The correlation between serum selenium, zinc, and COVID-19 severity: an observational study
et al., BMC Infectious Diseases, doi:10.1186/s12879-021-06617-3, Sep 2021
Zinc for COVID-19
2nd treatment shown to reduce risk in
July 2020, now with p = 0.00000028 from 47 studies, recognized in 23 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Prospective analysis of 84 patients in Iran, showing higher selenium and zinc levels associated with a decrease in serum CRP level. There was no statistically significant association between selenium/zinc levels and disease severity.
Study covers selenium and zinc.
Razeghi Jahromi et al., 3 Sep 2021, prospective, Iran, peer-reviewed, 14 authors.
Contact: toghae@sina.tums.ac.ir (corresponding author).
The correlation between serum selenium, zinc, and COVID-19 severity: an observational study
BMC Infectious Diseases, doi:10.1186/s12879-021-06617-3
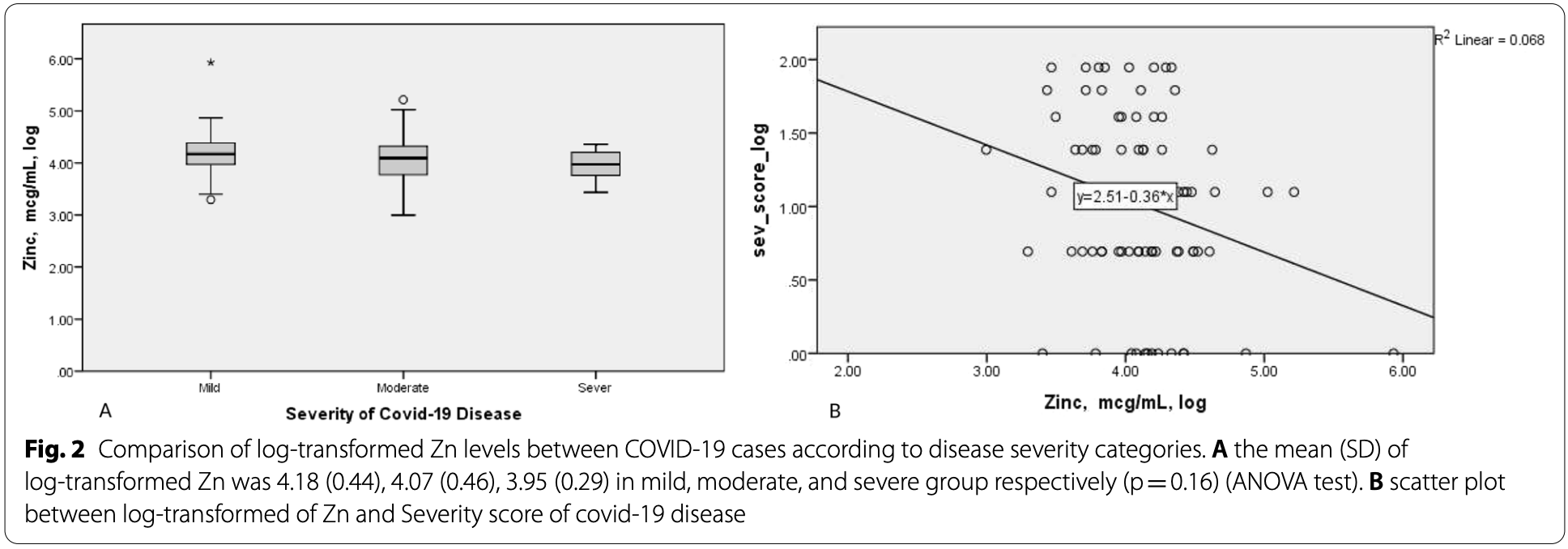
Background: Without an adequate immune response, SARS-CoV2 virus can simply spread throughout the body of the host. Two of the well-known immunonutrients are selenium (Se) and zinc (Zn). Se and Zn deficiency might lead to inflammation, oxidative stress, and viral entry into the cells by decreasing ACE-2 expression; three factors that are proposed to be involved in COVID-19 pathogenesis. Thus, in the current study we aimed at evaluating the correlation between serum Se and Zn status and COVID-19 severity. Methods: Eighty-four COVID-19 patients were enrolled in this observational study. Patients were diagnosed based on an infectious disease specialist diagnosis, using WHO interim guidance and the recommendations of the Iranian National Committee of Covid-19. The patients with acute respiratory tract infection symptoms were checked for compatibility of chest computed tomography (CT) scan results with that of Covid-19 and Real-time polymerase chain reaction (RT-PCR) for corona virus infection. The severity of Covid-19 was categorized into three groups (mild, moderate, and severe) using CDC criteria. Serum Zn and Se level of all subjects was measured. The severity of the disease was determined only once at the onset of disease. Results: According to the results of linear regression test, there was a significant association between Zn and Se level and COVID-19 severity (β = − 0.28, P-value = 0.01 for Se; β = − 0.26, P-value = 0.02). However the significance disappeared after adjusting for confounding factors. Spearman correlation analysis showed a significant negative association between serum Zn, Se and CRP level (r = − 0.35, P-value = 0.001 for Se; r = − 0.41, P-value < 0.001 for Zn).
Conclusion: Results suggest that increasing levels of Se and Zn were accompanied by a decrease in serum CRP level. However, the significant association between Se, Zn, and disease severity was lost after adjusting for confounding factors.
Supplementary Information The online version contains supplementary material available at https:// doi. org/ 10. 1186/ s12879-021-06617-3. Additional file 1: Table . Biochemical assessments of the COVID-19 patients according to the severity of COVID-19.
Authors' contributions SR designed this study, wrote and edited the manuscript, HM conducted laboratory managements, MT designed the study, investigated data, and edited the manuscript. SA conducted data investigation, extraction, and edited the manuscript, ZG was responsible for analysis, and interpretation of results. SN, SH, and HA participated in data gathering. AJ and MM, MT, and ME participated in laboratory measurements. AH participated in study design. EJ edited the manuscript. All authors read and approved the final manuscript.
Declarations Ethics approval and consent to participate All methods were carried out in accordance with relevant guidelines and regulations. The study was approved by the ethics committee of Tehran University of Medical Sciences (IR.TUMS.VCR.REC.1399.134). All participants provided informed written consent to participate in this study, which is attached to the medical documents of each hospitalized patient.
Consent for publication All participants provided informed written consent regarding publication of the results, which is attached to the medical documents of each hospitalized patient.
Competing interests The authors declare no potential competing interests with respect to the..
References
Arentz, Hunter, Yang, Goldenberg, Beardsley et al., Zinc for the prevention and treatment of SARS-CoV-2 and other acute viral respiratory infections: a rapid review, Adv Integr Med, doi:10.1016/j.aimed.2020.07.009
Boudreault, Pinilla-Vera, Englert, Kho, Isabelle et al., Zinc deficiency primes the lung for ventilator-induced injury, JCI Insight, doi:10.1172/jci.insight.86507
Brieger, Rink, Haase, Differential regulation of TLR-dependent MyD88 and TRIF signaling pathways by free zinc ions, J Immunol
Broman, Bernardson, Bursell, Wernerman, Fläring et al., Serum selenium in critically ill patients: profile and supplementation in a depleted region, Acta Anaesthesiol Scand
De Oliveira Iglesias, Leite, Paes, De Oliveira, Sarni, Low plasma selenium concentrations in critically ill children: the interaction effect between inflammation and selenium deficiency, Crit Care
Gallo Marin, Aghagoli, Lavine, Yang, Siff et al., Predictors of COVID-19 severity: A literature review, Rev med virol
Gavriilaki, Brodsky, Severe COVID-19 infection and thrombotic microangiopathy: success doesn't come easily, Br J Haematol, doi:10.1111/bjh.16783
Girodon, Lombard, Galan, Brunet-Lecomte, Monget et al., Effect of micronutrient supplementation on infection in institutionalized elderly subjects: a controlled trial, Ann Nutr Metab
Hiffler, Rakotoambinina, Selenium and RNA virus interactions: potential implications for SARS-CoV-2 infection (COVID-19), Front Nutr
Hirano, Murakami, COVID-19: a new virus, but a familiar receptor and cytokine release syndrome, Immunity, doi:10.1016/j.immuni.2020.04.003
Hoeger, Simon, Beeker, Marx, Haase et al., Persistent low serum zinc is associated with recurrent sepsis in critically ill patients-a pilot study, PLoS ONE
Im, Je, Baek, Chung, Kwon et al., Nutritional status of patients with COVID-19, Int J Infect Dis
Jothimani, Kailasam, Danielraj, Nallathambi, Ramachandran et al., COVID-19: Poor outcomes in patients with zinc deficiency, Int J Infectious Dis
Liu, Li, Liu, Liang, Wang et al., Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS-CoV-2 infected patients, EBioMedicine
Lopes-Pires, Ahmed, Vara, Gibbins, Pula et al., Zinc regulates reactive oxygen species generation in platelets, Platelets, doi:10.1080/09537104.2020.1742311
Maxfield, Crane, Zinc deficiency
Moghaddam, Heller, Sun, Seelig, Cherkezov et al., Selenium deficiency is associated with mortality risk from COVID-19, Nutrients
Pal, Squitti, Picozza, Pawar, Rongioletti et al., Zinc and COVID-19: basis of current clinical trials, Biol Trace Elem Res, doi:10.1007/s12011-020-02437-9
Roscioli, Jersmann, Lester, Badiei, Fon et al., Zinc deficiency as a codeterminant for airway epithelial barrier dysfunction in an ex vivo model of COPD, Int J Chron Obstruct Pulmon Dis
Smith, Butrimovitz, Purdy, Direct measurement of zinc in plasma by atomic absorption spectroscopy, Clin Chem
Talebpour, Hadadi, Oraii, Ashraf, Rationale and design of a registry in a referral and educational medical center in Tehran, Iran: Sina Hospital Covid-19 Registry (SHCo-19R), Adv J Emerg Med
Tan, Ho, Kalimuddin, Cherng, Teh et al., A cohort study to evaluate the effect of combination vitamin D, magnesium and vitamin B12 (DMB) on progression to severe outcome in older COVID-19 patients
Taylor, Pugh, The contribution of zinc to platelet behaviour during haemostasis and thrombosis, Metallomics
Taylor, Radding, Understanding selenium and glutathione as antiviral factors in COVID-19: does the viral Mpro protease target host selenoproteins and glutathione synthesis?, Front Nutr
Varga, Flammer, Steiger, Haberecker, Andermatt et al., Endothelial cell infection and endotheliitis in COVID-19, The Lancet
Wessels, Pupke, Trotha, Gombert, Himmelsbach et al., Zinc supplementation ameliorates lung injury by reducing neutrophil recruitment and activity, Thorax
Wessels, Rolles, Rink, The potential impact of zinc supplementation on COVID-19 pathogenesis, Front Immunol, doi:10.3389/fimmu.2020.01712
Xu, Gong, Sun, Cai, Liu et al., Impact of selenium deficiency on inflammation, oxidative stress, and phagocytosis in mouse macrophages, Biol Trace Elem Res
Zhang, Taylor, Bennett, Saad, Rayman, Association between regional selenium status and reported outcome of COVID-19 cases in China, Am J Clin Nutr
DOI record:
{
"DOI": "10.1186/s12879-021-06617-3",
"ISSN": [
"1471-2334"
],
"URL": "http://dx.doi.org/10.1186/s12879-021-06617-3",
"abstract": "<jats:title>Abstract</jats:title><jats:sec>\n <jats:title>Background</jats:title>\n <jats:p>Without an adequate immune response, SARS-CoV2 virus can simply spread throughout the body of the host. Two of the well-known immunonutrients are selenium (Se) and zinc (Zn). Se and Zn deficiency might lead to inflammation, oxidative stress, and viral entry into the cells by decreasing ACE-2 expression; three factors that are proposed to be involved in COVID-19 pathogenesis. Thus, in the current study we aimed at evaluating the correlation between serum Se and Zn status and COVID-19 severity.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>Eighty-four COVID-19 patients were enrolled in this observational study. Patients were diagnosed based on an infectious disease specialist diagnosis, using WHO interim guidance and the recommendations of the Iranian National Committee of Covid-19. The patients with acute respiratory tract infection symptoms were checked for compatibility of chest computed tomography (CT) scan results with that of Covid-19 and Real-time polymerase chain reaction (RT-PCR) for corona virus infection. The severity of Covid-19 was categorized into three groups (mild, moderate, and severe) using CDC criteria. Serum Zn and Se level of all subjects was measured. The severity of the disease was determined only once at the onset of disease.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>According to the results of linear regression test, there was a significant association between Zn and Se level and COVID-19 severity (β = − 0.28, P-value = 0.01 for Se; β = − 0.26, P-value = 0.02). However the significance disappeared after adjusting for confounding factors. Spearman correlation analysis showed a significant negative association between serum Zn, Se and CRP level (r = − 0.35, P-value = 0.001 for Se; r = − 0.41, P-value < 0.001 for Zn).</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Conclusion</jats:title>\n <jats:p>Results suggest that increasing levels of Se and Zn were accompanied by a decrease in serum CRP level. However, the significant association between Se, Zn, and disease severity was lost after adjusting for confounding factors.</jats:p>\n </jats:sec>",
"alternative-id": [
"6617"
],
"article-number": "899",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "13 March 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "22 August 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "3 September 2021"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Ethics approval and consent to participate",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "All methods were carried out in accordance with relevant guidelines and regulations. The study was approved by the ethics committee of Tehran University of Medical Sciences (IR.TUMS.VCR.REC.1399.134). All participants provided informed written consent to participate in this study, which is attached to the medical documents of each hospitalized patient."
},
{
"group": {
"label": "Consent for publication",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "All participants provided informed written consent regarding publication of the results, which is attached to the medical documents of each hospitalized patient."
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 4,
"value": "The authors declare no potential competing interests with respect to the research, authorship, and/or publication of this article."
}
],
"author": [
{
"affiliation": [],
"family": "Razeghi Jahromi",
"given": "Soodeh",
"sequence": "first"
},
{
"affiliation": [],
"family": "Moradi Tabriz",
"given": "Hedieh",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9368-6835",
"affiliation": [],
"authenticated-orcid": false,
"family": "Togha",
"given": "Mansoureh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ariyanfar",
"given": "Shadi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ghorbani",
"given": "Zeinab",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Naeeni",
"given": "Sima",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Haghighi",
"given": "Samaneh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jazayeri",
"given": "Aboozar",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Montazeri",
"given": "Mahnaz",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Talebpour",
"given": "Mohammad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ashraf",
"given": "Haleh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ebrahimi",
"given": "Mehdi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hekmatdoost",
"given": "Azita",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jafari",
"given": "Elham",
"sequence": "additional"
}
],
"container-title": "BMC Infectious Diseases",
"container-title-short": "BMC Infect Dis",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2021,
9,
3
]
],
"date-time": "2021-09-03T12:28:04Z",
"timestamp": 1630672084000
},
"deposited": {
"date-parts": [
[
2021,
9,
3
]
],
"date-time": "2021-09-03T12:30:03Z",
"timestamp": 1630672203000
},
"funder": [
{
"DOI": "10.13039/501100004484",
"award": [
"No: 99-1-118-47390",
"No: 99-1-118-47390",
"No: 99-1-118-47390",
"No: 99-1-118-47390",
"No: 99-1-118-47390",
"No: 99-1-118-47390",
"No: 99-1-118-47390",
"No: 99-1-118-47390",
"No: 99-1-118-47390",
"No: 99-1-118-47390",
"No: 99-1-118-47390",
"No: 99-1-118-47390",
"No: 99-1-118-47390",
"No: 99-1-118-47390"
],
"doi-asserted-by": "publisher",
"name": "Tehran University of Medical Sciences and Health Services"
}
],
"indexed": {
"date-parts": [
[
2022,
12,
5
]
],
"date-time": "2022-12-05T08:19:05Z",
"timestamp": 1670228345671
},
"is-referenced-by-count": 17,
"issue": "1",
"issued": {
"date-parts": [
[
2021,
9,
3
]
]
},
"journal-issue": {
"issue": "1",
"published-print": {
"date-parts": [
[
2021,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
9,
3
]
],
"date-time": "2021-09-03T00:00:00Z",
"timestamp": 1630627200000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
9,
3
]
],
"date-time": "2021-09-03T00:00:00Z",
"timestamp": 1630627200000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1186/s12879-021-06617-3.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1186/s12879-021-06617-3/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1186/s12879-021-06617-3.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1186",
"published": {
"date-parts": [
[
2021,
9,
3
]
]
},
"published-online": {
"date-parts": [
[
2021,
9,
3
]
]
},
"published-print": {
"date-parts": [
[
2021,
12
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.3389/fnut.2020.00164",
"author": "L Hiffler",
"doi-asserted-by": "publisher",
"first-page": "164",
"journal-title": "Front Nutr",
"key": "6617_CR1",
"unstructured": "Hiffler L, Rakotoambinina B. Selenium and RNA virus interactions: potential implications for SARS-CoV-2 infection (COVID-19). Front Nutr. 2020;7:164.",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.08.018",
"author": "JH Im",
"doi-asserted-by": "publisher",
"first-page": "390",
"journal-title": "Int J Infect Dis",
"key": "6617_CR2",
"unstructured": "Im JH, Je YS, Baek J, Chung M-H, Kwon HY, Lee J-S. Nutritional status of patients with COVID-19. Int J Infect Dis. 2020;100:390–3.",
"volume": "100",
"year": "2020"
},
{
"DOI": "10.3389/fnut.2020.00143",
"author": "EW Taylor",
"doi-asserted-by": "publisher",
"first-page": "143",
"journal-title": "Front Nutr",
"key": "6617_CR3",
"unstructured": "Taylor EW, Radding W. Understanding selenium and glutathione as antiviral factors in COVID-19: does the viral Mpro protease target host selenoproteins and glutathione synthesis? Front Nutr. 2020;7:143.",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1016/j.immuni.2020.04.003",
"author": "T Hirano",
"doi-asserted-by": "publisher",
"journal-title": "Immunity",
"key": "6617_CR4",
"unstructured": "Hirano T, Murakami M. COVID-19: a new virus, but a familiar receptor and cytokine release syndrome. Immunity. 2020. https://doi.org/10.1016/j.immuni.2020.04.003.",
"year": "2020"
},
{
"author": "World Health Organization",
"key": "6617_CR5",
"unstructured": "World Health Organization. The world health report 2002: reducing risks, promoting healthy life. Geneva: World Health Organization; 2002.",
"volume-title": "The world health report 2002: reducing risks, promoting healthy life",
"year": "2002"
},
{
"DOI": "10.1093/ajcn/nqaa095",
"author": "J Zhang",
"doi-asserted-by": "publisher",
"first-page": "1297",
"issue": "6",
"journal-title": "Am J Clin Nutr",
"key": "6617_CR6",
"unstructured": "Zhang J, Taylor EW, Bennett K, Saad R, Rayman MP. Association between regional selenium status and reported outcome of COVID-19 cases in China. Am J Clin Nutr. 2020;111(6):1297–9.",
"volume": "111",
"year": "2020"
},
{
"DOI": "10.3390/nu12072098",
"author": "A Moghaddam",
"doi-asserted-by": "publisher",
"first-page": "2098",
"issue": "7",
"journal-title": "Nutrients",
"key": "6617_CR7",
"unstructured": "Moghaddam A, Heller RA, Sun Q, Seelig J, Cherkezov A, Seibert L, et al. Selenium deficiency is associated with mortality risk from COVID-19. Nutrients. 2020;12(7):2098.",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2020.01712",
"author": "I Wessels",
"doi-asserted-by": "publisher",
"journal-title": "Front Immunol",
"key": "6617_CR8",
"unstructured": "Wessels I, Rolles B, Rink L. The potential impact of zinc supplementation on COVID-19 pathogenesis. Front Immunol. 2020. https://doi.org/10.3389/fimmu.2020.01712.",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0176069",
"author": "J Hoeger",
"doi-asserted-by": "publisher",
"first-page": "e0176069",
"issue": "5",
"journal-title": "PLoS ONE",
"key": "6617_CR9",
"unstructured": "Hoeger J, Simon T-P, Beeker T, Marx G, Haase H, Schuerholz T. Persistent low serum zinc is associated with recurrent sepsis in critically ill patients—a pilot study. PLoS ONE. 2017;12(5):e0176069.",
"volume": "12",
"year": "2017"
},
{
"DOI": "10.1136/thoraxjnl-2019-213357",
"author": "I Wessels",
"doi-asserted-by": "publisher",
"first-page": "253",
"issue": "3",
"journal-title": "Thorax",
"key": "6617_CR10",
"unstructured": "Wessels I, Pupke JT, von Trotha K-T, Gombert A, Himmelsbach A, Fischer HJ, et al. Zinc supplementation ameliorates lung injury by reducing neutrophil recruitment and activity. Thorax. 2020;75(3):253–61.",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.2147/COPD.S149589",
"author": "E Roscioli",
"doi-asserted-by": "publisher",
"first-page": "3503",
"journal-title": "Int J Chron Obstruct Pulmon Dis",
"key": "6617_CR11",
"unstructured": "Roscioli E, Jersmann HP, Lester S, Badiei A, Fon A, Zalewski P, et al. Zinc deficiency as a codeterminant for airway epithelial barrier dysfunction in an ex vivo model of COPD. Int J Chron Obstruct Pulmon Dis. 2017;12:3503.",
"volume": "12",
"year": "2017"
},
{
"DOI": "10.1172/jci.insight.86507",
"author": "F Boudreault",
"doi-asserted-by": "publisher",
"journal-title": "JCI Insight",
"key": "6617_CR12",
"unstructured": "Boudreault F, Pinilla-Vera M, Englert JA, Kho AT, Isabelle C, Arciniegas AJ, et al. Zinc deficiency primes the lung for ventilator-induced injury. JCI Insight. 2017. https://doi.org/10.1172/jci.insight.86507.",
"year": "2017"
},
{
"DOI": "10.1111/bjh.16783",
"author": "E Gavriilaki",
"doi-asserted-by": "publisher",
"journal-title": "Br J Haematol",
"key": "6617_CR13",
"unstructured": "Gavriilaki E, Brodsky RA. Severe COVID-19 infection and thrombotic microangiopathy: success doesn’t come easily. Br J Haematol. 2020. https://doi.org/10.1111/bjh.16783.",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30937-5",
"author": "Z Varga",
"doi-asserted-by": "publisher",
"first-page": "1417",
"issue": "10234",
"journal-title": "The Lancet",
"key": "6617_CR14",
"unstructured": "Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. The Lancet. 2020;395(10234):1417–8.",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1080/09537104.2020.1742311",
"author": "ME Lopes-Pires",
"doi-asserted-by": "publisher",
"journal-title": "Platelets",
"key": "6617_CR15",
"unstructured": "Lopes-Pires ME, Ahmed NS, Vara D, Gibbins JM, Pula G, Pugh N. Zinc regulates reactive oxygen species generation in platelets. Platelets. 2020. https://doi.org/10.1080/09537104.2020.1742311.",
"year": "2020"
},
{
"DOI": "10.1039/C5MT00251F",
"author": "K Taylor",
"doi-asserted-by": "publisher",
"first-page": "144",
"issue": "2",
"journal-title": "Metallomics",
"key": "6617_CR16",
"unstructured": "Taylor K, Pugh N. The contribution of zinc to platelet behaviour during haemostasis and thrombosis. Metallomics. 2016;8(2):144–55.",
"volume": "8",
"year": "2016"
},
{
"DOI": "10.1016/j.ebiom.2020.102763",
"author": "J Liu",
"doi-asserted-by": "publisher",
"first-page": "102763",
"journal-title": "EBioMedicine",
"key": "6617_CR17",
"unstructured": "Liu J, Li S, Liu J, Liang B, Wang X, Wang H, et al. Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS-CoV-2 infected patients. EBioMedicine. 2020;55:102763.",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.4049/jimmunol.1301261",
"author": "A Brieger",
"doi-asserted-by": "publisher",
"first-page": "1808",
"issue": "4",
"journal-title": "J Immunol",
"key": "6617_CR18",
"unstructured": "Brieger A, Rink L, Haase H. Differential regulation of TLR-dependent MyD88 and TRIF signaling pathways by free zinc ions. J Immunol. 2013;191(4):1808–17.",
"volume": "191",
"year": "2013"
},
{
"DOI": "10.1016/j.ijid.2020.09.014",
"author": "D Jothimani",
"doi-asserted-by": "publisher",
"first-page": "343",
"journal-title": "Int J Infectious Dis",
"key": "6617_CR19",
"unstructured": "Jothimani D, Kailasam E, Danielraj S, Nallathambi B, Ramachandran H, Sekar P, et al. COVID-19: Poor outcomes in patients with zinc deficiency. Int J Infectious Dis. 2020;100:343–9.",
"volume": "100",
"year": "2020"
},
{
"author": "M Talebpour",
"first-page": "e53",
"issue": "2s",
"journal-title": "Adv J Emerg Med",
"key": "6617_CR20",
"unstructured": "Talebpour M, Hadadi A, Oraii A, Ashraf H. Rationale and design of a registry in a referral and educational medical center in Tehran, Iran: Sina Hospital Covid-19 Registry (SHCo-19R). Adv J Emerg Med. 2020;4(2s):e53.",
"volume": "4",
"year": "2020"
},
{
"key": "6617_CR21",
"unstructured": "https://www.cdc.gov/."
},
{
"DOI": "10.1101/2020.06.01.20112334",
"doi-asserted-by": "crossref",
"key": "6617_CR22",
"unstructured": "Tan CW, Ho LP, Kalimuddin S, Cherng BPZ, Teh YE, Thien SY, et al. A cohort study to evaluate the effect of combination vitamin D, magnesium and vitamin B12 (DMB) on progression to severe outcome in older COVID-19 patients. medRxiv. 2020."
},
{
"key": "6617_CR23",
"unstructured": "https://www.mayocliniclabs.com/test-catalog/Clinical+and+Interpretive/9765."
},
{
"DOI": "10.1186/cc13877",
"author": "SB de Oliveira Iglesias",
"doi-asserted-by": "publisher",
"first-page": "R101",
"issue": "3",
"journal-title": "Crit Care",
"key": "6617_CR24",
"unstructured": "de Oliveira Iglesias SB, Leite HP, Paes ÂT, de Oliveira SV, Sarni ROS. Low plasma selenium concentrations in critically ill children: the interaction effect between inflammation and selenium deficiency. Crit Care. 2014;18(3):R101.",
"volume": "18",
"year": "2014"
},
{
"DOI": "10.1007/s12011-019-01775-7",
"author": "J Xu",
"doi-asserted-by": "publisher",
"first-page": "237",
"issue": "1",
"journal-title": "Biol Trace Elem Res",
"key": "6617_CR25",
"unstructured": "Xu J, Gong Y, Sun Y, Cai J, Liu Q, Bao J, et al. Impact of selenium deficiency on inflammation, oxidative stress, and phagocytosis in mouse macrophages. Biol Trace Elem Res. 2020;194(1):237–43.",
"volume": "194",
"year": "2020"
},
{
"DOI": "10.1002/rmv.2146",
"author": "B Gallo Marin",
"doi-asserted-by": "publisher",
"first-page": "1",
"issue": "1",
"journal-title": "Rev med virol",
"key": "6617_CR26",
"unstructured": "Gallo Marin B, Aghagoli G, Lavine K, Yang L, Siff EJ, Chiang SS, Salazar‐Mather TP, Dumenco L, Savaria MC, Aung SN, Flanigan T. Predictors of COVID‐19 severity: A literature review. Rev med virol. 2021;31(1):1–0.",
"volume": "31",
"year": "2021"
},
{
"DOI": "10.1159/000177984",
"author": "F Girodon",
"doi-asserted-by": "publisher",
"first-page": "98",
"issue": "2",
"journal-title": "Ann Nutr Metab",
"key": "6617_CR27",
"unstructured": "Girodon F, Lombard M, Galan P, Brunet-Lecomte P, Monget A-L, Arnaud J, et al. Effect of micronutrient supplementation on infection in institutionalized elderly subjects: a controlled trial. Ann Nutr Metab. 1997;41(2):98–107.",
"volume": "41",
"year": "1997"
},
{
"DOI": "10.1111/aas.13573",
"author": "LM Broman",
"doi-asserted-by": "publisher",
"first-page": "803",
"issue": "6",
"journal-title": "Acta Anaesthesiol Scand",
"key": "6617_CR28",
"unstructured": "Broman LM, Bernardson A, Bursell K, Wernerman J, Fläring U, Tjäder I. Serum selenium in critically ill patients: profile and supplementation in a depleted region. Acta Anaesthesiol Scand. 2020;64(6):803–9.",
"volume": "64",
"year": "2020"
},
{
"DOI": "10.1007/s12011-020-02437-9",
"author": "A Pal",
"doi-asserted-by": "publisher",
"journal-title": "Biol Trace Elem Res",
"key": "6617_CR29",
"unstructured": "Pal A, Squitti R, Picozza M, Pawar A, Rongioletti M, Dutta AK, et al. Zinc and COVID-19: basis of current clinical trials. Biol Trace Elem Res. 2020. https://doi.org/10.1007/s12011-020-02437-9.",
"year": "2020"
},
{
"DOI": "10.1016/j.aimed.2020.07.009",
"author": "S Arentz",
"doi-asserted-by": "publisher",
"journal-title": "Adv Integr Med",
"key": "6617_CR30",
"unstructured": "Arentz S, Hunter J, Yang G, Goldenberg J, Beardsley J, Myers SP, et al. Zinc for the prevention and treatment of SARS-CoV-2 and other acute viral respiratory infections: a rapid review. Adv Integr Med. 2020. https://doi.org/10.1016/j.aimed.2020.07.009.",
"year": "2020"
},
{
"DOI": "10.1093/clinchem/25.8.1487",
"author": "J Smith Jr",
"doi-asserted-by": "publisher",
"first-page": "1487",
"issue": "8",
"journal-title": "Clin Chem",
"key": "6617_CR31",
"unstructured": "Smith J Jr, Butrimovitz G, Purdy W. Direct measurement of zinc in plasma by atomic absorption spectroscopy. Clin Chem. 1979;25(8):1487–91.",
"volume": "25",
"year": "1979"
},
{
"author": "L Maxfield",
"key": "6617_CR32",
"unstructured": "Maxfield L, Crane JS. Zinc deficiency. In: StatPearls [Internet]. Treasure Island: StatPearls Publishing; 2019.",
"volume-title": "StatPearls [Internet]",
"year": "2019"
}
],
"reference-count": 32,
"references-count": 32,
"relation": {},
"resource": {
"primary": {
"URL": "https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-021-06617-3"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Infectious Diseases"
],
"subtitle": [],
"title": "The correlation between serum selenium, zinc, and COVID-19 severity: an observational study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "21"
}
