by": "crossref",
"first-page": "1589",
"journal-title": "J. Antimicrob. Chemother.",
"key": "ref_109",
"volume": "67",
"year": "2012"
},
{
"DOI": "10.1177/0022034520914246",
"article-title": "Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine",
"author": "Meng",
"doi-asserted-by": "crossref",
"first-page": "481",
"journal-title": "J. Dent. Res.",
"key": "ref_110",
"volume": "99",
"year": "2020"
},
{
"DOI": "10.1111/j.1600-051X.1989.tb02143.x",
"article-title": "Interaction between chlorhexidine digluconate and sodium lauryl sulfate in vivo",
"author": "Barkvoll",
"doi-asserted-by": "crossref",
"first-page": "593",
"journal-title": "J. Clin. Periodontol.",
"key": "ref_111",
"volume": "16",
"year": "1989"
},
{
"DOI": "10.1111/j.1600-0765.1970.tb00697.x",
"article-title": "The effect of chlorhexidine mouthrinses on the human oral flora",
"author": "Schiott",
"doi-asserted-by": "crossref",
"first-page": "84",
"journal-title": "J. Periodontal Res.",
"key": "ref_112",
"volume": "5",
"year": "1970"
},
{
"DOI": "10.3390/pathogens10030272",
"doi-asserted-by": "crossref",
"key": "ref_113",
"unstructured": "Xu, C., Wang, A., Hoskin, E.R., Cugini, C., Markowitz, K., Chang, T.L., and Fine, D.H. (2021). Differential Effects of Antiseptic Mouth Rinses on SARS-CoV-2 Infectivity In Vitro. Pathogens, 10."
},
{
"DOI": "10.3390/microorganisms9030521",
"doi-asserted-by": "crossref",
"key": "ref_114",
"unstructured": "Koch-Heier, J., Hoffmann, H., Schindler, M., Lussi, A., and Planz, O. (2021). Inactivation of SARS-CoV-2 through Treatment with the Mouth Rinsing Solutions ViruProX((R)) and BacterX((R)) Pro. Microorganisms, 9."
},
{
"DOI": "10.1016/j.eclinm.2021.101019",
"article-title": "Characterizing long COVID in an international cohort: 7 months of symptoms and their impact",
"author": "Davis",
"doi-asserted-by": "crossref",
"first-page": "101019",
"journal-title": "EClinicalMedicine",
"key": "ref_115",
"volume": "38",
"year": "2021"
},
{
"DOI": "10.1016/j.jiph.2021.07.020",
"article-title": "In vitro studies evaluating the efficacy of mouth rinses on SARS-CoV-2: A systematic review",
"author": "Tadakamadla",
"doi-asserted-by": "crossref",
"first-page": "1179",
"journal-title": "J. Infect. Public Health",
"key": "ref_116",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1177/0145561320957237",
"article-title": "Efficacy of Povidone-Iodine Nasal and Oral Antiseptic Preparations Against Severe Acute Respiratory Syndrome-Coronavirus 2 (SARS-CoV-2)",
"author": "Pelletier",
"doi-asserted-by": "crossref",
"first-page": "192S",
"journal-title": "Ear Nose Throat J.",
"key": "ref_117",
"volume": "100",
"year": "2021"
},
{
"article-title": "The In Vitro Virucidal Effects of Mouthwashes on SARS-CoV-2",
"author": "Ting",
"first-page": "387",
"journal-title": "Int. J. Transl. Med.",
"key": "ref_118",
"volume": "2",
"year": "2022"
},
{
"DOI": "10.1113/jphysiol.1972.sp009721",
"article-title": "Circadian rhythms in human salivary flow rate and composition",
"author": "Dawes",
"doi-asserted-by": "crossref",
"first-page": "529",
"journal-title": "J. Physiol.",
"key": "ref_119",
"volume": "220",
"year": "1972"
},
{
"DOI": "10.1016/j.sdentj.2022.01.006",
"article-title": "Antiviral effect of mouthwashes against SARS-CoV-2: A systematic review",
"author": "Mendoza",
"doi-asserted-by": "crossref",
"first-page": "167",
"journal-title": "Saudi Dent. J.",
"key": "ref_120",
"volume": "34",
"year": "2022"
},
{
"DOI": "10.1056/NEJMc2016359",
"article-title": "Saliva or Nasopharyngeal Swab Specimens for Detection of SARS-CoV-2",
"author": "Wyllie",
"doi-asserted-by": "crossref",
"first-page": "1283",
"journal-title": "N. Engl. J. Med.",
"key": "ref_121",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1016/j.jinf.2021.09.012",
"article-title": "Self-collected mid-nasal swabs and saliva specimens, compared with nasopharyngeal swabs, for SARS-CoV-2 detection in mild COVID-19 patients",
"author": "Alemany",
"doi-asserted-by": "crossref",
"first-page": "709",
"journal-title": "J. Infect.",
"key": "ref_122",
"volume": "83",
"year": "2021"
},
{
"DOI": "10.1016/j.jinf.2020.11.015",
"article-title": "Comparison of saliva and nasopharyngeal swab SARS-CoV-2 RT-qPCR testing in a community setting",
"author": "Torres",
"doi-asserted-by": "crossref",
"first-page": "84",
"journal-title": "J. Infect.",
"key": "ref_123",
"volume": "82",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2020.35057",
"article-title": "SARS-CoV-2 Transmission From People Without COVID-19 Symptoms",
"author": "Johansson",
"doi-asserted-by": "crossref",
"first-page": "e2035057",
"journal-title": "JAMA Netw. Open",
"key": "ref_124",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1038/s41586-020-03095-6",
"article-title": "Underdetection of cases of COVID-19 in France threatens epidemic control",
"author": "Pullano",
"doi-asserted-by": "crossref",
"first-page": "134",
"journal-title": "Nature",
"key": "ref_125",
"volume": "590",
"year": "2021"
},
{
"DOI": "10.1038/s41591-020-0869-5",
"article-title": "Temporal dynamics in viral shedding and transmissibility of COVID-19",
"author": "He",
"doi-asserted-by": "crossref",
"first-page": "672",
"journal-title": "Nat. Med.",
"key": "ref_126",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1128/JCM.02427-20",
"article-title": "Self-Collected Saline Gargle Samples as an Alternative to Health Care Worker-Collected Nasopharyngeal Swabs for COVID-19 Diagnosis in Outpatients",
"author": "Goldfarb",
"doi-asserted-by": "crossref",
"first-page": "e02427-20",
"journal-title": "J. Clin. Microbiol.",
"key": "ref_127",
"volume": "59",
"year": "2021"
},
{
"article-title": "Detection of SARS-CoV-2 in Different Types of Clinical Specimens",
"author": "Wang",
"first-page": "1843",
"journal-title": "JAMA",
"key": "ref_128",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciaa377",
"article-title": "Gargle Lavage as a Safe and Sensitive Alternative to Swab Samples to Diagnose COVID-19: A Case Report in Japan",
"author": "Saito",
"doi-asserted-by": "crossref",
"first-page": "893",
"journal-title": "Clin. Infect. Dis.",
"key": "ref_129",
"volume": "71",
"year": "2020"
},
{
"DOI": "10.1373/clinchem.2005.063206",
"article-title": "Characterization of RNA in saliva",
"author": "Park",
"doi-asserted-by": "crossref",
"first-page": "988",
"journal-title": "Clin. Chem.",
"key": "ref_130",
"volume": "52",
"year": "2006"
},
{
"DOI": "10.1007/s00784-020-03549-1",
"article-title": "A prospective clinical pilot study on the effects of a hydrogen peroxide mouthrinse on the intraoral viral load of SARS-CoV-2",
"author": "Gottsauner",
"doi-asserted-by": "crossref",
"first-page": "3707",
"journal-title": "Clin. Oral Investig.",
"key": "ref_131",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1038/s41586-020-2196-x",
"article-title": "Virological assessment of hospitalized patients with COVID-2019",
"author": "Corman",
"doi-asserted-by": "crossref",
"first-page": "465",
"journal-title": "Nature",
"key": "ref_132",
"volume": "581",
"year": "2020"
},
{
"DOI": "10.1016/j.ajoms.2021.02.002",
"article-title": "Virucidal activity of oral care products against SARS-CoV-2 in vitro",
"author": "Komine",
"doi-asserted-by": "crossref",
"first-page": "475",
"journal-title": "J. Oral Maxillofac. Surg. Med. Pathol.",
"key": "ref_133",
"volume": "33",
"year": "2021"
},
{
"DOI": "10.1177/03000605211063695",
"article-title": "Virucidal effect of povidone-iodine against SARS-CoV-2 in vitro",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "3000605211063695",
"journal-title": "J. Int. Med. Res.",
"key": "ref_134",
"volume": "49",
"year": "2021"
},
{
"DOI": "10.1152/ajplung.00552.2020",
"article-title": "Carrageenan-containing over-the-counter nasal and oral sprays inhibit SARS-CoV-2 infection of airway epithelial cultures",
"author": "Schutz",
"doi-asserted-by": "crossref",
"first-page": "L750",
"journal-title": "Am. J. Physiol. Lung Cell. Mol. Physiol.",
"key": "ref_135",
"volume": "320",
"year": "2021"
},
{
"DOI": "10.1016/S1473-3099(20)30237-1",
"article-title": "Understanding COVID-19: What does viral RNA load really mean?",
"author": "Joynt",
"doi-asserted-by": "crossref",
"first-page": "635",
"journal-title": "Lancet Infect. Dis.",
"key": "ref_136",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1111/j.1600-0765.1970.tb00696.x",
"article-title": "The effect of mouthrinses and topical application of chlorhexidine on the development of dental plaque and gingivitis in man",
"author": "Loe",
"doi-asserted-by": "crossref",
"first-page": "79",
"journal-title": "J. Periodontal Res.",
"key": "ref_137",
"volume": "5",
"year": "1970"
},
{
"article-title": "Effect of toothbrushing with chlorhexidine gel on salivary microflora, oral hygiene, and caries",
"author": "Emilson",
"first-page": "308",
"journal-title": "Scand. J. Dent. Res.",
"key": "ref_138",
"volume": "84",
"year": "1976"
},
{
"DOI": "10.1111/j.1600-051X.1993.tb00345.x",
"article-title": "A 6-month home usage trial of a 1% chlorhexidine toothpaste (II). Effects on the oral microflora",
"author": "Maynard",
"doi-asserted-by": "crossref",
"first-page": "207",
"journal-title": "J. Clin. Periodontol.",
"key": "ref_139",
"volume": "20",
"year": "1993"
},
{
"DOI": "10.1016/j.jhin.2016.08.018",
"article-title": "Acquired resistance to chlorhexidine—Is it time to establish an ‘antiseptic stewardship’ initiative?",
"author": "Kampf",
"doi-asserted-by": "crossref",
"first-page": "213",
"journal-title": "J. Hosp. Infect.",
"key": "ref_140",
"volume": "94",
"year": "2016"
},
{
"DOI": "10.3390/antibiotics7040110",
"doi-asserted-by": "crossref",
"key": "ref_141",
"unstructured": "Kampf, G. (2018). Biocidal Agents Used for Disinfection Can Enhance Antibiotic Resistance in Gram-Negative Species. Antibiotics, 7."
},
{
"DOI": "10.3389/fmicb.2019.00587",
"article-title": "Resistance Toward Chlorhexidine in Oral. Bacteria—Is There Cause for Concern?",
"author": "Cieplik",
"doi-asserted-by": "crossref",
"first-page": "587",
"journal-title": "Front. Microbiol.",
"key": "ref_142",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1016/S1473-3099(03)00833-8",
"article-title": "Biocide use and antibiotic resistance: The relevance of laboratory findings to clinical and environmental situations",
"author": "Russell",
"doi-asserted-by": "crossref",
"first-page": "794",
"journal-title": "Lancet Infect. Dis.",
"key": "ref_143",
"volume": "3",
"year": "2003"
},
{
"DOI": "10.1016/S0300-5712(95)00116-6",
"article-title": "Effect of use of 0.05% cetylpyridinium chloride mouthwash on normal oral flora",
"author": "Radford",
"doi-asserted-by": "crossref",
"first-page": "35",
"journal-title": "J. Dent.",
"key": "ref_144",
"volume": "25",
"year": "1997"
}
],
"reference-count": 144,
"references-count": 144,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2227-9059/11/6/1694"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Biochemistry, Genetics and Molecular Biology",
"Medicine (miscellaneous)"
],
"subtitle": [],
"title": "Preprocedural Viral Load Effects of Oral Antiseptics on SARS-CoV-2 in Patients with COVID-19: A Systematic Review",
"type": "journal-article",
"volume": "11"
}