SARS-CoV-2 infection causes a decline in renal megalin expression and affects vitamin D metabolism in the kidney of K18-hACE2 mice
et al., Scientific Reports, doi:10.1038/s41598-024-75338-9, Oct 2024
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
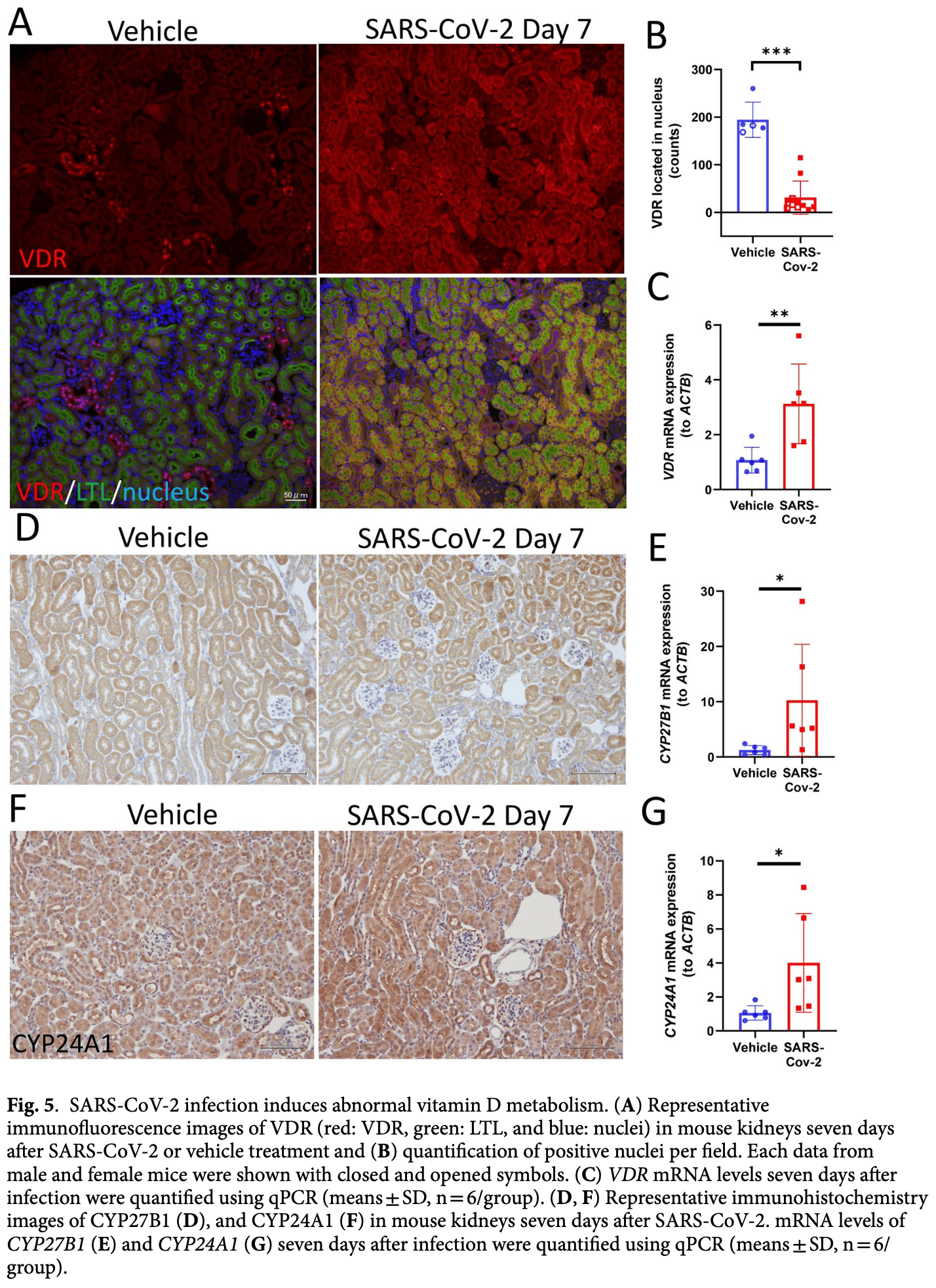
Mouse study showing that SARS-CoV-2 infection decreases renal megalin expression and affects vitamin D metabolism in K18-hACE2 mice. Authors found that infected mice experienced acute kidney injury, suppressed megalin protein levels in proximal tubules, decreased vitamin D receptor localization in the nucleus, and increased mRNA expression of vitamin D-related genes CYP27B1 and CYP24A1. Serum vitamin D levels were unchanged, but an increase in pro-inflammatory TNF-alpha and decrease in anti-inflammatory IL-4 were observed in kidneys of infected mice. The findings suggest megalin loss may impact the local immunomodulatory role of vitamin D in the kidney during SARS-CoV-2 infection.
29 preclinical studies support the efficacy of vitamin D for COVID-19:
Vitamin D has been identified by the European Food Safety Authority (EFSA) as having sufficient evidence for a causal relationship between intake and optimal immune system function27-30.
Vitamin D inhibits SARS-CoV-2 replication in vitro17,24, mitigates lung inflammation, damage, and lethality in mice with an MHV-3 model for β-CoV respiratory infections17,24, reduces SARS-CoV-2 replication in nasal epithelial cells via increased type I interferon expression20, downregulates proinflammatory cytokines IL-1β and TNF-α in SARS-CoV-2 spike protein-stimulated cells16, attenuates nucleocapsid protein-induced hyperinflammation by inactivating the NLRP3 inflammasome through the VDR-BRCC3 signaling pathway21, may be neuroprotective by protecting the blood-brain barrier, reducing neuroinflammation, and via immunomodulatory effects31, may mitigate hyperinflammation and cytokine storm by upregulating TLR10 expression which downregulates proinflammatory cytokines13, downregulates ACE2 and TMPRSS2 in human trophoblasts and minimizes spike protein-induced inflammation19, may minimize cytokine storm by dampening excessive cytokine production2, may suppress viral entry and replication via LL-37 induction11,12, and minimizes platelet aggregation mediated by SARS-CoV-2 spike protein via inhibiting integrin αIIbβ3 outside-in signaling15.
Cholecalciferol and calcifediol directly bind two allosteric pockets on the SARS-CoV-2 Spike RBD, bias the trimer toward a closed state, weaken ACE2 engagement, and reduce viral entry in cell models1.
Calcitriol may destabilize the Spike protein architecture and inhibit IL-17R dimerization, blocking viral entry and mitigating hyperinflammatory cytokine storm32.
Vitamin D improves regulatory immune cell levels and control of proinflammatory cytokines in severe COVID-1933.
Calcifediol inhibits SARS-CoV-2 papain-like protease (PLpro), a critical enzyme for viral replication14.
Symptomatic COVID-19 is associated with a lower frequency of natural killer (NK) cells and vitamin D has been shown to improve NK cell activity34,35.
1.
García-Marín et al., Exploring SARS-CoV-2 Spike RBD Pockets as Targets for Generic Drugs: A Combined Computational, Biophysical, and Biological Approach, ACS Omega, doi:10.1021/acsomega.5c05175.
2.
Alzahrani, A., A new investigation into the molecular mechanism of cholecalciferol towards reducing cytokines storm, Octahedron Drug Research, doi:10.21608/odr.2024.308273.1043.
3.
Haque et al., Exploring potential therapeutic candidates against COVID-19: a molecular docking study, Discover Molecules, doi:10.1007/s44345-024-00005-5.
4.
Morales-Bayuelo et al., New findings on ligand series used as SARS-CoV-2 virus inhibitors within the frameworks of molecular docking, molecular quantum similarity and chemical reactivity indices, F1000Research, doi:10.12688/f1000research.123550.3.
5.
Chellasamy et al., Docking and molecular dynamics studies of human ezrin protein with a modelled SARS-CoV-2 endodomain and their interaction with potential invasion inhibitors, Journal of King Saud University - Science, doi:10.1016/j.jksus.2022.102277.
6.
Pandya et al., Unravelling Vitamin B12 as a potential inhibitor against SARS-CoV-2: A computational approach, Informatics in Medicine Unlocked, doi:10.1016/j.imu.2022.100951.
7.
Mansouri et al., The impact of calcitriol and estradiol on the SARS-CoV-2 biological activity: a molecular modeling approach, Scientific Reports, doi:10.1038/s41598-022-04778-y.
8.
Song et al., Vitamin D3 and its hydroxyderivatives as promising drugs against COVID-19: a computational study, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2021.1964601.
9.
Qayyum et al., Vitamin D and lumisterol novel metabolites can inhibit SARS-CoV-2 replication machinery enzymes, Endocrinology and Metabolism, doi:10.1152/ajpendo.00174.2021.
10.
Al-Mazaideh et al., Vitamin D is a New Promising Inhibitor to the Main Protease (Mpro) of COVID-19 by Molecular Docking, Journal of Pharmaceutical Research International, doi:10.9734/jpri/2021/v33i29B31603.
11.
Roth et al., Vitamin D-inducible antimicrobial peptide LL-37 binds SARS-CoV-2 Spike and accessory proteins ORF7a and ORF8, Frontiers in Cellular and Infection Microbiology, doi:10.3389/fcimb.2025.1671738.
12.
Vercellino et al., Influence of Sex and 1,25α Dihydroxyvitamin D3 on SARS-CoV-2 Infection and Viral Entry, Pathogens, doi:10.3390/pathogens14080765.
13.
Knez et al., TLR10 overexpression modulates immune response in A549 lung epithelial cells challenged with SARS-CoV-2 S and N proteins, Frontiers in Immunology, doi:10.3389/fimmu.2024.1490478.
14.
Chen et al., In Vitro Characterization of Inhibition Function of Calcifediol to the Protease Activity of SARS-COV-2 PLpro, Journal of Medical Virology, doi:10.1002/jmv.70085.
15.
Wang et al., 1,25‐Dihydroxyvitamin D3 attenuates platelet aggregation potentiated by SARS‐CoV‐2 spike protein via inhibiting integrin αIIbβ3 outside‐in signaling, Cell Biochemistry and Function, doi:10.1002/cbf.4039.
16.
Alcalá-Santiago et al., Disentangling the Immunomodulatory Effects of Vitamin D on the SARS-CoV-2 Virus by In Vitro Approaches, The 14th European Nutrition Conference FENS 2023, doi:10.3390/proceedings2023091415.
17.
Campolina-Silva et al., Dietary Vitamin D Mitigates Coronavirus-Induced Lung Inflammation and Damage in Mice, Viruses, doi:10.3390/v15122434.
18.
Moatasim et al., Potent Antiviral Activity of Vitamin B12 against Severe Acute Respiratory Syndrome Coronavirus 2, Middle East Respiratory Syndrome Coronavirus, and Human Coronavirus 229E, Microorganisms, doi:10.3390/microorganisms11112777.
19.
Vargas-Castro et al., Calcitriol prevents SARS-CoV spike-induced inflammation in human trophoblasts through downregulating ACE2 and TMPRSS2 expression, The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2024.106625.
20.
Sposito et al., Age differential CD13 and interferon expression in airway epithelia affect SARS-CoV-2 infection - effects of vitamin D, Mucosal Immunology, doi:10.1016/j.mucimm.2023.08.002.
21.
Chen (B) et al., Vitamin D3 attenuates SARS‐CoV‐2 nucleocapsid protein‐caused hyperinflammation by inactivating the NLRP3 inflammasome through the VDR‐BRCC3 signaling pathway in vitro and in vivo, MedComm, doi:10.1002/mco2.318.
22.
Rybakovsky et al., Calcitriol modifies tight junctions, improves barrier function, and reduces TNF‐α‐induced barrier leak in the human lung‐derived epithelial cell culture model, 16HBE 14o‐, Physiological Reports, doi:10.14814/phy2.15592.
23.
DiGuilio et al., The multiphasic TNF-α-induced compromise of Calu-3 airway epithelial barrier function, Experimental Lung Research, doi:10.1080/01902148.2023.2193637.
24.
Pickard et al., Discovery of re-purposed drugs that slow SARS-CoV-2 replication in human cells, PLOS Pathogens, doi:10.1371/journal.ppat.1009840.
25.
Mok et al., Calcitriol, the active form of vitamin D, is a promising candidate for COVID-19 prophylaxis, bioRxiv, doi:10.1101/2020.06.21.162396.
26.
Fernandes de Souza et al., Lung Inflammation Induced by Inactivated SARS-CoV-2 in C57BL/6 Female Mice Is Controlled by Intranasal Instillation of Vitamin D, Cells, doi:10.3390/cells12071092.
27.
Galmés et al., Suboptimal Consumption of Relevant Immune System Micronutrients Is Associated with a Worse Impact of COVID-19 in Spanish Populations, Nutrients, doi:10.3390/nu14112254.
28.
Galmés (B) et al., Current State of Evidence: Influence of Nutritional and Nutrigenetic Factors on Immunity in the COVID-19 Pandemic Framework, Nutrients, doi:10.3390/nu12092738.
29.
EFSA, Scientific Opinion on the substantiation of a health claim related to vitamin D and contribution to the normal function of the immune system pursuant to Article 14 of Regulation (EC) No 1924/2006, EFSA Journal, doi:10.2903/j.efsa.2015.4096.
30.
EFSA (B), Scientific Opinion on the substantiation of health claims related to vitamin D and normal function of the immune system and inflammatory response (ID 154, 159), maintenance of normal muscle function (ID 155) and maintenance of normal cardiovascular function (ID 159) pursuant to Article 13(1) of Regulation (E, EFSA Journal, doi:10.2903/j.efsa.2010.1468.
31.
Gotelli et al., Understanding the immune-endocrine effects of vitamin D in SARS-CoV-2 infection: a role in protecting against neurodamage?, Neuroimmunomodulation, doi:10.1159/000533286.
32.
Fadel et al., Targeting asparagine and cysteine in SARS-CoV-2 variants and human pro-inflammatory mediators to alleviate COVID-19 severity; a cross-section and in-silico study, Scientific Reports, doi:10.1038/s41598-025-19359-y.
33.
Saheb Sharif-Askari et al., Increased blood immune regulatory cells in severe COVID-19 with autoantibodies to type I interferons, Scientific Reports, doi:10.1038/s41598-023-43675-w.
Kurosaki et al., 16 Oct 2024, peer-reviewed, 12 authors.
Contact: kuboma@kitasato-u.ac.jp.
SARS-CoV-2 infection causes a decline in renal megalin expression and affects vitamin D metabolism in the kidney of K18-hACE2 mice
Scientific Reports, doi:10.1038/s41598-024-75338-9
Patients with coronavirus disease 2019 (COVID-19) often experience acute kidney injury, linked to disease severity or mortality, along with renal tubular dysfunction and megalin loss in proximal tubules. Megalin plays a crucial role in kidney vitamin D metabolism. However, the impact of megalin loss on vitamin D metabolism during COVID-19 is unclear. This study investigated whether severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection reduces megalin expression in proximal tubules and its subsequent effect on vitamin D metabolism in mice expressing human angiotensin converting enzyme 2 (K18-hACE2 mice). Histological and immunohistochemical staining analyses revealed glomerular and capillary congestion, and elevated renal neutrophil gelatinase-associated lipocalin levels, indicative of acute kidney injury in K18-hACE2 mice. In SARS-CoV-2-infected mice, immunohistochemical staining revealed suppressed megalin protein levels. Decreased vitamin D receptor (VDR) localization in the nucleus and increased mRNA expression of VDR, CYP27B1, and CYP24A1 were observed by quantitative PCR in SARS-CoV-2-infected mice. Serum vitamin D levels remained similar in infected and vehicle-treated mice, but an increase in tumor necrosis factor-alpha and a decrease in IL-4 mRNA expression were observed in the kidneys of the SARS-CoV-2 group. These findings suggest that megalin loss in SARS-CoV-2 infection may impact the local role of vitamin D in kidney immunomodulation, even when blood vitamin D levels remain unchanged. Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has become a global pandemic. Studies have reported a correlation between acute kidney injury (AKI) and overall disease severity or mortality 1,2 . A systematic review and meta-analysis of 20 cohorts with COVID-19-associated AKI (CoV-AKI) reported a prevalence of AKI ranging from 0.5 to 80% (with an average of 17%) and 77% of the patients with AKI exhibited severe COVID-19 manifestation 3 . Some mechanisms for kidney injury in COVID-19 have been proposed, including direct infection, inflammatory injury followed by a cytokine storm, and ischemic injury caused by multiorgan failure 4,5 ; however, the cause of kidney injury in COVID-19 remains unclear. Previous studies have reported that acute tubular injury is the main finding in patients with CoV-AKI [6] [7] [8] . A postmortem study patients revealed significant acute tubular injury in all patients 9 . Low-grade proteinuria has been detected in patients with COVID-19 without AKI 10, 11 . Proteinuria during hospitalization was significantly associated with an increased risk of death 12 , which suggests that renal tubular dysfunction
Author contributions Y.K., H.K., H.H., and M.K. provided conception and design of research; Y.K., T.M., T.U., and M.I. performed experiments; Y.K., T.M., F.K., R.K., and S.T. analyzed data; Y.K., T.U., F.K., R.K., T.I., N.I., H.K., H.H., and M.K. interpreted results of experiments; Y.K. and T.M. prepared figures; Y.K. drafted manuscript; Y.K., T.U., T.I., N.I., H.K., H.H., and M.K. edited and revised manuscript; Y.K., T.M., T.U., F.K., R.K., S.T., M.I., T.I., N.I., H.K., H.H., and M.K. approved final version of manuscript.
Competing interests The authors declare no competing interests.
Additional information
Supplementary Information The online version contains supplementary material available at https://doi. org/10.1038/s41598-024-75338-9 . Correspondence and requests for materials should be addressed to M.K. Reprints and permissions information is available at www.nature.com/reprints. Publisher's note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence..
References
Akilesh, Multicenter Clinicopathologic Correlation of Kidney Biopsies Performed in COVID-19 Patients Presenting With Acute Kidney Injury or Proteinuria, Am. J. Kidney Dis
Azrielant, Shoenfeld, Vitamin D and the immune system, Isr. Med. Assoc. J
Baeke, Takiishi, Korf, Gysemans, Mathieu, Vitamin D: modulator of the immune system, Curr. Opin. Pharmacol
Basalamah, Vitamin D alleviates lead induced renal and testicular injuries by immunomodulatory and antioxidant mechanisms in rats, Sci. Rep
Biemesderfer, Regulated intramembrane proteolysis of megalin: linking urinary protein and gene regulation in proximal tubule?, Kidney Int
Bikle, Vitamin D regulation of immune function during covid-19, Rev. Endocr. Metab. Disord
Bosworth, De Boer, Impaired vitamin D metabolism in CKD, Semin. Nephrol
Bowe, Xie, Xu, Al-Aly, Kidney outcomes in long COVID, J. Am. Soc. Nephrol
Camargo, Cord-blood 25-hydroxyvitamin D levels and risk of respiratory infection, wheezing, and asthma, Pediatrics
Chan, AKI in hospitalized patients with COVID-19, J. Am. Soc. Nephrol
Chaudhri, Association of proteinuria and hematuria with acute kidney injury and mortality in hospitalized patients with COVID-19, Kidney Blood Press. Res
Chavez-Valencia, Orizaga-De-La-Cruz, Lagunas-Rangel, Acute kidney injury in COVID-19 patients: Pathogenesis, clinical characteristics, therapy, and mortality, Diseases
Cheng, Kidney disease is associated with in-hospital death of patients with COVID-19, Kidney Int
Costagliola, Nutraceuticals in viral infections: An overview of the immunomodulating properties, Nutrients
Curtis, Sex and gender differences in AKI, Kidney
Daniel, Sartory, Zahn, Radeke, Stein, Immune modulatory treatment of trinitrobenzene sulfonic acid colitis with calcitriol is associated with a change of a T helper (Th) 1/Th17 to a Th2 and regulatory T cell profile, J. Pharmacol. Exp. Ther
De Braganca, Vitamin D deficiency aggravates ischemic acute kidney injury in rats, Physiol. Rep
Durvasula, Wellington, Mcnamara, Watnick, COVID-19 and kidney failure in the acute care setting: Our experience from seattle, Am. J. Kidney Dis
Farkash, Wilson, Jentzen, Ultrastructural evidence for direct renal infection with SARS-CoV-2, J. Am. Soc. Nephrol
Fatah, Reduced proximal tubular expression of protein endocytic receptors in proteinuria is associated with urinary receptor shedding, Nephrol. Dial. Transplant
Fisher, AKI in hospitalized patients with and without COVID-19: A comparison study, J. Am. Soc. Nephrol
George, Evidence for SARS-CoV-2 Spike Protein in the Urine of COVID-19 Patients, Kidney
Graidis, Papavramidis, Papaioannou, Vitamin D and acute kidney injury: A two-way causality relation and a predictive, prognostic, and therapeutic role of vitamin D, Front Nutr
Hirsch, Acute kidney injury in patients hospitalized with COVID-19, Kidney Int
Hjalm, Cloning and sequencing of human gp330, a Ca(2+)-binding receptor with potential intracellular signaling properties, Eur. J. Biochem
Holick, Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease, Am. J. Clin. Nutr
Holick, Vitamin, Deficiency, None, N. Engl. J. Med
Jin, Interleukin-10 deficiency aggravates kidney inflammation and fibrosis in the unilateral ureteral obstruction mouse model, Lab. Invest
Jones, Prosser, Kaufmann, 25-Hydroxyvitamin D-24-hydroxylase (CYP24A1): Its important role in the degradation of vitamin D, Arch. Biochem. Biophys
Kazemi, Association of vitamin D status with SARS-CoV-2 infection or COVID-19 severity: A systematic review and meta-analysis, Adv. Nutr
Kellum, Chawla, Cell-cycle arrest and acute kidney injury: the light and the dark sides, Nephrol. Dial. Transplant
Kilari, Yang, Sharma, Mccall, Misra, Increased transforming growth factor beta (TGF-beta) and pSMAD3 signaling in a murine model for contrast induced kidney injury, Sci. Rep
Kozai, Thyroid hormones decrease plasma 1alpha,25-dihydroxyvitamin D levels through transcriptional repression of the renal 25-hydroxyvitamin D3 1alpha-hydroxylase gene (CYP27B1), Endocrinology
Kurosaki, In vitro study on effect of bardoxolone methyl on cisplatin-induced cellular senescence in human proximal tubular cells, Mol. Cell. Biochem
Kurosaki, Oxidative stress increases megalin expression in the renal proximal tubules during the normoalbuminuric stage of diabetes mellitus, Am. J. Physiol. Renal Physiol
Leaf, Wolf, Stern, Elevated FGF-23 in a patient with rhabdomyolysis-induced acute kidney injury, Nephrol. Dial. Transplant
Li, Cong, Biemesderfer, The COOH terminus of megalin regulates gene expression in opossum kidney proximal tubule cells, Am. J. Physiol. Cell Physiol
Maritzen, Rickheit, Schmitt, Jentsch, Kidney-specific upregulation of vitamin D3 target genes in ClC-5 KO mice, Kidney Int
Matsuyama, Enhanced isolation of SARS-CoV-2 by TMPRSS2-expressing cells, Proc. Natl. Acad. Sci. U. S. A
Mazanova, The link between vitamin D status and NF-kappaB-associated renal dysfunction in experimental diabetes mellitus, Biochim. Biophys. Acta Gen. Subj
Mccray, Lethal infection of K18-hACE2 mice infected with severe acute respiratory syndrome coronavirus, J. Virol
Mizuiri, Ohashi, ACE and ACE2 in kidney disease, World J. Nephrol
Mohamed, Acute kidney injury associated with coronavirus disease 2019 in urban new orleans, Kidney
Mohamed, Velez, Proteinuria in COVID-19, Clin Kidney J
Murai, Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: A randomized clinical trial, JAMA
Naicker, The Novel Coronavirus 2019 epidemic and kidneys, Kidney Int
Nykjaer, An endocytic pathway essential for renal uptake and activation of the steroid 25-(OH) vitamin D3, Cell
Nykjaer, Cubilin dysfunction causes abnormal metabolism of the steroid hormone 25(OH) vitamin D(3), Proc. Natl. Acad. Sci
Omer, Human kidney spheroids and monolayers provide insights into SARS-CoV-2 renal interactions, J. Am. Soc. Nephrol
Robbins-Juarez, Outcomes for patients with COVID-19 and acute kidney injury: A systematic review and meta-analysis, Kidney Int Rep
Rowling, Kemmis, Taffany, Welsh, Megalin-mediated endocytosis of vitamin D binding protein correlates with 25-hydroxycholecalciferol actions in human mammary cells, J. Nutr
Saito, Pietromonaco, Loo, Farquhar, Complete cloning and sequencing of rat gp330/"megalin," a distinctive member of the low density lipoprotein receptor gene family, Proc. Natl. Acad. Sci
Santoriello, Postmortem kidney pathology findings in patients with COVID-19, J. Am. Soc. Nephrol
Sapartini, Wong, Indrati, Kartasasmita, Setiabudiawan, The association between vitamin D, interleukin-4, and interleukin-10 levels and CD23+ expression with bronchial asthma in stunted children, Biomedicines
Schuster, Cytochromes P450 are essential players in the vitamin D signaling system, Biochim. Biophys. Acta
Silva-Aguiar, SARS-CoV-2 spike protein inhibits megalin-mediated albumin endocytosis in proximal tubule epithelial cells, Biochim. Biophys. Acta Mol. Basis Dis
Su, Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China, Kidney Int
Tourigny, CYP24A1 exacerbated activity during diabetes contributes to kidney tubular apoptosis via caspase-3 increased expression and activation, PLoS One
Wang, Sun, Gao, Lian, Zhou, Cell cycle arrest as a therapeutic target of acute kidney injury, Curr. Protein Pept. Sci
Werion, SARS-CoV-2 causes a specific dysfunction of the kidney proximal tubule, Kidney Int
Wolf, Forging forward with 10 burning questions on FGF23 in kidney disease, J. Am. Soc. Nephrol
Xu, The importance of vitamin d metabolism as a potential prophylactic, immunoregulatory and neuroprotective treatment for COVID-19, J. Transl. Med
Yin, Agrawal, Vitamin D and inflammatory diseases, J Inflamm. Res
Zehnder, Reduction of the vitamin D hormonal system in kidney disease is associated with increased renal inflammation, Kidney Int
Zhou, A pneumonia outbreak associated with a new coronavirus of probable bat origin, Nature
DOI record:
{
"DOI": "10.1038/s41598-024-75338-9",
"ISSN": [
"2045-2322"
],
"URL": "http://dx.doi.org/10.1038/s41598-024-75338-9",
"alternative-id": [
"75338"
],
"article-number": "24313",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "25 January 2024"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "4 October 2024"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "16 October 2024"
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1,
"value": "The authors declare no competing interests."
}
],
"author": [
{
"affiliation": [],
"family": "Kurosaki",
"given": "Yoshifumi",
"sequence": "first"
},
{
"affiliation": [],
"family": "Matsumoto",
"given": "Toshihide",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Uematsu",
"given": "Takayuki",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kawakami",
"given": "Fumitaka",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kawashima",
"given": "Rei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tamaki",
"given": "Shun",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Imai",
"given": "Motoki",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ichikawa",
"given": "Takafumi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ishii",
"given": "Naohito",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kitasato",
"given": "Hidero",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hanaki",
"given": "Hideaki",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kubo",
"given": "Makoto",
"sequence": "additional"
}
],
"container-title": "Scientific Reports",
"container-title-short": "Sci Rep",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2024,
10,
16
]
],
"date-time": "2024-10-16T18:02:21Z",
"timestamp": 1729101741000
},
"deposited": {
"date-parts": [
[
2024,
10,
16
]
],
"date-time": "2024-10-16T18:04:03Z",
"timestamp": 1729101843000
},
"funder": [
{
"DOI": "10.13039/501100020291",
"award": [
"Grant-in-Aid for Research Project No. 2022-1020"
],
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/501100020291",
"id-type": "DOI"
}
],
"name": "School of Allied Health Sciences, Kitasato University"
},
{
"name": "COVID-19 Kitasato Project"
}
],
"indexed": {
"date-parts": [
[
2024,
10,
17
]
],
"date-time": "2024-10-17T04:28:14Z",
"timestamp": 1729139294747,
"version": "3.27.0"
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2024,
10,
16
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2024,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc-nd/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
10,
16
]
],
"date-time": "2024-10-16T00:00:00Z",
"timestamp": 1729036800000
}
},
{
"URL": "https://creativecommons.org/licenses/by-nc-nd/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
10,
16
]
],
"date-time": "2024-10-16T00:00:00Z",
"timestamp": 1729036800000
}
}
],
"link": [
{
"URL": "https://www.nature.com/articles/s41598-024-75338-9.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-024-75338-9",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-024-75338-9.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1038",
"published": {
"date-parts": [
[
2024,
10,
16
]
]
},
"published-online": {
"date-parts": [
[
2024,
10,
16
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.34067/KID.0002652020",
"author": "MMB Mohamed",
"doi-asserted-by": "publisher",
"first-page": "614",
"journal-title": "Kidney",
"key": "75338_CR1",
"unstructured": "Mohamed, M. M. B. et al. Acute kidney injury associated with coronavirus disease 2019 in urban new orleans. Kidney 1, 614–622 (2020).",
"volume": "1",
"year": "2020"
},
{
"DOI": "10.1681/ASN.2020050615",
"author": "L Chan",
"doi-asserted-by": "publisher",
"first-page": "151",
"journal-title": "J. Am. Soc. Nephrol.",
"key": "75338_CR2",
"unstructured": "Chan, L. et al. AKI in hospitalized patients with COVID-19. J. Am. Soc. Nephrol. 32, 151–160 (2021).",
"volume": "32",
"year": "2021"
},
{
"DOI": "10.1016/j.ekir.2020.06.013",
"author": "SY Robbins-Juarez",
"doi-asserted-by": "publisher",
"first-page": "1149",
"journal-title": "Kidney Int Rep.",
"key": "75338_CR3",
"unstructured": "Robbins-Juarez, S. Y. et al. Outcomes for patients with COVID-19 and acute kidney injury: A systematic review and meta-analysis. Kidney Int Rep. 5, 1149–1160 (2020).",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1016/j.kint.2020.03.001",
"author": "S Naicker",
"doi-asserted-by": "publisher",
"first-page": "824",
"journal-title": "Kidney Int.",
"key": "75338_CR4",
"unstructured": "Naicker, S. et al. The Novel Coronavirus 2019 epidemic and kidneys. Kidney Int. 97, 824–828 (2020).",
"volume": "97",
"year": "2020"
},
{
"DOI": "10.1053/j.ajkd.2020.04.001",
"author": "R Durvasula",
"doi-asserted-by": "publisher",
"first-page": "4",
"journal-title": "Am. J. Kidney Dis.",
"key": "75338_CR5",
"unstructured": "Durvasula, R., Wellington, T., McNamara, E. & Watnick, S. COVID-19 and kidney failure in the acute care setting: Our experience from seattle. Am. J. Kidney Dis. 76, 4–6 (2020).",
"volume": "76",
"year": "2020"
},
{
"DOI": "10.1681/ASN.2020050744",
"author": "D Santoriello",
"doi-asserted-by": "publisher",
"first-page": "2158",
"journal-title": "J. Am. Soc. Nephrol.",
"key": "75338_CR6",
"unstructured": "Santoriello, D. et al. Postmortem kidney pathology findings in patients with COVID-19. J. Am. Soc. Nephrol. 31, 2158–2167 (2020).",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1053/j.ajkd.2020.10.001",
"author": "S Akilesh",
"doi-asserted-by": "publisher",
"first-page": "82",
"journal-title": "Am. J. Kidney Dis.",
"key": "75338_CR7",
"unstructured": "Akilesh, S. et al. Multicenter Clinicopathologic Correlation of Kidney Biopsies Performed in COVID-19 Patients Presenting With Acute Kidney Injury or Proteinuria. Am. J. Kidney Dis. 77, 82–93 (2021).",
"volume": "77",
"year": "2021"
},
{
"DOI": "10.1093/ckj/sfab036",
"author": "MMB Mohamed",
"doi-asserted-by": "publisher",
"first-page": "i40",
"journal-title": "Clin Kidney J.",
"key": "75338_CR8",
"unstructured": "Mohamed, M. M. B. & Velez, J. C. Q. Proteinuria in COVID-19. Clin Kidney J. 14, i40–i47 (2021).",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1016/j.kint.2020.04.003",
"author": "H Su",
"doi-asserted-by": "publisher",
"first-page": "219",
"journal-title": "Kidney Int.",
"key": "75338_CR9",
"unstructured": "Su, H. et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 98, 219–227 (2020).",
"volume": "98",
"year": "2020"
},
{
"DOI": "10.1681/ASN.2020040509",
"author": "M Fisher",
"doi-asserted-by": "publisher",
"first-page": "2145",
"journal-title": "J. Am. Soc. Nephrol.",
"key": "75338_CR10",
"unstructured": "Fisher, M. et al. AKI in hospitalized patients with and without COVID-19: A comparison study. J. Am. Soc. Nephrol. 31, 2145–2157 (2020).",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1016/j.kint.2020.03.005",
"author": "Y Cheng",
"doi-asserted-by": "publisher",
"first-page": "829",
"journal-title": "Kidney Int.",
"key": "75338_CR11",
"unstructured": "Cheng, Y. et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 97, 829–838 (2020).",
"volume": "97",
"year": "2020"
},
{
"DOI": "10.1159/000511946",
"author": "I Chaudhri",
"doi-asserted-by": "publisher",
"first-page": "1018",
"journal-title": "Kidney Blood Press. Res.",
"key": "75338_CR12",
"unstructured": "Chaudhri, I. et al. Association of proteinuria and hematuria with acute kidney injury and mortality in hospitalized patients with COVID-19. Kidney Blood Press. Res. 45, 1018–1032 (2020).",
"volume": "45",
"year": "2020"
},
{
"DOI": "10.1093/advances/nmab012",
"author": "A Kazemi",
"doi-asserted-by": "publisher",
"first-page": "1636",
"journal-title": "Adv. Nutr.",
"key": "75338_CR13",
"unstructured": "Kazemi, A. et al. Association of vitamin D status with SARS-CoV-2 infection or COVID-19 severity: A systematic review and meta-analysis. Adv. Nutr. 12, 1636–1658 (2021).",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1542/peds.2010-0442",
"author": "CA Camargo Jr",
"doi-asserted-by": "publisher",
"first-page": "e180",
"journal-title": "Pediatrics.",
"key": "75338_CR14",
"unstructured": "Camargo, C. A. Jr. et al. Cord-blood 25-hydroxyvitamin D levels and risk of respiratory infection, wheezing, and asthma. Pediatrics. 127, e180-187 (2011).",
"volume": "127",
"year": "2011"
},
{
"DOI": "10.1007/s11154-021-09707-4",
"author": "DD Bikle",
"doi-asserted-by": "publisher",
"first-page": "279",
"journal-title": "Rev. Endocr. Metab. Disord.",
"key": "75338_CR15",
"unstructured": "Bikle, D. D. Vitamin D regulation of immune function during covid-19. Rev. Endocr. Metab. Disord. 23, 279–285 (2022).",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.3390/nu13072410",
"author": "G Costagliola",
"doi-asserted-by": "publisher",
"first-page": "2410",
"journal-title": "Nutrients",
"key": "75338_CR16",
"unstructured": "Costagliola, G. et al. Nutraceuticals in viral infections: An overview of the immunomodulating properties. Nutrients 13, 2410 (2021).",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.26848",
"author": "IH Murai",
"doi-asserted-by": "publisher",
"first-page": "1053",
"journal-title": "JAMA",
"key": "75338_CR17",
"unstructured": "Murai, I. H. et al. Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: A randomized clinical trial. JAMA 325, 1053–1060 (2021).",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.1016/j.bbapap.2010.06.022",
"author": "I Schuster",
"doi-asserted-by": "publisher",
"first-page": "186",
"journal-title": "Biochim. Biophys. Acta.",
"key": "75338_CR18",
"unstructured": "Schuster, I. Cytochromes P450 are essential players in the vitamin D signaling system. Biochim. Biophys. Acta. 1814, 186–199 (2011).",
"volume": "1814",
"year": "2011"
},
{
"DOI": "10.1093/ajcn/80.6.1678S",
"author": "MF Holick",
"doi-asserted-by": "publisher",
"first-page": "1678S",
"journal-title": "Am. J. Clin. Nutr.",
"key": "75338_CR19",
"unstructured": "Holick, M. F. Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am. J. Clin. Nutr. 80, 1678S-1688S (2004).",
"volume": "80",
"year": "2004"
},
{
"author": "K Yin",
"first-page": "69",
"journal-title": "J Inflamm. Res.",
"key": "75338_CR20",
"unstructured": "Yin, K. & Agrawal, D. K. Vitamin D and inflammatory diseases. J Inflamm. Res. 7, 69–87 (2014).",
"volume": "7",
"year": "2014"
},
{
"DOI": "10.1056/NEJMra070553",
"author": "MF Holick",
"doi-asserted-by": "publisher",
"first-page": "266",
"journal-title": "N. Engl. J. Med.",
"key": "75338_CR21",
"unstructured": "Holick, M. F. Vitamin D deficiency. N. Engl. J. Med. 357, 266–281 (2007).",
"volume": "357",
"year": "2007"
},
{
"DOI": "10.1016/j.abb.2011.11.003",
"author": "G Jones",
"doi-asserted-by": "publisher",
"first-page": "9",
"journal-title": "Arch. Biochem. Biophys.",
"key": "75338_CR22",
"unstructured": "Jones, G., Prosser, D. E. & Kaufmann, M. 25-Hydroxyvitamin D-24-hydroxylase (CYP24A1): Its important role in the degradation of vitamin D. Arch. Biochem. Biophys. 523, 9–18 (2012).",
"volume": "523",
"year": "2012"
},
{
"DOI": "10.3389/fnut.2020.630951",
"author": "S Graidis",
"doi-asserted-by": "publisher",
"journal-title": "Front Nutr.",
"key": "75338_CR23",
"unstructured": "Graidis, S., Papavramidis, T. S. & Papaioannou, M. Vitamin D and acute kidney injury: A two-way causality relation and a predictive, prognostic, and therapeutic role of vitamin D. Front Nutr. 7, 630951 (2020).",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1016/j.semnephrol.2012.12.016",
"author": "C Bosworth",
"doi-asserted-by": "publisher",
"first-page": "158",
"journal-title": "Semin. Nephrol.",
"key": "75338_CR24",
"unstructured": "Bosworth, C. & de Boer, I. H. Impaired vitamin D metabolism in CKD. Semin. Nephrol. 33, 158–168 (2013).",
"volume": "33",
"year": "2013"
},
{
"DOI": "10.1073/pnas.241516998",
"author": "A Nykjaer",
"doi-asserted-by": "publisher",
"first-page": "13895",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "75338_CR25",
"unstructured": "Nykjaer, A. et al. Cubilin dysfunction causes abnormal metabolism of the steroid hormone 25(OH) vitamin D(3). Proc. Natl. Acad. Sci. USA 98, 13895–13900 (2001).",
"volume": "98",
"year": "2001"
},
{
"DOI": "10.1073/pnas.91.21.9725",
"author": "A Saito",
"doi-asserted-by": "publisher",
"first-page": "9725",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "75338_CR26",
"unstructured": "Saito, A., Pietromonaco, S., Loo, A. K. & Farquhar, M. G. Complete cloning and sequencing of rat gp330/\"megalin,\" a distinctive member of the low density lipoprotein receptor gene family. Proc. Natl. Acad. Sci. USA 91, 9725–9729 (1994).",
"volume": "91",
"year": "1994"
},
{
"DOI": "10.1111/j.1432-1033.1996.0132u.x",
"author": "G Hjalm",
"doi-asserted-by": "publisher",
"first-page": "132",
"journal-title": "Eur. J. Biochem.",
"key": "75338_CR27",
"unstructured": "Hjalm, G. et al. Cloning and sequencing of human gp330, a Ca(2+)-binding receptor with potential intracellular signaling properties. Eur. J. Biochem. 239, 132–137 (1996).",
"volume": "239",
"year": "1996"
},
{
"DOI": "10.1016/S0092-8674(00)80655-8",
"author": "A Nykjaer",
"doi-asserted-by": "publisher",
"first-page": "507",
"journal-title": "Cell",
"key": "75338_CR28",
"unstructured": "Nykjaer, A. et al. An endocytic pathway essential for renal uptake and activation of the steroid 25-(OH) vitamin D3. Cell 96, 507–515 (1999).",
"volume": "96",
"year": "1999"
},
{
"DOI": "10.1016/j.kint.2020.07.019",
"author": "A Werion",
"doi-asserted-by": "publisher",
"first-page": "1296",
"journal-title": "Kidney Int.",
"key": "75338_CR29",
"unstructured": "Werion, A. et al. SARS-CoV-2 causes a specific dysfunction of the kidney proximal tubule. Kidney Int. 98, 1296–1307 (2020).",
"volume": "98",
"year": "2020"
},
{
"DOI": "10.1681/ASN.2020111546",
"author": "D Omer",
"doi-asserted-by": "publisher",
"first-page": "2242",
"journal-title": "J. Am. Soc. Nephrol.",
"key": "75338_CR30",
"unstructured": "Omer, D. et al. Human kidney spheroids and monolayers provide insights into SARS-CoV-2 renal interactions. J. Am. Soc. Nephrol. 32, 2242–2254 (2021).",
"volume": "32",
"year": "2021"
},
{
"DOI": "10.2174/1389203717666160915162238",
"author": "WG Wang",
"doi-asserted-by": "publisher",
"first-page": "1224",
"journal-title": "Curr. Protein Pept. Sci.",
"key": "75338_CR31",
"unstructured": "Wang, W. G., Sun, W. X., Gao, B. S., Lian, X. & Zhou, H. L. Cell cycle arrest as a therapeutic target of acute kidney injury. Curr. Protein Pept. Sci. 18, 1224–1231 (2017).",
"volume": "18",
"year": "2017"
},
{
"DOI": "10.1093/ndt/gfv130",
"author": "JA Kellum",
"doi-asserted-by": "publisher",
"first-page": "16",
"journal-title": "Nephrol. Dial. Transplant.",
"key": "75338_CR32",
"unstructured": "Kellum, J. A. & Chawla, L. S. Cell-cycle arrest and acute kidney injury: the light and the dark sides. Nephrol. Dial. Transplant. 31, 16–22 (2016).",
"volume": "31",
"year": "2016"
},
{
"DOI": "10.1038/s41598-018-24340-z",
"author": "S Kilari",
"doi-asserted-by": "publisher",
"first-page": "6630",
"journal-title": "Sci. Rep.",
"key": "75338_CR33",
"unstructured": "Kilari, S., Yang, B., Sharma, A., McCall, D. L. & Misra, S. Increased transforming growth factor beta (TGF-beta) and pSMAD3 signaling in a murine model for contrast induced kidney injury. Sci. Rep. 8, 6630 (2018).",
"volume": "8",
"year": "2018"
},
{
"DOI": "10.1016/j.kint.2020.05.006",
"author": "JS Hirsch",
"doi-asserted-by": "publisher",
"first-page": "209",
"journal-title": "Kidney Int.",
"key": "75338_CR34",
"unstructured": "Hirsch, J. S. et al. Acute kidney injury in patients hospitalized with COVID-19. Kidney Int. 98, 209–218 (2020).",
"volume": "98",
"year": "2020"
},
{
"DOI": "10.3390/diseases10030053",
"author": "V Chavez-Valencia",
"doi-asserted-by": "publisher",
"first-page": "53",
"journal-title": "Diseases",
"key": "75338_CR35",
"unstructured": "Chavez-Valencia, V., Orizaga-de-la-Cruz, C. & Lagunas-Rangel, F. A. Acute kidney injury in COVID-19 patients: Pathogenesis, clinical characteristics, therapy, and mortality. Diseases 10, 53 (2022).",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1681/ASN.2020040432",
"author": "EA Farkash",
"doi-asserted-by": "publisher",
"first-page": "1683",
"journal-title": "J. Am. Soc. Nephrol.",
"key": "75338_CR36",
"unstructured": "Farkash, E. A., Wilson, A. M. & Jentzen, J. M. Ultrastructural evidence for direct renal infection with SARS-CoV-2. J. Am. Soc. Nephrol. 31, 1683–1687 (2020).",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1038/s41586-020-2012-7",
"author": "P Zhou",
"doi-asserted-by": "publisher",
"first-page": "270",
"journal-title": "Nature",
"key": "75338_CR37",
"unstructured": "Zhou, P. et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579, 270–273 (2020).",
"volume": "579",
"year": "2020"
},
{
"DOI": "10.5527/wjn.v4.i1.74",
"author": "S Mizuiri",
"doi-asserted-by": "publisher",
"first-page": "74",
"journal-title": "World J. Nephrol.",
"key": "75338_CR38",
"unstructured": "Mizuiri, S. & Ohashi, Y. ACE and ACE2 in kidney disease. World J. Nephrol. 4, 74–82 (2015).",
"volume": "4",
"year": "2015"
},
{
"DOI": "10.34067/KID.0002172021",
"author": "S George",
"doi-asserted-by": "publisher",
"first-page": "924",
"journal-title": "Kidney",
"key": "75338_CR39",
"unstructured": "George, S. et al. Evidence for SARS-CoV-2 Spike Protein in the Urine of COVID-19 Patients. Kidney 2, 924–936 (2021).",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.1016/j.bbadis.2022.166496",
"author": "RP Silva-Aguiar",
"doi-asserted-by": "publisher",
"first-page": "166496",
"journal-title": "Biochim. Biophys. Acta Mol. Basis Dis.",
"key": "75338_CR40",
"unstructured": "Silva-Aguiar, R. P. et al. SARS-CoV-2 spike protein inhibits megalin-mediated albumin endocytosis in proximal tubule epithelial cells. Biochim. Biophys. Acta Mol. Basis Dis. 1868, 166496 (2022).",
"volume": "1868",
"year": "2022"
},
{
"DOI": "10.1038/sj.ki.5000298",
"author": "D Biemesderfer",
"doi-asserted-by": "publisher",
"first-page": "1717",
"journal-title": "Kidney Int.",
"key": "75338_CR41",
"unstructured": "Biemesderfer, D. Regulated intramembrane proteolysis of megalin: linking urinary protein and gene regulation in proximal tubule?. Kidney Int. 69, 1717–1721 (2006).",
"volume": "69",
"year": "2006"
},
{
"DOI": "10.1152/ajpcell.00037.2008",
"author": "Y Li",
"doi-asserted-by": "publisher",
"first-page": "C529",
"journal-title": "Am. J. Physiol. Cell Physiol.",
"key": "75338_CR42",
"unstructured": "Li, Y., Cong, R. & Biemesderfer, D. The COOH terminus of megalin regulates gene expression in opossum kidney proximal tubule cells. Am. J. Physiol. Cell Physiol. 295, C529-537 (2008).",
"volume": "295",
"year": "2008"
},
{
"DOI": "10.1093/ndt/gfx321",
"author": "H Fatah",
"doi-asserted-by": "publisher",
"first-page": "934",
"journal-title": "Nephrol. Dial. Transplant.",
"key": "75338_CR43",
"unstructured": "Fatah, H. et al. Reduced proximal tubular expression of protein endocytic receptors in proteinuria is associated with urinary receptor shedding. Nephrol. Dial. Transplant. 33, 934–943 (2018).",
"volume": "33",
"year": "2018"
},
{
"DOI": "10.1038/sj.ki.5000445",
"author": "T Maritzen",
"doi-asserted-by": "publisher",
"first-page": "79",
"journal-title": "Kidney Int.",
"key": "75338_CR44",
"unstructured": "Maritzen, T., Rickheit, G., Schmitt, A. & Jentsch, T. J. Kidney-specific upregulation of vitamin D3 target genes in ClC-5 KO mice. Kidney Int. 70, 79–87 (2006).",
"volume": "70",
"year": "2006"
},
{
"DOI": "10.1186/s12967-020-02488-5",
"author": "Y Xu",
"doi-asserted-by": "publisher",
"first-page": "322",
"journal-title": "J. Transl. Med.",
"key": "75338_CR45",
"unstructured": "Xu, Y. et al. The importance of vitamin d metabolism as a potential prophylactic, immunoregulatory and neuroprotective treatment for COVID-19. J. Transl. Med. 18, 322 (2020).",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.14814/phy2.12331",
"author": "AC de Braganca",
"doi-asserted-by": "publisher",
"first-page": "e12331",
"journal-title": "Physiol. Rep.",
"key": "75338_CR46",
"unstructured": "de Braganca, A. C. et al. Vitamin D deficiency aggravates ischemic acute kidney injury in rats. Physiol. Rep. 3, e12331 (2015).",
"volume": "3",
"year": "2015"
},
{
"DOI": "10.1371/journal.pone.0048652",
"author": "A Tourigny",
"doi-asserted-by": "publisher",
"journal-title": "PLoS One.",
"key": "75338_CR47",
"unstructured": "Tourigny, A. et al. CYP24A1 exacerbated activity during diabetes contributes to kidney tubular apoptosis via caspase-3 increased expression and activation. PLoS One. 7, e48652 (2012).",
"volume": "7",
"year": "2012"
},
{
"DOI": "10.1681/ASN.2009121293",
"author": "M Wolf",
"doi-asserted-by": "publisher",
"first-page": "1427",
"journal-title": "J. Am. Soc. Nephrol.",
"key": "75338_CR48",
"unstructured": "Wolf, M. Forging forward with 10 burning questions on FGF23 in kidney disease. J. Am. Soc. Nephrol. 21, 1427–1435 (2010).",
"volume": "21",
"year": "2010"
},
{
"DOI": "10.1093/ndt/gfp682",
"author": "DE Leaf",
"doi-asserted-by": "publisher",
"first-page": "1335",
"journal-title": "Nephrol. Dial. Transplant.",
"key": "75338_CR49",
"unstructured": "Leaf, D. E., Wolf, M. & Stern, L. Elevated FGF-23 in a patient with rhabdomyolysis-induced acute kidney injury. Nephrol. Dial. Transplant. 25, 1335–1337 (2010).",
"volume": "25",
"year": "2010"
},
{
"DOI": "10.1038/s41598-018-23258-w",
"author": "MA BaSalamah",
"doi-asserted-by": "publisher",
"first-page": "4853",
"journal-title": "Sci. Rep.",
"key": "75338_CR50",
"unstructured": "BaSalamah, M. A. et al. Vitamin D alleviates lead induced renal and testicular injuries by immunomodulatory and antioxidant mechanisms in rats. Sci. Rep. 8, 4853 (2018).",
"volume": "8",
"year": "2018"
},
{
"DOI": "10.1016/j.bbagen.2022.130136",
"author": "A Mazanova",
"doi-asserted-by": "publisher",
"journal-title": "Biochim. Biophys. Acta Gen. Subj.",
"key": "75338_CR51",
"unstructured": "Mazanova, A. et al. The link between vitamin D status and NF-kappaB-associated renal dysfunction in experimental diabetes mellitus. Biochim. Biophys. Acta Gen. Subj. 1866, 130136 (2022).",
"volume": "1866",
"year": "2022"
},
{
"DOI": "10.1038/ki.2008.453",
"author": "D Zehnder",
"doi-asserted-by": "publisher",
"first-page": "1343",
"journal-title": "Kidney Int.",
"key": "75338_CR52",
"unstructured": "Zehnder, D. et al. Reduction of the vitamin D hormonal system in kidney disease is associated with increased renal inflammation. Kidney Int. 74, 1343–1353 (2008).",
"volume": "74",
"year": "2008"
},
{
"DOI": "10.1093/jn/136.11.2754",
"author": "MJ Rowling",
"doi-asserted-by": "publisher",
"first-page": "2754",
"journal-title": "J. Nutr.",
"key": "75338_CR53",
"unstructured": "Rowling, M. J., Kemmis, C. M., Taffany, D. A. & Welsh, J. Megalin-mediated endocytosis of vitamin D binding protein correlates with 25-hydroxycholecalciferol actions in human mammary cells. J. Nutr. 136, 2754–2759 (2006).",
"volume": "136",
"year": "2006"
},
{
"DOI": "10.1016/j.coph.2010.04.001",
"author": "F Baeke",
"doi-asserted-by": "publisher",
"first-page": "482",
"journal-title": "Curr. Opin. Pharmacol.",
"key": "75338_CR54",
"unstructured": "Baeke, F., Takiishi, T., Korf, H., Gysemans, C. & Mathieu, C. Vitamin D: modulator of the immune system. Curr. Opin. Pharmacol. 10, 482–496 (2010).",
"volume": "10",
"year": "2010"
},
{
"DOI": "10.1210/en.2012-1647",
"author": "M Kozai",
"doi-asserted-by": "publisher",
"first-page": "609",
"journal-title": "Endocrinology",
"key": "75338_CR55",
"unstructured": "Kozai, M. et al. Thyroid hormones decrease plasma 1alpha,25-dihydroxyvitamin D levels through transcriptional repression of the renal 25-hydroxyvitamin D3 1alpha-hydroxylase gene (CYP27B1). Endocrinology 154, 609–622 (2013).",
"volume": "154",
"year": "2013"
},
{
"DOI": "10.1124/jpet.107.127209",
"author": "C Daniel",
"doi-asserted-by": "publisher",
"first-page": "23",
"journal-title": "J. Pharmacol. Exp. Ther.",
"key": "75338_CR56",
"unstructured": "Daniel, C., Sartory, N. A., Zahn, N., Radeke, H. H. & Stein, J. M. Immune modulatory treatment of trinitrobenzene sulfonic acid colitis with calcitriol is associated with a change of a T helper (Th) 1/Th17 to a Th2 and regulatory T cell profile. J. Pharmacol. Exp. Ther. 324, 23–33 (2008).",
"volume": "324",
"year": "2008"
},
{
"DOI": "10.3390/biomedicines11092542",
"author": "G Sapartini",
"doi-asserted-by": "publisher",
"first-page": "2542",
"journal-title": "Biomedicines",
"key": "75338_CR57",
"unstructured": "Sapartini, G., Wong, G. W. K., Indrati, A. R., Kartasasmita, C. B. & Setiabudiawan, B. The association between vitamin D, interleukin-4, and interleukin-10 levels and CD23+ expression with bronchial asthma in stunted children. Biomedicines 11, 2542 (2023).",
"volume": "11",
"year": "2023"
},
{
"DOI": "10.1038/labinvest.2013.64",
"author": "Y Jin",
"doi-asserted-by": "publisher",
"first-page": "801",
"journal-title": "Lab. Invest.",
"key": "75338_CR58",
"unstructured": "Jin, Y. et al. Interleukin-10 deficiency aggravates kidney inflammation and fibrosis in the unilateral ureteral obstruction mouse model. Lab. Invest. 93, 801–811 (2013).",
"volume": "93",
"year": "2013"
},
{
"author": "S Azrielant",
"first-page": "510",
"journal-title": "Isr. Med. Assoc. J.",
"key": "75338_CR59",
"unstructured": "Azrielant, S. & Shoenfeld, Y. Vitamin D and the immune system. Isr. Med. Assoc. J. 19, 510–511 (2017).",
"volume": "19",
"year": "2017"
},
{
"DOI": "10.1681/ASN.2021060734",
"author": "B Bowe",
"doi-asserted-by": "publisher",
"first-page": "2851",
"journal-title": "J. Am. Soc. Nephrol.",
"key": "75338_CR60",
"unstructured": "Bowe, B., Xie, Y., Xu, E. & Al-Aly, Z. Kidney outcomes in long COVID. J. Am. Soc. Nephrol. 32, 2851–2862 (2021).",
"volume": "32",
"year": "2021"
},
{
"DOI": "10.34067/KID.0000000000000321",
"author": "LM Curtis",
"doi-asserted-by": "publisher",
"first-page": "160",
"journal-title": "Kidney",
"key": "75338_CR61",
"unstructured": "Curtis, L. M. Sex and gender differences in AKI. Kidney 5, 160–167 (2024).",
"volume": "5",
"year": "2024"
},
{
"DOI": "10.1128/JVI.02012-06",
"author": "PB McCray Jr",
"doi-asserted-by": "publisher",
"first-page": "813",
"journal-title": "J. Virol.",
"key": "75338_CR62",
"unstructured": "McCray, P. B. Jr. et al. Lethal infection of K18-hACE2 mice infected with severe acute respiratory syndrome coronavirus. J. Virol. 81, 813–821 (2007).",
"volume": "81",
"year": "2007"
},
{
"DOI": "10.1073/pnas.2002589117",
"author": "S Matsuyama",
"doi-asserted-by": "publisher",
"first-page": "7001",
"journal-title": "Proc. Natl. Acad. Sci. U. S. A.",
"key": "75338_CR63",
"unstructured": "Matsuyama, S. et al. Enhanced isolation of SARS-CoV-2 by TMPRSS2-expressing cells. Proc. Natl. Acad. Sci. U. S. A. 117, 7001–7003 (2020).",
"volume": "117",
"year": "2020"
},
{
"DOI": "10.1152/ajprenal.00108.2017",
"author": "Y Kurosaki",
"doi-asserted-by": "publisher",
"first-page": "F462",
"journal-title": "Am. J. Physiol. Renal Physiol.",
"key": "75338_CR64",
"unstructured": "Kurosaki, Y. et al. Oxidative stress increases megalin expression in the renal proximal tubules during the normoalbuminuric stage of diabetes mellitus. Am. J. Physiol. Renal Physiol. 314, F462–F470 (2018).",
"volume": "314",
"year": "2018"
},
{
"DOI": "10.1007/s11010-021-04295-y",
"author": "Y Kurosaki",
"doi-asserted-by": "publisher",
"first-page": "689",
"journal-title": "Mol. Cell. Biochem.",
"key": "75338_CR65",
"unstructured": "Kurosaki, Y. et al. In vitro study on effect of bardoxolone methyl on cisplatin-induced cellular senescence in human proximal tubular cells. Mol. Cell. Biochem. 477, 689–699 (2022).",
"volume": "477",
"year": "2022"
}
],
"reference-count": 65,
"references-count": 65,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.nature.com/articles/s41598-024-75338-9"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "SARS-CoV-2 infection causes a decline in renal megalin expression and affects vitamin D metabolism in the kidney of K18-hACE2 mice",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "14"
}
