Zinc Supplementation Associated With a Decrease in Mortality in COVID-19 Patients: A Meta-Analysis
et al., Cureus, doi:10.7759/cureus.40231, Jun 2023
Zinc for COVID-19
2nd treatment shown to reduce risk in
July 2020, now with p = 0.00000019 from 42 studies, recognized in 23 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
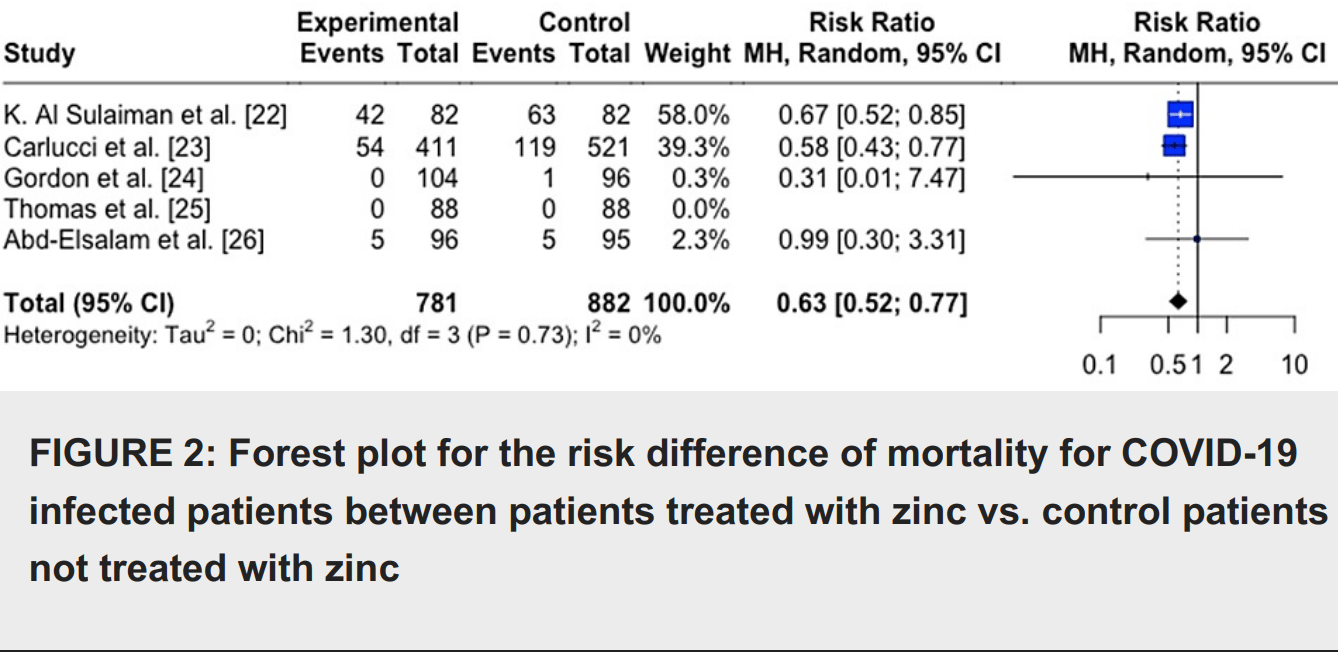
Meta analysis showing lower mortality in COVID-19 patients with zinc treatment.
Currently there are 42 zinc treatment for COVID-19 studies, showing 33% lower mortality [15‑47%], 40% lower ventilation [-1‑65%], 28% lower ICU admission [-8‑51%], 23% lower hospitalization [6‑38%], and 22% fewer cases [-10‑45%].
|
risk of death, 37.0% lower, RR 0.63, p < 0.001.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Tabatabaeizadeh, S., Zinc supplementation and COVID-19 mortality: a meta-analysis, European Journal of Medical Research, doi:10.1186/s40001-022-00694-z.
2.
Olczak-Pruc et al., The effect of zinc supplementation on the course of COVID-19 – A systematic review and meta-analysis, Annals of Agricultural and Environmental Medicine, doi:10.26444/aaem/155846.
3.
Xie et al., Micronutrient perspective on COVID-19: Umbrella review and reanalysis of meta-analyses, Critical Reviews in Food Science and Nutrition, doi:10.1080/10408398.2023.2174948.
4.
Abuhelwa, Z., Do Zinc Supplements Reduce Mortality in Patients with COVID-19?, Translation: The University of Toledo Journal of Medical Sciences, doi:10.46570/utjms.vol11-2023-749.
5.
Rheingold et al., Zinc Supplementation Associated With a Decrease in Mortality in COVID-19 Patients: A Meta-Analysis, Cureus, doi:10.7759/cureus.40231.
Rheingold et al., 10 Jun 2023, peer-reviewed, 4 authors.
Contact: patrick@nova.edu.
Zinc Supplementation Associated With a Decrease in Mortality in COVID-19 Patients: A Meta-Analysis
Cureus, doi:10.7759/cureus.40231
The COVID-19 pandemic has had a significant impact on the world, resulting in millions of deaths worldwide and imposing economic, political, and social problems. The use of nutritional supplementation for the prevention and mitigation of COVID-19 remains controversial. This meta-analysis aims to investigate the association between zinc supplementation, mortality, and symptomatology, among COVID-19-infected patients. A meta-analysis was conducted to compare the outcomes of mortality and symptomology of patients with COVID-19 receiving zinc supplementation and those not receiving zinc supplementation. PubMed/Medline, Cochrane, Web of Science, and CINAHL Complete were independently searched with the search terms "zinc" AND "covid" OR "sars-cov-2" "COVID-19" OR "coronavirus". After duplicates were removed, 1215 articles were identified. Five of these studies were used to assess mortality outcomes, and two were used to assess symptomatology outcomes. The meta-analysis was conducted through R 4.2.1 software (R Foundation, Vienna, Austria). Heterogeneity was evaluated by calculating the I 2 index. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were used. It was found that COVID-19-infected individuals treated with zinc supplements had a reduced risk of mortality compared with individuals not treated with a zinc supplement RR=0.63 (95%CI;0.52,0.77), p=0.005. For symptomology, it was found that COVID-19-infected individuals treated with zinc had no difference in symptomology than individuals not treated with a zinc supplement RR=0.52 (95%CI;0.00,24315.42), p=0.578. This data indicates that zinc supplementation is associated with decreased mortality in those with COVID-19 but does not change symptomatology. This is promising as zinc is widely available and may be valuable as a cost-effective way to prevent poor outcomes for those with COVID-19.
Additional Information
Disclosures
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
References
Abd-Elsalam, Soliman, Esmail, Do zinc supplements enhance the clinical efficacy of hydroxychloroquine?: a randomized, multicenter trial, Biol Trace Elem Res, doi:10.1007/s12011-020-02512-1
Barnard, Wong, Bailey, Day, Sidwell et al., Effect of oral gavage treatment with ZnAL42 and other metallo-ion formulations on influenza A H5N1 and H1N1 virus infections in mice, Antivir Chem Chemother, doi:10.1177/095632020701800302
Carlucci, Ahuja, Petrilli, Rajagopalan, Jones et al., Zinc sulfate in combination with a zinc ionophore may improve outcomes in hospitalized COVID-19 patients, J Med Microbiol, doi:10.1099/jmm.0.001250
Decoursey, Morgan, Cherny, The voltage dependence of NADPH oxidase reveals why phagocytes need proton channels, Nature, doi:10.1038/nature01523
Devaux, Rolain, Colson, Raoult, New insights on the antiviral effects of chloroquine against coronavirus: what to expect for COVID-19?, Int J Antimicrob Agents, doi:10.1016/j.ijantimicag.2020.105938
Elezkurtaj, Greuel, Ihlow, Causes of death and comorbidities in hospitalized patients with COVID-19, Sci Rep, doi:10.1038/s41598-021-82862-5
Gammoh, Rink, Zinc in infection and inflammation, Nutrients, doi:10.3390/nu9060624
Gordon, Hardigan, A case-control study for the effectiveness of oral zinc in the prevention and mitigation of COVID-19, Front Med (Lausanne), doi:10.3389/fmed.2021.756707
Haase, Rink, Zinc signals and immune function, Biofactors, doi:10.1002/biof.1114
Hasegawa, Suzuki, Suzuki, Effects of zinc on the reactive oxygen species generating capacity of human neutrophils and on the serum opsonic activity in vitro, Luminescence, doi:10.1002/1522-7243(200009/10)15:5<321::AID-BIO605>3.0.CO;2-O
Hemilä, Zinc lozenges may shorten the duration of colds: a systematic review, Open Respir Med J, doi:10.2174/1874306401105010051
Hunter, Arentz, Goldenberg, Zinc for the prevention or treatment of acute viral respiratory tract infections in adults: a rapid systematic review and meta-analysis of randomised controlled trials, BMJ Open, doi:10.1136/bmjopen-2020-047474
Jeong, Eide, The SLC39 family of zinc transporters, Mol Aspects Med, doi:10.1016/j.mam.2012.05.011
Krenn, Gaudernak, Holzer, Lanke, Van Kuppeveld et al., 6 of 7 ionophores pyrithione and hinokitiol against picornavirus infections, J Virol, doi:10.1128/JVI.01543-08
Pormohammad, Monych, Turner, Zinc and SARS-CoV-2: a molecular modeling study of Zn interactions with RNA-dependent RNA-polymerase and 3C-like proteinase enzymes, Int J Mol Med, doi:10.3892/ijmm.2020.4790
Rink, Gabriel, Zinc and the immune system, Proc Nutr Soc, doi:10.1017/s0029665100000781
Skalny, Rink, Ajsuvakova, Zinc and respiratory tract infections: perspectives for COVID-19 (review), Int J Mol Med, doi:10.3892/ijmm.2020.4575
Speth, Carrera, Jean-Baptiste, Concentration-dependent effects of zinc on angiotensinconverting enzyme-2 activity, The FASEB Journal, doi:10.1096/fasebj.28.1_supplement.1067.4
Sulaiman, Aljuhani, Shaya, Evaluation of zinc sulfate as an adjunctive therapy in COVID-19 critically ill patients: a two center propensity-score matched study, Crit Care, doi:10.1186/s13054-021-03785-1
Szarpak, Pruc, Gasecka, Should we supplement zinc in COVID-19 patients? Evidence from a meta-analysis, Pol Arch Intern Med, doi:10.20452/pamw.16048
Tabatabaeizadeh, Zinc supplementation and COVID-19 mortality: a meta-analysis, Eur J Med Res, doi:10.1186/s40001-022-00694-z
Thomas, Patel, Bittel, Effect of high-dose zinc and ascorbic acid supplementation vs usual care on symptom length and reduction among ambulatory patients with SARS-CoV-2 infection: the Covid a to Z randomized clinical trial, JAMA Netw Open, doi:10.1001/jamanetworkopen.2021.0369
Velthuis, Van Den Worm, Sims, Baric, Snijder et al., +) inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture, PLoS Pathog, doi:10.1371/journal.ppat.1001176
Wang, Hu, Hu, Zinc supplementation associated with a decrease in mortality in COVID-19 patients: a meta-analysis, JAMA, doi:10.1001/jama.2020.1585
Xue, Moyer, Peng, Wu, Hannafon et al., Chloroquine is a zinc ionophore, PLoS One, doi:10.1371/journal.pone.0109180
Yan, Zhang, Li, Xia, Guo et al., Structural basis for the recognition of SARS-CoV-2 by fulllength human ACE2, Science, doi:10.1126/science.abb2762
Yasui, Yasui, Suzuki, Analysis of the predictive factors for a critical illness of COVID-19 during treatment relationship between serum zinc level and critical illness of COVID-19, Int J Infect Dis, doi:10.1016/j.ijid.2020.09.008
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet, doi:10.1016/S0140-6736(20)30566-3
DOI record:
{
"DOI": "10.7759/cureus.40231",
"ISSN": [
"2168-8184"
],
"URL": "http://dx.doi.org/10.7759/cureus.40231",
"author": [
{
"affiliation": [],
"family": "Rheingold",
"given": "Spencer Z",
"sequence": "first"
},
{
"affiliation": [],
"family": "Raval",
"given": "Chirag",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gordon",
"given": "Antonio M",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hardigan",
"given": "Patrick",
"sequence": "additional"
}
],
"container-title": "Cureus",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
6,
10
]
],
"date-time": "2023-06-10T20:27:10Z",
"timestamp": 1686428830000
},
"deposited": {
"date-parts": [
[
2023,
6,
10
]
],
"date-time": "2023-06-10T20:27:15Z",
"timestamp": 1686428835000
},
"indexed": {
"date-parts": [
[
2023,
6,
11
]
],
"date-time": "2023-06-11T04:17:48Z",
"timestamp": 1686457068368
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
6,
10
]
]
},
"language": "en",
"link": [
{
"URL": "https://www.cureus.com/articles/141805-zinc-supplementation-associated-with-a-decrease-in-mortality-in-covid-19-patients-a-meta-analysis",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.7759",
"published": {
"date-parts": [
[
2023,
6,
10
]
]
},
"published-print": {
"date-parts": [
[
2023,
6,
10
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"key": "ref1",
"unstructured": "WHO coronavirus (COVID-19) dashboard. (2022). Accessed. August 14, 2022: https://covid19.who.int/."
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"article-title": "Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study",
"author": "Zhou F",
"doi-asserted-by": "publisher",
"journal-title": "Lancet",
"key": "ref2",
"unstructured": "Zhou F, Yu T, Du R, et al.. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020, 395:1054-62. 10.1016/S0140-6736(20)30566-3",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.1585",
"article-title": "Zinc supplementation associated with a decrease in mortality in COVID-19 patients: a meta-analysis",
"author": "Wang D",
"doi-asserted-by": "publisher",
"journal-title": "JAMA",
"key": "ref3",
"unstructured": "Wang D, Hu B, Hu C, et al.. Zinc supplementation associated with a decrease in mortality in COVID-19 patients: a meta-analysis. JAMA. 2020, 323:1061-9. 10.1001/jama.2020.1585",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.09.008",
"article-title": "Analysis of the predictive factors for a critical illness of COVID-19 during treatment-relationship between serum zinc level and critical illness of COVID-19",
"author": "Yasui Y",
"doi-asserted-by": "publisher",
"journal-title": "Int J Infect Dis",
"key": "ref4",
"unstructured": "Yasui Y, Yasui H, Suzuki K, et al.. Analysis of the predictive factors for a critical illness of COVID-19 during treatment-relationship between serum zinc level and critical illness of COVID-19. Int J Infect Dis. 2020, 100:230-6. 10.1016/j.ijid.2020.09.008",
"volume": "100",
"year": "2020"
},
{
"DOI": "10.3390/nu9060624",
"article-title": "Zinc in infection and inflammation",
"author": "Gammoh NZ",
"doi-asserted-by": "publisher",
"journal-title": "Nutrients",
"key": "ref5",
"unstructured": "Gammoh NZ, Rink L. Zinc in infection and inflammation. Nutrients. 2017, 9:624. 10.3390/nu9060624",
"volume": "9",
"year": "2017"
},
{
"DOI": "10.1017/s0029665100000781",
"article-title": "Zinc and the immune system",
"author": "Rink L",
"doi-asserted-by": "publisher",
"journal-title": "Proc Nutr Soc",
"key": "ref6",
"unstructured": "Rink L, Gabriel P. Zinc and the immune system. Proc Nutr Soc. 2000, 59:541-52. 10.1017/s0029665100000781",
"volume": "59",
"year": "2000"
},
{
"article-title": "Dietary Reference Intakes: Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc",
"author": "Institute of Medicine (US) Panel on Micronutrients",
"key": "ref7",
"unstructured": "Institute of Medicine (US) Panel on Micronutrients. Dietary Reference Intakes: Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. National Academy Press, Washington, DC; 2001.",
"year": "2001"
},
{
"DOI": "10.1038/nature01523",
"article-title": "The voltage dependence of NADPH oxidase reveals why phagocytes need proton channels",
"author": "DeCoursey TE",
"doi-asserted-by": "publisher",
"journal-title": "Nature",
"key": "ref8",
"unstructured": "DeCoursey TE, Morgan D, Cherny VV. The voltage dependence of NADPH oxidase reveals why phagocytes need proton channels. Nature. 2003, 422:531-4. 10.1038/nature01523",
"volume": "422",
"year": "2003"
},
{
"DOI": "10.1002/1522-7243(200009/10)15:5<321::AID-BIO605>3.0.CO;2-O",
"article-title": "Effects of zinc on the reactive oxygen species generating capacity of human neutrophils and on the serum opsonic activity in vitro",
"author": "Hasegawa H",
"doi-asserted-by": "publisher",
"journal-title": "Luminescence",
"key": "ref9",
"unstructured": "Hasegawa H, Suzuki K, Suzuki K, et al.. Effects of zinc on the reactive oxygen species generating capacity of human neutrophils and on the serum opsonic activity in vitro. Luminescence. 2000, 15:321-7. 10.1002/1522-7243(200009/10)15:5<321::AID-BIO605>3.0.CO;2-O",
"volume": "15",
"year": "2000"
},
{
"DOI": "10.1016/j.mam.2012.05.011",
"article-title": "The SLC39 family of zinc transporters",
"author": "Jeong J",
"doi-asserted-by": "publisher",
"journal-title": "Mol Aspects Med",
"key": "ref10",
"unstructured": "Jeong J, Eide DJ. The SLC39 family of zinc transporters. Mol Aspects Med. 2013, 34:612-9. 10.1016/j.mam.2012.05.011",
"volume": "34",
"year": "2013"
},
{
"DOI": "10.1002/biof.1114",
"article-title": "Zinc signals and immune function",
"author": "Haase H",
"doi-asserted-by": "publisher",
"journal-title": "Biofactors",
"key": "ref11",
"unstructured": "Haase H, Rink L. Zinc signals and immune function. Biofactors. 2014, 40:27-40. 10.1002/biof.1114",
"volume": "40",
"year": "2014"
},
{
"DOI": "10.3892/ijmm.2020.4575",
"article-title": "Zinc and respiratory tract infections: perspectives for COVID‑19 (review)",
"author": "Skalny AV",
"doi-asserted-by": "publisher",
"journal-title": "Int J Mol Med",
"key": "ref12",
"unstructured": "Skalny AV, Rink L, Ajsuvakova OP, et al.. Zinc and respiratory tract infections: perspectives for COVID‑19 (review). Int J Mol Med. 2020, 46:17-26. 10.3892/ijmm.2020.4575",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1128/JVI.01543-08",
"article-title": "Antiviral activity of the zinc ionophores pyrithione and hinokitiol against picornavirus infections",
"author": "Krenn BM",
"doi-asserted-by": "publisher",
"journal-title": "J Virol",
"key": "ref13",
"unstructured": "Krenn BM, Gaudernak E, Holzer B, Lanke K, Van Kuppeveld FJ, Seipelt J. Antiviral activity of the zinc ionophores pyrithione and hinokitiol against picornavirus infections. J Virol. 2009, 83:58-64. 10.1128/JVI.01543-08",
"volume": "83",
"year": "2009"
},
{
"DOI": "10.2174/1874306401105010051",
"article-title": "Zinc lozenges may shorten the duration of colds: a systematic review",
"author": "Hemilä H",
"doi-asserted-by": "publisher",
"journal-title": "Open Respir Med J",
"key": "ref14",
"unstructured": "Hemilä H. Zinc lozenges may shorten the duration of colds: a systematic review. Open Respir Med J. 2011, 5:51-8. 10.2174/1874306401105010051",
"volume": "5",
"year": "2011"
},
{
"DOI": "10.1177/095632020701800302",
"article-title": "Effect of oral gavage treatment with ZnAL42 and other metallo-ion formulations on influenza A H5N1 and H1N1 virus infections in mice",
"author": "Barnard DL",
"doi-asserted-by": "publisher",
"journal-title": "Antivir Chem Chemother",
"key": "ref15",
"unstructured": "Barnard DL, Wong MH, Bailey K, Day CW, Sidwell RW, Hickok SS, Hall TJ. Effect of oral gavage treatment with ZnAL42 and other metallo-ion formulations on influenza A H5N1 and H1N1 virus infections in mice. Antivir Chem Chemother. 2007, 18:125-32. 10.1177/095632020701800302",
"volume": "18",
"year": "2007"
},
{
"DOI": "10.1371/journal.ppat.1001176",
"article-title": "Zn(2+) inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture",
"author": "te Velthuis AJ",
"doi-asserted-by": "publisher",
"journal-title": "PLoS Pathog",
"key": "ref16",
"unstructured": "te Velthuis AJ, van den Worm SH, Sims AC, Baric RS, Snijder EJ, van Hemert MJ. Zn(2+) inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture. PLoS Pathog. 2010, 6:e1001176. 10.1371/journal.ppat.1001176",
"volume": "6",
"year": "2010"
},
{
"DOI": "10.3892/ijmm.2020.4790",
"article-title": "Zinc and SARS‑CoV‑2: a molecular modeling study of Zn interactions with RNA‑dependent RNA‑polymerase and 3C‑like proteinase enzymes",
"author": "Pormohammad A",
"doi-asserted-by": "publisher",
"journal-title": "Int J Mol Med",
"key": "ref17",
"unstructured": "Pormohammad A, Monych NK, Turner RJ. Zinc and SARS‑CoV‑2: a molecular modeling study of Zn interactions with RNA‑dependent RNA‑polymerase and 3C‑like proteinase enzymes. Int J Mol Med. 2021, 47:326-34. 10.3892/ijmm.2020.4790",
"volume": "47",
"year": "2021"
},
{
"DOI": "10.1126/science.abb2762",
"article-title": "Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2",
"author": "Yan R",
"doi-asserted-by": "publisher",
"journal-title": "Science",
"key": "ref18",
"unstructured": "Yan R, Zhang Y, Li Y, Xia L, Guo Y, Zhou Q. Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science. 2020, 367:1444-8. 10.1126/science.abb2762",
"volume": "367",
"year": "2020"
},
{
"DOI": "10.1096/fasebj.28.1_supplement.1067.4",
"article-title": "Concentration-dependent effects of zinc on angiotensin-converting enzyme-2 activity",
"author": "Speth R",
"doi-asserted-by": "publisher",
"journal-title": "The FASEB Journal",
"key": "ref19",
"unstructured": "Speth R, Carrera E, Jean-Baptiste M, et al.. Concentration-dependent effects of zinc on angiotensin-converting enzyme-2 activity. The FASEB Journal. 2014, 28:1067-4. 10.1096/fasebj.28.1_supplement.1067.4",
"volume": "28",
"year": "2014"
},
{
"DOI": "10.1371/journal.pone.0109180",
"article-title": "Chloroquine is a zinc ionophore",
"author": "Xue J",
"doi-asserted-by": "publisher",
"journal-title": "PLoS One",
"key": "ref20",
"unstructured": "Xue J, Moyer A, Peng B, Wu J, Hannafon BN, Ding WQ. Chloroquine is a zinc ionophore. PLoS One. 2014, 9:e109180. 10.1371/journal.pone.0109180",
"volume": "9",
"year": "2014"
},
{
"DOI": "10.1016/j.ijantimicag.2020.105938",
"article-title": "New insights on the antiviral effects of chloroquine against coronavirus: what to expect for COVID-19?",
"author": "Devaux CA",
"doi-asserted-by": "publisher",
"journal-title": "Int J Antimicrob Agents",
"key": "ref21",
"unstructured": "Devaux CA, Rolain JM, Colson P, Raoult D. New insights on the antiviral effects of chloroquine against coronavirus: what to expect for COVID-19?. Int J Antimicrob Agents. 2020, 55:105938. 10.1016/j.ijantimicag.2020.105938",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.1186/s13054-021-03785-1",
"article-title": "Evaluation of zinc sulfate as an adjunctive therapy in COVID-19 critically ill patients: a two center propensity-score matched study",
"author": "Al Sulaiman K",
"doi-asserted-by": "publisher",
"journal-title": "Crit Care",
"key": "ref22",
"unstructured": "Al Sulaiman K, Aljuhani O, Al Shaya AI, et al.. Evaluation of zinc sulfate as an adjunctive therapy in COVID-19 critically ill patients: a two center propensity-score matched study. Crit Care. 2021, 25:363. 10.1186/s13054-021-03785-1",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.1099/jmm.0.001250",
"article-title": "Zinc sulfate in combination with a zinc ionophore may improve outcomes in hospitalized COVID-19 patients",
"author": "Carlucci PM",
"doi-asserted-by": "publisher",
"journal-title": "J Med Microbiol",
"key": "ref23",
"unstructured": "Carlucci PM, Ahuja T, Petrilli C, Rajagopalan H, Jones S, Rahimian J. Zinc sulfate in combination with a zinc ionophore may improve outcomes in hospitalized COVID-19 patients. J Med Microbiol. 2020, 69:1228-34. 10.1099/jmm.0.001250",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.3389/fmed.2021.756707",
"article-title": "A case-control study for the effectiveness of oral zinc in the prevention and mitigation of COVID-19",
"author": "Gordon AM",
"doi-asserted-by": "publisher",
"journal-title": "Front Med (Lausanne)",
"key": "ref24",
"unstructured": "Gordon AM, Hardigan PC. A case-control study for the effectiveness of oral zinc in the prevention and mitigation of COVID-19. Front Med (Lausanne). 2021, 8:756707. 10.3389/fmed.2021.756707",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.0369",
"article-title": "Effect of high-dose zinc and ascorbic acid supplementation vs usual care on symptom length and reduction among ambulatory patients with SARS-CoV-2 infection: the Covid a to Z randomized clinical trial",
"author": "Thomas S",
"doi-asserted-by": "publisher",
"journal-title": "JAMA Netw Open",
"key": "ref25",
"unstructured": "Thomas S, Patel D, Bittel B, et al.. Effect of high-dose zinc and ascorbic acid supplementation vs usual care on symptom length and reduction among ambulatory patients with SARS-CoV-2 infection: the Covid a to Z randomized clinical trial. JAMA Netw Open. 2021, 4:e210369. 10.1001/jamanetworkopen.2021.0369",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1007/s12011-020-02512-1",
"article-title": "Do zinc supplements enhance the clinical efficacy of hydroxychloroquine?: a randomized, multicenter trial",
"author": "Abd-Elsalam S",
"doi-asserted-by": "publisher",
"journal-title": "Biol Trace Elem Res",
"key": "ref26",
"unstructured": "Abd-Elsalam S, Soliman S, Esmail ES, et al.. Do zinc supplements enhance the clinical efficacy of hydroxychloroquine?: a randomized, multicenter trial. Biol Trace Elem Res. 2021, 199:3642-6. 10.1007/s12011-020-02512-1",
"volume": "199",
"year": "2021"
},
{
"DOI": "10.1038/s41598-021-82862-5",
"article-title": "Causes of death and comorbidities in hospitalized patients with COVID-19",
"author": "Elezkurtaj S",
"doi-asserted-by": "publisher",
"journal-title": "Sci Rep",
"key": "ref27",
"unstructured": "Elezkurtaj S, Greuel S, Ihlow J, et al.. Causes of death and comorbidities in hospitalized patients with COVID-19. Sci Rep. 2021, 11:4263. 10.1038/s41598-021-82862-5",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1186/s40001-022-00694-z",
"article-title": "Zinc supplementation and COVID-19 mortality: a meta-analysis",
"author": "Tabatabaeizadeh SA",
"doi-asserted-by": "publisher",
"journal-title": "Eur J Med Res",
"key": "ref28",
"unstructured": "Tabatabaeizadeh SA. Zinc supplementation and COVID-19 mortality: a meta-analysis. Eur J Med Res. 2022, 27:70. 10.1186/s40001-022-00694-z",
"volume": "27",
"year": "2022"
},
{
"DOI": "10.20452/pamw.16048",
"article-title": "Should we supplement zinc in COVID-19 patients? Evidence from a meta-analysis",
"author": "Szarpak L",
"doi-asserted-by": "publisher",
"journal-title": "Pol Arch Intern Med",
"key": "ref29",
"unstructured": "Szarpak L, Pruc M, Gasecka A, et al.. Should we supplement zinc in COVID-19 patients? Evidence from a meta-analysis. Pol Arch Intern Med. 2021, 131:802-7. 10.20452/pamw.16048",
"volume": "131",
"year": "2021"
},
{
"DOI": "10.1136/bmjopen-2020-047474",
"article-title": "Zinc for the prevention or treatment of acute viral respiratory tract infections in adults: a rapid systematic review and meta-analysis of randomised controlled trials",
"author": "Hunter J",
"doi-asserted-by": "publisher",
"journal-title": "BMJ Open",
"key": "ref30",
"unstructured": "Hunter J, Arentz S, Goldenberg J, et al.. Zinc for the prevention or treatment of acute viral respiratory tract infections in adults: a rapid systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2021, 11:e047474. 10.1136/bmjopen-2020-047474",
"volume": "11",
"year": "2021"
}
],
"reference-count": 30,
"references-count": 30,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.cureus.com/articles/141805-zinc-supplementation-associated-with-a-decrease-in-mortality-in-covid-19-patients-a-meta-analysis"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Aerospace Engineering"
],
"subtitle": [],
"title": "Zinc Supplementation Associated With a Decrease in Mortality in COVID-19 Patients: A Meta-Analysis",
"type": "journal-article"
}
