Predictors for cause-specific and timing of deaths in patients with COVID-19: a cohort study in Taiwan
et al., BMC Infectious Diseases, doi:10.1186/s12879-024-09654-w, Aug 2024
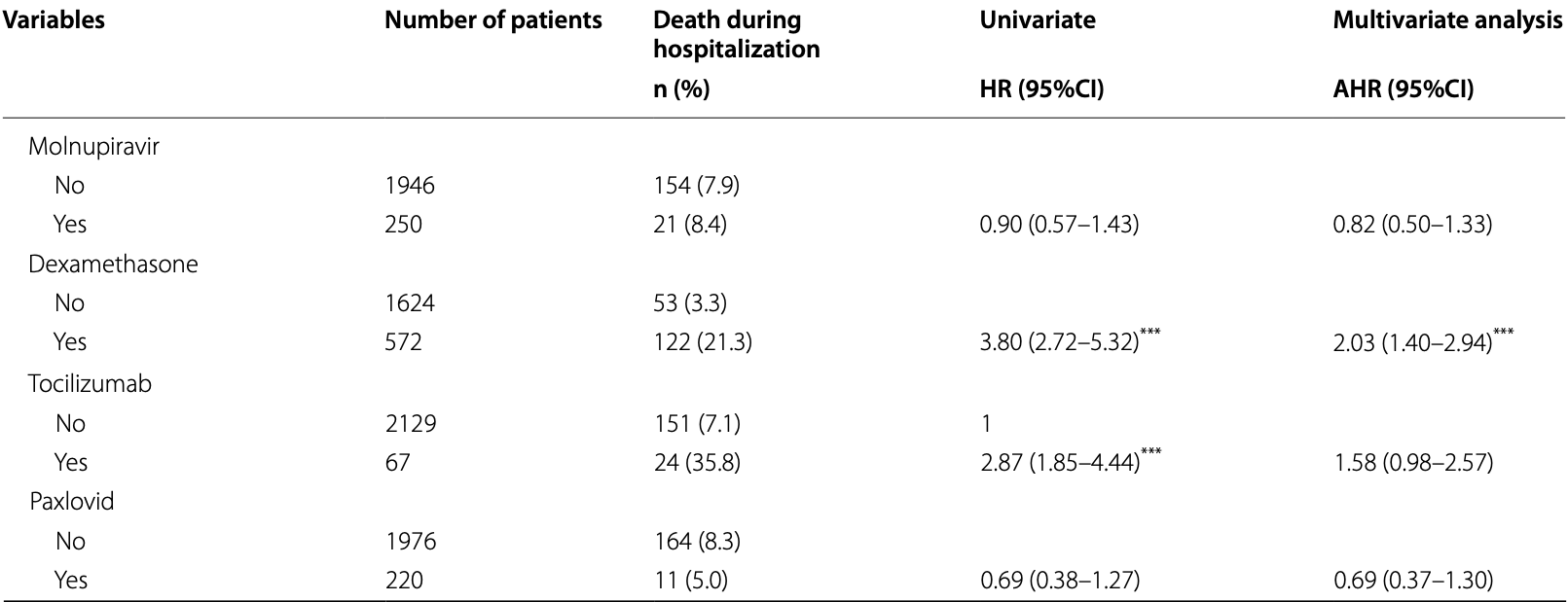
Retrospective 2,196 COVID-19 patients in Taiwan (49% mild cases, 44% moderate, 7% severe) showing lower mortality with molnupiravir, without statistical significance.
Authors report that all infected patients were hospitalized at the time of the study in Taiwan.
Potential risks of molnupiravir include the creation of dangerous variants, and mutagenicity, carcinogenicity, teratogenicity, and embryotoxicity1-15. Multiple analyses have identified variants potentially created by molnupiravir16-20. Studies show significantly increased risk of acute kidney injury21, cardiovascular toxocity22, and neurological symptoms21. Treatment may increase viral rebound23,24.
|
risk of death, 18.0% lower, HR 0.82, p = 0.43, treatment 250, control 1,946, adjusted per study, multivariable, Cox proportional hazards.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Swanstrom et al., Lethal mutagenesis as an antiviral strategy, Science, doi:10.1126/science.abn0048.
2.
Hadj Hassine et al., Lethal Mutagenesis of RNA Viruses and Approved Drugs with Antiviral Mutagenic Activity, Viruses, doi:10.3390/v14040841.
3.
Shum, C., An investigational study into the drug-associated mutational signature in SARS-CoV-2 viruses, The University of Hong Kong, PhD Thesis, hub.hku.hk/handle/10722/344396.
4.
Waters et al., Human genetic risk of treatment with antiviral nucleoside analog drugs that induce lethal mutagenesis: the special case of molnupiravir, Environmental and Molecular Mutagenesis, doi:10.1002/em.22471.
5.
Huntsman, M., An assessment of the reproductive toxicity of the anti-COVID-19 drug molnupiravir using stem cell-based embryo models, Master's Thesis, scholarspace.manoa.hawaii.edu/items/cd11342c-b4dc-44c0-8b44-ce6e3369c40b.
6.
Huntsman (B) et al., Detection of developmental toxicity of the anti-COVID-19 drug molnupiravir using gastruloid-based in vitro assays, Toxicological Sciences, doi:10.1093/toxsci/kfaf093.
7.
Zibat et al., N4-hydroxycytidine, the active compound of Molnupiravir, promotes SARS-CoV-2 mutagenesis and escape from a neutralizing nanobody, iScience, doi:10.1016/j.isci.2023.107786.
8.
Shiraki et al., Convenient screening of the reproductive toxicity of favipiravir and antiviral drugs in Caenorhabditis elegans, Heliyon, doi:10.1016/j.heliyon.2024.e35331.
9.
Gruber et al., Molnupiravir increases SARS‐CoV‐2 genome diversity and complexity: A case‐control cohort study, Journal of Medical Virology, doi:10.1002/jmv.29642.
10.
Marikawa et al., An active metabolite of the anti-COVID-19 drug molnupiravir impairs mouse preimplantation embryos at clinically relevant concentrations, Reproductive Toxicology, doi:10.1016/j.reprotox.2023.108475.
11.
Rahman, M., Elucidation of the DNA repair mechanisms involved in the repair of DNA damage caused by the Arabinosides and Anti-COVID-19 drugs, tokyo-metro-u.repo.nii.ac.jp/records/2000972.
12.
Zhou et al., β-D-N4-hydroxycytidine Inhibits SARS-CoV-2 Through Lethal Mutagenesis But Is Also Mutagenic To Mammalian Cells, The Journal of Infectious Diseases, doi:10.1093/infdis/jiab247.
13.
Chamod et al., Molnupiravir Metabolite--N4-hydroxycytidine Causes Cytotoxicity and DNA Damage in Mammalian Cells in vitro: N4-hydroxycytidine Induced Cytotoxicity DNA Damage, Asian Medical Journal and Alternative Medicine, 23:3, asianmedjam.com/index.php/amjam/article/view/1448.
14.
Standing et al., Randomized controlled trial of molnupiravir SARS-CoV-2 viral and antibody response in at-risk adult outpatients, Nature Communications, doi:10.1038/s41467-024-45641-0.
15.
Mori et al., Reactive oxygen species-mediated cytotoxic and DNA-damaging mechanism of N4-hydroxycytidine, a metabolite of the COVID-19 therapeutic drug molnupiravir, Free Radical Research, doi:10.1080/10715762.2025.2469738.
16.
Focosi et al., The fitness of molnupiravir-signed SARS-CoV-2 variants: imputation analysis based on prescription counts and GISAID analyses by country, Intervirology, doi:10.1159/000540282.
17.
Sanderson et al., A molnupiravir-associated mutational signature in global SARS-CoV-2 genomes, Nature, doi:10.1038/s41586-023-06649-6.
18.
Fountain-Jones et al., Effect of molnupiravir on SARS-CoV-2 evolution in immunocompromised patients: a retrospective observational study, The Lancet Microbe, doi:10.1016/S2666-5247(23)00393-2.
19.
Kosakovsky Pond et al., Anti-COVID drug accelerates viral evolution, Nature, doi:10.1038/d41586-023-03248-3.
21.
Siby et al., Temporal Trends in Serious Adverse Events Associated with Oral Antivirals During the COVID-19 Pandemic: Insights from the FAERS Database (2020–2023), Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1825.
22.
Ozhan et al., Evaluation of the cardiopulmonary effects of repurposed COVID-19 therapeutics in healthy rats, Scientific Reports, doi:10.1038/s41598-025-31048-4.
Yen et al., 20 Aug 2024, retrospective, Taiwan, peer-reviewed, 6 authors, study period 1 January, 2022 - 31 July, 2022.
Contact: dxd41@tpech.gov.tw.
Predictors for cause-specific and timing of deaths in patients with COVID-19: a cohort study in Taiwan
doi:10.1186/s12879-024-09654-w
Background This cohort study determines the predictors for cause-specific and timing of deaths in patients with COVID-19 in Taiwan. Methods Patients with laboratory-confirmed COVID-19 admitted to Taipei City Hospital from January 1 to July 31, 2022, were recruited in this cohort. All patients were followed up until death, discharge from the hospital, or August 31, 2022. Early deaths within the first 2 weeks were recorded, and the cause of death was confirmed by the death certificate database of Taiwan. Predictors of cause-specific and timing of deaths of patients with COVID-19 were determined using multinomial Cox proportional hazards regression analysis.
Results Of the 195 (8.0%) patients who died during hospitalization, 147 (84.0%) had COVID-19-specific deaths. Moreover, 54.9% of the deceased patients had early death. After controlling for other covariates, patients aged ≥ 65 years had a higher risk of COVID-19-specific, non-COVID-19-specific, early, and late deaths [adjusted hazards ratio (AHR): 3.85, 6.45, 3.33, and 6.57; 95% confidence interval (CI): 1. 91-7.78, 1.17-35.68, 1.51-7.36, and 2.18-19.76, respectively]. Fully vaccinated patients had a lower risk of COVID-19-specific (AHR: 0.68; 95% CI: 0.47-0.98) and early deaths (AHR: 0.54; 95% CI: 0.35-0.84), whereas comorbid patients with chronic obstructive pulmonary disease had a higher risk of non-COVID-19-specific deaths (AHR: 5.43; 95% CI: 1.73-17.03).
Conclusions This study suggests that prioritizing COVID-19 vaccination and carefully monitoring comorbid patients during hospitalization can reduce the risk of COVID-19-specific and early deaths and non-COVID-19-specific mortalities, respectively.
Abbreviations
Declarations Ethics approval and consent to participate This study was approved by the Institutional Review Board of Taipei City Hospital (no. TCHIRB-10904014-E). Formal consent is waived for this type of study.
Consent for publication Not Applicable.
Competing interests The authors declare no competing interests.
Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Berrino, Donzelli, Bellavite, Malatesta, COVID-19 vaccination and all-cause and non-COVID-19 mortality. A revaluation of a study carried out in an Italian Province, Epidemiologia e prevenzione
Bienvenu, Noonan, Wang, Peter, Higher mortality of COVID-19 in males: sex differences in immune response and cardiovascular comorbidities, Cardiovasc Res
Chen, Cheuh, Chen, Kuo, Epidemiological characteristics of the three waves of COVID-19 epidemic in Taiwan during April 2022 to March 2023, J Formos Med Assoc
De Roquetaillade, Bredin, Lascarrou, Soumagne, Cojocaru et al., Timing and causes of death in severe COVID-19 patients, Crit Care
Finelli, Gupta, Petigara, Yu, Bauer et al., Mortality among US patients hospitalized with SARS-CoV-2 infection in 2020, JAMA Netw Open
Gray, Navaratnam, Day, Wendon, Briggs, Changes in COVID-19 in-hospital mortality in hospitalised adults in England over the first seven months of the pandemic: an observational study using administrative data, Lancet Reg Health Eur
Hiscott, Alexandridi, Muscolini, Tassone, Palermo et al., The global impact of the coronavirus pandemic, Cytokine Growth Factor Rev
Hu, Guo, Zhou, Shi, Characteristics of SARS-CoV-2 and COVID-19, Nat Rev Microbiol
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet
Kabir, Ahmed, Chowdhury, Iqbal, Paulmurugan et al., Management of COVID-19: current status and future prospects, Microbes Infect
Lu, Lee, Chou, Accuracy of cause-of-death coding in Taiwan: types of miscoding and effects on mortality statistics, Int J Epidemiol
Meng, Lu, Guo, Liu, Yang et al., Cancer history is an independent risk factor for mortality in hospitalized COVID-19 patients: a propensity score-matched analysis, J Hematol Oncol
Mølhave, Agergaard, Wejse, Clinical management of COVID-19 patients -an update, Semin Nucl Med
Opal, Girard, Ely, The immunopathogenesis of sepsis in elderly patients, Clin Infect Dis
Peña, Rascón-Pacheco, Ascencio-Montiel, González-Figueroa, Fernández-Gárate et al., Hypertension, diabetes and obesity, major risk factors for death in patients with COVID-19 in Mexico, Arch Med Res
Rahmani, Shavaleh, Forouhi, Disfani, Kamandi et al., The effectiveness of COVID-19 vaccines in reducing the incidence, hospitalization, and mortality from COVID-19: a systematic review and meta-analysis, Front Public Health
Sadarangani, Marchant, Kollmann, Immunological mechanisms of vaccine-induced protection against COVID-19 in humans, Nat Rev Immunol
Sheng, Hsieh, Chang, Achievements of COVID-19 vaccination programs: Taiwanese perspective, J Formos Med Assoc
Smits, De Lang, Van Den Brand, Leijten, Van et al., Exacerbated innate host response to SARS-CoV in aged non-human primates, PLoS pathogens
Watson, Barnsley, Toor, Hogan, Winskill et al., Global impact of the first year of COVID-19 vaccination: a mathematical modelling study, Lancet Infect Dis
Wu, Mcgoogan, Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention, JAMA
Yung, Li, Kehm, Cone, Parton et al., COVID-19-Specific Mortality among World Trade Center Health Registry Enrollees Who Resided in New York City, Int J Environ Res Public Health
Zheng, Shao, Chen, Zhang, Wang et al., Real-world effectiveness of COVID-19 vaccines: a literature review and meta-analysis, Int J Infect Dis
DOI record:
{
"DOI": "10.1186/s12879-024-09654-w",
"ISSN": [
"1471-2334"
],
"URL": "http://dx.doi.org/10.1186/s12879-024-09654-w",
"alternative-id": [
"9654"
],
"article-number": "840",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "18 October 2023"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "23 July 2024"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "20 August 2024"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Ethics approval and consent to participate",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "This study was approved by the Institutional Review Board of Taipei City Hospital (no. TCHIRB-10904014-E). Formal consent is waived for this type of study."
},
{
"group": {
"label": "Consent for publication",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "Not Applicable."
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 4,
"value": "The authors declare no competing interests."
}
],
"author": [
{
"affiliation": [],
"family": "Yen",
"given": "Yung-Feng",
"sequence": "first"
},
{
"affiliation": [],
"family": "Chan",
"given": "Shang-Yih",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lai",
"given": "Yun-Ju",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yen",
"given": "Muh-Yong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chen",
"given": "Chu-Chieh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chen",
"given": "Mei-Ju",
"sequence": "additional"
}
],
"container-title": "BMC Infectious Diseases",
"container-title-short": "BMC Infect Dis",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2024,
8,
20
]
],
"date-time": "2024-08-20T06:02:39Z",
"timestamp": 1724133759000
},
"deposited": {
"date-parts": [
[
2024,
8,
20
]
],
"date-time": "2024-08-20T06:02:44Z",
"timestamp": 1724133764000
},
"funder": [
{
"DOI": "10.13039/501100015835",
"award": [
"No. 11101-62-042; No. 11201-62-023"
],
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/501100015835",
"id-type": "DOI"
}
],
"name": "Department of Health, Taipei City Government"
}
],
"indexed": {
"date-parts": [
[
2024,
8,
28
]
],
"date-time": "2024-08-28T14:10:53Z",
"timestamp": 1724854253046
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2024,
8,
20
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2024,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc-nd/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
8,
20
]
],
"date-time": "2024-08-20T00:00:00Z",
"timestamp": 1724112000000
}
},
{
"URL": "https://creativecommons.org/licenses/by-nc-nd/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
8,
20
]
],
"date-time": "2024-08-20T00:00:00Z",
"timestamp": 1724112000000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1186/s12879-024-09654-w.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1186/s12879-024-09654-w/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1186/s12879-024-09654-w.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1186",
"published": {
"date-parts": [
[
2024,
8,
20
]
]
},
"published-online": {
"date-parts": [
[
2024,
8,
20
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1016/j.cytogfr.2020.05.010",
"author": "J Hiscott",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Cytokine Growth Factor Rev",
"key": "9654_CR1",
"unstructured": "Hiscott J, Alexandridi M, Muscolini M, Tassone E, Palermo E, Soultsioti M, Zevini A. The global impact of the coronavirus pandemic. Cytokine Growth Factor Rev. 2020;53:1–9.",
"volume": "53",
"year": "2020"
},
{
"key": "9654_CR2",
"unstructured": "World Health Organization: Coronavirus disease (COVID-19) Pandemic. https://www.who.int/publications/m/item/covid-19-weekly-epidemiological-update---21-december-2022. Accessed 16 July 2023."
},
{
"DOI": "10.1093/cvr/cvaa284",
"author": "LA Bienvenu",
"doi-asserted-by": "publisher",
"first-page": "2197",
"issue": "14",
"journal-title": "Cardiovasc Res",
"key": "9654_CR3",
"unstructured": "Bienvenu LA, Noonan J, Wang X, Peter K. Higher mortality of COVID-19 in males: sex differences in immune response and cardiovascular comorbidities. Cardiovasc Res. 2020;116(14):2197–206.",
"volume": "116",
"year": "2020"
},
{
"DOI": "10.1016/j.arcmed.2020.12.002",
"author": "JE Peña",
"doi-asserted-by": "publisher",
"first-page": "443",
"issue": "4",
"journal-title": "Arch Med Res",
"key": "9654_CR4",
"unstructured": "Peña JE, Rascón-Pacheco RA, Ascencio-Montiel IJ, González-Figueroa E, Fernández-Gárate JE, Medina-Gómez OS, Borja-Bustamante P, Santillán-Oropeza JA, Borja-Aburto VH. Hypertension, diabetes and obesity, major risk factors for death in patients with COVID-19 in Mexico. Arch Med Res. 2021;52(4):443–9.",
"volume": "52",
"year": "2021"
},
{
"DOI": "10.1186/s13045-020-00907-0",
"author": "Y Meng",
"doi-asserted-by": "publisher",
"first-page": "75",
"issue": "1",
"journal-title": "J Hematol Oncol",
"key": "9654_CR5",
"unstructured": "Meng Y, Lu W, Guo E, Liu J, Yang B, Wu P, Lin S, Peng T, Fu Y, Li F, et al. Cancer history is an independent risk factor for mortality in hospitalized COVID-19 patients: a propensity score-matched analysis. J Hematol Oncol. 2020;13(1):75.",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.3390/ijerph192114348",
"author": "J Yung",
"doi-asserted-by": "publisher",
"first-page": "14348",
"issue": "21",
"journal-title": "Int J Environ Res Public Health",
"key": "9654_CR6",
"unstructured": "Yung J, Li J, Kehm RD, Cone JE, Parton H, Huynh M, Farfel MR. COVID-19-Specific Mortality among World Trade Center Health Registry Enrollees Who Resided in New York City. Int J Environ Res Public Health. 2022;19(21):14348.",
"volume": "19",
"year": "2022"
},
{
"DOI": "10.1001/jama.2020.2648",
"author": "Z Wu",
"doi-asserted-by": "publisher",
"first-page": "1239",
"issue": "13",
"journal-title": "JAMA",
"key": "9654_CR7",
"unstructured": "Wu Z, McGoogan JM. Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–42.",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1038/s41579-020-00459-7",
"author": "B Hu",
"doi-asserted-by": "publisher",
"first-page": "141",
"issue": "3",
"journal-title": "Nat Rev Microbiol",
"key": "9654_CR8",
"unstructured": "Hu B, Guo H, Zhou P, Shi ZL. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol. 2021;19(3):141–54.",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.6556",
"author": "L Finelli",
"doi-asserted-by": "publisher",
"first-page": "e216556",
"issue": "4",
"journal-title": "JAMA Netw Open",
"key": "9654_CR9",
"unstructured": "Finelli L, Gupta V, Petigara T, Yu K, Bauer KA, Puzniak LA. Mortality among US patients hospitalized with SARS-CoV-2 infection in 2020. JAMA Netw Open. 2021;4(4):e216556.",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"author": "C Huang",
"doi-asserted-by": "publisher",
"first-page": "497",
"issue": "10223",
"journal-title": "Lancet (London, England)",
"key": "9654_CR10",
"unstructured": "Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet (London, England). 2020;395(10223):497–506.",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1186/s13054-021-03639-w",
"author": "C de Roquetaillade",
"doi-asserted-by": "publisher",
"first-page": "224",
"issue": "1",
"journal-title": "Crit Care (London, England)",
"key": "9654_CR11",
"unstructured": "de Roquetaillade C, Bredin S, Lascarrou JB, Soumagne T, Cojocaru M, Chousterman BG, Leclerc M, Gouhier A, Piton G, Pène F, et al. Timing and causes of death in severe COVID-19 patients. Crit Care (London, England). 2021;25(1):224.",
"volume": "25",
"year": "2021"
},
{
"key": "9654_CR12",
"unstructured": "Taiwan Centers for Disease Control and Prevention. [Surveillance of COVID-19]. https://www.cdc.gov.tw/En. Accessed 29 Apr 2020."
},
{
"DOI": "10.1093/ije/29.2.336",
"author": "TH Lu",
"doi-asserted-by": "publisher",
"first-page": "336",
"issue": "2",
"journal-title": "Int J Epidemiol",
"key": "9654_CR13",
"unstructured": "Lu TH, Lee MC, Chou MC. Accuracy of cause-of-death coding in Taiwan: types of miscoding and effects on mortality statistics. Int J Epidemiol. 2000;29(2):336–43.",
"volume": "29",
"year": "2000"
},
{
"key": "9654_CR14",
"unstructured": "Taiwan Centers for Disease Control and Prevention: Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19). https://www.cdc.gov.tw/Category/Page/xCSwc5oznwcqunujPc-qmQ. Accessed 21 Mar 2023."
},
{
"DOI": "10.1016/j.lanepe.2021.100104",
"author": "WK Gray",
"doi-asserted-by": "publisher",
"first-page": "100104",
"journal-title": "Lancet Reg Health Eur",
"key": "9654_CR15",
"unstructured": "Gray WK, Navaratnam AV, Day J, Wendon J, Briggs TWR. Changes in COVID-19 in-hospital mortality in hospitalised adults in England over the first seven months of the pandemic: an observational study using administrative data. Lancet Reg Health Eur. 2021;5:100104.",
"volume": "5",
"year": "2021"
},
{
"DOI": "10.3389/fpubh.2022.873596",
"author": "K Rahmani",
"doi-asserted-by": "publisher",
"first-page": "873596",
"journal-title": "Front Public Health",
"key": "9654_CR16",
"unstructured": "Rahmani K, Shavaleh R, Forouhi M, Disfani HF, Kamandi M, Oskooi RK, Foogerdi M, Soltani M, Rahchamani M, Mohaddespour M, et al. The effectiveness of COVID-19 vaccines in reducing the incidence, hospitalization, and mortality from COVID-19: a systematic review and meta-analysis. Front Public Health. 2022;10:873596.",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1053/j.semnuclmed.2021.06.004",
"author": "M Mølhave",
"doi-asserted-by": "publisher",
"first-page": "4",
"issue": "1",
"journal-title": "Semin Nucl Med",
"key": "9654_CR17",
"unstructured": "Mølhave M, Agergaard J, Wejse C. Clinical management of COVID-19 patients - an update. Semin Nucl Med. 2022;52(1):4–10.",
"volume": "52",
"year": "2022"
},
{
"DOI": "10.1016/j.micinf.2021.104832",
"author": "MA Kabir",
"doi-asserted-by": "publisher",
"first-page": "104832",
"issue": "4–5",
"journal-title": "Microbes Infect",
"key": "9654_CR18",
"unstructured": "Kabir MA, Ahmed R, Chowdhury R, Iqbal SMA, Paulmurugan R, Demirci U, Asghar W. Management of COVID-19: current status and future prospects. Microbes Infect. 2021;23(4–5):104832.",
"volume": "23",
"year": "2021"
},
{
"DOI": "10.1086/432007",
"author": "SM Opal",
"doi-asserted-by": "publisher",
"first-page": "S504",
"issue": "Suppl 7",
"journal-title": "Clin Infect Dis",
"key": "9654_CR19",
"unstructured": "Opal SM, Girard TD, Ely EW. The immunopathogenesis of sepsis in elderly patients. Clin Infect Dis. 2005;41(Suppl 7):S504-512.",
"volume": "41",
"year": "2005"
},
{
"DOI": "10.1371/journal.ppat.1000756",
"author": "SL Smits",
"doi-asserted-by": "publisher",
"first-page": "e1000756",
"issue": "2",
"journal-title": "PLoS pathogens",
"key": "9654_CR20",
"unstructured": "Smits SL, de Lang A, van den Brand JM, Leijten LM, van IWF, Eijkemans MJ, van Amerongen G, Kuiken T, Andeweg AC, Osterhaus AD, et al. Exacerbated innate host response to SARS-CoV in aged non-human primates. PLoS pathogens. 2010;6(2):e1000756.",
"volume": "6",
"year": "2010"
},
{
"DOI": "10.1016/j.jfma.2023.04.017",
"author": "WH Sheng",
"doi-asserted-by": "publisher",
"first-page": "S70",
"issue": "Suppl 1",
"journal-title": "J Formos Med Assoc",
"key": "9654_CR21",
"unstructured": "Sheng WH, Hsieh SM, Chang SC. Achievements of COVID-19 vaccination programs: Taiwanese perspective. J Formos Med Assoc. 2024;123(Suppl 1):S70-s76.",
"volume": "123",
"year": "2024"
},
{
"DOI": "10.1016/S1473-3099(22)00320-6",
"author": "OJ Watson",
"doi-asserted-by": "publisher",
"first-page": "1293",
"issue": "9",
"journal-title": "Lancet Infect Dis",
"key": "9654_CR22",
"unstructured": "Watson OJ, Barnsley G, Toor J, Hogan AB, Winskill P, Ghani AC. Global impact of the first year of COVID-19 vaccination: a mathematical modelling study. Lancet Infect Dis. 2022;22(9):1293–302.",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.1016/j.ijid.2021.11.009",
"author": "C Zheng",
"doi-asserted-by": "publisher",
"first-page": "252",
"journal-title": "Int J Infect Dis",
"key": "9654_CR23",
"unstructured": "Zheng C, Shao W, Chen X, Zhang B, Wang G, Zhang W. Real-world effectiveness of COVID-19 vaccines: a literature review and meta-analysis. Int J Infect Dis. 2022;114:252–60.",
"volume": "114",
"year": "2022"
},
{
"DOI": "10.1038/s41577-021-00578-z",
"author": "M Sadarangani",
"doi-asserted-by": "publisher",
"first-page": "475",
"issue": "8",
"journal-title": "Nat Rev Immunol",
"key": "9654_CR24",
"unstructured": "Sadarangani M, Marchant A, Kollmann TR. Immunological mechanisms of vaccine-induced protection against COVID-19 in humans. Nat Rev Immunol. 2021;21(8):475–84.",
"volume": "21",
"year": "2021"
},
{
"author": "F Berrino",
"first-page": "374",
"issue": "6",
"journal-title": "Epidemiologia e prevenzione",
"key": "9654_CR25",
"unstructured": "Berrino F, Donzelli A, Bellavite P, Malatesta G. COVID-19 vaccination and all-cause and non-COVID-19 mortality. A revaluation of a study carried out in an Italian Province. Epidemiologia e prevenzione. 2023;47(6):374–8.",
"volume": "47",
"year": "2023"
},
{
"DOI": "10.1016/j.jfma.2023.05.027",
"author": "YH Chen",
"doi-asserted-by": "publisher",
"first-page": "1174",
"issue": "11",
"journal-title": "J Formos Med Assoc",
"key": "9654_CR26",
"unstructured": "Chen YH, Cheuh YN, Chen CM, Kuo HW. Epidemiological characteristics of the three waves of COVID-19 epidemic in Taiwan during April 2022 to March 2023. J Formos Med Assoc. 2023;122(11):1174–82.",
"volume": "122",
"year": "2023"
}
],
"reference-count": 26,
"references-count": 26,
"relation": {},
"resource": {
"primary": {
"URL": "https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-024-09654-w"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Predictors for cause-specific and timing of deaths in patients with COVID-19: a cohort study in Taiwan",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "24"
}