A Case-Control Study for the Effectiveness of Oral Zinc in the Prevention and Mitigation of COVID-19
et al., Frontiers in Medicine, doi:10.3389/fmed.2021.756707, Dec 2021
Zinc for COVID-19
2nd treatment shown to reduce risk in
July 2020, now with p = 0.00000019 from 42 studies, recognized in 23 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Prospective study of zinc supplementation with 104 patients randomized to receive 10mg, 25mg, or 50mg of zinc picolinate daily, and a matched sample of 96 control patients from the adjacent clinic that did not routinely recommend/use zinc, showing significantly lower symptomatic COVID-19 with treatment.
The treatment group was monitored via telemedicine every 2-3 weeks, whereas the control group was a retrospective cohort checked via front-desk questionnaires, introducing ascertainment bias.
The reported p-value of 0.999 for cardiovascular disease in Table 1 is incorrect.
In Table 2, the number of missing values for HgbA1c in the treatment group is reported as 132, which is larger than the group size.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 67.6% lower, RR 0.32, p = 0.48, treatment 0 of 104 (0.0%), control 1 of 96 (1.0%), NNT 96, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm).
|
|
risk of symptomatic case, 85.3% lower, RR 0.15, p = 0.02, treatment 2 of 104 (1.9%), control 9 of 96 (9.4%), NNT 13, adjusted per study, inverted to make RR<1 favor treatment, odds ratio converted to relative risk.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Gordon et al., 13 Dec 2021, prospective, USA, peer-reviewed, 2 authors.
A Case-Control Study for the Effectiveness of Oral Zinc in the Prevention and Mitigation of COVID-19
Frontiers in Medicine, doi:10.3389/fmed.2021.756707
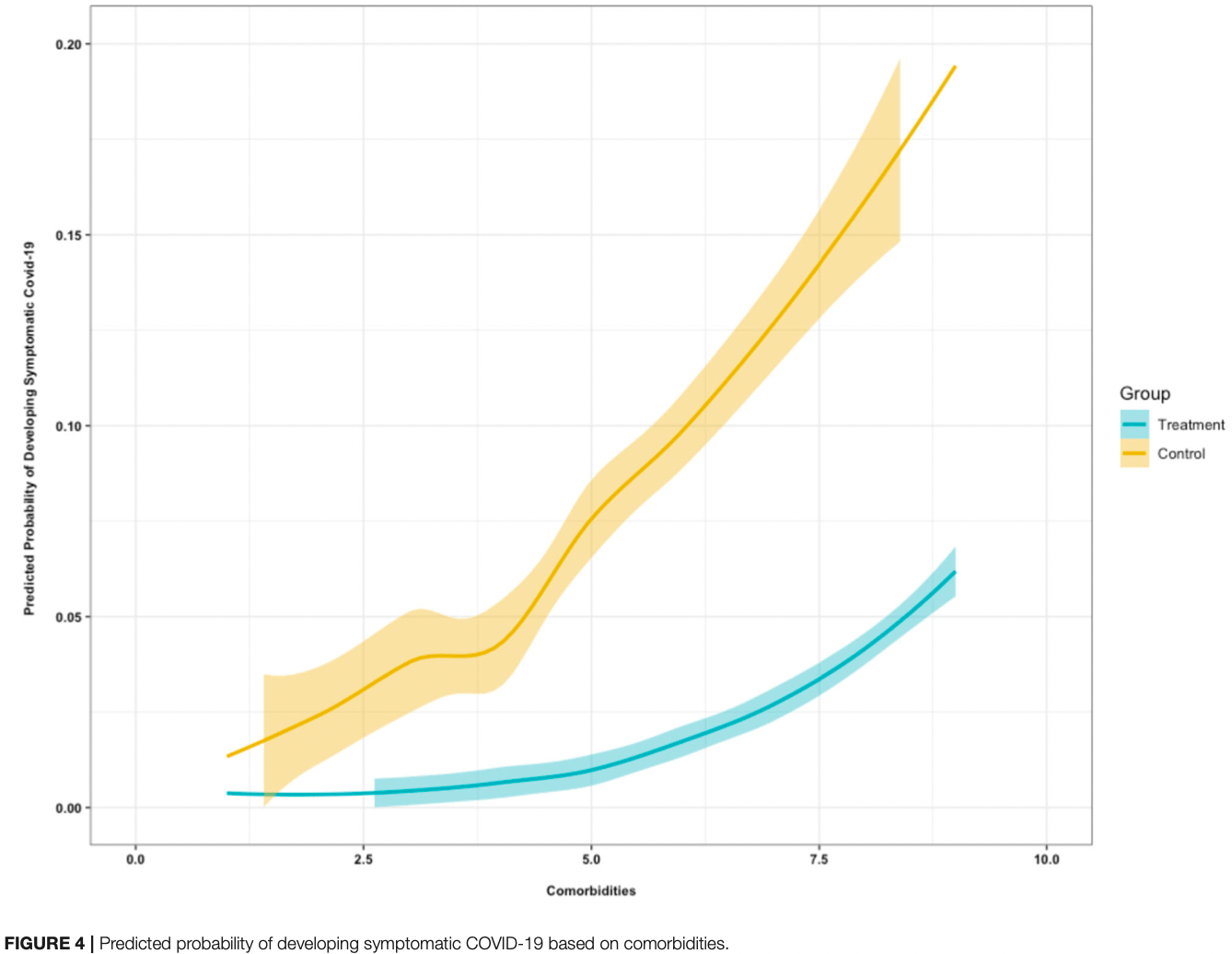
Background: The ongoing coronavirus disease-19 (COVID-19) pandemic (caused by an infection with severe acute respiratory syndrome (SARS)-coronavirus (CoV-2) has put a burden on the medical community and society at large. Efforts to reduce the disease burden and mortality over the course of the pandemic have focused on research to rapidly determine age-stratified seroepidemiologic surveys, a centralized research program to fast-track the most promising rapid diagnostics and serologic assays, and the testing of potential anti-viral agents, immunologic therapies, and vaccine candidates. Despite the lack of official recognition for the role of nutrition in the fight against COVID-19 infection, multiple groups proposed zinc supplementation as an adjuvant for the management of participants. Method: In an ambulatory, interventional, prospective, single-blind study, we evaluated the effectiveness of zinc supplementation in the prevention and mitigation of COVID-19 in two similar participant groups. In Clinic A (n = 104) participants were randomized to receive 10 mg, 25 mg, or 50 mg zinc picolinate daily, and Clinic B control participants paired according to their demographics and clinical parameters (n = 96). All participants were compared based on demographics, clinical comorbidities, blood counts, renal functions, vitamin D levels, and their development of symptomatic COVID-19 infection. Results: Symptomatic COVID-19 infection was significantly higher among the control group participants (N = 9, 10.4%) than the treatment participants (N = 2, 1.9%), p = 0.015. The unadjusted odds ratio indicates that symptomatic COVID-19 infection was 5.93 [95% CI: 1.51, 39.26] higher in the control group, p < 0.01. Controlling for co-morbidities, individuals in the control group were 7.38 (95% CI: 1.80, 50.28) times more likely to develop symptomatic COVID-19 infection as compared with individuals in the treatment group (p < 0.01). For every-one unit increase in the number of co-morbidities, the likelihood of developing symptomatic COVID-19 infection increased 1.57 (95% CI: 1.16, 2.19) (p = 0.01).
Discussion: The findings from our study suggest that zinc supplementation in all three doses (10, 25, and 50 mg) may be an effective prophylaxis of symptomatic COVID-19 and may mitigate the severity of COVID-19 infection.
Gordon and Hardigan
Effectiveness of Oral Zinc Conclusion: Zinc is a relatively inexpensive mineral nutrient that is an effective prophylactic agent to prevent and mitigate the potentially deadly symptomatic SARS-CoV-2 infection. As the COVID-19 pandemic continues with a lag in vaccinations in some regions and the continued emergence of dangerously infectious variants of SARS-CoV-2, it is important to replicate our data in other populations and locations and to engage public health and nutrition services on the emergent need to use zinc supplantation or fortification of staple foods in the prevention and mitigation of COVID-19 infection severity.
ETHICS STATEMENT The studies involving human participants were reviewed and approved by Sal Castaner, JD and VP of University Health Care for legal issues and compliance. The patients/participants provided their written informed consent to participate in this study.
AUTHOR CONTRIBUTIONS AG designed and implemented the study. PH performed the data analysis. All authors discussed the results and contributed to the final manuscript.
Conflict of Interest: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. Publisher's Note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abdelmaksoud, Ghweil, Hassan, Khodeary, Aref, Olfactory disturbances as presenting manifestation among egyptian patients with COVID-19: possible role of zinc, Biol Trace Elem Res, doi:10.1007/s12011-020-02546-5
Adil, Rahman, Whitelaw, Jain, Al-Taan et al., SARS-CoV-2 and the pandemic of COVID-19, Postgrad Med J, doi:10.1136/postgradmedj-2020-138386
Bernal, Andrews, Gower, Gallagher, Simmons et al., Effectiveness of covid-19 vaccines against the B.1.617.2 (Delta) variant, N Engl J Med, doi:10.1056/NEJMoa2108891
Cabrera, Zinc, aging, and immunosenescence: an overview, Pathobiol Aging Age Relat Dis, doi:10.3402/pba.v5.25592
Calder, Nutrition, immunity, and COVID-19, BMJ Nutr Prevent Health, doi:10.1136/bmjnph-2020-000085
Chisholm, Martin, Hypozincemia, ageusia dysgeusia and toilet tissue pica, J Natl Med Assoc
Diaz-Curiel, Cabello, Arboiro-Pinel, Mansur, Heili-Frades et al., The relationship between 25(OH) vitamin D levels and COVID-19 onset and disease course in Spanish participants, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2021.105928
Gasmi, Peana, Pivina, Srinath, Benahmed et al., Interrelations between COVID-19 and other disorders, Clin Immunol, doi:10.1016/j.clim.2020.108651
Hemila, Chalker, Vitamin C and zinc lozenges for COVID-19?, J Am Pharm Assoc, doi:10.1016/j.japh.2021.05.018
Hyams, Marlow, Maseko, King, Ward et al., Effectiveness of BNT162b2 and ChAdOx1 nCoV-19 COVID-19 vaccination at preventing hospitalizations in people aged at least 80 years: a test-negative, case-control study, Lancet Infect Dis, doi:10.1016/S1473-3099(21)00330-3
Mariani, Neri, Cattini, Mocchegiani, Malavolta et al., Effect of zinc supplementation on plasma IL-6 and MCP-1 production and NK cell function in healthy elderly: interactive influence of +647 MT1a and−174 IL-6 polymorphic alleles, Exp Gerontol, doi:10.1016/j.exger.2007.12.003
Marreiro, Cruz, Oliveira, Morais, Freitas et al., Antiviral and immunological activity of zinc and possible role in COVID-19, Br J Nutr, doi:10.1017/S0007114521002099
Matteo, Giovanni, The malnutritional status of the host as a virulence factor for new coronavirus SARS-CoV-2, Front Med, doi:10.3389/fmed.2020.00146
Mayor-Ibarguren, Busca-Arenzana, Robles-Marhuenda, A hypothesis for the possible role of zinc in the immunological pathways related to COVID-19 infection, Front Immunol, doi:10.3389/fimmu.2020.01736
Mcmillan, Rowe, Clinical significance of diurnal variation in the estimation of plasma zinc, Clin Exp Derm, doi:10.1111/j.1365-2230.1982.tb02488.x
Mocchegiani, Romeo, Malavolta, Costarelli, Giacconi et al., Zinc: dietary intake and impact of supplementation on immune function in elderly, Age, doi:10.1007/s11357-011-9377-3
Pathania, Bhardwaj, Pathania, Rathaur, Amisha, A review on exploring evidence-based approach to harnessing the immune system in times of corona virus pandemic: Best of modern and traditional Indian system of medicine, J Fam Med Prim Care, doi:10.4103/jfmpc.jfmpc_504_20
Perera, Khoury, Chinni, Bolton, Qu et al., Randomised controlled trial for high-dose intravenous zinc as adjunctive therapy in SARS-CoV-2 (COVID-19) positive critically ill participants: trial protocol, BMJ Open, doi:10.1136/bmjopen-2020-040580
Prasad, Discovery of human zinc deficiency: its impact on human health and disease, Adv Nutr, doi:10.3945/an.112.003210
Rani, Goyal, Bhatnagar, Manhas, Goel et al., Potential molecular mechanisms of zinc-and copper-mediated antiviral activity on COVID-19, Nutr Res, doi:10.1016/j.nutres.2021.05.008
Skalny, Rink, Ajsuvakova, Aschner, Gritsenko et al., Zinc and respiratory tract infections: perspectives for COVID-19
Trujillo-Mayol, Guerra-Valle, Casas-Forero Nidia, Sobral, Viegas, Western dietary pattern antioxidant intakes and oxidative stress: importance during the SARS-CoV-2/COVID-19 pandemic, Adv Nutr, doi:10.1093/advances/nmaa171
Velthuis, Van Den Worm, Sims, Baric, Snijder et al., Zn2+ Inhibits coronavirus and arterivirus rna polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture, PLoS Pathogens, doi:10.1371/journal.ppat.1001176
Who, None
Yasui, Yasui, Suzuki, Saitou, Yamamoto et al., Analysis of the predictive factors for a critical illness of COVID-19 during treatmentrelationship between serum zinc level and critical illness of COVID-19, Int J Infect Dis, doi:10.1016/j.ijid.2020.09.008
Zhang, Wu, Li, Zhao, Wang, Cytokine release syndrome in severe COVID-19: interleukin-6 receptor antagonist tocilizumab may be the key to reduce mortality, Int J Antimicrob Agents, doi:10.1016/j.ijantimicag.2020.105954
DOI record:
{
"DOI": "10.3389/fmed.2021.756707",
"ISSN": [
"2296-858X"
],
"URL": "http://dx.doi.org/10.3389/fmed.2021.756707",
"abstract": "<jats:p><jats:bold>Background:</jats:bold> The ongoing coronavirus disease-19 (COVID-19) pandemic (caused by an infection with severe acute respiratory syndrome (SARS)-coronavirus (CoV-2) has put a burden on the medical community and society at large. Efforts to reduce the disease burden and mortality over the course of the pandemic have focused on research to rapidly determine age-stratified seroepidemiologic surveys, a centralized research program to fast-track the most promising rapid diagnostics and serologic assays, and the testing of potential anti-viral agents, immunologic therapies, and vaccine candidates. Despite the lack of official recognition for the role of nutrition in the fight against COVID-19 infection, multiple groups proposed zinc supplementation as an adjuvant for the management of participants.</jats:p><jats:p><jats:bold>Method:</jats:bold> In an ambulatory, interventional, prospective, single-blind study, we evaluated the effectiveness of zinc supplementation in the prevention and mitigation of COVID-19 in two similar participant groups. In Clinic A (<jats:italic>n</jats:italic> = 104) participants were randomized to receive 10 mg, 25 mg, or 50 mg zinc picolinate daily, and Clinic B control participants paired according to their demographics and clinical parameters (<jats:italic>n</jats:italic> = 96). All participants were compared based on demographics, clinical comorbidities, blood counts, renal functions, vitamin D levels, and their development of symptomatic COVID-19 infection.</jats:p><jats:p><jats:bold>Results:</jats:bold> Symptomatic COVID-19 infection was significantly higher among the control group participants (<jats:italic>N</jats:italic> = 9, 10.4%) than the treatment participants (<jats:italic>N</jats:italic> = 2, 1.9%), <jats:italic>p</jats:italic> = 0.015. The unadjusted odds ratio indicates that symptomatic COVID-19 infection was 5.93 [95% CI: 1.51, 39.26] higher in the control group, <jats:italic>p</jats:italic> &lt; 0.01. Controlling for co-morbidities, individuals in the control group were 7.38 (95% CI: 1.80, 50.28) times more likely to develop symptomatic COVID-19 infection as compared with individuals in the treatment group (<jats:italic>p</jats:italic> &lt; 0.01). For every-one unit increase in the number of co-morbidities, the likelihood of developing symptomatic COVID-19 infection increased 1.57 (95% CI: 1.16, 2.19) (<jats:italic>p</jats:italic> = 0.01).</jats:p><jats:p><jats:bold>Discussion:</jats:bold> The findings from our study suggest that zinc supplementation in all three doses (10, 25, and 50 mg) may be an effective prophylaxis of symptomatic COVID-19 and may mitigate the severity of COVID-19 infection.</jats:p><jats:p><jats:bold>Conclusion:</jats:bold> Zinc is a relatively inexpensive mineral nutrient that is an effective prophylactic agent to prevent and mitigate the potentially deadly symptomatic SARS-CoV-2 infection. As the COVID-19 pandemic continues with a lag in vaccinations in some regions and the continued emergence of dangerously infectious variants of SARS-CoV-2, it is important to replicate our data in other populations and locations and to engage public health and nutrition services on the emergent need to use zinc supplantation or fortification of staple foods in the prevention and mitigation of COVID-19 infection severity.</jats:p>",
"alternative-id": [
"10.3389/fmed.2021.756707"
],
"author": [
{
"affiliation": [],
"family": "Gordon",
"given": "Antonio M.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Hardigan",
"given": "Patrick C.",
"sequence": "additional"
}
],
"container-title": [
"Frontiers in Medicine"
],
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2021,
12,
13
]
],
"date-time": "2021-12-13T05:13:28Z",
"timestamp": 1639372408000
},
"deposited": {
"date-parts": [
[
2021,
12,
13
]
],
"date-time": "2021-12-13T05:13:31Z",
"timestamp": 1639372411000
},
"indexed": {
"date-parts": [
[
2021,
12,
21
]
],
"date-time": "2021-12-21T13:54:19Z",
"timestamp": 1640094859412
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "electronic",
"value": "2296-858X"
}
],
"issued": {
"date-parts": [
[
2021,
12,
13
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
12,
13
]
],
"date-time": "2021-12-13T00:00:00Z",
"timestamp": 1639353600000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fmed.2021.756707/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2021,
12,
13
]
]
},
"published-online": {
"date-parts": [
[
2021,
12,
13
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"key": "B1",
"unstructured": "2021"
},
{
"DOI": "10.1136/postgradmedj-2020-138386",
"article-title": "SARS-CoV-2 and the pandemic of COVID-19",
"author": "Adil",
"doi-asserted-by": "publisher",
"first-page": "110",
"journal-title": "Postgrad Med J.",
"key": "B2",
"volume": "97",
"year": "2020"
},
{
"DOI": "10.1016/j.clim.2020.108651",
"article-title": "Interrelations between COVID-19 and other disorders",
"author": "Gasmi",
"doi-asserted-by": "publisher",
"first-page": "10865",
"journal-title": "Clin Immunol.",
"key": "B3",
"volume": "224",
"year": "2021"
},
{
"DOI": "10.1016/j.ijid.2020.09.008",
"article-title": "Analysis of the predictive factors for a critical illness of COVID-19 during treatment—relationship between serum zinc level and critical illness of COVID-19",
"author": "Yasui",
"doi-asserted-by": "publisher",
"first-page": "230",
"journal-title": "Int J Infect Dis.",
"key": "B4",
"volume": "100",
"year": "2020"
},
{
"DOI": "10.1371/journal.ppat.1001176",
"article-title": "Zn2+ Inhibits coronavirus and arterivirus rna polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture",
"author": "te Velthuis",
"doi-asserted-by": "publisher",
"first-page": "e1001176",
"journal-title": "PLoS Pathogens.",
"key": "B5",
"volume": "6",
"year": "2010"
},
{
"DOI": "10.3389/fimmu.2020.01736",
"article-title": "A hypothesis for the possible role of zinc in the immunological pathways related to COVID-19 infection",
"author": "Mayor-Ibarguren",
"doi-asserted-by": "publisher",
"first-page": "1736",
"journal-title": "Front Immunol.",
"key": "B6",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.3892/ijmm.2020.4575",
"article-title": "Zinc and respiratory tract infections: perspectives for COVID-19 (Review)",
"author": "Skalny",
"doi-asserted-by": "publisher",
"first-page": "17",
"journal-title": "Int J Mol Med.",
"key": "B7",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1016/j.jsbmb.2021.105928",
"article-title": "The relationship between 25(OH) vitamin D levels and COVID-19 onset and disease course in Spanish participants",
"author": "Diaz-Curiel",
"doi-asserted-by": "publisher",
"first-page": "105928",
"journal-title": "J Steroid Biochem Mol Biol.",
"key": "B8",
"volume": "212",
"year": "2021"
},
{
"DOI": "10.3945/an.112.003210",
"article-title": "Discovery of human zinc deficiency: its impact on human health and disease",
"author": "Prasad",
"doi-asserted-by": "publisher",
"first-page": "176",
"journal-title": "Adv Nutr.",
"key": "B9",
"volume": "4",
"year": "2013"
},
{
"DOI": "10.1136/bmjopen-2020-040580",
"article-title": "Randomised controlled trial for high-dose intravenous zinc as adjunctive therapy in SARS-CoV-2 (COVID-19) positive critically ill participants: trial protocol",
"author": "Perera",
"doi-asserted-by": "publisher",
"first-page": "e040580",
"journal-title": "BMJ Open.",
"key": "B10",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1016/S0750-7658(05)81996-3",
"doi-asserted-by": "publisher",
"first-page": "R187",
"journal-title": "Fr Ann Anesth Resuscitation.",
"key": "B11",
"volume": "11",
"year": "1992"
},
{
"DOI": "10.1016/j.ijantimicag.2020.105954",
"article-title": "Cytokine release syndrome in severe COVID-19: interleukin-6 receptor antagonist tocilizumab may be the key to reduce mortality",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "105954",
"journal-title": "Int J Antimicrob Agents.",
"key": "B12",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.1016/S1473-3099(21)00330-3",
"article-title": "Effectiveness of BNT162b2 and ChAdOx1 nCoV-19 COVID-19 vaccination at preventing hospitalizations in people aged at least 80 years: a test-negative, case-control study",
"author": "Hyams",
"doi-asserted-by": "publisher",
"first-page": "1539",
"journal-title": "Lancet Infect Dis.",
"key": "B13",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2108891",
"article-title": "Effectiveness of covid-19 vaccines against the B.1.617.2 (Delta) variant",
"author": "Bernal",
"doi-asserted-by": "publisher",
"first-page": "585",
"journal-title": "N Engl J Med.",
"key": "B14",
"volume": "385",
"year": "2021"
},
{
"DOI": "10.1016/j.japh.2021.05.018",
"article-title": "Vitamin C and zinc lozenges for COVID-19?",
"author": "Hemila",
"doi-asserted-by": "publisher",
"first-page": "e39",
"journal-title": "J Am Pharm Assoc.",
"key": "B15",
"volume": "61",
"year": "2003"
},
{
"DOI": "10.4103/jfmpc.jfmpc_504_20",
"article-title": "Amisha. A review on exploring evidence-based approach to harnessing the immune system in times of corona virus pandemic: Best of modern and traditional Indian system of medicine",
"author": "Pathania",
"doi-asserted-by": "publisher",
"first-page": "3826",
"journal-title": "J Fam Med Prim Care.",
"key": "B16",
"volume": "9",
"year": "2020"
},
{
"key": "B17",
"volume-title": "Zinc deficiency in participants with HIV/AIDS and Adjunctive Zinc therapy in AIDS participants",
"year": "1992"
},
{
"DOI": "10.1007/s11357-011-9377-3",
"article-title": "Zinc: dietary intake and impact of supplementation on immune function in elderly",
"author": "Mocchegiani",
"doi-asserted-by": "publisher",
"first-page": "839",
"journal-title": "Age.",
"key": "B18",
"volume": "35",
"year": "2012"
},
{
"DOI": "10.1093/advances/nmaa171",
"article-title": "Western dietary pattern antioxidant intakes and oxidative stress: importance during the SARS-CoV-2/COVID-19 pandemic",
"author": "Trujillo-Mayol",
"doi-asserted-by": "publisher",
"first-page": "670",
"journal-title": "Adv Nutr.",
"key": "B19",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1017/S0007114521002099",
"article-title": "Antiviral and immunological activity of zinc and possible role in COVID-19",
"author": "Marreiro",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Br J Nutr",
"key": "B20",
"year": "2021"
},
{
"DOI": "10.3389/fmed.2020.00146",
"article-title": "The malnutritional status of the host as a virulence factor for new coronavirus SARS-CoV-2",
"author": "Matteo",
"doi-asserted-by": "publisher",
"first-page": "146",
"journal-title": "Front Med.",
"key": "B21",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1016/j.exger.2007.12.003",
"article-title": "Effect of zinc supplementation on plasma IL-6 and MCP-1 production and NK cell function in healthy elderly: interactive influence of +647 MT1a and−174 IL-6 polymorphic alleles",
"author": "Mariani",
"doi-asserted-by": "publisher",
"first-page": "462",
"journal-title": "Exp Gerontol.",
"key": "B22",
"volume": "43",
"year": "2008"
},
{
"DOI": "10.1136/bmjnph-2020-000085",
"article-title": "Nutrition, immunity, and COVID-19",
"author": "Calder",
"doi-asserted-by": "publisher",
"first-page": "74",
"journal-title": "BMJ Nutr Prevent Health",
"key": "B23",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1016/j.nutres.2021.05.008",
"article-title": "Potential molecular mechanisms of zinc- and copper-mediated antiviral activity on COVID-19",
"author": "Rani",
"doi-asserted-by": "publisher",
"first-page": "109",
"journal-title": "Nutr Res.",
"key": "B24",
"volume": "92",
"year": "2021"
},
{
"DOI": "10.1007/s12011-020-02546-5",
"article-title": "Olfactory disturbances as presenting manifestation among egyptian patients with COVID-19: possible role of zinc",
"author": "Abdelmaksoud",
"doi-asserted-by": "publisher",
"first-page": "4101",
"journal-title": "Biol Trace Elem Res.",
"key": "B25",
"volume": "199",
"year": "2021"
},
{
"DOI": "10.3402/pba.v5.25592",
"article-title": "Zinc, aging, and immunosenescence: an overview",
"author": "Cabrera",
"doi-asserted-by": "publisher",
"first-page": "25592",
"journal-title": "Pathobiol Aging Age Relat Dis.",
"key": "B26",
"volume": "5",
"year": "2019"
},
{
"article-title": "Hypozincemia, ageusia dysgeusia and toilet tissue pica",
"author": "Chisholm JC",
"first-page": "163",
"journal-title": "J Natl Med Assoc.",
"key": "B27",
"volume": "73",
"year": "1981"
},
{
"DOI": "10.1111/j.1365-2230.1982.tb02488.x",
"article-title": "Clinical significance of diurnal variation in the estimation of plasma zinc",
"author": "McMillan",
"doi-asserted-by": "publisher",
"first-page": "629",
"journal-title": "Clin Exp Derm",
"key": "B28",
"volume": "7",
"year": "1982"
}
],
"reference-count": 28,
"references-count": 28,
"relation": {},
"score": 1,
"short-container-title": [
"Front. Med."
],
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": [
"A Case-Control Study for the Effectiveness of Oral Zinc in the Prevention and Mitigation of COVID-19"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "8"
}
