Association of Trace Element Status in COVID-19 Patients with Disease Severity
et al., Journal of Trace Elements in Medicine and Biology, doi:10.1016/j.jtemb.2022.127055, Aug 2022
Zinc for COVID-19
2nd treatment shown to reduce risk in
July 2020, now with p = 0.00000028 from 47 studies, recognized in 23 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
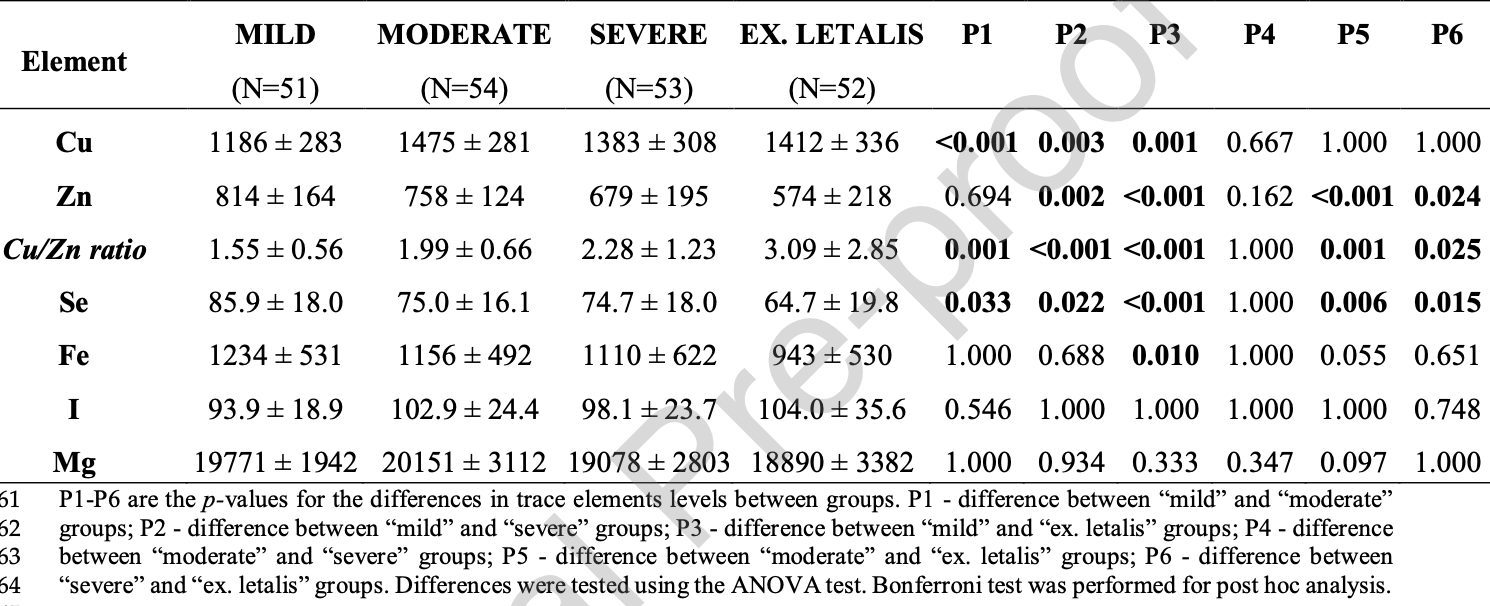
Analysis of 210 hospitalized patients in Bosnia and Herzegovina with serum levels measured on admission, showing significantly lower zinc and selenium levels in patients that died or had severe cases, compared to mild cases.
Study covers selenium and zinc.
Bego et al., 4 Aug 2022, Bosnia and Herzegovina, peer-reviewed, 10 authors, study period January 2021 - July 2021.
Contact: tamer.bego@ffsa.unsa.ba.
Association of trace element status in COVID-19 patients with disease severity
Journal of Trace Elements in Medicine and Biology, doi:10.1016/j.jtemb.2022.127055
This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
Ahmed, Jadhav, Hassan, Meng, Acute phase reactants as novel predictors of cardiovascular disease, ISRN inflammation, doi:10.5402/2012/953461
Alexander, Tinkov, Strand, Alehagen, Skalny et al., Early Nutritional Interventions with Zinc, Selenium and Vitamin D for Raising Anti-Viral Resistance Against Progressive COVID-19, Nutrients, doi:10.3390/nu12082358
Andreou, Trantza, Filippou, Sipsas, Tsiodras, COVID-19: The Potential Role of Copper and N-acetylcysteine (NAC) in a Combination of Candidate Antiviral Treatments Against SARS-CoV-2, vivo
Anuk, Polat, Akdas, Erol, Tanacan et al., The Relation Between Trace Element Status (Zinc, Copper, Magnesium) and Clinical Outcomes in COVID-19 Infection During Pregnancy, Biological trace element research, doi:10.1007/s12011-020-02496-y
Arezes, Nemeth, Hepcidin and iron disorders: new biology and clinical approaches, International journal of laboratory hematology, doi:10.1111/ijlh.12358
Asl, Nikfarjam, Majidi Zolbanin, Nassiri, Jafari, Immunopharmacological perspective on zinc in SARS-CoV-2 infection, International immunopharmacology
Baj, Karakula-Juchnowicz, Teresinski, Buszewicz, Ciesielka et al., None
Barnett, Dao, Hamer, Kandel, Brandeis et al., None
Bilal, Dambaeva, Kwak-Kim, Gilman-Sachs, Beaman, A Role for Iodide and Thyroglobulin in Modulating the Function of Human Immune Cells, Frontiers in immunology
Bockerman, Bryson, Viinikainen, Viikari, Lehtimaki et al., None
Bonham, O'connor, Hannigan, Strain, The immune system as a physiological indicator of marginal copper status?, The British journal of nutrition, doi:10.1079/BJNBJN2002558
Brix, Hegedus, Hallas, Lund, Risk and course of SARS-CoV-2 infection in patients treated for hypothyroidism and hyperthyroidism, The lancet, Diabetes & endocrinology, doi:10.1016/S2213-8587(21)00028-0
Butler, Barrientos, The impact of nutrition on COVID-19 susceptibility and long-term consequences, Brain, behavior, and immunity, doi:10.1016/j.bbi.2020.04.040
Buxaderas, Farre-Rovira, Whole blood and serum copper levels in relation to sex and age, Revista espanola de fisiologia
Caccialanza, Laviano, Lobascio, Montagna, Bruno et al., Early nutritional supplementation in non-critically ill patients hospitalized for the 2019 novel coronavirus disease (COVID-19): Rationale and feasibility of a shared pragmatic protocol, Nutrition, doi:10.1016/j.nut.2020.110835
Calder, Nutrition and immunity: lessons for COVID-19, European journal of clinical nutrition, doi:10.1038/s41430-021-00949-8
Carsetti, Zaffina, Piano, Mortari, Terreri et al., Different Innate and Adaptive Immune Responses to SARS-CoV-2 Infection of Asymptomatic, Mild, and Severe Cases, Frontiers in immunology
Chandra, Nutrition and the immune system: an introduction, The American journal of clinical nutrition, doi:10.1093/ajcn/66.2.460S
Cherayil, Iron and immunity: immunological consequences of iron deficiency and overload, Archivum immunologiae et therapiae experimentalis, doi:10.1007/s00005-010-0095-9
Chung, Iodine and thyroid function, Annals of pediatric endocrinology & metabolism, doi:10.6065/apem.2014.19.1.8
De Jesus, Andrade, Understanding the relationship between viral infections and trace elements from a metallomics perspective: implications for COVID-19, Metallomics, doi:10.1039/d0mt00220h
Dharmalingam, Birdi, Tomo, Sreenivasulu, Charan et al., Trace Elements as Immunoregulators in SARS-CoV-2 and Other Viral Infections, Indian journal of clinical biochemistry
Dinicolantonio, O'keefe, Wilson, Subclinical magnesium deficiency: a principal driver of cardiovascular disease and a public health crisis, Open heart, doi:10.1136/openhrt-2017-000668
Domingo, Marques, The effects of some essential and toxic metals/metalloids in COVID-19: A review, Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association, doi:10.1016/j.fct.2021.112161
Ehsani, COVID-19 and iron dysregulation: distant sequence similarity between hepcidin and the novel coronavirus spike glycoprotein, Biology direct
Farebrother, Zimmermann, Andersson, Excess iodine intake: sources, assessment, and effects on thyroid function, Annals of the New York Academy of Sciences, doi:10.1111/nyas.14041
Farshbafnadi, Kamali, Zonouzi, Sabahi, Dolatshahi et al., Aging & COVID-19 susceptibility, disease severity, and clinical outcomes: The role of entangled risk factors, Experimental gerontology, doi:10.1016/j.exger.2021.111507
Flieger, Portincasa, Maciejewski, COVID-19: Specific and Non-Specific Clinical Manifestations and Symptoms: The Current State of Knowledge, Journal of clinical medicine, doi:10.3390/jcm9061753
Fooladi, Matin, Mahmoodpoor, Copper as a potential adjunct therapy for critically ill COVID-19 patients, Clin Nutr Espen, doi:10.1016/j.clnesp.2020.09.022
Forceville, Mostert, Pierantoni, Vitoux, Le Toumelin et al., Rather than Glutathione Peroxidase, as a Potential Marker of Septic Shock and Related Syndromes, Eur Surg Res, doi:10.1159/000239763
Galaris, Barbouti, Pantopoulos, Iron homeostasis and oxidative stress: An intimate relationship, Biochimica et biophysica acta. Molecular cell research, doi:10.1016/j.bbamcr.2019.118535
Galloway, Mcmillan, Sattar, Effect of the inflammatory response on trace element and vitamin status, Annals of clinical biochemistry, doi:10.1258/0004563001899429
Gammoh, Rink, None, Zinc in Infection and Inflammation, doi:10.3390/nu9060624
Goulle, Mahieu, Castermant, Neveu, Bonneau et al., Metal and metalloid multi-elementary ICP-MS validation in whole blood, plasma, urine and hair. Reference values, Forensic science international, doi:10.1016/j.forsciint.2005.04.020
Guillin, Vindry, Ohlmann, Chavatte, Selenium, Selenoproteins and Viral Infection, Nutrients, doi:10.3390/nu11092101
Hackler, Heller, Sun, Schwarzer, Diegmann et al., Relation of Serum Copper Status to Survival in COVID-19, Nutrients, doi:10.3390/nu13061898
Harthill, Review: micronutrient selenium deficiency influences evolution of some viral infectious diseases, Biological trace element research, doi:10.1007/s12011-011-8977-1
Jahnen-Dechent, Ketteler, Magnesium basics, Clinical kidney journal, doi:10.1093/ndtplus/sfr163
Jin, Jiang, Liu, Jia, Liu et al., The application of serum iodine in assessing individual iodine status, Clinical endocrinology, doi:10.1111/cen.13421
Joachimiak, Zinc against COVID-19? Symptom surveillance and deficiency risk groups, PLoS neglected tropical diseases, doi:10.1016/j.intimp.2021.107630
Khatiwada, Subedi, A Mechanistic Link Between Selenium and Coronavirus Disease 2019 (COVID-19), Curr Nutr Rep, doi:10.1007/s13668-021-00354-4
Kieliszek, Lipinski, Selenium supplementation in the prevention of coronavirus infections (COVID-19), Medical hypotheses, doi:10.1016/j.mehy.2020.109878
Kong, Meydani, Effect of zinc supplementation on serum zinc concentration and T cell proliferation in nursing home elderly: a randomized, double-blind, placebo-controlled trial, The American journal of clinical nutrition, doi:10.3945/ajcn.115.115188
Liu, Zhao, Ma, Mu, Wang et al., Selenium (Se) plays a key role in the biological effects of some viruses: Implications for COVID-19, Environ Res, doi:10.1016/j.envres.2021.110984
Lv, Chen, Liang, Liu, Gao et al., Association between iron status and the risk of adverse outcomes in COVID-19, Clinical nutrition, doi:10.1016/j.clnu.2020.11.033
Majeed, Nagabhushanam, Gowda, Mundkur, An exploratory study of selenium status in healthy individuals and in patients with COVID-19 in a south Indian population: The case for adequate selenium status, Nutrition, doi:10.1016/j.nut.2020.111053
Maret, Zinc biochemistry: from a single zinc enzyme to a key element of life, Advances in nutrition, doi:10.3945/an.112.003038
Micke, Pourdowlat, Scarpati, Wolf, Maier, The relevance of magnesium homeostasis in COVID-19, European journal of nutrition, doi:10.1007/s00394-021-02704-y
Montesinos, Pellizas, Thyroid Hormone Action on Innate Immunity, Frontiers in endocrinology, doi:10.3389/fendo.2019.00350
Mutiawati, Fahriani, Mamada, Fajar, Frediansyah et al., Anosmia and dysgeusia in SARS-CoV-2 infection: incidence and effects on COVID-19 severity and mortality, and the possible pathobiology mechanisms -a systematic review and meta-analysis, F1000Research
Olea, Albert, Torres, Amat, Remigia et al., Adaptive immune responses to SARS-CoV-2 in recovered severe COVID-19 patients, Journal of clinical virology : the official publication of the Pan American Society for Clinical Virology
Osredkar, Copper and zinc, biological role and significance of copper/zinc imbalance, J Clin Toxicol
Paces, Strizova, Smrz, Cerny, COVID-19 and the immune system, Physiological research, doi:10.33549/physiolres.934492
Pan, Cui, Chen, Gao, Pearce et al., Serum iodine concentration in pregnant women and its association with urinary iodine concentration and thyroid function, Clinical endocrinology, doi:10.1111/cen.13945
Raitakari, Pehkonen, The serum copper/zinc ratio in childhood and educational attainment: a population-based study, Journal of public health, doi:10.1093/pubmed/fdv187
Ravell, Chaigne-Delalande, Lenardo, X-linked immunodeficiency with magnesium defect, Epstein-Barr virus infection, and neoplasia disease: a combined immune deficiency with magnesium defect, Current opinion in pediatrics
Read, Obeid, Ahlenstiel, Ahlenstiel, The Role of Zinc in Antiviral Immunity, Advances in nutrition, doi:10.1093/advances/nmz013
Reilev, Kristensen, Pottegard, Lund, Hallas et al., Characteristics and predictors of hospitalization and death in the first 11 122 cases with a positive RT-PCR test for SARS-CoV-2 in Denmark: a nationwide cohort, International journal of epidemiology, doi:10.1093/ije/dyaa140
Selenium, None
Sharma, Reddy, Kumar, Trace Element Zinc, a Nature's Gift to Fight Unprecedented Global Pandemic COVID-19, Biological trace element research, doi:10.1007/s12011-020-02462-8
Skalny, Timashev, Aschner, Aaseth, Chernova et al., Serum Zinc, Copper, and Other Biometals Are Associated with COVID-19 Severity Markers, Metabolites, doi:10.3390/metabo11040244
Sonnweber, Boehm, Sahanic, Pizzini, Aichner et al., Persisting alterations of iron homeostasis in COVID-19 are associated with non-resolving lung pathologies and poor patients' performance: a prospective observational cohort study, Respiratory research, doi:10.1186/s12931-020-01546-2
Taheri, Asadi, Nilashi, Ali Abumalloh, Ghabban et al., A literature review on beneficial role of vitamins and trace elements: Evidence from published clinical studies, Journal of trace elements in medicine and biology : organ of the Society for Minerals and Trace Elements
Taheri, Bahrami, Habibi, Nouri, A Review on the Serum Electrolytes and Trace Elements Role in the Pathophysiology of COVID-19, Biological trace element research, doi:10.1007/s12011-020-02377-4
Tam, Gomez, Gonzalez-Gross, Marcos, Possible roles of magnesium on the immune system, European journal of clinical nutrition, doi:10.1038/sj.ejcn.1601689
Tay, Poh, Renia, Macary, Ng, The trinity of COVID-19: immunity, inflammation and intervention, Nature reviews, Immunology, doi:10.1038/s41577-020-0311-8
Trapani, Rosanoff, Baniasadi, Barbagallo, Castiglioni et al., None
Uauy, Olivares, Gonzalez, Essentiality of copper in humans, The American journal of clinical nutrition, doi:10.1093/ajcn/67.5.952S
Van Gerwen, Alsen, Little, Barlow, Naymagon et al., Outcomes of Patients With Hypothyroidism and COVID-19: A Retrospective Cohort Study, Frontiers in endocrinology, doi:10.3389/fendo.2020.00565
Verheesen, Traksel, Iodine, a preventive and curative agent in the COVID-19 pandemic?, Medical hypotheses, doi:10.1016/j.mehy.2020.109860
Yaqoob, Ageing alters the impact of nutrition on immune function, The Proceedings of the Nutrition Society, doi:10.1017/S0029665116000781
Zhang, Liu, Potential interventions for novel coronavirus in China: A systematic review, Journal of medical virology, doi:10.1002/jmv.25707
Zhang, Taylor, Bennett, Saad, Rayman, Association between regional selenium status and reported outcome of COVID-19 cases in China, The American journal of clinical nutrition, doi:10.1093/ajcn/nqaa095
Zhang, Zhang, Lu, Zhang, Zhang et al., Association between fatality rate of COVID-19 and selenium deficiency in China, Bmc Infect Dis, doi:10.1186/s12879-021-06167-8
Zhao, Huang, Dai, Feng, Liu et al., Serum Iron Level as a Potential Predictor of Coronavirus Disease 2019 Severity and Mortality: A Retrospective Study, Open forum infectious diseases, doi:10.1093/ofid/ofaa250
Zhou, Chen, Ji, He, Xue, Increased Serum Levels of Hepcidin and Ferritin Are Associated with Severity of COVID-19, Medical science monitor : international medical journal of experimental and clinical research
Zimmermann, Boelaert, Iodine deficiency and thyroid disorders, Lancet Diabetes Endo, doi:10.1016/S2213-8587(14)70225-6
DOI record:
{
"DOI": "10.1016/j.jtemb.2022.127055",
"ISSN": [
"0946-672X"
],
"URL": "http://dx.doi.org/10.1016/j.jtemb.2022.127055",
"alternative-id": [
"S0946672X22001353"
],
"article-number": "127055",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Association of Trace Element Status in COVID-19 Patients with Disease Severity"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Journal of Trace Elements in Medicine and Biology"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.jtemb.2022.127055"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2022 Elsevier GmbH. All rights reserved."
}
],
"author": [
{
"affiliation": [],
"family": "Bego",
"given": "Tamer",
"sequence": "first"
},
{
"affiliation": [],
"family": "Meseldžić",
"given": "Neven",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Prnjavorac",
"given": "Besim",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Prnjavorac",
"given": "Lejla",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Marjanović",
"given": "Damir",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Azevedo",
"given": "Rui",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pinto",
"given": "Edgar",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Duro",
"given": "Mary",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Couto",
"given": "Cristina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Almeida",
"given": "Agostinho",
"sequence": "additional"
}
],
"container-title": "Journal of Trace Elements in Medicine and Biology",
"container-title-short": "Journal of Trace Elements in Medicine and Biology",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2022,
8,
4
]
],
"date-time": "2022-08-04T06:14:01Z",
"timestamp": 1659593641000
},
"deposited": {
"date-parts": [
[
2022,
8,
4
]
],
"date-time": "2022-08-04T22:19:42Z",
"timestamp": 1659651582000
},
"funder": [
{
"DOI": "10.13039/501100003621",
"award": [
"27-02-11-4375-10/21"
],
"doi-asserted-by": "publisher",
"name": "Ministry of Science, ICT and Future Planning"
}
],
"indexed": {
"date-parts": [
[
2022,
8,
4
]
],
"date-time": "2022-08-04T22:41:56Z",
"timestamp": 1659652916357
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
8
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
8,
1
]
],
"date-time": "2022-08-01T00:00:00Z",
"timestamp": 1659312000000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0946672X22001353?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0946672X22001353?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "127055",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2022,
8
]
]
},
"published-print": {
"date-parts": [
[
2022,
8
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"key": "10.1016/j.jtemb.2022.127055_bib1",
"unstructured": "Government of Canada. COVID-19 signs, symptoms and severity of disease: A clinician guide. Available online: 〈https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/guidance-documents/signs-symptoms-severity.html〉 (accessed on 16/11/2021)."
},
{
"DOI": "10.12688/f1000research.28393.1",
"article-title": "Anosmia and dysgeusia in SARS-CoV-2 infection: incidence and effects on COVID-19 severity and mortality, and the possible pathobiology mechanisms - a systematic review and meta-analysis",
"author": "Mutiawati",
"doi-asserted-by": "crossref",
"first-page": "40",
"journal-title": "F1000Research",
"key": "10.1016/j.jtemb.2022.127055_bib2",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1016/j.exger.2021.111507",
"article-title": "Aging & COVID-19 susceptibility, disease severity, and clinical outcomes: The role of entangled risk factors",
"author": "Farshbafnadi",
"doi-asserted-by": "crossref",
"journal-title": "Experimental gerontology",
"key": "10.1016/j.jtemb.2022.127055_bib3",
"volume": "154",
"year": "2021"
},
{
"key": "10.1016/j.jtemb.2022.127055_bib4",
"unstructured": "WHO Coronavirus (COVID-19) Dashboard. Available online: 〈https://covid19.who.int/〉 (accessed on 6/12/2021)."
},
{
"DOI": "10.1038/s41577-020-0311-8",
"article-title": "The trinity of COVID-19: immunity, inflammation and intervention",
"author": "Tay",
"doi-asserted-by": "crossref",
"first-page": "363",
"issue": "6",
"journal-title": "Nature reviews. Immunology",
"key": "10.1016/j.jtemb.2022.127055_bib5",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.33549/physiolres.934492",
"article-title": "COVID-19 and the immune system",
"author": "Paces",
"doi-asserted-by": "crossref",
"first-page": "379",
"issue": "3",
"journal-title": "Physiological research",
"key": "10.1016/j.jtemb.2022.127055_bib6",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1016/j.jcv.2021.104943",
"article-title": "Adaptive immune responses to SARS-CoV-2 in recovered severe COVID-19 patients",
"author": "Olea",
"doi-asserted-by": "crossref",
"journal-title": "Journal of clinical virology: the official publication of the Pan American Society for Clinical Virology",
"key": "10.1016/j.jtemb.2022.127055_bib7",
"volume": "142",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2020.610300",
"article-title": "Different Innate and Adaptive Immune Responses to SARS-CoV-2 Infection of Asymptomatic, Mild, and Severe Cases",
"author": "Carsetti",
"doi-asserted-by": "crossref",
"journal-title": "Frontiers in immunology",
"key": "10.1016/j.jtemb.2022.127055_bib8",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1093/ajcn/66.2.460S",
"article-title": "Nutrition and the immune system: an introduction",
"author": "Chandra",
"doi-asserted-by": "crossref",
"first-page": "460S",
"issue": "2",
"journal-title": "The American journal of clinical nutrition",
"key": "10.1016/j.jtemb.2022.127055_bib9",
"volume": "66",
"year": "1997"
},
{
"DOI": "10.1016/j.nut.2020.110835",
"article-title": "Early nutritional supplementation in non-critically ill patients hospitalized for the 2019 novel coronavirus disease (COVID-19): Rationale and feasibility of a shared pragmatic protocol",
"author": "Caccialanza",
"doi-asserted-by": "crossref",
"journal-title": "Nutrition",
"key": "10.1016/j.jtemb.2022.127055_bib10",
"volume": "74",
"year": "2020"
},
{
"DOI": "10.1002/jmv.25707",
"article-title": "Potential interventions for novel coronavirus in China: A systematic review",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "479",
"issue": "5",
"journal-title": "Journal of medical virology",
"key": "10.1016/j.jtemb.2022.127055_bib11",
"volume": "92",
"year": "2020"
},
{
"DOI": "10.1016/j.fct.2021.112161",
"article-title": "The effects of some essential and toxic metals/metalloids in COVID-19: A review",
"author": "Domingo",
"doi-asserted-by": "crossref",
"journal-title": "Food and chemical toxicology: an international journal published for the British Industrial Biological Research Association",
"key": "10.1016/j.jtemb.2022.127055_bib12",
"volume": "152",
"year": "2021"
},
{
"DOI": "10.1016/j.bbi.2020.04.040",
"article-title": "The impact of nutrition on COVID-19 susceptibility and long-term consequences",
"author": "Butler",
"doi-asserted-by": "crossref",
"first-page": "53",
"journal-title": "Brain, behavior, and immunity",
"key": "10.1016/j.jtemb.2022.127055_bib13",
"volume": "87",
"year": "2020"
},
{
"DOI": "10.1017/S0029665116000781",
"article-title": "Ageing alters the impact of nutrition on immune function",
"author": "Yaqoob",
"doi-asserted-by": "crossref",
"first-page": "347",
"issue": "3",
"journal-title": "The Proceedings of the Nutrition Society",
"key": "10.1016/j.jtemb.2022.127055_bib14",
"volume": "76",
"year": "2017"
},
{
"DOI": "10.1016/j.jtemb.2021.126789",
"article-title": "A literature review on beneficial role of vitamins and trace elements: Evidence from published clinical studies",
"author": "Taheri",
"doi-asserted-by": "crossref",
"journal-title": "Journal of trace elements in medicine and biology: organ of the Society for Minerals and Trace Elements",
"key": "10.1016/j.jtemb.2022.127055_bib15",
"volume": "67",
"year": "2021"
},
{
"DOI": "10.1038/s41430-021-00949-8",
"article-title": "Nutrition and immunity: lessons for COVID-19",
"author": "Calder",
"doi-asserted-by": "crossref",
"first-page": "1309",
"issue": "9",
"journal-title": "European journal of clinical nutrition",
"key": "10.1016/j.jtemb.2022.127055_bib16",
"volume": "75",
"year": "2021"
},
{
"DOI": "10.3390/jcm9061753",
"article-title": "COVID-19: Specific and Non-Specific Clinical Manifestations and Symptoms: The Current State of Knowledge",
"author": "Baj",
"doi-asserted-by": "crossref",
"issue": "6",
"journal-title": "Journal of clinical medicine",
"key": "10.1016/j.jtemb.2022.127055_bib17",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1016/j.forsciint.2005.04.020",
"article-title": "Metal and metalloid multi-elementary ICP-MS validation in whole blood, plasma, urine and hair",
"author": "Goulle",
"doi-asserted-by": "crossref",
"first-page": "39",
"issue": "1",
"journal-title": "Reference values, Forensic science international",
"key": "10.1016/j.jtemb.2022.127055_bib18",
"volume": "153",
"year": "2005"
},
{
"key": "10.1016/j.jtemb.2022.127055_bib19",
"unstructured": "Urine Iodine ICPMS. Centers for Disease Control and Prevention (CDC) Laboratory Procedure Manual, 2001. Available online: 〈https://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/l06uio_c_met_urine_iodine_icpms.pdf〉 (accessed on 3/12/2021)."
},
{
"key": "10.1016/j.jtemb.2022.127055_bib20",
"unstructured": "Risk for COVID-19 infection, hospitalization, and death by age group. Available online: 〈https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-age.html〉 (accessed on 18/11/2021)."
},
{
"DOI": "10.1093/ije/dyaa140",
"article-title": "Characteristics and predictors of hospitalization and death in the first 11 122 cases with a positive RT-PCR test for SARS-CoV-2 in Denmark: a nationwide cohort",
"author": "Reilev",
"doi-asserted-by": "crossref",
"first-page": "1468",
"issue": "5",
"journal-title": "International journal of epidemiology",
"key": "10.1016/j.jtemb.2022.127055_bib21",
"volume": "49",
"year": "2020"
},
{
"DOI": "10.1039/d0mt00220h",
"article-title": "Understanding the relationship between viral infections and trace elements from a metallomics perspective: implications for COVID-19",
"author": "de Jesus",
"doi-asserted-by": "crossref",
"first-page": "1912",
"issue": "12",
"journal-title": "Metallomics",
"key": "10.1016/j.jtemb.2022.127055_bib22",
"volume": "12",
"year": "2020"
},
{
"article-title": "Trace Elements as Immunoregulators in SARS-CoV-2 and Other Viral Infections",
"author": "Dharmalingam",
"first-page": "1",
"journal-title": "Indian journal of clinical biochemistry: IJCB",
"key": "10.1016/j.jtemb.2022.127055_bib23",
"year": "2021"
},
{
"DOI": "10.1136/openhrt-2017-000668",
"article-title": "Subclinical magnesium deficiency: a principal driver of cardiovascular disease and a public health crisis",
"author": "DiNicolantonio",
"doi-asserted-by": "crossref",
"issue": "1",
"journal-title": "Open heart",
"key": "10.1016/j.jtemb.2022.127055_bib24",
"volume": "5",
"year": "2018"
},
{
"DOI": "10.1038/sj.ejcn.1601689",
"article-title": "Possible roles of magnesium on the immune system",
"author": "Tam",
"doi-asserted-by": "crossref",
"first-page": "1193",
"issue": "10",
"journal-title": "European journal of clinical nutrition",
"key": "10.1016/j.jtemb.2022.127055_bib25",
"volume": "57",
"year": "2003"
},
{
"DOI": "10.1097/MOP.0000000000000156",
"article-title": "X-linked immunodeficiency with magnesium defect, Epstein-Barr virus infection, and neoplasia disease: a combined immune deficiency with magnesium defect",
"author": "Ravell",
"doi-asserted-by": "crossref",
"first-page": "713",
"issue": "6",
"journal-title": "Current opinion in pediatrics",
"key": "10.1016/j.jtemb.2022.127055_bib26",
"volume": "26",
"year": "2014"
},
{
"key": "10.1016/j.jtemb.2022.127055_bib27",
"unstructured": "Mayo Clinic Laboratories – Magnesium. Available onliine: 〈https://www.mayocliniclabs.com/test-catalog/Clinical+and+Interpretive/8448〉 (accessed on 21/11/2021)."
},
{
"DOI": "10.3390/metabo11040244",
"article-title": "Serum Zinc, Copper, and Other Biometals Are Associated with COVID-19 Severity Markers",
"author": "Skalny",
"doi-asserted-by": "crossref",
"issue": "4",
"journal-title": "Metabolites",
"key": "10.1016/j.jtemb.2022.127055_bib28",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1093/ndtplus/sfr163",
"article-title": "Magnesium basics",
"author": "Jahnen-Dechent",
"doi-asserted-by": "crossref",
"first-page": "i3",
"issue": "Suppl 1",
"journal-title": "Clinical kidney journal",
"key": "10.1016/j.jtemb.2022.127055_bib29",
"volume": "5",
"year": "2012"
},
{
"article-title": "The relevance of magnesium homeostasis in COVID-19",
"author": "Trapani",
"journal-title": "European journal of nutrition",
"key": "10.1016/j.jtemb.2022.127055_bib30",
"year": "2021"
},
{
"DOI": "10.1007/s12011-020-02496-y",
"article-title": "The Relation Between Trace Element Status (Zinc, Copper, Magnesium) and Clinical Outcomes in COVID-19 Infection During Pregnancy",
"author": "Anuk",
"doi-asserted-by": "crossref",
"first-page": "3608",
"issue": "10",
"journal-title": "Biological trace element research",
"key": "10.1016/j.jtemb.2022.127055_bib31",
"volume": "199",
"year": "2021"
},
{
"article-title": "Iron homeostasis and oxidative stress: An intimate relationship, Biochimica et biophysica acta",
"author": "Galaris",
"issue": "12",
"journal-title": "Molecular cell research",
"key": "10.1016/j.jtemb.2022.127055_bib32",
"volume": "1866",
"year": "2019"
},
{
"DOI": "10.1007/s00005-010-0095-9",
"article-title": "Iron and immunity: immunological consequences of iron deficiency and overload",
"author": "Cherayil",
"doi-asserted-by": "crossref",
"first-page": "407",
"issue": "6",
"journal-title": "Archivum immunologiae et therapiae experimentalis",
"key": "10.1016/j.jtemb.2022.127055_bib33",
"volume": "58",
"year": "2010"
},
{
"DOI": "10.1111/ijlh.12358",
"article-title": "Hepcidin and iron disorders: new biology and clinical approaches",
"author": "Arezes",
"doi-asserted-by": "crossref",
"first-page": "92",
"issue": "Suppl 1",
"journal-title": "International journal of laboratory hematology",
"key": "10.1016/j.jtemb.2022.127055_bib34",
"volume": "37",
"year": "2015"
},
{
"DOI": "10.1186/s13062-020-00275-2",
"article-title": "COVID-19 and iron dysregulation: distant sequence similarity between hepcidin and the novel coronavirus spike glycoprotein",
"author": "Ehsani",
"doi-asserted-by": "crossref",
"first-page": "19",
"issue": "1",
"journal-title": "Biology direct",
"key": "10.1016/j.jtemb.2022.127055_bib35",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1007/s12011-020-02377-4",
"article-title": "A Review on the Serum Electrolytes and Trace Elements Role in the Pathophysiology of COVID-19",
"author": "Taheri",
"doi-asserted-by": "crossref",
"first-page": "2475",
"issue": "7",
"journal-title": "Biological trace element research",
"key": "10.1016/j.jtemb.2022.127055_bib36",
"volume": "199",
"year": "2021"
},
{
"key": "10.1016/j.jtemb.2022.127055_bib37",
"unstructured": "Mayo Clinic Laboratories. Iron and Total Iron-Binding Capacity, Serum. Available online: 〈https://www.mayocliniclabs.com/test-catalog/Clinical+and+Interpretive/34624〉 (accessed on 6/12/2021)."
},
{
"DOI": "10.12659/MSM.926178",
"article-title": "Increased Serum Levels of Hepcidin and Ferritin Are Associated with Severity of COVID-19",
"author": "Zhou",
"doi-asserted-by": "crossref",
"journal-title": "Medical science monitor: international medical journal of experimental and clinical research",
"key": "10.1016/j.jtemb.2022.127055_bib38",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1093/ofid/ofaa250",
"article-title": "Serum Iron Level as a Potential Predictor of Coronavirus Disease 2019 Severity and Mortality: A Retrospective Study",
"author": "Zhao",
"doi-asserted-by": "crossref",
"issue": "7",
"journal-title": "Open forum infectious diseases",
"key": "10.1016/j.jtemb.2022.127055_bib39",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1186/s12931-020-01546-2",
"article-title": "Persisting alterations of iron homeostasis in COVID-19 are associated with non-resolving lung pathologies and poor patients' performance: a prospective observational cohort study",
"author": "Sonnweber",
"doi-asserted-by": "crossref",
"first-page": "276",
"issue": "1",
"journal-title": "Respiratory research",
"key": "10.1016/j.jtemb.2022.127055_bib40",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1016/j.clnu.2020.11.033",
"article-title": "Association between iron status and the risk of adverse outcomes in COVID-19",
"author": "Lv",
"doi-asserted-by": "crossref",
"first-page": "3462",
"issue": "5",
"journal-title": "Clinical nutrition",
"key": "10.1016/j.jtemb.2022.127055_bib41",
"volume": "40",
"year": "2021"
},
{
"DOI": "10.1093/ajcn/67.5.952S",
"article-title": "Essentiality of copper in humans",
"author": "Uauy",
"doi-asserted-by": "crossref",
"first-page": "952S",
"issue": "5 Suppl",
"journal-title": "The American journal of clinical nutrition",
"key": "10.1016/j.jtemb.2022.127055_bib42",
"volume": "67",
"year": "1998"
},
{
"DOI": "10.1079/BJN2002558",
"article-title": "The immune system as a physiological indicator of marginal copper status?",
"author": "Bonham",
"doi-asserted-by": "crossref",
"first-page": "393",
"issue": "5",
"journal-title": "The British journal of nutrition",
"key": "10.1016/j.jtemb.2022.127055_bib43",
"volume": "87",
"year": "2002"
},
{
"DOI": "10.21873/invivo.11946",
"article-title": "COVID-19: The Potential Role of Copper and N-acetylcysteine (NAC) in a Combination of Candidate Antiviral Treatments Against SARS-CoV-2",
"author": "Andreou",
"doi-asserted-by": "crossref",
"first-page": "1567",
"issue": "3 Suppl",
"journal-title": "In vivo",
"key": "10.1016/j.jtemb.2022.127055_bib44",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.1016/j.clnesp.2020.09.022",
"article-title": "Copper as a potential adjunct therapy for critically ill COVID-19 patients",
"author": "Fooladi",
"doi-asserted-by": "crossref",
"first-page": "90",
"journal-title": "Clin Nutr Espen",
"key": "10.1016/j.jtemb.2022.127055_bib45",
"volume": "40",
"year": "2020"
},
{
"DOI": "10.3390/nu13061898",
"article-title": "Relation of Serum Copper Status to Survival in COVID-19",
"author": "Hackler",
"doi-asserted-by": "crossref",
"issue": "6",
"journal-title": "Nutrients",
"key": "10.1016/j.jtemb.2022.127055_bib46",
"volume": "13",
"year": "2021"
},
{
"article-title": "Whole blood and serum copper levels in relation to sex and age",
"author": "Buxaderas",
"first-page": "213",
"issue": "2",
"journal-title": "Revista espanola de fisiologia",
"key": "10.1016/j.jtemb.2022.127055_bib47",
"volume": "42",
"year": "1986"
},
{
"key": "10.1016/j.jtemb.2022.127055_bib48",
"unstructured": "ARUP Laboratories. Copper, Serum or Plasma. Available online: 〈https://ltd.aruplab.com/Tests/Pub/0020096〉 (accessed on 06/12/2021)."
},
{
"DOI": "10.1258/0004563001899429",
"article-title": "Effect of the inflammatory response on trace element and vitamin status",
"author": "Galloway",
"doi-asserted-by": "crossref",
"first-page": "289",
"issue": "Pt 3",
"journal-title": "Annals of clinical biochemistry",
"key": "10.1016/j.jtemb.2022.127055_bib49",
"volume": "37",
"year": "2000"
},
{
"DOI": "10.5402/2012/953461",
"article-title": "Acute phase reactants as novel predictors of cardiovascular disease",
"author": "Ahmed",
"doi-asserted-by": "crossref",
"journal-title": "ISRN inflammation",
"key": "10.1016/j.jtemb.2022.127055_bib50",
"volume": "2012",
"year": "2012"
},
{
"DOI": "10.3945/an.112.003038",
"article-title": "Zinc biochemistry: from a single zinc enzyme to a key element of life",
"author": "Maret",
"doi-asserted-by": "crossref",
"first-page": "82",
"issue": "1",
"journal-title": "Advances in nutrition",
"key": "10.1016/j.jtemb.2022.127055_bib51",
"volume": "4",
"year": "2013"
},
{
"DOI": "10.3390/nu9060624",
"article-title": "Zinc in Infection and Inflammation",
"author": "Gammoh",
"doi-asserted-by": "crossref",
"issue": "6",
"journal-title": "Nutrients",
"key": "10.1016/j.jtemb.2022.127055_bib52",
"volume": "9",
"year": "2017"
},
{
"DOI": "10.3945/ajcn.115.115188",
"article-title": "Effect of zinc supplementation on serum zinc concentration and T cell proliferation in nursing home elderly: a randomized, double-blind, placebo-controlled trial",
"author": "Barnett",
"doi-asserted-by": "crossref",
"first-page": "942",
"issue": "3",
"journal-title": "The American journal of clinical nutrition",
"key": "10.1016/j.jtemb.2022.127055_bib53",
"volume": "103",
"year": "2016"
},
{
"DOI": "10.1093/advances/nmz013",
"article-title": "The Role of Zinc in Antiviral Immunity",
"author": "Read",
"doi-asserted-by": "crossref",
"first-page": "696",
"issue": "4",
"journal-title": "Advances in nutrition",
"key": "10.1016/j.jtemb.2022.127055_bib54",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1007/s12011-020-02462-8",
"article-title": "Trace Element Zinc, a Nature's Gift to Fight Unprecedented Global Pandemic COVID-19",
"author": "Sharma",
"doi-asserted-by": "crossref",
"first-page": "3213",
"issue": "9",
"journal-title": "Biological trace element research",
"key": "10.1016/j.jtemb.2022.127055_bib55",
"volume": "199",
"year": "2021"
},
{
"DOI": "10.1016/j.intimp.2021.107630",
"article-title": "Immunopharmacological perspective on zinc in SARS-CoV-2 infection",
"author": "Asl",
"doi-asserted-by": "crossref",
"journal-title": "International immunopharmacology",
"key": "10.1016/j.jtemb.2022.127055_bib56",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1371/journal.pntd.0008895",
"article-title": "Zinc against COVID-19? Symptom surveillance and deficiency risk groups",
"author": "Joachimiak",
"doi-asserted-by": "crossref",
"issue": "1",
"journal-title": "PLoS neglected tropical diseases",
"key": "10.1016/j.jtemb.2022.127055_bib57",
"volume": "15",
"year": "2021"
},
{
"key": "10.1016/j.jtemb.2022.127055_bib58",
"unstructured": "ARUP Laboratories. Zinc, Serum or Plasma. Available online: 〈https://ltd.aruplab.com/Tests/Pub/0020097〉 (accessed on 25/11/2021)."
},
{
"DOI": "10.1093/pubmed/fdv187",
"article-title": "The serum copper/zinc ratio in childhood and educational attainment: a population-based study",
"author": "Bockerman",
"doi-asserted-by": "crossref",
"first-page": "696",
"issue": "4",
"journal-title": "Journal of public health",
"key": "10.1016/j.jtemb.2022.127055_bib59",
"volume": "38",
"year": "2016"
},
{
"DOI": "10.4172/2161-0495.S3-001",
"article-title": "Copper and zinc, biological role and significance of copper/zinc imbalance",
"author": "Osredkar",
"doi-asserted-by": "crossref",
"journal-title": "J Clin Toxicol",
"key": "10.1016/j.jtemb.2022.127055_bib60",
"year": "2011"
},
{
"DOI": "10.3390/nu11092101",
"article-title": "Selenium, Selenoproteins and Viral Infection",
"author": "Guillin",
"doi-asserted-by": "crossref",
"issue": "9",
"journal-title": "Nutrients",
"key": "10.1016/j.jtemb.2022.127055_bib61",
"volume": "11",
"year": "2019"
},
{
"DOI": "10.1007/s12011-011-8977-1",
"article-title": "Review: micronutrient selenium deficiency influences evolution of some viral infectious diseases",
"author": "Harthill",
"doi-asserted-by": "crossref",
"first-page": "1325",
"issue": "3",
"journal-title": "Biological trace element research",
"key": "10.1016/j.jtemb.2022.127055_bib62",
"volume": "143",
"year": "2011"
},
{
"DOI": "10.1093/ajcn/nqaa095",
"article-title": "Association between regional selenium status and reported outcome of COVID-19 cases in China",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "1297",
"issue": "6",
"journal-title": "The American journal of clinical nutrition",
"key": "10.1016/j.jtemb.2022.127055_bib63",
"volume": "111",
"year": "2020"
},
{
"DOI": "10.1016/j.envres.2021.110984",
"article-title": "Selenium (Se) plays a key role in the biological effects of some viruses: Implications for COVID-19",
"author": "Liu",
"doi-asserted-by": "crossref",
"journal-title": "Environ Res",
"key": "10.1016/j.jtemb.2022.127055_bib64",
"volume": "196",
"year": "2021"
},
{
"article-title": "Association between fatality rate of COVID-19 and selenium deficiency in China",
"author": "Zhang",
"issue": "1",
"journal-title": "Bmc Infect Dis",
"key": "10.1016/j.jtemb.2022.127055_bib65",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1159/000239763",
"article-title": "Selenoprotein P, Rather than Glutathione Peroxidase, as a Potential Marker of Septic Shock and Related Syndromes",
"author": "Forceville",
"doi-asserted-by": "crossref",
"first-page": "338",
"issue": "4",
"journal-title": "Eur Surg Res",
"key": "10.1016/j.jtemb.2022.127055_bib66",
"volume": "43",
"year": "2009"
},
{
"key": "10.1016/j.jtemb.2022.127055_bib67",
"unstructured": "Mayo Clinic Laboratories. Selenium, Serum. Available online: 〈https://www.mayocliniclabs.com/test-catalog/overview/9765#Clinical-and-Interpretive〉 (accessed on 6/12/2021)."
},
{
"DOI": "10.1016/j.nut.2020.111053",
"article-title": "An exploratory study of selenium status in healthy individuals and in patients with COVID-19 in a south Indian population: The case for adequate selenium status",
"author": "Majeed",
"doi-asserted-by": "crossref",
"journal-title": "Nutrition",
"key": "10.1016/j.jtemb.2022.127055_bib68",
"volume": "82",
"year": "2021"
},
{
"DOI": "10.1007/s13668-021-00354-4",
"article-title": "A Mechanistic Link Between Selenium and Coronavirus Disease 2019 (COVID-19",
"author": "Khatiwada",
"doi-asserted-by": "crossref",
"first-page": "125",
"issue": "2",
"journal-title": "Curr Nutr Rep",
"key": "10.1016/j.jtemb.2022.127055_bib69",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1016/j.mehy.2020.109878",
"article-title": "Selenium supplementation in the prevention of coronavirus infections (COVID-19",
"author": "Kieliszek",
"doi-asserted-by": "crossref",
"journal-title": "Medical hypotheses",
"key": "10.1016/j.jtemb.2022.127055_bib70",
"volume": "143",
"year": "2020"
},
{
"DOI": "10.3390/nu12082358",
"article-title": "Early Nutritional Interventions with Zinc, Selenium and Vitamin D for Raising Anti-Viral Resistance Against Progressive COVID-19",
"author": "Alexander",
"doi-asserted-by": "crossref",
"issue": "8",
"journal-title": "Nutrients",
"key": "10.1016/j.jtemb.2022.127055_bib71",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(14)70225-6",
"article-title": "Iodine deficiency and thyroid disorders",
"author": "Zimmermann",
"doi-asserted-by": "crossref",
"first-page": "286",
"issue": "4",
"journal-title": "Lancet Diabetes Endo",
"key": "10.1016/j.jtemb.2022.127055_bib72",
"volume": "3",
"year": "2015"
},
{
"article-title": "Thyroid Hormone Action on Innate Immunity",
"author": "Montesinos",
"journal-title": "Frontiers in endocrinology",
"key": "10.1016/j.jtemb.2022.127055_bib73",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.3389/fimmu.2017.01573",
"article-title": "A Role for Iodide and Thyroglobulin in Modulating the Function of Human Immune Cells",
"author": "Bilal",
"doi-asserted-by": "crossref",
"first-page": "1573",
"journal-title": "Frontiers in immunology",
"key": "10.1016/j.jtemb.2022.127055_bib74",
"volume": "8",
"year": "2017"
},
{
"DOI": "10.1016/j.mehy.2020.109860",
"article-title": "Iodine, a preventive and curative agent in the COVID-19 pandemic?",
"author": "Verheesen",
"doi-asserted-by": "crossref",
"journal-title": "Medical hypotheses",
"key": "10.1016/j.jtemb.2022.127055_bib75",
"volume": "144",
"year": "2020"
},
{
"article-title": "Excess iodine intake: sources, assessment, and effects on thyroid function",
"author": "Farebrother",
"first-page": "44",
"issue": "1",
"journal-title": "Annals of the New York Academy of Sciences",
"key": "10.1016/j.jtemb.2022.127055_bib76",
"volume": "1446",
"year": "2019"
},
{
"DOI": "10.6065/apem.2014.19.1.8",
"article-title": "Iodine and thyroid function",
"author": "Chung",
"doi-asserted-by": "crossref",
"first-page": "8",
"issue": "1",
"journal-title": "Annals of pediatric endocrinology & metabolism",
"key": "10.1016/j.jtemb.2022.127055_bib77",
"volume": "19",
"year": "2014"
},
{
"DOI": "10.1111/cen.13421",
"article-title": "The application of serum iodine in assessing individual iodine status",
"author": "Jin",
"doi-asserted-by": "crossref",
"first-page": "807",
"issue": "6",
"journal-title": "Clinical endocrinology",
"key": "10.1016/j.jtemb.2022.127055_bib78",
"volume": "87",
"year": "2017"
},
{
"DOI": "10.1111/cen.13945",
"article-title": "Serum iodine concentration in pregnant women and its association with urinary iodine concentration and thyroid function",
"author": "Pan",
"doi-asserted-by": "crossref",
"first-page": "711",
"issue": "5",
"journal-title": "Clinical endocrinology",
"key": "10.1016/j.jtemb.2022.127055_bib79",
"volume": "90",
"year": "2019"
},
{
"DOI": "10.1016/S2213-8587(21)00028-0",
"article-title": "Risk and course of SARS-CoV-2 infection in patients treated for hypothyroidism and hyperthyroidism",
"author": "Brix",
"doi-asserted-by": "crossref",
"first-page": "197",
"issue": "4",
"journal-title": "The lancet. Diabetes & endocrinology",
"key": "10.1016/j.jtemb.2022.127055_bib80",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.3389/fendo.2020.00565",
"article-title": "Outcomes of Patients With Hypothyroidism and COVID-19: A Retrospective Cohort Study",
"author": "van Gerwen",
"doi-asserted-by": "crossref",
"first-page": "565",
"journal-title": "Frontiers in endocrinology",
"key": "10.1016/j.jtemb.2022.127055_bib81",
"volume": "11",
"year": "2020"
}
],
"reference-count": 81,
"references-count": 81,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S0946672X22001353"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Inorganic Chemistry",
"Molecular Medicine",
"Biochemistry"
],
"subtitle": [],
"title": "Association of Trace Element Status in COVID-19 Patients with Disease Severity",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy"
}
