Evaluation of zinc, copper, and Cu:Zn ratio in serum, and their implications in the course of COVID-19
et al., Journal of Trace Elements in Medicine and Biology, doi:10.1016/j.jtemb.2022.126944, Feb 2022
Zinc for COVID-19
2nd treatment shown to reduce risk in
July 2020, now with p = 0.00000028 from 47 studies, recognized in 23 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
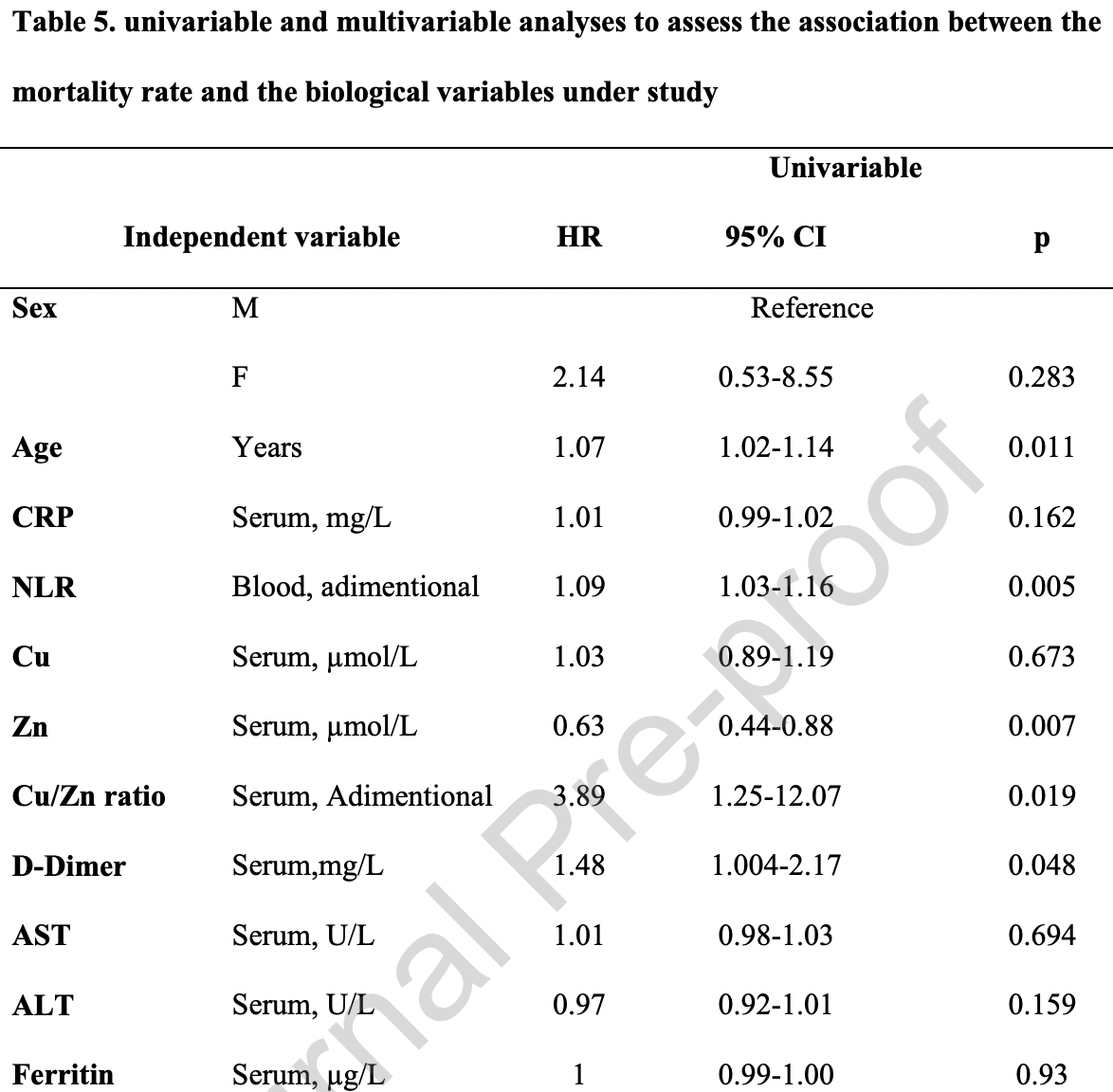
Retrospective 75 COVID-19 hospitalized patients and 68 healthy controls in Bulgaria, showing mortality associated with lower zinc levels.
Ivanova et al., 8 Feb 2022, retrospective, Bulgaria, peer-reviewed, 7 authors, study period January 2021 - April 2021.
Evaluation of zinc, copper, and Cu:Zn ratio in serum, and their implications in the course of COVID-19
Journal of Trace Elements in Medicine and Biology, doi:10.1016/j.jtemb.2022.126944
This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Table 4 Number (%) of the acute COVID-19 patients with values of the studied biological variables outside the reference range
Subjects with Acute patients n=75 (%) CRP values outside of the reference interval 66 (88%) Cu values outside of the reference interval less than the lower limit of the reference interval (<12.3 µmol/L) 9 (12%) higher than the upper limit of the reference interval (>24. less than the lower lower lower limit of the reference interval 1 (1.6%) higher than the upper upper limit of the reference interval 51 (79.7%) Ferritin values>500 µg/L 34 (53.1%)
J o u r n a l P r e -p r o o f
Authors statements The content of the paper has not been yet published or submitted for publication elsewhere. Authors also confirm that all authors have contributed significantly, and that all authors are in agreement with the content of the manuscript. Specifically, Irena Ivanova has contribute in the conceptualization, methodology, original draft, and writingreview of the revised manuscript; Ilaria Simonelli contributed in the software, data curation, statistical analyses, and visualization of the results writing of the original and revised manuscript; Amit Pal, Mauro Rongioletti and Mariacarla Ventriglia in writing -original draft, and writing -review and editing; Bisera Atanasova contributed in writing -review and editing of the revised manuscript and Rosanna Squitti contributed to the conceptualization, on writing the original draft, and writing -review and..
References
Abd-Elsalam, Soliman, Esmail, Khalaf, Mostafa et al., Do Zinc Supplements Enhance the Clinical Efficacy of Hydroxychloroquine?: a Randomized, Multicenter Trial, Biological trace element research
Anuk, Polat, Akdas, Erol, Tanacan et al., The Relation Between Trace Element Status (Zinc, Copper, Magnesium) and Clinical Outcomes in COVID-19 Infection During Pregnancy, Biological trace element research
Carlucci, Ahuja, Petrilli, Rajagopalan, Jones et al., Zinc sulfate in combination with a zinc ionophore may improve outcomes in hospitalized COVID-19 patients, J Med Microbiol
Del Giudice, Gangestad, Rethinking IL-6 and CRP: Why they are more than inflammatory biomarkers, and why it matters, Brain Behav Immun
Forget, Khalifa, Defour, Latinne, Van Pel et al., What is the normal value of the neutrophil-to-lymphocyte ratio?, BMC Res Notes
Guo, Chen, Yeh, Hsiung, Wang, Cu/Zn ratios are associated with nutritional status, oxidative stress, inflammation, and immune abnormalities in patients on peritoneal dialysis, Clinical biochemistry
Gupta, Read, Shackel, Hebbard, George et al., The Role of Micronutrients in the Infection and Subsequent Response to Hepatitis C Virus, Cells
Hackler, Heller, Sun, Schwarzer, Diegmann et al., Relation of Serum Copper Status to Survival in COVID-19, Nutrients
Heller, Sun, Hackler, Seelig, Seibert et al., Prediction of survival odds in COVID-19 by zinc, age and selenoprotein P as composite biomarker, Redox Biol
Henderson, Canna, Schulert, Volpi, Lee et al., On the Alert for Cytokine Storm: Immunopathology in COVID-19, Arthritis Rheumatol
Im, Je, Baek, Chung, Kwon et al., Nutritional status of patients with COVID-19, Int J Infect Dis
Jothimani, Kailasam, Danielraj, Nallathambi, Ramachandran et al., COVID-19: Poor outcomes in patients with zinc deficiency, Int J Infect Dis
Laine, Tuomainen, Salonen, Virtanen, Serum copper-to-zinc-ratio and risk of incident infection in men: the Kuopio Ischaemic Heart Disease Risk Factor Study, European journal of epidemiology
Malavolta, Piacenza, Basso, Giacconi, Costarelli et al., Serum copper to zinc ratio: Relationship with aging and health status, Mech Ageing Dev
Mocchegiani, Malavolta, Lattanzio, Piacenza, Basso et al., Cu to Zn ratio, physical function, disability, and mortality risk in older elderly (ilSIRENTE study), Age
Pal, Squitti, Picozza, Pawar, Rongioletti et al., Zinc and COVID-19: Basis of Current Clinical Trials, Biological trace element research
Pereira, Campos, Bogo, Copper toxicology, oxidative stress and inflammation using zebrafish as experimental model, J Appl Toxicol
Rakotoarimanana, Nutrition and infection, Rev Med Suisse
Rani, Goyal, Bhatnagar, Manhas, Goel et al., Potential molecular mechanisms of zinc-and copper-mediated antiviral activity on COVID-19, Nutr Res
Read, Obeid, Ahlenstiel, Ahlenstiel, The Role of Zinc in Antiviral Immunity, Adv Nutr
Ribeiro, Moya, Braga, Domenici, Feitosa et al., Copper-Zinc ratio and nutritional status in colorectal cancer patients during the perioperative period, Acta Cir Bras
Richardson, Lovegrove, Nutritional status of micronutrients as a possible and modifiable risk factor for COVID-19: a UK perspective, Br J Nutr
Scrimshaw, INCAP studies of nutrition and infection, Food Nutr Bull
Skalny, Timashev, Aschner, Aaseth, Chernova et al., Serum Zinc, Copper, and Other Biometals Are Associated with COVID-19 Severity Markers, Metabolites
Squitti, Faller, Hureau, Granzotto, White et al., Copper Imbalance in Alzheimer's Disease and Its Link with the Amyloid Hypothesis: Towards a Combined Clinical, Chemical, and Genetic Etiology, J Alzheimers Dis
Thomas, Patel, Bittel, Wolski, Wang et al., Effect of High-Dose Zinc and Ascorbic Acid Supplementation vs Usual Care on Symptom Length and Reduction Among J o u r n a l P r e -p r o o f Ambulatory Patients With SARS-CoV-2 Infection: The COVID A to Z Randomized Clinical Trial, JAMA Netw Open
Velthuis, Van Den Worm, Sims, Baric, Snijder et al., Zn(2+) inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture, PLoS Pathog
Wang, C-reactive protein levels in the early stage of COVID-19, Med Mal Infect
Wang, Li, Lu, Huang, Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis, Aging
Wiersinga, Rhodes, Cheng, Peacock, Prescott, Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review, JAMA
Willoughby, Bowen, Zinc deficiency and toxicity in pediatric practice, Curr Opin Pediatr
Wu, Mcgoogan, Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases From the Chinese Center for Disease Control and Prevention, JAMA
Yan, Li, Wang, Yan, Zhu et al., Neutrophil to lymphocyte ratio as prognostic and predictive factor in patients with coronavirus disease 2019: A retrospective cross-sectional study, J Med Virol
Yao, Paguio, Dee, Tan, Moulick et al., The Minimal Effect of Zinc on the Survival of Hospitalized Patients With COVID-19: An Observational Study, Chest
DOI record:
{
"DOI": "10.1016/j.jtemb.2022.126944",
"ISSN": [
"0946-672X"
],
"URL": "http://dx.doi.org/10.1016/j.jtemb.2022.126944",
"alternative-id": [
"S0946672X22000244"
],
"article-number": "126944",
"author": [
{
"affiliation": [],
"family": "Ivanova",
"given": "Irena D.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Pal",
"given": "Amit",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Simonelli",
"given": "Ilaria",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Atanasova",
"given": "Bisera",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ventriglia",
"given": "Mariacarla",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rongioletti",
"given": "Mauro",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Squitti",
"given": "Rosanna",
"sequence": "additional"
}
],
"container-title": [
"Journal of Trace Elements in Medicine and Biology"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
2,
8
]
],
"date-time": "2022-02-08T04:48:18Z",
"timestamp": 1644295698000
},
"deposited": {
"date-parts": [
[
2022,
2,
8
]
],
"date-time": "2022-02-08T04:48:38Z",
"timestamp": 1644295718000
},
"indexed": {
"date-parts": [
[
2022,
2,
8
]
],
"date-time": "2022-02-08T05:11:25Z",
"timestamp": 1644297085752
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "print",
"value": "0946-672X"
}
],
"issued": {
"date-parts": [
[
2022,
2
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
2,
1
]
],
"date-time": "2022-02-01T00:00:00Z",
"timestamp": 1643673600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0946672X22000244?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0946672X22000244?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "126944",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2022,
2
]
]
},
"published-print": {
"date-parts": [
[
2022,
2
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1001/jama.2020.12839",
"article-title": "Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review",
"author": "Wiersinga",
"doi-asserted-by": "crossref",
"first-page": "782",
"issue": "8",
"journal-title": "JAMA",
"key": "10.1016/j.jtemb.2022.126944_bib1",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1002/art.41285",
"article-title": "On the Alert for Cytokine Storm: Immunopathology in COVID-19",
"author": "Henderson",
"doi-asserted-by": "crossref",
"first-page": "1059",
"issue": "7",
"journal-title": "Arthritis Rheumatol",
"key": "10.1016/j.jtemb.2022.126944_bib2",
"volume": "72",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.2648",
"article-title": "Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases From the Chinese Center for Disease Control and Prevention",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "1239",
"issue": "13",
"journal-title": "JAMA",
"key": "10.1016/j.jtemb.2022.126944_bib3",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.18632/aging.103000",
"article-title": "Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "6049",
"issue": "7",
"journal-title": "Aging",
"key": "10.1016/j.jtemb.2022.126944_bib4",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1186/s13104-016-2335-5",
"article-title": "What is the normal value of the neutrophil-to-lymphocyte ratio?",
"author": "Forget",
"doi-asserted-by": "crossref",
"first-page": "12",
"issue": "1",
"journal-title": "BMC Res Notes",
"key": "10.1016/j.jtemb.2022.126944_bib5",
"volume": "10",
"year": "2017"
},
{
"DOI": "10.1002/jmv.26061",
"article-title": "Neutrophil to lymphocyte ratio as prognostic and predictive factor in patients with coronavirus disease 2019: A retrospective cross-sectional study",
"author": "Yan",
"doi-asserted-by": "crossref",
"first-page": "2573",
"issue": "11",
"journal-title": "J Med Virol",
"key": "10.1016/j.jtemb.2022.126944_bib6",
"volume": "92",
"year": "2020"
},
{
"article-title": "[Nutrition and infection]",
"author": "Rakotoarimanana",
"first-page": "1975",
"issue": "220",
"journal-title": "Rev Med Suisse",
"key": "10.1016/j.jtemb.2022.126944_bib7",
"volume": "5",
"year": "2009"
},
{
"DOI": "10.1177/156482651003100107",
"article-title": "INCAP studies of nutrition and infection",
"author": "Scrimshaw",
"doi-asserted-by": "crossref",
"first-page": "54",
"issue": "1",
"journal-title": "Food Nutr Bull",
"key": "10.1016/j.jtemb.2022.126944_bib8",
"volume": "31",
"year": "2010"
},
{
"DOI": "10.1016/j.mad.2015.01.004",
"article-title": "Serum copper to zinc ratio: Relationship with aging and health status",
"author": "Malavolta",
"doi-asserted-by": "crossref",
"first-page": "93",
"journal-title": "Mech Ageing Dev",
"key": "10.1016/j.jtemb.2022.126944_bib9",
"volume": "151",
"year": "2015"
},
{
"DOI": "10.1007/s11357-011-9252-2",
"article-title": "Cu to Zn ratio, physical function, disability, and mortality risk in older elderly (ilSIRENTE study)",
"author": "Mocchegiani",
"doi-asserted-by": "crossref",
"first-page": "539",
"issue": "3",
"journal-title": "Age",
"key": "10.1016/j.jtemb.2022.126944_bib10",
"volume": "34",
"year": "2012"
},
{
"DOI": "10.3390/nu13061898",
"article-title": "Relation of Serum Copper Status to Survival in COVID-19",
"author": "Hackler",
"doi-asserted-by": "crossref",
"issue": "6",
"journal-title": "Nutrients",
"key": "10.1016/j.jtemb.2022.126944_bib11",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.3390/metabo11040244",
"article-title": "Serum Zinc, Copper, and Other Biometals Are Associated with COVID-19 Severity Markers",
"author": "Skalny",
"doi-asserted-by": "crossref",
"issue": "4",
"journal-title": "Metabolites",
"key": "10.1016/j.jtemb.2022.126944_bib12",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1007/s12011-020-02496-y",
"article-title": "The Relation Between Trace Element Status (Zinc, Copper, Magnesium) and Clinical Outcomes in COVID-19 Infection During Pregnancy",
"author": "Anuk",
"doi-asserted-by": "crossref",
"first-page": "3608",
"issue": "10",
"journal-title": "Biological trace element research",
"key": "10.1016/j.jtemb.2022.126944_bib13",
"volume": "199",
"year": "2021"
},
{
"DOI": "10.1007/s12011-020-02512-1",
"article-title": "Do Zinc Supplements Enhance the Clinical Efficacy of Hydroxychloroquine?: a Randomized, Multicenter Trial",
"author": "Abd-Elsalam",
"doi-asserted-by": "crossref",
"first-page": "3642",
"issue": "10",
"journal-title": "Biological trace element research",
"key": "10.1016/j.jtemb.2022.126944_bib14",
"volume": "199",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.0369",
"article-title": "Effect of High-Dose Zinc and Ascorbic Acid Supplementation vs Usual Care on Symptom Length and Reduction Among Ambulatory Patients With SARS-CoV-2 Infection: The COVID A to Z Randomized Clinical Trial",
"author": "Thomas",
"doi-asserted-by": "crossref",
"issue": "2",
"journal-title": "JAMA Netw Open",
"key": "10.1016/j.jtemb.2022.126944_bib15",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1007/s12011-020-02437-9",
"article-title": "Zinc and COVID-19: Basis of Current Clinical Trials",
"author": "Pal",
"doi-asserted-by": "crossref",
"first-page": "2882",
"issue": "8",
"journal-title": "Biological trace element research",
"key": "10.1016/j.jtemb.2022.126944_bib16",
"volume": "199",
"year": "2021"
},
{
"DOI": "10.1590/S0102-86502016001300006",
"article-title": "Copper-Zinc ratio and nutritional status in colorectal cancer patients during the perioperative period",
"author": "Ribeiro",
"doi-asserted-by": "crossref",
"first-page": "24",
"issue": "Suppl 1",
"journal-title": "Acta Cir Bras",
"key": "10.1016/j.jtemb.2022.126944_bib17",
"volume": "31",
"year": "2016"
},
{
"DOI": "10.1016/j.clinbiochem.2010.12.017",
"article-title": "Cu/Zn ratios are associated with nutritional status, oxidative stress, inflammation, and immune abnormalities in patients on peritoneal dialysis",
"author": "Guo",
"doi-asserted-by": "crossref",
"first-page": "275",
"issue": "4",
"journal-title": "Clinical biochemistry",
"key": "10.1016/j.jtemb.2022.126944_bib18",
"volume": "44",
"year": "2011"
},
{
"DOI": "10.1093/advances/nmz013",
"article-title": "The Role of Zinc in Antiviral Immunity",
"author": "Read",
"doi-asserted-by": "crossref",
"first-page": "696",
"issue": "4",
"journal-title": "Adv Nutr",
"key": "10.1016/j.jtemb.2022.126944_bib19",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.3390/cells8060603",
"article-title": "The Role of Micronutrients in the Infection and Subsequent Response to Hepatitis C Virus",
"author": "Gupta",
"doi-asserted-by": "crossref",
"issue": "6",
"journal-title": "Cells",
"key": "10.1016/j.jtemb.2022.126944_bib20",
"volume": "8",
"year": "2019"
},
{
"DOI": "10.1371/journal.ppat.1001176",
"article-title": "Zn(2+) inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture",
"author": "te Velthuis",
"doi-asserted-by": "crossref",
"issue": "11",
"journal-title": "PLoS Pathog",
"key": "10.1016/j.jtemb.2022.126944_bib21",
"volume": "6",
"year": "2010"
},
{
"DOI": "10.1016/j.nutres.2021.05.008",
"article-title": "Potential molecular mechanisms of zinc- and copper-mediated antiviral activity on COVID-19",
"author": "Rani",
"doi-asserted-by": "crossref",
"first-page": "109",
"journal-title": "Nutr Res",
"key": "10.1016/j.jtemb.2022.126944_bib22",
"volume": "92",
"year": "2021"
},
{
"DOI": "10.1016/j.redox.2020.101764",
"article-title": "Prediction of survival odds in COVID-19 by zinc, age and selenoprotein P as composite biomarker",
"author": "Heller",
"doi-asserted-by": "crossref",
"journal-title": "Redox Biol",
"key": "10.1016/j.jtemb.2022.126944_bib23",
"volume": "38",
"year": "2021"
},
{
"DOI": "10.1099/jmm.0.001250",
"article-title": "Zinc sulfate in combination with a zinc ionophore may improve outcomes in hospitalized COVID-19 patients",
"author": "Carlucci",
"doi-asserted-by": "crossref",
"first-page": "1228",
"issue": "10",
"journal-title": "J Med Microbiol",
"key": "10.1016/j.jtemb.2022.126944_bib24",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1016/j.chest.2020.06.082",
"article-title": "The Minimal Effect of Zinc on the Survival of Hospitalized Patients With COVID-19: An Observational Study",
"author": "Yao",
"doi-asserted-by": "crossref",
"first-page": "108",
"issue": "1",
"journal-title": "Chest",
"key": "10.1016/j.jtemb.2022.126944_bib25",
"volume": "159",
"year": "2021"
},
{
"DOI": "10.1017/S000711452000330X",
"article-title": "Nutritional status of micronutrients as a possible and modifiable risk factor for COVID-19: a UK perspective",
"author": "Richardson",
"doi-asserted-by": "crossref",
"first-page": "678",
"issue": "6",
"journal-title": "Br J Nutr",
"key": "10.1016/j.jtemb.2022.126944_bib26",
"volume": "125",
"year": "2021"
},
{
"DOI": "10.1016/j.ijid.2020.08.018",
"article-title": "Nutritional status of patients with COVID-19",
"author": "Im",
"doi-asserted-by": "crossref",
"first-page": "390",
"journal-title": "Int J Infect Dis",
"key": "10.1016/j.jtemb.2022.126944_bib27",
"volume": "100",
"year": "2020"
},
{
"key": "10.1016/j.jtemb.2022.126944_bib28",
"unstructured": "M.U.-S. Department of Clinical Laboratory and Clinical Immunology, University Hospital \"Alexandrovska\", 2001., Reference intervals for clinical laboratory parameters, 2021."
},
{
"DOI": "10.1016/j.ijid.2020.09.014",
"article-title": "COVID-19: Poor outcomes in patients with zinc deficiency",
"author": "Jothimani",
"doi-asserted-by": "crossref",
"first-page": "343",
"journal-title": "Int J Infect Dis",
"key": "10.1016/j.jtemb.2022.126944_bib29",
"volume": "100",
"year": "2020"
},
{
"DOI": "10.1016/j.medmal.2020.03.007",
"article-title": "C-reactive protein levels in the early stage of COVID-19",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "332",
"issue": "4",
"journal-title": "Med Mal Infect",
"key": "10.1016/j.jtemb.2022.126944_bib30",
"volume": "50",
"year": "2020"
},
{
"DOI": "10.1016/j.bbi.2018.02.013",
"article-title": "Rethinking IL-6 and CRP: Why they are more than inflammatory biomarkers, and why it matters",
"author": "Del Giudice",
"doi-asserted-by": "crossref",
"first-page": "61",
"journal-title": "Brain Behav Immun",
"key": "10.1016/j.jtemb.2022.126944_bib31",
"volume": "70",
"year": "2018"
},
{
"DOI": "10.1002/jat.3303",
"article-title": "Copper toxicology, oxidative stress and inflammation using zebrafish as experimental model",
"author": "Pereira",
"doi-asserted-by": "crossref",
"first-page": "876",
"issue": "7",
"journal-title": "J Appl Toxicol",
"key": "10.1016/j.jtemb.2022.126944_bib32",
"volume": "36",
"year": "2016"
},
{
"DOI": "10.1007/s10654-020-00644-1",
"article-title": "Serum copper-to-zinc-ratio and risk of incident infection in men: the Kuopio Ischaemic Heart Disease Risk Factor Study",
"author": "Laine",
"doi-asserted-by": "crossref",
"first-page": "1149",
"issue": "12",
"journal-title": "European journal of epidemiology",
"key": "10.1016/j.jtemb.2022.126944_bib33",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.3233/JAD-201556",
"article-title": "Copper Imbalance in Alzheimer's Disease and Its Link with the Amyloid Hypothesis: Towards a Combined Clinical, Chemical, and Genetic Etiology",
"author": "Squitti",
"doi-asserted-by": "crossref",
"first-page": "23",
"issue": "1",
"journal-title": "J Alzheimers Dis",
"key": "10.1016/j.jtemb.2022.126944_bib34",
"volume": "83",
"year": "2021"
},
{
"DOI": "10.1097/MOP.0000000000000132",
"article-title": "Zinc deficiency and toxicity in pediatric practice",
"author": "Willoughby",
"doi-asserted-by": "crossref",
"first-page": "579",
"issue": "5",
"journal-title": "Curr Opin Pediatr",
"key": "10.1016/j.jtemb.2022.126944_bib35",
"volume": "26",
"year": "2014"
}
],
"reference-count": 35,
"references-count": 35,
"relation": {},
"score": 1,
"short-container-title": [
"Journal of Trace Elements in Medicine and Biology"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Inorganic Chemistry",
"Molecular Medicine",
"Biochemistry"
],
"subtitle": [],
"title": [
"Evaluation of zinc, copper, and Cu:Zn ratio in serum, and their implications in the course of COVID-19"
],
"type": "journal-article"
}
