Zinc and selenium status in coronavirus disease 2019
et al., BioMetals, doi:10.1007/s10534-023-00501-0, Apr 2023
Zinc for COVID-19
2nd treatment shown to reduce risk in
July 2020, now with p = 0.00000028 from 47 studies, recognized in 23 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
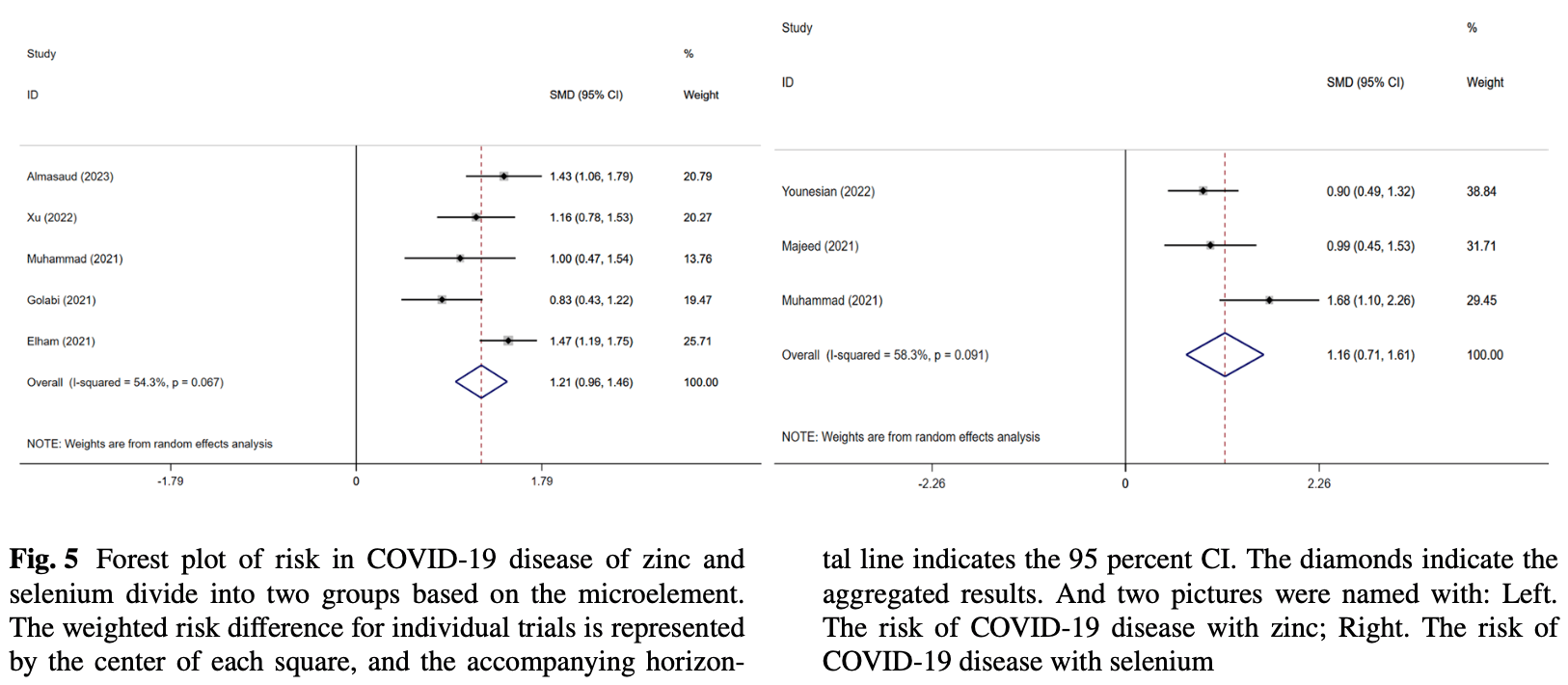
Meta analysis showing increased risk of COVID-19 with zinc deficiency and selenium deficiency. Zinc deficiency was also associated with severity, while there was no significant association for mortality.
Currently there are 47 zinc treatment for COVID-19 studies, showing 30% lower mortality [12‑44%], 40% lower ventilation [2‑63%], 24% lower ICU admission [-5‑46%], 20% lower hospitalization [4‑34%], and 22% fewer cases [-10‑45%].
Study covers selenium and zinc.
1.
Tabatabaeizadeh, S., Zinc supplementation and COVID-19 mortality: a meta-analysis, European Journal of Medical Research, doi:10.1186/s40001-022-00694-z.
2.
Olczak-Pruc et al., The effect of zinc supplementation on the course of COVID-19 – A systematic review and meta-analysis, Annals of Agricultural and Environmental Medicine, doi:10.26444/aaem/155846.
3.
Xie et al., Micronutrient perspective on COVID-19: Umbrella review and reanalysis of meta-analyses, Critical Reviews in Food Science and Nutrition, doi:10.1080/10408398.2023.2174948.
4.
Abuhelwa, Z., Do Zinc Supplements Reduce Mortality in Patients with COVID-19?, Translation: The University of Toledo Journal of Medical Sciences, doi:10.46570/utjms.vol11-2023-749.
5.
Rheingold et al., Zinc Supplementation Associated With a Decrease in Mortality in COVID-19 Patients: A Meta-Analysis, Cureus, doi:10.7759/cureus.40231.
Fan et al., 20 Apr 2023, peer-reviewed, 9 authors.
Contact: qjxue9797@126.com.
Zinc and selenium status in coronavirus disease 2019
BioMetals, doi:10.1007/s10534-023-00501-0
We systematically analyzed and attempted to discuss the possibility that deficiencies of zinc or selenium were associated with the incidence and severity of COVID-19. We searched for published and unpublished articles in PubMed, Embase, Web of Science and Cochrane up to 9 February 2023. And we selected healthy individuals, mild/severe, and even deceased COVID-19 patients to analyze their serum data. Data related to 2319 patients from 20 studies were analyzed. In the mild/severe group, zinc deficiency was associated with the degree of severe disease (SMD = 0.50, 95% CI 0.32-0.68, I 2 = 50.5%) and we got an Egger's test of p = 0.784; but selenium deficiency was not associated with the degree of severe disease (SMD = − 0.03, 95% CI − 0.98-0.93, I 2 = 96.7%). In the surviving/death group, zinc deficiency was not associated with mortality of COVID-19 (SMD = 1.66, 95%CI − 1.42-4.47), nor was selenium (SMD = − 0.16, 95%CI − 1.33-1.01). In the risk group, zinc deficiency was positively associated with the prevalence of COVID-19 (SMD = 1.21, 95% CI 0.96-1.46, I 2 = 54.3%) and selenium deficiency was also positively associated with the prevalence of it (SMD = 1.16, 95% CI 0.71-1.61, I 2 = 58.3%). Currently, serum zinc and selenium deficiencies increase the incidence of COVID-19 and zinc deficiency exacerbates the disease; however, neither zinc nor selenium was associated with mortality in patients with COVID-19. Nevertheless, our conclusions may change when new clinical studies are published.
Supplementary Information The online version contains supplementary material available at https:// doi. org/ 10. 1007/ s10534-023-00501-0. Author contributions QX conceived ideas, analyzed data; LF drafted the manuscript, contributed towards the conception; YC, ZL, JG, XG, YZ, WT, and JZ made great efforts to polish and revise the manuscript. All the authors provided critical review and approved the final manuscript before submission.
Funding
Data availability The datasets generated during and/or analysed during the current study are available in the PubMed, Embase and, WOS repository.
Declarations Conflict of interest The authors declare that there is no conflict of interest.
Ethical Approval Not applicable. Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
References
Abd-Elsalam, Soliman, Esmail, Khalaf, Mostafa et al., Do zinc supplements enhance the clinical efficacy of hydroxychloroquine?: A randomized multicenter trial, Biol Trace Elem Res, doi:10.1007/s12011-020-02512-1
Al-Saleh, Alrushud, Alnuwaysir, Elkhatib, Shoukri et al., Essential metals, vitamins and antioxidant enzyme activities in COVID-19 patients and their potential associations with the disease severity, Biometals, doi:10.1007/s10534-021-00355-4
Almasaud, Chalabi, Arfaj, Qarni, Alkroud et al., Association of serum zinc and inflammatory markers with the severity of covid-19 infection in adult patients, Nutrients, doi:10.3390/nu15020340
Balboni, Zagnoli, Filippini, Fairweather-Tait, Vinceti, Zinc and selenium supplementation in COVID-19 prevention and treatment: a systematic review of the experimental studies, J Trace Elem Med Biol, doi:10.1016/j.jtemb.2022.126956
Bego, Meseldžić, Prnjavorac, Prnjavorac, Marjanović et al., Association of trace element status in COVID-19 patients with disease severity, J Trace Elem Med Biol, doi:10.1016/j.jtemb.2022.127055
Carlucci, Ahuja, Petrilli, Rajagopalan, Jones et al., Zinc sulfate in combination with a zinc ionophore may improve outcomes in hospitalized COVID-19 patients, J Med Microbiol, doi:10.1099/jmm.0.001250
Derwand, Scholz, Zelenko, COVID-19 outpatients: early risk-stratified treatment with zinc plus low-dose hydroxychloroquine and azithromycin: a retrospective case series study, Int J Antimicrob Agents, doi:10.1016/j.ijantimicag.2020.106214
Elham, Azam, Azam, Mostafa, Nasrin et al., Serum vitamin D, calcium, and zinc levels in patients with COVID-19, Clin Nutr ESPEN, doi:10.1016/j.clnesp.2021.03.040
Gammoh, Rink, Zinc in infection and inflammation, Nutrients, doi:10.3390/nu9060624
Golabi, Adelipour, Mobarak, Piri, Seyedtabib et al., The association between vitamin D and zinc status and the progression of clinical symptoms among outpatients infected with SARS-CoV-2 and potentially non-infected participants: a cross-sectional study, Nutrients, doi:10.3390/nu13103368
Gombart, Pierre, Maggini, A review of micronutrients and the immune system-working in harmony to reduce the risk of infection, Nutrients, doi:10.3390/nu12010236
Gouda, Adbelruhman, Elbendary, Alharbi, Alhamrani et al., A comprehensive insight into the role of zinc deficiency in the reninangiotensin and kinin-kallikrein system dysfunctions in COVID-19 patients, Saudi J Biol Sci, doi:10.1016/j.sjbs.2021.03.027
Hoang, Han, A possible application of hinokitiol as a natural zinc ionophore and anti-infective agent for the prevention and treatment of COVID-19 and viral infections, Med Hypotheses, doi:10.1016/j.mehy.2020.110333
Hoffmann, Berry, The influence of selenium on immune responses, Mol Nutr Food Res, doi:10.1002/mnfr.200700330
Hosseini, Moradi, Marhemati, Firouzian, Ildarabadi et al., Comparing serum levels of vitamin d and zinc in novel coronavirusinfected patients and healthy individuals in northeastern Iran, 2020, Infect Dis Clin Pract, doi:10.1097/IPC.0000000000001051
Im, Je, Baek, Chung, Kwon et al., Nutritional status of patients with COVID-19, Int J Infect Dis, doi:10.1016/j.ijid.2020.08.018
Ivanova, Pal, Simonelli, Atanasova, Ventriglia et al., Evaluation of zinc, copper, and Cu: Zn ratio in serum, and their implications in the course of COVID-19, J Trace Elem Med Biol, doi:10.1016/j.jtemb.2022.126944
Jahromi, Tabriz, Togha, The correlation between serum selenium, zinc, and COVID-19 severity: an observational study, BMC Infect Dis, doi:10.1186/s12879-021-06617-3
Jayawardena, Sooriyaarachchi, Chourdakis, Jeewandara, Ranasinghe, Enhancing immunity in viral infections, with special emphasis on COVID-19: review, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.04.015
Keshavarzi, Moore, Najmeddin, Rahmani, Malekzadeh, Quality of drinking water and high incidence rate of esophageal cancer in Golestan province of Iran: a probable link, Environ Geochem Health, doi:10.1007/s10653-011-9377-3
Kieliszek, Lipinski, Selenium supplementation in the prevention of coronavirus infections (COVID-19), Med Hypotheses, doi:10.1016/j.mehy.2020.109878
Kieliszek, Selenium in the prevention of SARS-CoV-2 and other viruses, Biol Trace Elem Res, doi:10.1007/s12011-022-03208-4
Kocak, Ozgeris, Parlak, Kadıoglu, Yuce et al., Evaluation of serum trace element levels and biochemical parameters of COVID-19 patients according to disease severity, Biol Trace Elem Res, doi:10.1007/s12011-021-02946-1
Laing, Petrovic, Lachat, Boevre, Klingenberg et al., Course and survival of COVID-19 patients with comorbidities in relation to the trace element status at hospital admission, Nutrients, doi:10.3390/nu13103304
Luo, Wan, Liu, Tong, Optimally estimating the sample mean from the sample size, median, midrange, and/or mid-quartile range, Stat Methods Med Res, doi:10.1177/0962280216669183
Majeed, Nagabhushanam, Gowda, Mundkur, An exploratory study of selenium status in healthy individuals and in patients with COVID-19 in a south Indian population: the case for adequate selenium status, Nutrition, doi:10.1016/j.nut.2020.111053
Malavolta, Piacenza, Basso, Giacconi, Costarelli et al., Serum copper to zinc ratio: relationship with aging and health status, Mech Ageing Dev, doi:10.1016/j.mad.2015.01.004
Mcguinness, Higgins, Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments, Research Synthesis Methods, doi:10.1002/jrsm.1411
Moghaddam, Heller, Sun, Seelig, Cherkezov et al., Selenium deficiency is associated with mortality risk from COVID-19, Nutrients, doi:10.3390/nu12072098
Muhammad, Kani, Iliya, Muhammad, Binji et al., Deficiency of antioxidants and increased oxidative stress in COVID-19 patients: a cross-sectional comparative study in Jigawa, Open Med, doi:10.1177/2050312121991246
Nouarie, Pourshams, Kamangar, Sotoudeh, Derakhshan et al., Ecologic study of serum selenium and upper gastrointestinal cancers in Iran, World J Gastroentero, doi:10.3748/wjg.v10.i17.2544
Patel, Chinni, El-Khoury, Perera, Neto et al., A pilot double-blind safety and feasibility randomized controlled trial of high-dose intravenous zinc in hospitalized COVID-19 patients, J Med Virol, doi:10.1002/jmv.26895
Pour, Yahyavi, Karimi, Khamaneh, Milani et al., Serum trace elements levels and clinical outcomes among Iranian COVID-19 patients, Int J Infect Dis, doi:10.1016/j.ijid.2021.08.053
Pourbagheri-Sigaroodi, Bashash, Fateh, Abolghasemi, Laboratory findings in COVID-19 diagnosis and prognosis, Clin Chim Acta, doi:10.1016/j.cca.2020.08.019
Rataan, Geary, Zakharia, Rustum, Salem, Potential role of selenium in the treatment of cancer and viral infections, Int J Mol Sci, doi:10.3390/ijms23042215
Rayman, Selenium and human health, Lancet, doi:10.1016/S0140-6736(11)61452-9
Schroeder, Cousins, Interleukin 6 regulates metallothionein gene expression and zinc metabolism in hepatocyte monolayer cultures, Proc Natl Acad Sci U S A, doi:10.1073/pnas.87.8.3137
Shakeri, Azimian, Ghasemzadeh-Moghaddam, Safdari, Haresabadi et al., Evaluation of the relationship between serum levels of zinc, vitamin B12, vitamin D, and clinical outcomes in patients with COVID-19, J Med Virol, doi:10.1002/jmv.27277
Shamblott, Axelman, Wang, Bugg, Littlefield et al., Derivation of pluripotent stem cells from cultured human primordial germ cells, Proc Natl Acad Sci, doi:10.1073/pnas.95.23.13726
Shang, Dong, Ren, Tian, Li et al., The value of clinical parameters in predicting the severity of COVID-19, J Med Virol, doi:10.1002/jmv.26031
Skalny, Rink, Ajsuvakova, Aschner, Gritsenko et al., Zinc and respiratory tract infections: perspectives for COVID-19 (Review), Int J Mol Med, doi:10.3892/ijmm.2020.4575
Skalny, Timashev, Aschner, Aaseth, Chernova et al., Serum zinc, copper, and other biometals are associated with COVID-19 severity markers, Metabolites, doi:10.3390/metabo11040244
Tanumihardjo, Russell, Stephensen, Gannon, Ne et al., Biomarkers of Nutrition for Development (BOND)-Vitamin a review, J Nutr, doi:10.3945/jn.115.229708
Thomas, Patel, Bittel, Wolski, Wang et al., Effect of high-dose zinc and ascorbic acid supplementation vs usual care on symptom length and reduction among ambulatory patients with SARS-CoV-2 infection: the COVID A to Z randomized clinical trial, JAMA Netw Open, doi:10.1001/jamanetworkopen.2021.0369
Voelkle, Gregoriano, Neyer, Koch, Kutz et al., Prevalence of micronutrient deficiencies in patients hospitalized with COVID-19: an observational cohort study, Nutrients, doi:10.3390/nu14091862
Wan, Wang, Liu, Tong, Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range, BMC Med Res Methodol, doi:10.1186/1471-2288-14-135
Wessels, Rolles, Rink, The potential impact of zinc supplementation on COVID-19 pathogenesis, Front Immunol, doi:10.3389/fimmu.2020.01712
Wessels, Rolles, Slusarenko, Rink, Zinc deficiency as a possible risk factor for increased susceptibility and severe progression of corona virus disease 19, Br J Nutr, doi:10.1017/S0007114521000738
Wintergerst, Maggini, Hornig, Immuneenhancing role of vitamin C and zinc and effect on clinical conditions, Ann Nutr Metab, doi:10.1159/000090495
Xu, Liu, Zou, Luo, Wu et al., Hypozincemia in COVID-19 patients correlates with stronger antibody response, Front Immunol, doi:10.3389/fimmu.2021.785599
Yasui, Yasui, Suzuki, Saitou, Yamamoto et al., Analysis of the predictive factors for a critical illness of COVID-19 during treatment-Relationship between serum zinc level and critical illness of COVID-19, Int J Infect Dis, doi:10.1016/j.ijid.2020.09.008
Younesian, Khodabakhshi, Abdolahi, Norouzi, Behnampour et al., Decreased serum selenium levels of covid-19 patients in comparison with healthy individuals, Biol Trace Elem Res, doi:10.1007/s12011-021-02797-w
Zeng, Yang, Yuan, Wang, Cheng, Associations of essential and toxic metals/metalloids in whole blood with both disease severity and mortality in patients with COVID-19, FASEB J, doi:10.1096/fj.202002346RR
Zhang, Saad, Taylor, Rayman, Selenium and selenoproteins in viral infection with potential relevance to COVID-19, Redox Biol, doi:10.1016/j.redox.2020.101715
Zhang, Taylor, Bennett, Saad, Rayman, Association between regional selenium status and reported outcome of COVID-19 cases in China, Am J Clin Nutr, doi:10.1093/ajcn/nqaa095
DOI record:
{
"DOI": "10.1007/s10534-023-00501-0",
"ISSN": [
"0966-0844",
"1572-8773"
],
"URL": "http://dx.doi.org/10.1007/s10534-023-00501-0",
"alternative-id": [
"501"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "28 November 2022"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "3 April 2023"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "20 April 2023"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Conflict of interest",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "The authors declare that there is no conflict of interest."
},
{
"group": {
"label": "Ethical Approval",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "Not applicable."
},
{
"label": "Free to read",
"name": "free",
"value": "This content has been made available to all."
}
],
"author": [
{
"affiliation": [],
"family": "Fan",
"given": "Liding",
"sequence": "first"
},
{
"affiliation": [],
"family": "Cui",
"given": "Yanshuo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Liu",
"given": "Zonghao",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Guo",
"given": "Jiayue",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gong",
"given": "Xiaohui",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Yunfei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tang",
"given": "Weihao",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhao",
"given": "Jiahe",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Xue",
"given": "Qingjie",
"sequence": "additional"
}
],
"container-title": "BioMetals",
"container-title-short": "Biometals",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2023,
4,
20
]
],
"date-time": "2023-04-20T12:22:16Z",
"timestamp": 1681993336000
},
"deposited": {
"date-parts": [
[
2023,
4,
20
]
],
"date-time": "2023-04-20T14:46:27Z",
"timestamp": 1682001987000
},
"funder": [
{
"award": [
"no. 202110443046",
"no. 202110443046",
"no. 202110443046",
"no. 202110443046"
],
"name": "National Innovation and Entrepreneurship Training Program for College Students"
}
],
"indexed": {
"date-parts": [
[
2023,
4,
21
]
],
"date-time": "2023-04-21T06:38:30Z",
"timestamp": 1682059110725
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
4,
20
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.springernature.com/gp/researchers/text-and-data-mining",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
4,
20
]
],
"date-time": "2023-04-20T00:00:00Z",
"timestamp": 1681948800000
}
},
{
"URL": "https://www.springernature.com/gp/researchers/text-and-data-mining",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
4,
20
]
],
"date-time": "2023-04-20T00:00:00Z",
"timestamp": 1681948800000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1007/s10534-023-00501-0.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1007/s10534-023-00501-0/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1007/s10534-023-00501-0.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1007",
"published": {
"date-parts": [
[
2023,
4,
20
]
]
},
"published-online": {
"date-parts": [
[
2023,
4,
20
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1007/s12011-020-02512-1",
"author": "S Abd-Elsalam",
"doi-asserted-by": "publisher",
"first-page": "3642",
"issue": "10",
"journal-title": "Biol Trace Elem Res",
"key": "501_CR1",
"unstructured": "Abd-Elsalam S, Soliman S, Esmail ES, Khalaf M, Mostafa EF, Medhat MA, Ahmed OA, El Ghafar MSA, Alboraie M, Hassany SM (2021) Do zinc supplements enhance the clinical efficacy of hydroxychloroquine?: A randomized multicenter trial. Biol Trace Elem Res 199(10):3642–3646. https://doi.org/10.1007/s12011-020-02512-1",
"volume": "199",
"year": "2021"
},
{
"DOI": "10.3390/nu15020340",
"author": "AS Almasaud",
"doi-asserted-by": "publisher",
"first-page": "340",
"issue": "2",
"journal-title": "Nutrients",
"key": "501_CR2",
"unstructured": "Almasaud AS, Chalabi J, Arfaj AA, Qarni AA, Alkroud A, Nagoor Z, Akhtar S, Iqbal J (2023) Association of serum zinc and inflammatory markers with the severity of covid-19 infection in adult patients. Nutrients 15(2):340. https://doi.org/10.3390/nu15020340",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.1007/s10534-021-00355-4",
"author": "I Al-Saleh",
"doi-asserted-by": "publisher",
"first-page": "125",
"issue": "1",
"journal-title": "Biometals",
"key": "501_CR3",
"unstructured": "Al-Saleh I, Alrushud N, Alnuwaysir H, Elkhatib R, Shoukri M, Aldayel F, Bakheet R, Almozaini M (2022) Essential metals, vitamins and antioxidant enzyme activities in COVID-19 patients and their potential associations with the disease severity. Biometals 35(1):125–145. https://doi.org/10.1007/s10534-021-00355-4",
"volume": "35",
"year": "2022"
},
{
"DOI": "10.1016/j.jtemb.2022.126956",
"author": "E Balboni",
"doi-asserted-by": "publisher",
"first-page": "126956",
"journal-title": "J Trace Elem Med Biol",
"key": "501_CR4",
"unstructured": "Balboni E, Zagnoli F, Filippini T, Fairweather-Tait SJ, Vinceti M (2022) Zinc and selenium supplementation in COVID-19 prevention and treatment: a systematic review of the experimental studies. J Trace Elem Med Biol 71:126956. https://doi.org/10.1016/j.jtemb.2022.126956",
"volume": "71",
"year": "2022"
},
{
"DOI": "10.1016/j.jtemb.2022.127055",
"author": "T Bego",
"doi-asserted-by": "publisher",
"first-page": "127055",
"journal-title": "J Trace Elem Med Biol",
"key": "501_CR5",
"unstructured": "Bego T, Meseldžić N, Prnjavorac B, Prnjavorac L, Marjanović D, Azevedo R, Pinto E, Duro M, Couto C, Almeida A (2022) Association of trace element status in COVID-19 patients with disease severity. J Trace Elem Med Biol 74:127055. https://doi.org/10.1016/j.jtemb.2022.127055",
"volume": "74",
"year": "2022"
},
{
"DOI": "10.1099/jmm.0.001250",
"author": "PM Carlucci",
"doi-asserted-by": "publisher",
"first-page": "1228",
"issue": "10",
"journal-title": "J Med Microbiol",
"key": "501_CR6",
"unstructured": "Carlucci PM, Ahuja T, Petrilli C, Rajagopalan H, Jones S, Rahimian J (2020) Zinc sulfate in combination with a zinc ionophore may improve outcomes in hospitalized COVID-19 patients. J Med Microbiol 69(10):1228–1234. https://doi.org/10.1099/jmm.0.001250",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1016/j.ijantimicag.2020.106214",
"author": "R Derwand",
"doi-asserted-by": "publisher",
"first-page": "106214",
"issue": "6",
"journal-title": "Int J Antimicrob Agents",
"key": "501_CR7",
"unstructured": "Derwand R, Scholz M, Zelenko V (2020) COVID-19 outpatients: early risk-stratified treatment with zinc plus low-dose hydroxychloroquine and azithromycin: a retrospective case series study. Int J Antimicrob Agents 56(6):106214. https://doi.org/10.1016/j.ijantimicag.2020.106214",
"volume": "56",
"year": "2020"
},
{
"DOI": "10.3390/nu13103304",
"author": "G Du Laing",
"doi-asserted-by": "publisher",
"first-page": "3304",
"issue": "10",
"journal-title": "Nutrients",
"key": "501_CR8",
"unstructured": "Du Laing G, Petrovic M, Lachat C, De Boevre M, Klingenberg GJ, Sun Q, De Saeger S, De Clercq J, Ide L, Vandekerckhove L, Schomburg L (2021) Course and survival of COVID-19 patients with comorbidities in relation to the trace element status at hospital admission. Nutrients 13(10):3304. https://doi.org/10.3390/nu13103304",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1016/j.clnesp.2021.03.040",
"author": "AS Elham",
"doi-asserted-by": "publisher",
"first-page": "276",
"journal-title": "Clin Nutr ESPEN",
"key": "501_CR9",
"unstructured": "Elham AS, Azam K, Azam J, Mostafa L, Nasrin B, Marzieh N (2021) Serum vitamin D, calcium, and zinc levels in patients with COVID-19. Clin Nutr ESPEN 43:276–282. https://doi.org/10.1016/j.clnesp.2021.03.040",
"volume": "43",
"year": "2021"
},
{
"DOI": "10.3390/nu9060624",
"author": "NZ Gammoh",
"doi-asserted-by": "publisher",
"first-page": "624",
"issue": "6",
"journal-title": "Nutrients",
"key": "501_CR10",
"unstructured": "Gammoh NZ, Rink L (2017) Zinc in infection and inflammation. Nutrients 9(6):624. https://doi.org/10.3390/nu9060624",
"volume": "9",
"year": "2017"
},
{
"DOI": "10.3390/nu13103368",
"author": "S Golabi",
"doi-asserted-by": "publisher",
"first-page": "3368",
"issue": "10",
"journal-title": "Nutrients",
"key": "501_CR11",
"unstructured": "Golabi S, Adelipour M, Mobarak S, Piri M, Seyedtabib M, Bagheri R, Suzuki K, Ashtary-Larky D, Maghsoudi F, Naghashpour M (2021) The association between vitamin D and zinc status and the progression of clinical symptoms among outpatients infected with SARS-CoV-2 and potentially non-infected participants: a cross-sectional study. Nutrients 13(10):3368. https://doi.org/10.3390/nu13103368",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.3390/nu12010236",
"author": "AF Gombart",
"doi-asserted-by": "publisher",
"first-page": "236",
"issue": "1",
"journal-title": "Nutrients",
"key": "501_CR12",
"unstructured": "Gombart AF, Pierre A, Maggini S (2020) A review of micronutrients and the immune system-working in harmony to reduce the risk of infection. Nutrients 12(1):236. https://doi.org/10.3390/nu12010236",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/j.sjbs.2021.03.027",
"author": "AS Gouda",
"doi-asserted-by": "publisher",
"first-page": "3540",
"issue": "6",
"journal-title": "Saudi J Biol Sci",
"key": "501_CR13",
"unstructured": "Gouda AS, Adbelruhman FG, Elbendary RN, Alharbi FA, Alhamrani SQ, Mégarbane B (2021) A comprehensive insight into the role of zinc deficiency in the renin-angiotensin and kinin-kallikrein system dysfunctions in COVID-19 patients. Saudi J Biol Sci 28(6):3540–3547. https://doi.org/10.1016/j.sjbs.2021.03.027",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.1016/j.mehy.2020.110333",
"author": "BX Hoang",
"doi-asserted-by": "publisher",
"first-page": "110333",
"journal-title": "Med Hypotheses",
"key": "501_CR14",
"unstructured": "Hoang BX, Han B (2020) A possible application of hinokitiol as a natural zinc ionophore and anti-infective agent for the prevention and treatment of COVID-19 and viral infections. Med Hypotheses 145:110333. https://doi.org/10.1016/j.mehy.2020.110333",
"volume": "145",
"year": "2020"
},
{
"DOI": "10.1002/mnfr.200700330",
"author": "PR Hoffmann",
"doi-asserted-by": "publisher",
"first-page": "1273",
"issue": "11",
"journal-title": "Mol Nutr Food Res",
"key": "501_CR15",
"unstructured": "Hoffmann PR, Berry MJ (2008) The influence of selenium on immune responses. Mol Nutr Food Res 52(11):1273–1280. https://doi.org/10.1002/mnfr.200700330",
"volume": "52",
"year": "2008"
},
{
"DOI": "10.1097/IPC.0000000000001051",
"author": "SJ Hosseini",
"doi-asserted-by": "publisher",
"first-page": "e390",
"issue": "6",
"journal-title": "Infect Dis Clin Pract",
"key": "501_CR16",
"unstructured": "Hosseini SJ, Moradi B, Marhemati M, Firouzian AA, Ildarabadi E, Abedi A, Firooz M (2021) Comparing serum levels of vitamin d and zinc in novel coronavirus-infected patients and healthy individuals in northeastern Iran, 2020. Infect Dis Clin Pract 29(6):e390–e394. https://doi.org/10.1097/IPC.0000000000001051",
"volume": "29",
"year": "2021"
},
{
"DOI": "10.1016/j.ijid.2020.08.018",
"author": "JH Im",
"doi-asserted-by": "publisher",
"first-page": "390",
"journal-title": "Int J Infect Dis",
"key": "501_CR17",
"unstructured": "Im JH, Je YS, Baek J, Chung MH, Kwon HY, Lee JS (2020) Nutritional status of patients with COVID-19. Int J Infect Dis 100:390–393. https://doi.org/10.1016/j.ijid.2020.08.018",
"volume": "100",
"year": "2020"
},
{
"DOI": "10.1016/j.jtemb.2022.126944",
"author": "ID Ivanova",
"doi-asserted-by": "publisher",
"first-page": "126944",
"journal-title": "J Trace Elem Med Biol",
"key": "501_CR18",
"unstructured": "Ivanova ID, Pal A, Simonelli I, Atanasova B, Ventriglia M, Rongioletti M, Squitti R (2022) Evaluation of zinc, copper, and Cu: Zn ratio in serum, and their implications in the course of COVID-19. J Trace Elem Med Biol 71:126944. https://doi.org/10.1016/j.jtemb.2022.126944",
"volume": "71",
"year": "2022"
},
{
"DOI": "10.1186/s12879-021-06617-3",
"author": "SR Jahromi",
"doi-asserted-by": "publisher",
"first-page": "899",
"journal-title": "BMC Infect Dis",
"key": "501_CR19",
"unstructured": "Jahromi SR, Tabriz HM, Togha M et al (2021) The correlation between serum selenium, zinc, and COVID-19 severity: an observational study. BMC Infect Dis 21:899. https://doi.org/10.1186/s12879-021-06617-3",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2020.04.015",
"author": "R Jayawardena",
"doi-asserted-by": "publisher",
"first-page": "367",
"issue": "4",
"journal-title": "Diabetes Metab Syndr",
"key": "501_CR20",
"unstructured": "Jayawardena R, Sooriyaarachchi P, Chourdakis M, Jeewandara C, Ranasinghe P (2020) Enhancing immunity in viral infections, with special emphasis on COVID-19: a review. Diabetes Metab Syndr 14(4):367–382. https://doi.org/10.1016/j.dsx.2020.04.015",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1007/s10653-011-9377-3",
"author": "B Keshavarzi",
"doi-asserted-by": "publisher",
"first-page": "15",
"issue": "1",
"journal-title": "Environ Geochem Health",
"key": "501_CR21",
"unstructured": "Keshavarzi B, Moore F, Najmeddin A, Rahmani F, Malekzadeh A (2012) Quality of drinking water and high incidence rate of esophageal cancer in Golestan province of Iran: a probable link. Environ Geochem Health 34(1):15–26. https://doi.org/10.1007/s10653-011-9377-3",
"volume": "34",
"year": "2012"
},
{
"DOI": "10.1007/s12011-022-03208-4",
"author": "M Kieliszek",
"doi-asserted-by": "publisher",
"first-page": "655",
"issue": "2",
"journal-title": "Biol Trace Elem Res",
"key": "501_CR22",
"unstructured": "Kieliszek M (2023) Selenium in the prevention of SARS-CoV-2 and other viruses. Biol Trace Elem Res 201(2):655–662. https://doi.org/10.1007/s12011-022-03208-4",
"volume": "201",
"year": "2023"
},
{
"DOI": "10.1016/j.mehy.2020.109878",
"author": "M Kieliszek",
"doi-asserted-by": "publisher",
"first-page": "109878",
"journal-title": "Med Hypotheses",
"key": "501_CR23",
"unstructured": "Kieliszek M, Lipinski B (2020) Selenium supplementation in the prevention of coronavirus infections (COVID-19). Med Hypotheses 143:109878. https://doi.org/10.1016/j.mehy.2020.109878",
"volume": "143",
"year": "2020"
},
{
"DOI": "10.1007/s12011-021-02946-1",
"author": "OF Kocak",
"doi-asserted-by": "publisher",
"first-page": "3138",
"issue": "7",
"journal-title": "Biol Trace Elem Res",
"key": "501_CR24",
"unstructured": "Kocak OF, Ozgeris FB, Parlak E, Kadıoglu Y, Yuce N, Yaman ME, Bakan E (2022) Evaluation of serum trace element levels and biochemical parameters of COVID-19 patients according to disease severity. Biol Trace Elem Res 200(7):3138–3146. https://doi.org/10.1007/s12011-021-02946-1",
"volume": "200",
"year": "2022"
},
{
"DOI": "10.1177/0962280216669183",
"author": "D Luo",
"doi-asserted-by": "publisher",
"first-page": "1785",
"issue": "6",
"journal-title": "Stat Methods Med Res",
"key": "501_CR25",
"unstructured": "Luo D, Wan X, Liu J, Tong T (2018) Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res 27(6):1785–1805. https://doi.org/10.1177/0962280216669183",
"volume": "27",
"year": "2018"
},
{
"DOI": "10.1016/j.nut.2020.111053",
"author": "M Majeed",
"doi-asserted-by": "publisher",
"first-page": "111053",
"journal-title": "Nutrition",
"key": "501_CR26",
"unstructured": "Majeed M, Nagabhushanam K, Gowda S, Mundkur L (2021) An exploratory study of selenium status in healthy individuals and in patients with COVID-19 in a south Indian population: the case for adequate selenium status. Nutrition 82:111053. https://doi.org/10.1016/j.nut.2020.111053",
"volume": "82",
"year": "2021"
},
{
"DOI": "10.1016/j.mad.2015.01.004",
"author": "M Malavolta",
"doi-asserted-by": "publisher",
"first-page": "93",
"journal-title": "Mech Ageing Dev",
"key": "501_CR27",
"unstructured": "Malavolta M, Piacenza F, Basso A, Giacconi R, Costarelli L, Mocchegiani E (2015) Serum copper to zinc ratio: relationship with aging and health status. Mech Ageing Dev 151:93–100. https://doi.org/10.1016/j.mad.2015.01.004",
"volume": "151",
"year": "2015"
},
{
"DOI": "10.1002/jrsm.1411",
"author": "LA McGuinness",
"doi-asserted-by": "publisher",
"first-page": "55",
"journal-title": "Research Synthesis Methods",
"key": "501_CR28",
"unstructured": "McGuinness LA, Higgins JP (2020) Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Research Synthesis Methods 12:55–61. https://doi.org/10.1002/jrsm.1411",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.3390/nu12072098",
"author": "A Moghaddam",
"doi-asserted-by": "publisher",
"first-page": "2098",
"issue": "7",
"journal-title": "Nutrients",
"key": "501_CR29",
"unstructured": "Moghaddam A, Heller RA, Sun Q, Seelig J, Cherkezov A, Seibert L, Hackler J, Seemann P, Diegmann J, Pilz M, Bachmann M, Minich WB, Schomburg L (2020) Selenium deficiency is associated with mortality risk from COVID-19. Nutrients 12(7):2098. https://doi.org/10.3390/nu12072098",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1177/2050312121991246",
"author": "Y Muhammad",
"doi-asserted-by": "publisher",
"journal-title": "Northwestern Nigeria SAGE Open Med",
"key": "501_CR30",
"unstructured": "Muhammad Y, Kani YA, Iliya S, Muhammad JB, Binji A, El-Fulaty Ahmad A, Kabir MB, Umar Bindawa K, Ahmed A (2021) Deficiency of antioxidants and increased oxidative stress in COVID-19 patients: a cross-sectional comparative study in Jigawa. Northwestern Nigeria SAGE Open Med. https://doi.org/10.1177/2050312121991246",
"year": "2021"
},
{
"DOI": "10.3748/wjg.v10.i17.2544",
"author": "M Nouarie",
"doi-asserted-by": "publisher",
"first-page": "2544",
"issue": "17",
"journal-title": "World J Gastroentero",
"key": "501_CR31",
"unstructured": "Nouarie M, Pourshams A, Kamangar F, Sotoudeh M, Derakhshan MH, Akbari MR, Fakheri H, Zahedi MJ, Caldwell K, Abnet CC, Taylor PR, Malekzadeh R, Dawsey SM (2004) Ecologic study of serum selenium and upper gastrointestinal cancers in Iran. World J Gastroentero 10(17):2544–2546. https://doi.org/10.3748/wjg.v10.i17.2544",
"volume": "10",
"year": "2004"
},
{
"DOI": "10.1002/jmv.26895",
"author": "O Patel",
"doi-asserted-by": "publisher",
"first-page": "3261",
"issue": "5",
"journal-title": "J Med Virol",
"key": "501_CR32",
"unstructured": "Patel O, Chinni V, El-Khoury J, Perera M, Neto AS, McDonald C, See E, Jones D, Bolton D, Bellomo R, Trubiano J, Ischia J (2021) A pilot double-blind safety and feasibility randomized controlled trial of high-dose intravenous zinc in hospitalized COVID-19 patients. J Med Virol 93(5):3261–3267. https://doi.org/10.1002/jmv.26895",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1016/j.ijid.2021.08.053",
"author": "OB Pour",
"doi-asserted-by": "publisher",
"first-page": "164",
"journal-title": "Int J Infect Dis",
"key": "501_CR33",
"unstructured": "Pour OB, Yahyavi Y, Karimi A, Khamaneh AM, Milani M, Khalili M, Sharifi A (2021) Serum trace elements levels and clinical outcomes among Iranian COVID-19 patients. Int J Infect Dis 111:164–168. https://doi.org/10.1016/j.ijid.2021.08.053",
"volume": "111",
"year": "2021"
},
{
"DOI": "10.1016/j.cca.2020.08.019",
"author": "A Pourbagheri-Sigaroodi",
"doi-asserted-by": "publisher",
"first-page": "475",
"journal-title": "Clin Chim Acta",
"key": "501_CR34",
"unstructured": "Pourbagheri-Sigaroodi A, Bashash D, Fateh F, Abolghasemi H (2020) Laboratory findings in COVID-19 diagnosis and prognosis. Clin Chim Acta 510:475–482. https://doi.org/10.1016/j.cca.2020.08.019",
"volume": "510",
"year": "2020"
},
{
"DOI": "10.3390/ijms23042215",
"author": "AO Rataan",
"doi-asserted-by": "publisher",
"first-page": "2215",
"issue": "4",
"journal-title": "Int J Mol Sci",
"key": "501_CR35",
"unstructured": "Rataan AO, Geary SM, Zakharia Y, Rustum YM, Salem AK (2022) Potential role of selenium in the treatment of cancer and viral infections. Int J Mol Sci 23(4):2215. https://doi.org/10.3390/ijms23042215",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.1016/S0140-6736(11)61452-9",
"author": "MP Rayman",
"doi-asserted-by": "publisher",
"first-page": "9822",
"journal-title": "Lancet",
"key": "501_CR36",
"unstructured": "Rayman MP (2012) Selenium and human health. Lancet 379:9822. https://doi.org/10.1016/S0140-6736(11)61452-9",
"volume": "379",
"year": "2012"
},
{
"DOI": "10.1073/pnas.87.8.3137",
"author": "JJ Schroeder",
"doi-asserted-by": "publisher",
"first-page": "3137",
"issue": "8",
"journal-title": "Proc Natl Acad Sci U S A",
"key": "501_CR37",
"unstructured": "Schroeder JJ, Cousins RJ (1990) Interleukin 6 regulates metallothionein gene expression and zinc metabolism in hepatocyte monolayer cultures. Proc Natl Acad Sci U S A 87(8):3137–3141. https://doi.org/10.1073/pnas.87.8.3137",
"volume": "87",
"year": "1990"
},
{
"DOI": "10.1002/jmv.27277",
"author": "H Shakeri",
"doi-asserted-by": "publisher",
"first-page": "141",
"issue": "1",
"journal-title": "J Med Virol",
"key": "501_CR38",
"unstructured": "Shakeri H, Azimian A, Ghasemzadeh-Moghaddam H, Safdari M, Haresabadi M, Daneshmand T, Namdar Ahmadabad H (2022) Evaluation of the relationship between serum levels of zinc, vitamin B12, vitamin D, and clinical outcomes in patients with COVID-19. J Med Virol 94(1):141–146. https://doi.org/10.1002/jmv.27277",
"volume": "94",
"year": "2022"
},
{
"DOI": "10.1073/pnas.95.23.13726",
"author": "MJ Shamblott",
"doi-asserted-by": "publisher",
"first-page": "13726",
"issue": "23",
"journal-title": "Proc Natl Acad Sci USA",
"key": "501_CR39",
"unstructured": "Shamblott MJ, Axelman J, Wang S, Bugg EM, Littlefield JW, Donovan PJ, Blumenthal PD, Huggins GR, Gearhart JD (1998) Derivation of pluripotent stem cells from cultured human primordial germ cells. Proc Natl Acad Sci USA 95(23):13726–13731. https://doi.org/10.1073/pnas.95.23.13726",
"volume": "95",
"year": "1998"
},
{
"DOI": "10.1002/jmv.26031",
"author": "W Shang",
"doi-asserted-by": "publisher",
"first-page": "2188",
"issue": "10",
"journal-title": "J Med Virol",
"key": "501_CR40",
"unstructured": "Shang W, Dong J, Ren Y, Tian M, Li W, Hu J, Li Y (2020) The value of clinical parameters in predicting the severity of COVID-19. J Med Virol 92(10):2188–2192. https://doi.org/10.1002/jmv.26031",
"volume": "92",
"year": "2020"
},
{
"DOI": "10.3892/ijmm.2020.4575",
"author": "AV Skalny",
"doi-asserted-by": "publisher",
"first-page": "17",
"issue": "1",
"journal-title": "Int J Mol Med",
"key": "501_CR41",
"unstructured": "Skalny AV, Rink L, Ajsuvakova OP, Aschner M, Gritsenko VA, Alekseenko SI, Svistunov AA, Petrakis D, Spandidos DA, Aaseth J, Tsatsakis A, Tinkov AA (2020) Zinc and respiratory tract infections: perspectives for COVID-19 (Review). Int J Mol Med 46(1):17–26. https://doi.org/10.3892/ijmm.2020.4575",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.3390/metabo11040244",
"author": "AV Skalny",
"doi-asserted-by": "publisher",
"first-page": "244",
"issue": "4",
"journal-title": "Metabolites",
"key": "501_CR42",
"unstructured": "Skalny AV, Timashev PS, Aschner M, Aaseth J, Chernova LN, Belyaev VE, Grabeklis AR, Notova SV, Lobinski R, Tsatsakis A, Svistunov AA, Fomin VV, Tinkov AA, Glybochko PV (2021) Serum zinc, copper, and other biometals are associated with COVID-19 severity markers. Metabolites 11(4):244. https://doi.org/10.3390/metabo11040244",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.3945/jn.115.229708",
"author": "SA Tanumihardjo",
"doi-asserted-by": "publisher",
"first-page": "9",
"journal-title": "J Nutr",
"key": "501_CR43",
"unstructured": "Tanumihardjo SA, Russell RM, Stephensen CB, Gannon BM, Craft NE, Haskell MJ, Lietz G, Schulze K, Raiten DJ (2016) Biomarkers of Nutrition for Development (BOND)—Vitamin a review. J Nutr 146:9. https://doi.org/10.3945/jn.115.229708",
"volume": "146",
"year": "2016"
},
{
"DOI": "10.1001/jamanetworkopen.2021.0369",
"author": "S Thomas",
"doi-asserted-by": "publisher",
"first-page": "e210369",
"issue": "2",
"journal-title": "JAMA Netw Open",
"key": "501_CR44",
"unstructured": "Thomas S, Patel D, Bittel B, Wolski K, Wang Q, Kumar A, Il’Giovine ZJ, Mehra R, McWilliams C, Nissen SE, Desai MY (2021) Effect of high-dose zinc and ascorbic acid supplementation vs usual care on symptom length and reduction among ambulatory patients with SARS-CoV-2 infection: the COVID A to Z randomized clinical trial. JAMA Netw Open 4(2):e210369. https://doi.org/10.1001/jamanetworkopen.2021.0369",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.3390/nu14091862",
"author": "M Voelkle",
"doi-asserted-by": "publisher",
"first-page": "1862",
"issue": "9",
"journal-title": "Nutrients",
"key": "501_CR45",
"unstructured": "Voelkle M, Gregoriano C, Neyer P, Koch D, Kutz A, Bernasconi L, Conen A, Mueller B, Schuetz P (2022) Prevalence of micronutrient deficiencies in patients hospitalized with COVID-19: an observational cohort study. Nutrients 14(9):1862. https://doi.org/10.3390/nu14091862",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1186/1471-2288-14-135",
"author": "X Wan",
"doi-asserted-by": "publisher",
"first-page": "135",
"journal-title": "BMC Med Res Methodol",
"key": "501_CR46",
"unstructured": "Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135. https://doi.org/10.1186/1471-2288-14-135",
"volume": "14",
"year": "2014"
},
{
"DOI": "10.3389/fimmu.2020.01712",
"author": "I Wessels",
"doi-asserted-by": "publisher",
"first-page": "1712",
"journal-title": "Front Immunol",
"key": "501_CR47",
"unstructured": "Wessels I, Rolles B, Rink L (2020) The potential impact of zinc supplementation on COVID-19 pathogenesis. Front Immunol 11:1712. https://doi.org/10.3389/fimmu.2020.01712",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1017/S0007114521000738",
"author": "I Wessels",
"doi-asserted-by": "publisher",
"first-page": "214",
"issue": "2",
"journal-title": "Br J Nutr",
"key": "501_CR48",
"unstructured": "Wessels I, Rolles B, Slusarenko AJ, Rink L (2022) Zinc deficiency as a possible risk factor for increased susceptibility and severe progression of corona virus disease 19. Br J Nutr 127(2):214–232. https://doi.org/10.1017/S0007114521000738",
"volume": "127",
"year": "2022"
},
{
"DOI": "10.1159/000090495",
"author": "ES Wintergerst",
"doi-asserted-by": "publisher",
"first-page": "85",
"issue": "2",
"journal-title": "Ann Nutr Metab",
"key": "501_CR49",
"unstructured": "Wintergerst ES, Maggini S, Hornig DH (2006) Immune-enhancing role of vitamin C and zinc and effect on clinical conditions. Ann Nutr Metab 50(2):85–94. https://doi.org/10.1159/000090495",
"volume": "50",
"year": "2006"
},
{
"DOI": "10.3389/fimmu.2021.785599",
"author": "W Xu",
"doi-asserted-by": "publisher",
"first-page": "785599",
"journal-title": "Front Immunol",
"key": "501_CR50",
"unstructured": "Xu W, Liu Y, Zou X, Luo H, Wu W, Xia J, Chan MTV, Fang S, Shu Y, Wu WKK, Zhang L (2022) Hypozincemia in COVID-19 patients correlates with stronger antibody response. Front Immunol 12:785599. https://doi.org/10.3389/fimmu.2021.785599",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1016/j.ijid.2020.09.008",
"author": "Y Yasui",
"doi-asserted-by": "publisher",
"first-page": "230",
"journal-title": "Int J Infect Dis",
"key": "501_CR51",
"unstructured": "Yasui Y, Yasui H, Suzuki K, Saitou T, Yamamoto Y, Ishizaka T, Nishida K, Yoshihara S, Gohma I, Ogawa Y (2020) Analysis of the predictive factors for a critical illness of COVID-19 during treatment—Relationship between serum zinc level and critical illness of COVID-19. Int J Infect Dis 100:230–236. https://doi.org/10.1016/j.ijid.2020.09.008",
"volume": "100",
"year": "2020"
},
{
"DOI": "10.1007/s12011-021-02797-w",
"author": "O Younesian",
"doi-asserted-by": "publisher",
"first-page": "1562",
"issue": "4",
"journal-title": "Biol Trace Elem Res",
"key": "501_CR52",
"unstructured": "Younesian O, Khodabakhshi B, Abdolahi N, Norouzi A, Behnampour N, Hosseinzadeh S, Alarzi SSH, Joshaghani H (2022) Decreased serum selenium levels of covid-19 patients in comparison with healthy individuals. Biol Trace Elem Res 200(4):1562–1567. https://doi.org/10.1007/s12011-021-02797-w",
"volume": "200",
"year": "2022"
},
{
"DOI": "10.1096/fj.202002346RR",
"author": "HL Zeng",
"doi-asserted-by": "publisher",
"first-page": "e21392",
"issue": "3",
"journal-title": "FASEB J",
"key": "501_CR53",
"unstructured": "Zeng HL, Yang Q, Yuan P, Wang X, Cheng L (2021) Associations of essential and toxic metals/metalloids in whole blood with both disease severity and mortality in patients with COVID-19. FASEB J 35(3):e21392. https://doi.org/10.1096/fj.202002346RR",
"volume": "35",
"year": "2021"
},
{
"DOI": "10.1016/j.redox.2020.101715",
"author": "J Zhang",
"doi-asserted-by": "publisher",
"first-page": "101715",
"issue": "37",
"journal-title": "Redox Biol",
"key": "501_CR54",
"unstructured": "Zhang J, Saad R, Taylor EW, Rayman MP (2020a) Selenium and selenoproteins in viral infection with potential relevance to COVID-19. Redox Biol 2020(37):101715. https://doi.org/10.1016/j.redox.2020.101715",
"volume": "2020",
"year": "2020"
},
{
"DOI": "10.1093/ajcn/nqaa095",
"author": "J Zhang",
"doi-asserted-by": "publisher",
"first-page": "1297",
"issue": "6",
"journal-title": "Am J Clin Nutr",
"key": "501_CR55",
"unstructured": "Zhang J, Taylor EW, Bennett K, Saad R, Rayman MP (2020b) Association between regional selenium status and reported outcome of COVID-19 cases in China. Am J Clin Nutr 111(6):1297–1299. https://doi.org/10.1093/ajcn/nqaa095",
"volume": "111",
"year": "2020"
}
],
"reference-count": 55,
"references-count": 55,
"relation": {},
"resource": {
"primary": {
"URL": "https://link.springer.com/10.1007/s10534-023-00501-0"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Metals and Alloys",
"General Agricultural and Biological Sciences",
"General Biochemistry, Genetics and Molecular Biology",
"Biomaterials"
],
"subtitle": [],
"title": "Zinc and selenium status in coronavirus disease 2019",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy"
}
