Impact of Disease on Plasma and Lung Exposure of Chloroquine, Hydroxychloroquine and Azithromycin: Application of PBPK Modeling
et al., Clinical Pharmacology & Therapeutics, doi:10.1002/cpt.1955, Jul 2020
HCQ for COVID-19
1st treatment shown to reduce risk in
March 2020, now with p < 0.00000000001 from 423 studies, used in 59 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
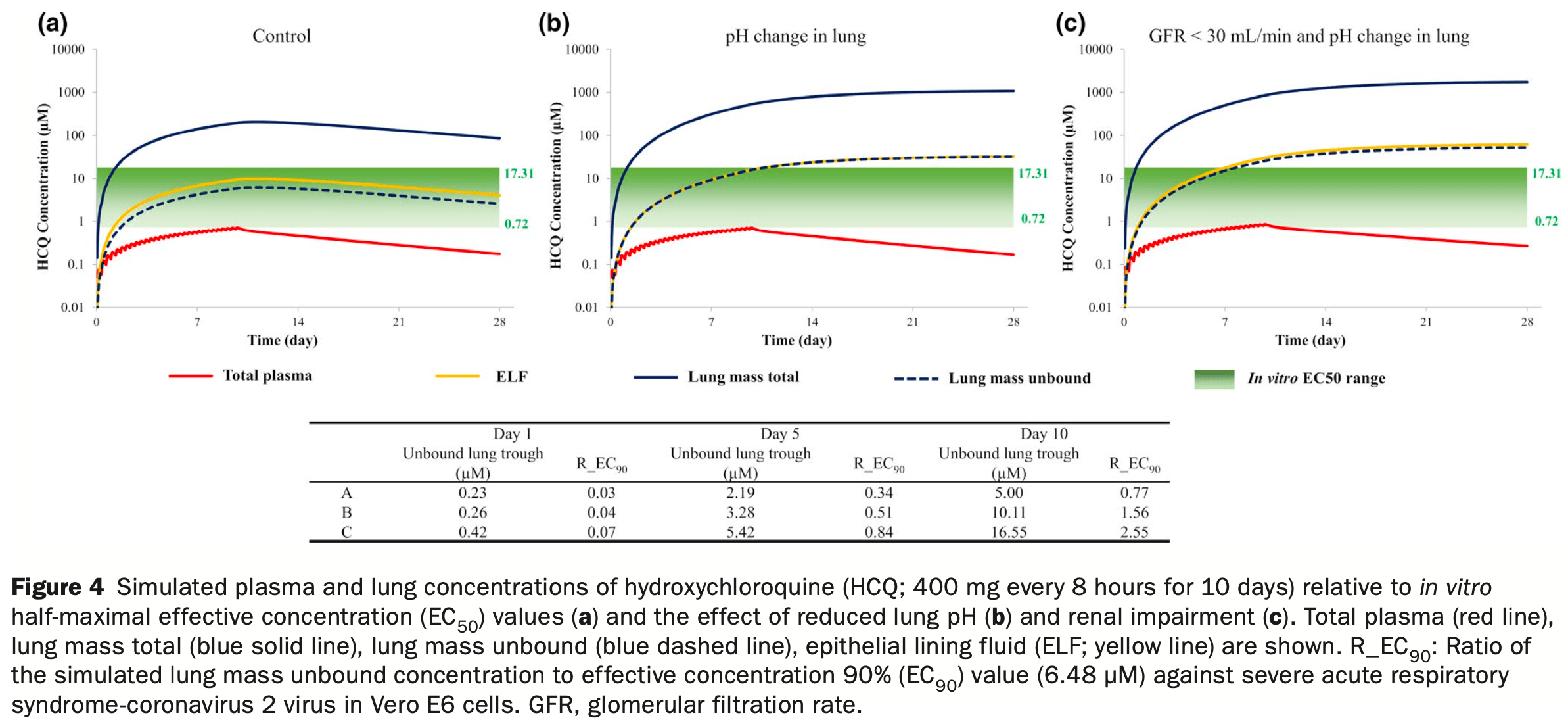
In silico study using physiologically-based pharmacokinetic modeling to demonstrate that accumulation of chloroquine (CQ), hydroxychloroquine (HCQ), and azithromycin (AZ) in the lungs is sensitive to changes in lung pH, which can be affected in patients with COVID-19. A reduction in lung pH from 6.7 to 6.0 led to 20-fold, 4.0-fold, and 2.7-fold increases in lung exposure of CQ, HCQ, and AZ, respectively. Simulations indicated that relatively high concentrations of CQ and HCQ in lung tissue were sustained long after drug administration stopped. Patients with COVID-19 often present with kidney failure. Simulations indicate that renal impairment plus lung pH reduction caused 30-fold, 8.0-fold, and 3.4-fold increases in lung exposures for CQ, HCQ, and AZ, respectively, with relatively small accompanying increases in systemic exposure.
39 preclinical studies support the efficacy of HCQ for COVID-19:
1.
Shang et al., Identification of Cathepsin L as the molecular target of hydroxychloroquine with chemical proteomics, Molecular & Cellular Proteomics, doi:10.1016/j.mcpro.2025.101314.
2.
González-Paz et al., Biophysical Analysis of Potential Inhibitors of SARS-CoV-2 Cell Recognition and Their Effect on Viral Dynamics in Different Cell Types: A Computational Prediction from In Vitro Experimental Data, ACS Omega, doi:10.1021/acsomega.3c06968.
3.
Alkafaas et al., A study on the effect of natural products against the transmission of B.1.1.529 Omicron, Virology Journal, doi:10.1186/s12985-023-02160-6.
4.
Guimarães Silva et al., Are Non-Structural Proteins From SARS-CoV-2 the Target of Hydroxychloroquine? An in Silico Study, ACTA MEDICA IRANICA, doi:10.18502/acta.v61i2.12533.
5.
Nguyen et al., The Potential of Ameliorating COVID-19 and Sequelae From Andrographis paniculata via Bioinformatics, Bioinformatics and Biology Insights, doi:10.1177/11779322221149622.
7.
Yadav et al., Repurposing the Combination Drug of Favipiravir, Hydroxychloroquine and Oseltamivir as a Potential Inhibitor Against SARS-CoV-2: A Computational Study, Research Square, doi:10.21203/rs.3.rs-628277/v1.
8.
Hussein et al., Molecular Docking Identification for the efficacy of Some Zinc Complexes with Chloroquine and Hydroxychloroquine against Main Protease of COVID-19, Journal of Molecular Structure, doi:10.1016/j.molstruc.2021.129979.
9.
Baildya et al., Inhibitory capacity of Chloroquine against SARS-COV-2 by effective binding with Angiotensin converting enzyme-2 receptor: An insight from molecular docking and MD-simulation studies, Journal of Molecular Structure, doi:10.1016/j.molstruc.2021.129891.
10.
Noureddine et al., Quantum chemical studies on molecular structure, AIM, ELF, RDG and antiviral activities of hybrid hydroxychloroquine in the treatment of COVID-19: molecular docking and DFT calculations, Journal of King Saud University - Science, doi:10.1016/j.jksus.2020.101334.
11.
Tarek et al., Pharmacokinetic Basis of the Hydroxychloroquine Response in COVID-19: Implications for Therapy and Prevention, European Journal of Drug Metabolism and Pharmacokinetics, doi:10.1007/s13318-020-00640-6.
12.
Rowland Yeo et al., Impact of Disease on Plasma and Lung Exposure of Chloroquine, Hydroxychloroquine and Azithromycin: Application of PBPK Modeling, Clinical Pharmacology & Therapeutics, doi:10.1002/cpt.1955.
13.
Hitti et al., Hydroxychloroquine attenuates double-stranded RNA-stimulated hyper-phosphorylation of tristetraprolin/ZFP36 and AU-rich mRNA stabilization, Immunology, doi:10.1111/imm.13835.
14.
Yan et al., Super-resolution imaging reveals the mechanism of endosomal acidification inhibitors against SARS-CoV-2 infection, ChemBioChem, doi:10.1002/cbic.202400404.
15.
Mohd Abd Razak et al., In Vitro Anti-SARS-CoV-2 Activities of Curcumin and Selected Phenolic Compounds, Natural Product Communications, doi:10.1177/1934578X231188861.
16.
Alsmadi et al., The In Vitro, In Vivo, and PBPK Evaluation of a Novel Lung-Targeted Cardiac-Safe Hydroxychloroquine Inhalation Aerogel, AAPS PharmSciTech, doi:10.1208/s12249-023-02627-3.
17.
Wen et al., Cholinergic α7 nAChR signaling suppresses SARS-CoV-2 infection and inflammation in lung epithelial cells, Journal of Molecular Cell Biology, doi:10.1093/jmcb/mjad048.
18.
Kamga Kapchoup et al., In vitro effect of hydroxychloroquine on pluripotent stem cells and their cardiomyocytes derivatives, Frontiers in Pharmacology, doi:10.3389/fphar.2023.1128382.
19.
Milan Bonotto et al., Cathepsin inhibitors nitroxoline and its derivatives inhibit SARS-CoV-2 infection, Antiviral Research, doi:10.1016/j.antiviral.2023.105655.
20.
Miao et al., SIM imaging resolves endocytosis of SARS-CoV-2 spike RBD in living cells, Cell Chemical Biology, doi:10.1016/j.chembiol.2023.02.001.
21.
Yuan et al., Hydroxychloroquine blocks SARS-CoV-2 entry into the endocytic pathway in mammalian cell culture, Communications Biology, doi:10.1038/s42003-022-03841-8.
22.
Faísca et al., Enhanced In Vitro Antiviral Activity of Hydroxychloroquine Ionic Liquids against SARS-CoV-2, Pharmaceutics, doi:10.3390/pharmaceutics14040877.
23.
Delandre et al., Antiviral Activity of Repurposing Ivermectin against a Panel of 30 Clinical SARS-CoV-2 Strains Belonging to 14 Variants, Pharmaceuticals, doi:10.3390/ph15040445.
24.
Purwati et al., An in vitro study of dual drug combinations of anti-viral agents, antibiotics, and/or hydroxychloroquine against the SARS-CoV-2 virus isolated from hospitalized patients in Surabaya, Indonesia, PLOS One, doi:10.1371/journal.pone.0252302.
25.
Zhang et al., SARS-CoV-2 spike protein dictates syncytium-mediated lymphocyte elimination, Cell Death & Differentiation, doi:10.1038/s41418-021-00782-3.
26.
Dang et al., Structural basis of anti-SARS-CoV-2 activity of hydroxychloroquine: specific binding to NTD/CTD and disruption of LLPS of N protein, bioRxiv, doi:10.1101/2021.03.16.435741.
27.
Shang (B) et al., Inhibitors of endosomal acidification suppress SARS-CoV-2 replication and relieve viral pneumonia in hACE2 transgenic mice, Virology Journal, doi:10.1186/s12985-021-01515-1.
28.
Wang et al., Chloroquine and hydroxychloroquine as ACE2 blockers to inhibit viropexis of 2019-nCoV Spike pseudotyped virus, Phytomedicine, doi:10.1016/j.phymed.2020.153333.
29.
Sheaff, R., A New Model of SARS-CoV-2 Infection Based on (Hydroxy)Chloroquine Activity, bioRxiv, doi:10.1101/2020.08.02.232892.
30.
Ou et al., Hydroxychloroquine-mediated inhibition of SARS-CoV-2 entry is attenuated by TMPRSS2, PLOS Pathogens, doi:10.1371/journal.ppat.1009212.
31.
Andreani et al., In vitro testing of combined hydroxychloroquine and azithromycin on SARS-CoV-2 shows synergistic effect, Microbial Pathogenesis, doi:10.1016/j.micpath.2020.104228.
32.
Clementi et al., Combined Prophylactic and Therapeutic Use Maximizes Hydroxychloroquine Anti-SARS-CoV-2 Effects in vitro, Front. Microbiol., 10 July 2020, doi:10.3389/fmicb.2020.01704.
33.
Liu et al., Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro, Cell Discovery 6, 16 (2020), doi:10.1038/s41421-020-0156-0.
34.
Yao et al., In Vitro Antiviral Activity and Projection of Optimized Dosing Design of Hydroxychloroquine for the Treatment of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), Clin. Infect. Dis., 2020 Mar 9, doi:10.1093/cid/ciaa237.
Rowland Yeo et al., 16 Jul 2020, peer-reviewed, 7 authors.
In silico studies are an important part of preclinical research, however results may be very different in vivo.
Impact of Disease on Plasma and Lung Exposure of Chloroquine, Hydroxychloroquine and Azithromycin: Application of PBPK Modeling
Clinical Pharmacology & Therapeutics, doi:10.1002/cpt.1955
We use a mechanistic lung model to demonstrate that accumulation of chloroquine (CQ), hydroxychloroquine (HCQ), and azithromycin (AZ) in the lungs is sensitive to changes in lung pH, a parameter that can be affected in patients with coronavirus disease 2019 (COVID-19). A reduction in pH from 6.7 to 6 in the lungs, as observed in respiratory disease, led to 20-fold, 4.0-fold, and 2.7-fold increases in lung exposure of CQ, HCQ, and AZ, respectively. Simulations indicated that the relatively high concentrations of CQ and HCQ in lung tissue were sustained long after administration of the drugs had stopped. Patients with COVID-19 often present with kidney failure. Our simulations indicate that renal impairment (plus lung pH reduction) caused 30-fold, 8.0-fold, and 3.4-fold increases in lung exposures for CQ, HCQ, and AZ, respectively, with relatively small accompanying increases (20 to 30%) in systemic exposure. Although a number of different dosage regimens were assessed, the purpose of our study was not to provide recommendations for a dosing strategy, but to demonstrate the utility of a physiologically-based pharmacokinetic modeling approach to estimate lung concentrations. This, used in conjunction with robust in vitro and clinical data, can help in the assessment of COVID-19 therapeutics going forward.
Coronavirus disease 2019 (COVID-19 ) has rapidly become a global pandemic, since the outbreak was initially identified in Wuhan, China, in December 2019. The virus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), can infect the lower respiratory tract causing fevers, cough, and pneumonia. As new drug candidates are being investigated for treatment of COVID-19, efforts are being made to repurpose existing antimalarial drugs, as they are readily available, and have a known safety profile. Specifically, it has been reported that chloroquine (CQ) has been successful in treating SARS-CoV-2 infections in China. 1 In vitro studies have since confirmed that hydroxychloroquine (HCQ), an analog of CQ, is a more potent inhibitor of SARS-CoV-2 (5-fold to 7-fold). 2 Given that HCQ also has a more favorable safety profile than CQ during chronic dosing, a clinical study was conducted in France to determine whether HCQ (600 mg daily; 465 mg base) could be a more viable option for COVID-19
SUPPORTING INFORMATION Supplementary information accompanies this paper on the Clinical Pharmacology & Therapeutics website (www.cpt-journal.com).
CONFLICT OF INTEREST All authors are paid employees of Certara UK Limited (Simcyp Division) or Certara Inc.
References
Adelusi, Salako, Kinetics of the distribution and elimination of chloroquine in the rat, Gen. Pharmacol
Adelusi, Salako, Tissue and blood concentrations of chloroquine following chronic administration in the rat, J. Pharm. Pharmacol
Arnold, Buckner, Hydroxychloroquine for treatment of SARS-CoV-2 infection? Improving our confidence in a modelbased approach to dose selection, Clin. Transl. Sci
Bohte, Mattie, Van Den Broek, Levels of azithromycin and alpha-1 acid glycoprotein in serum in patients with community-acquired pneumonia, Antimicrob. Agents Chemother
Cheng, Kidney impairment is associated with inhospital death of COVID-19 patients, Kidney Int
Collins, Jackson, Gustafson, Hydroxychloroquine: a physiologically-based pharmacokinetic model in the context of cancer-related autophagy modulation, J. Pharmacol. Exp. Ther
Effros, Chinard, The in vivo pH of the extravascular space of the lung, J. Clin. Invest
Fan, Connecting hydroxychloroquine in vitro antiviral activity to in vivo concentration for prediction of antiviral effect: a critical step in treating COVID-19 patients, Clin. Infect. Dis, doi:10.1093/cid/ciaa623.
Ferrari, Cutler, Kinetics and thermodynamics of chloroquine and hydroxychloroquine transport across the human erythrocyte membrane, Biochem. Pharmacol
Fischer, Widdicombe, Mechanisms of acid and base secretion by the airway epithelium, J. Membr. Biol
Gao, Tian, Yang, Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies, Biosci. Trends
Gaohua, Development of a multicompartment permeability-limited lung PBPK model and its application in predicting pulmonary pharmacokinetics of antituberculosis drugs, CPT Pharmacometrics Syst. Pharmacol
Gautret, Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label nonrandomized clinical trial, Int. J. Antimicrob. Agents, doi:10.1016/j.ijantimicag.2020.105949.
Gessner, Exhaled breath condensate acidification in acute lung injury, Respir. Med
Giudicessi, Noseworthy, Friedman, Ackerman, Urgent guidance for navigating and circumventing the QTc-prolonging and torsadogenic potential of possible pharmacotherapies for coronavirus disease 19 (COVID-19), Mayo Clin. Proc
Hallifax, Houston, Saturable uptake of lipophilic amine drugs into isolated hepatocytes: mechanisms and consequences for quantitative clearance prediction, Drug Metab. Disposition
Jamei, A mechanistic framework for in vitro-in vivo extrapolation of liver membrane transporters: prediction of drugdrug interaction between rosuvastatin and cyclosporine, Clin. Pharmacokinet
Johnson, Boussery, Rowland-Yeo, Tucker, Rostami-Hodjegan, A semi-mechanistic model to predict the effects of liver cirrhosis on drug clearance, Clin. Pharmacokinet
Johnson, Jamei, Rowland-Yeo, How does in vivo biliary elimination of drugs change with age? Evidence from in vitro and clinical data using a systems pharmacology approach, Drug Metab. Disposition
Jones, Rowland-Yeo, Basic concepts in physiologically based pharmacokinetic modeling in drug discovery and development, CPT Pharmacometrics Syst. Pharmacol
Katneni, Using human plasma as an assay medium in Caco-2 studies improves mass balance for lipophilic compounds, Pharm. Res
Kiem, Schentag, Interpretation of antibiotic concentration ratios measured in epithelial lining fluid, Antimicrob. Agents Chemother
Liu, Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro, Cell Discov
Lucchi, Pharmacokinetics of azithromycin in serum, bronchial washings, alveolar macrophages and lung tissue following a single oral dose of extended or immediate release formulations of azithromycin, J. Antimicrob. Chemother
Mcchesney, Fasco, Banks, Kersch, The metabolism of chloroquine in man during and after repeated oral dosage, J. Pharmacol. Exp. Ther
Munster, Hydroxychloroquine concentration-response relationships in patients with rheumatoid arthritis, Arthritis Rheum
Nožinić, Milić, Mikac, Ralić, Padovan et al., Assessment of macrolide transport using PAMPA, Caco-2 and MDCKII-hMDR1 assays, Croat. Chem. Acta
Pan, Xu, Zhang, Zhou, Wang et al., Identification of a potential mechanism of acute kidney injury during the covid-19 outbreak: a study based on single-cell transcriptome analysis, Intensive Care Med
Polak, Quantitative approach for cardiac risk assessment and interpretation in tuberculosis drug development, J. Pharmacokinet. Pharmacodyn
Rodgers, Leahy, Rowland, Physiologically based pharmacokinetic modeling 1: predicting the tissue distribution of moderate-to-strong bases, J. Pharm. Sci
Touret, In vitro screening of a FDA approved chemical library reveals potential inhibitors of SARS-CoV-2 replication, bioRxiv, doi:10.1101/2020.04.03.023846
Viasus, Prognostic value of serum albumin levels in hospitalized adults with community-acquired pneumonia, J. Infect
Wan, Inflammation inhibitors were remarkably upregulated in plasma of severe acute respiratory syndrome patients at progressive phase, Proteomics
Wang, Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro, Cell Res
Wi, Kim, Peck, Serum albumin level as a predictor of intensive respiratory or vasopressor support in influenza A (H1N1) virus infection, Int. J. Clin. Pract
Yao, In vitro antiviral activity and projection of optimized dosing design of hydroxychloroquine for the treatment of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), Clin. Infect. Dis, doi:10.1093/cid/ciaa237
Yeo, Aarabi, Jamei, Rostami-Hodjegan, Modeling and predicting drug pharmacokinetics in patients with renal impairment, Expert Rev. Clin. Pharmacol
DOI record:
{
"DOI": "10.1002/cpt.1955",
"ISSN": [
"0009-9236",
"1532-6535"
],
"URL": "http://dx.doi.org/10.1002/cpt.1955",
"abstract": "<jats:p>We use a mechanistic lung model to demonstrate that accumulation of chloroquine (CQ), hydroxychloroquine (HCQ), and azithromycin (AZ) in the lungs is sensitive to changes in lung pH, a parameter that can be affected in patients with coronavirus disease 2019 (COVID‐19). A reduction in pH from 6.7 to 6 in the lungs, as observed in respiratory disease, led to 20‐fold, 4.0‐fold, and 2.7‐fold increases in lung exposure of CQ, HCQ, and AZ, respectively. Simulations indicated that the relatively high concentrations of CQ and HCQ in lung tissue were sustained long after administration of the drugs had stopped. Patients with COVID‐19 often present with kidney failure. Our simulations indicate that renal impairment (plus lung pH reduction) caused 30‐fold, 8.0‐fold, and 3.4‐fold increases in lung exposures for CQ, HCQ, and AZ, respectively, with relatively small accompanying increases (20 to 30%) in systemic exposure. Although a number of different dosage regimens were assessed, the purpose of our study was not to provide recommendations for a dosing strategy, but to demonstrate the utility of a physiologically‐based pharmacokinetic modeling approach to estimate lung concentrations. This, used in conjunction with robust <jats:italic>in vitro</jats:italic> and clinical data, can help in the assessment of COVID‐19 therapeutics going forward.</jats:p>",
"alternative-id": [
"10.1002/cpt.1955"
],
"assertion": [
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2020-04-22"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 1,
"value": "2020-06-06"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 2,
"value": "2020-07-16"
}
],
"author": [
{
"affiliation": [
{
"name": "Certara UK Limited (Simcyp Division) Sheffield UK"
}
],
"family": "Rowland Yeo",
"given": "Karen",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Certara UK Limited (Simcyp Division) Sheffield UK"
}
],
"family": "Zhang",
"given": "Mian",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Certara UK Limited (Simcyp Division) Sheffield UK"
}
],
"family": "Pan",
"given": "Xian",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Certara UK Limited (Simcyp Division) Sheffield UK"
}
],
"family": "Ban Ke",
"given": "Alice",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Certara UK Limited (Simcyp Division) Sheffield UK"
}
],
"family": "Jones",
"given": "Hannah M.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Certara Inc. Princeton New Jersey USA"
}
],
"family": "Wesche",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Certara UK Limited (Simcyp Division) Sheffield UK"
}
],
"family": "Almond",
"given": "Lisa M.",
"sequence": "additional"
}
],
"container-title": "Clinical Pharmacology & Therapeutics",
"container-title-short": "Clin Pharma and Therapeutics",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"ascpt.onlinelibrary.wiley.com"
]
},
"created": {
"date-parts": [
[
2020,
6,
12
]
],
"date-time": "2020-06-12T22:16:08Z",
"timestamp": 1592000168000
},
"deposited": {
"date-parts": [
[
2023,
11,
7
]
],
"date-time": "2023-11-07T13:29:07Z",
"timestamp": 1699363747000
},
"indexed": {
"date-parts": [
[
2024,
7,
18
]
],
"date-time": "2024-07-18T05:58:29Z",
"timestamp": 1721282309826
},
"is-referenced-by-count": 28,
"issue": "5",
"issued": {
"date-parts": [
[
2020,
7,
16
]
]
},
"journal-issue": {
"issue": "5",
"published-print": {
"date-parts": [
[
2020,
11
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
7,
16
]
],
"date-time": "2020-07-16T00:00:00Z",
"timestamp": 1594857600000
}
}
],
"link": [
{
"URL": "https://api.wiley.com/onlinelibrary/tdm/v1/articles/10.1002%2Fcpt.1955",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1002/cpt.1955",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://onlinelibrary.wiley.com/doi/full-xml/10.1002/cpt.1955",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://ascpt.onlinelibrary.wiley.com/doi/pdf/10.1002/cpt.1955",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "311",
"original-title": [],
"page": "976-984",
"prefix": "10.1111",
"published": {
"date-parts": [
[
2020,
7,
16
]
]
},
"published-online": {
"date-parts": [
[
2020,
7,
16
]
]
},
"published-print": {
"date-parts": [
[
2020,
11
]
]
},
"publisher": "Wiley",
"reference": [
{
"DOI": "10.5582/bst.2020.01047",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_1_1"
},
{
"article-title": "In vitro antiviral activity and projection of optimized dosing design of hydroxychloroquine for the treatment of severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2)",
"author": "Yao X.",
"journal-title": "Clin. Infect. Dis.",
"key": "e_1_2_10_2_1"
},
{
"article-title": "Hydroxychloroquine and azithromycin as a treatment of COVID‐19: results of an open‐label non‐randomized clinical trial",
"author": "Gautret P.",
"journal-title": "Int. J. Antimicrob. Agents",
"key": "e_1_2_10_3_1"
},
{
"DOI": "10.1124/dmd.107.015131",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_4_1"
},
{
"DOI": "10.1124/jpet.117.245639",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_5_1"
},
{
"DOI": "10.1016/j.kint.2020.03.005",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_6_1"
},
{
"DOI": "10.1007/s00134-020-06026-1",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_7_1"
},
{
"DOI": "10.1038/psp.2013.41",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_8_1"
},
{
"DOI": "10.1586/ecp.10.143",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_9_1"
},
{
"DOI": "10.2165/11318160-000000000-00000",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_10_1"
},
{
"DOI": "10.1111/cts.12797",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_11_1"
},
{
"DOI": "10.1002/psp4.12034",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_12_1"
},
{
"DOI": "10.1038/s41421-019-0132-8",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_13_1"
},
{
"article-title": "In vitro screening of a FDA approved chemical library reveals potential inhibitors of SARS‐CoV‐2 replication",
"author": "Touret F.",
"journal-title": "bioRxiv",
"key": "e_1_2_10_14_1"
},
{
"DOI": "10.1038/s41422-020-0282-0",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_15_1"
},
{
"DOI": "10.1124/dmd.115.068643",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_16_1"
},
{
"DOI": "10.1128/AAC.00133-06",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_17_1"
},
{
"DOI": "10.1007/s40262-013-0097-y",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_18_1"
},
{
"DOI": "10.1002/jps.20322",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_19_1"
},
{
"DOI": "10.1007/s11095-018-2493-3",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_20_1"
},
{
"DOI": "10.1016/0006-2952(91)90006-Q",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_21_1"
},
{
"article-title": "Assessment of macrolide transport using PAMPA, Caco‐2 and MDCKII‐hMDR1 assays",
"author": "Nožinić D.",
"first-page": "323",
"journal-title": "Croat. Chem. Acta",
"key": "e_1_2_10_22_1",
"volume": "83",
"year": "2010"
},
{
"DOI": "10.1007/s00232-006-0861-0",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_23_1"
},
{
"DOI": "10.1016/S0954-6111(03)00225-7",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_24_1"
},
{
"DOI": "10.1172/JCI106164",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_25_1"
},
{
"DOI": "10.1016/j.jinf.2012.12.007",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_26_1"
},
{
"DOI": "10.1111/ijcp.12249",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_27_1"
},
{
"DOI": "10.1128/AAC.39.12.2801",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_28_1"
},
{
"DOI": "10.1002/pmic.200500638",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_29_1"
},
{
"article-title": "The metabolism of chloroquine in man during and after repeated oral dosage",
"author": "McChesney E.",
"first-page": "323",
"journal-title": "J. Pharmacol. Exp. Ther.",
"key": "e_1_2_10_30_1",
"volume": "158",
"year": "1967"
},
{
"DOI": "10.1002/art.10307",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_31_1"
},
{
"DOI": "10.1093/jac/dkn032",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_32_1"
},
{
"article-title": "Connecting hydroxychloroquine in vitro antiviral activity to in vivo concentration for prediction of antiviral effect: a critical step in treating COVID‐19 patients",
"author": "Fan J.",
"journal-title": "Clin. Infect. Dis.",
"key": "e_1_2_10_33_1"
},
{
"DOI": "10.1016/j.mayocp.2020.03.024",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_34_1"
},
{
"DOI": "10.1007/s10928-018-9580-2",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_35_1"
},
{
"DOI": "10.1016/0306-3623(82)90110-0",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_36_1"
},
{
"DOI": "10.1111/j.2042-7158.1982.tb06211.x",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_37_1"
}
],
"reference-count": 37,
"references-count": 37,
"relation": {},
"resource": {
"primary": {
"URL": "https://ascpt.onlinelibrary.wiley.com/doi/10.1002/cpt.1955"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Impact of Disease on Plasma and Lung Exposure of Chloroquine, Hydroxychloroquine and Azithromycin: Application of PBPK Modeling",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1002/crossmark_policy",
"volume": "108"
}
