Micronutrient Status of Critically Ill Patients with COVID-19 Pneumonia
et al., Nutrients, doi:10.3390/nu16030385, Jan 2024
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
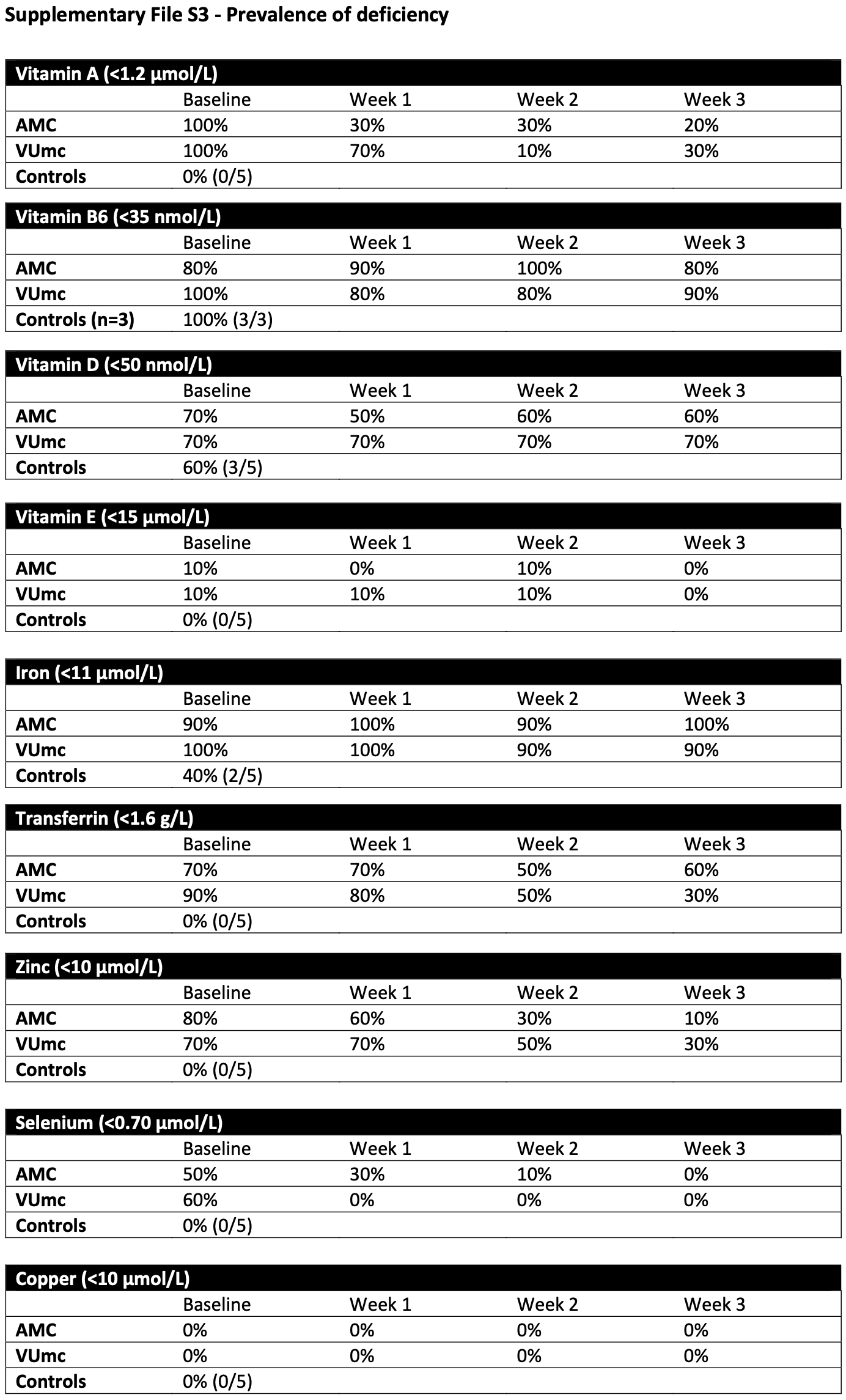
Prospective pilot study of 20 critically ill COVID-19 ICU patients showing high deficiency rates of 50-100% for vitamins A, B6, and D; zinc; and selenium at admission. Deficiencies of vitamins B6 and D, and low iron status, persisted after 3 weeks. Plasma levels of vitamins A and E, zinc, and selenium increased over time as inflammation resolved, suggesting redistribution may explain some observed deficiencies. All patients received daily micronutrient administration. Additional intravenous and oral micronutrient administration for 10 patients did not significantly impact micronutrient levels or deficiency rates, however authors note that the administered doses may be too low. The form of vitamin D is not specified but may have been cholecalciferol which is expected to have a very long onset of action compared to more appropriate forms such as calcifediol or calcitriol.
This is the 193rd of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of ICU admission, 35.7% lower, OR 0.64, p = 0.67, high D levels (≥50nmol/L) 6 of 20 (30.0%) cases,
2 of 5 (40.0%) controls, NNT 14, case control OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Rozemeijer et al., 29 Jan 2024, prospective, Netherlands, peer-reviewed, 9 authors.
Micronutrient Status of Critically Ill Patients with COVID-19 Pneumonia
Nutrients, doi:10.3390/nu16030385
Micronutrient deficiencies can develop in critically ill patients, arising from factors such as decreased intake, increased losses, drug interactions, and hypermetabolism. These deficiencies may compromise important immune functions, with potential implications for patient outcomes. Alternatively, micronutrient blood levels may become low due to inflammation-driven redistribution rather than consumption. This explorative pilot study investigates blood micronutrient concentrations during the first three weeks of ICU stay in critically ill COVID-19 patients and evaluates the impact of additional micronutrient administration. Moreover, associations between inflammation, disease severity, and micronutrient status were explored. We measured weekly concentrations of vitamins A, B6, D, and E; iron; zinc; copper; selenium; and CRP as a marker of inflammation state and the SOFA score indicating disease severity in 20 critically ill COVID-19 patients during three weeks of ICU stay. Half of the patients received additional (intravenous) micronutrient administration. Data were analyzed with linear mixed models and Pearson's correlation coefficient. High deficiency rates of vitamins A, B6, and D; zinc; and selenium (50-100%) were found at ICU admission, along with low iron status. After three weeks, vitamins B6 and D deficiencies persisted, and iron status remained low. Plasma levels of vitamins A and E, zinc, and selenium improved. No significant differences in micronutrient levels were found between patient groups. Negative correlations were identified between the CRP level and levels of vitamins A and E, iron, transferrin, zinc, and selenium. SOFA scores negatively correlated with vitamin D and selenium levels. Our findings reveal high micronutrient deficiency rates at ICU admission. Additional micronutrient administration did not enhance levels or expedite their increase. Spontaneous increases in vitamins A and E, zinc, and selenium levels were associated with inflammation resolution, suggesting that observed low levels may be attributed, at least in part, to redistribution rather than true deficiencies.
Conflicts of Interest: The authors declare no conflict of interest.
References
Argano, Mallaci Bocchio, Natoli, Scibetta, Lo Monaco et al., Protective Effect of Vitamin D Supplementation on COVID-19-Related Intensive Care Hospitalization and Mortality: Definitive Evidence from Meta-Analysis and Trial Sequential Analysis, Pharmaceuticals, doi:10.3390/ph16010130
Beigmohammadi, Bitarafan, Abdollahi, Amoozadeh, Salahshour et al., The association between serum levels of micronutrients and the severity of disease in patients with COVID-19, Nutrition, doi:10.1016/j.nut.2021.111400
Beigmohammadi, Bitarafan, Hoseindokht, Abdollahi, Amoozadeh et al., The effect of supplementation with vitamins A, B, C, D, and E on disease severity and inflammatory responses in patients with COVID-19: A randomized clinical trial, Trials, doi:10.1186/s13063-021-05795-4
Berger, Shenkin, Schweinlin, Amrein, Augsburger et al., ESPEN micronutrient guideline, Clin. Nutr, doi:10.1016/j.clnu.2022.02.015
Bilezikian, Binkley, De Luca, Fassio, Formenti et al., Consensus and Controversial Aspects of Vitamin D and COVID-19, J. Clin. Endocrinol. Metab, doi:10.1210/clinem/dgac719
Bolondi, Russo, Gamberini, Circelli, Meca et al., Iron metabolism and lymphocyte characterisation during COVID-19 infection in ICU patients: An observational cohort study, World J. Emerg. Surg, doi:10.1186/s13017-020-00323-2
Calder, Carr, Gombart, Eggersdorfer, Optimal Nutritional Status for a Well-Functioning Immune System Is an Important Factor to Protect against Viral Infections, Nutrients, doi:10.3390/nu12041181
Dignass, Farrag, Stein, Limitations of Serum Ferritin in Diagnosing Iron Deficiency in Inflammatory Conditions, Int. J. Chronic. Dis, doi:10.1155/2018/9394060
Dirks, Ackermans, Jonge, Heijboer, Reference values for 24,25-dihydroxyvitamin D and the 25hydroxyvitamin D/24,25-dihydroxyvitamin D ratio, Clin. Chem. Lab. Med. (CCLM), doi:10.1515/cclm-2018-1096
Driskell, Neese, Bryant, Bashor, Measurement of vitamin A and vitamin E in human serum by highperformance liquid chromatography, J. Chromatogr, doi:10.1016/S0378-4347(00)81869-1
Duncan, Talwar, Mcmillan, Stefanowicz, O'reilly, Quantitative data on the magnitude of the systemic inflammatory response and its effect on micronutrient status based on plasma measurements, Am. J. Clin. Nutr, doi:10.3945/ajcn.111.023812
Fakhrolmobasheri, Mazaheri-Tehrani, Kieliszek, Zeinalian, Abbasi et al., COVID-19 and Selenium Deficiency: A Systematic Review, Biol. Trace Elem. Res, doi:10.1007/s12011-021-02997-4
Fernandez-Quintela, Milton-Laskibar, Trepiana, Gomez-Zorita, Kajarabille et al., Key Aspects in Nutritional Management of COVID-19 Patients, J. Clin. Med, doi:10.3390/jcm9082589
Herrera-Quintana, Gamarra-Morales, Vázquez-Lorente, Molina-López, Castaño-Pérez et al., Bad Prognosis in Critical Ill Patients with COVID-19 during Short-Term ICU Stay regarding Vitamin D Levels, Nutrients, doi:10.3390/nu13061988
Hippchen, Altamura, Muckenthaler, Merle, ypoferremia is Associated With Increased Hospitalization and Oxygen Demand in COVID-19 Patients, Hemasphere, doi:10.1097/HS9.0000000000000492
Im, Je, Baek, Chung, Kwon et al., Nutritional status of patients with COVID-19, Int. J. Infect. Dis, doi:10.1016/j.ijid.2020.08.018
Jain, Chaurasia, Sengar, Singh, Mahor et al., Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers, Sci. Rep, doi:10.1038/s41598-020-77093-z
Kazemi, Mohammadi, Aghababaee, Golzarand, Clark et al., Association of Vitamin D Status with SARS-CoV-2 Infection or COVID-19 Severity: A Systematic Review and Meta-analysis, Adv. Nutr, doi:10.1093/advances/nmab012
Luo, Liao, Shen, Li, Cheng, Vitamin D Deficiency Is Associated with COVID-19 Incidence and Disease Severity in Chinese People, J. Nutr, doi:10.1093/jn/nxaa332
Manzanares, Lemieux, Elke, Langlois, Bloos et al., High-dose intravenous selenium does not improve clinical outcomes in the critically ill: A systematic review and meta-analysis, Crit. Care, doi:10.1186/s13054-016-1529-5
Manzanares, Moreira, Hardy, Pharmaconutrition revisited for critically ill patients with coronavirus disease 2019 (COVID-19): Does selenium have a place?, Nutrition, doi:10.1016/j.nut.2020.110989
Moghaddam, Heller, Sun, Seelig, Cherkezov et al., Selenium Deficiency Is Associated with Mortality Risk from COVID-19, Nutrients, doi:10.3390/nu12072098
Mousavi, Saghaleini, Mahmoodpoor, Ghojazadeh, Mousavi, Daily parenteral selenium therapy in critically ill patients: An updated systematic review and meta-analysis of randomized controlled trials, Clin. Nutr. ESPEN, doi:10.1016/j.clnesp.2020.11.026
Murai, Fernandes, Sales, Pinto, Goessler et al., Effect of a Single High Dose of Vitamin D3 on Hospital Length of Stay in Patients With Moderate to Severe COVID-19: A Randomized Clinical Trial, JAMA, doi:10.1001/jama.2020.26848
Notz, Herrmann, Schlesinger, Helmer, Sudowe et al., Clinical Significance of Micronutrient Supplementation in Critically Ill COVID-19 Patients with Severe ARDS, Nutrients, doi:10.3390/nu13062113
Panagiotou, Tee, Ihsan, Athar, Marchitelli et al., Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalized with COVID-19 are associated with greater disease severity, Clin. Endocrinol, doi:10.1111/cen.14276
Patel, Chinni, El-Khoury, Perera, Neto et al., A pilot double-blind safety and feasibility randomized controlled trial of high-dose intravenous zinc in hospitalized COVID-19 patients, J. Med. Virol, doi:10.1002/jmv.26895
Romano, Bilotta, Dauri, Macheda, Pujia et al., Short Report-Medical nutrition therapy for critically ill patients with COVID-19, Eur. Rev. Med. Pharmacol. Sci
Shah, Frost, Aaron, Donovan, Drakesmith et al., Systemic hypoferremia and severity of hypoxemic respiratory failure in COVID-19, Crit. Care, doi:10.1186/s13054-020-03051-w
Smolders, Van Den Ouweland, Geven, Pickkers, Kox, Letter to the Editor: Vitamin D deficiency in COVID-19: Mixing up cause and consequence, Metabolism, doi:10.1016/j.metabol.2020.154434
Talwar, Quasim, Mcmillan, Kinsella, Williamson et al., Optimisation and validation of a sensitive high-performance liquid chromatography assay for routine measurement of pyridoxal 5-phosphate in human plasma and red cells using pre-column semicarbazide derivatisation, J. Chromatogr. B Analyt. Technol. Biomed. Life Sci, doi:10.1016/S1570-0232(03)00320-9
Tepasse, Vollenberg, Fobker, Kabar, Schmidt et al., Vitamin A Plasma Levels in COVID-19 Patients: A Prospective Multicenter Study and Hypothesis, Nutrients, doi:10.3390/nu13072173
Thomas, Patel, Bittel, Wolski, Wang et al., Effect of High-Dose Zinc and Ascorbic Acid Supplementation vs Usual Care on Symptom Length and Reduction Among Ambulatory Patients With SARS-CoV-2 Infection: The COVID A to Z Randomized Clinical Trial, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2021.0369
Tomasa-Irriguible, Bielsa-Berrocal, Bordeje-Laguna, Tural-Llacher, Barallat et al., Low Levels of Few Micronutrients May Impact COVID-19 Disease Progression: An Observational Study on the First Wave, Metabolites, doi:10.3390/metabo11090565
Vasheghani, Jannati, Baghaei, Rezaei, Aliyari et al., The relationship between serum 25-hydroxyvitamin D levels and the severity of COVID-19 disease and its mortality, Sci. Rep, doi:10.1038/s41598-021-97017-9
Zhang, Liu, Potential interventions for novel coronavirus in China: A systematic review, J. Med. Virol, doi:10.1002/jmv.25707
Zhao, Huang, Dai, Feng, Liu et al., Serum Iron Level as a Potential Predictor of Coronavirus Disease 2019 Severity and Mortality: A Retrospective Study, Open Forum. Infect. Dis, doi:10.1093/ofid/ofaa250
DOI record:
{
"DOI": "10.3390/nu16030385",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu16030385",
"abstract": "<jats:p>Micronutrient deficiencies can develop in critically ill patients, arising from factors such as decreased intake, increased losses, drug interactions, and hypermetabolism. These deficiencies may compromise important immune functions, with potential implications for patient outcomes. Alternatively, micronutrient blood levels may become low due to inflammation-driven redistribution rather than consumption. This explorative pilot study investigates blood micronutrient concentrations during the first three weeks of ICU stay in critically ill COVID-19 patients and evaluates the impact of additional micronutrient administration. Moreover, associations between inflammation, disease severity, and micronutrient status were explored. We measured weekly concentrations of vitamins A, B6, D, and E; iron; zinc; copper; selenium; and CRP as a marker of inflammation state and the SOFA score indicating disease severity in 20 critically ill COVID-19 patients during three weeks of ICU stay. Half of the patients received additional (intravenous) micronutrient administration. Data were analyzed with linear mixed models and Pearson’s correlation coefficient. High deficiency rates of vitamins A, B6, and D; zinc; and selenium (50–100%) were found at ICU admission, along with low iron status. After three weeks, vitamins B6 and D deficiencies persisted, and iron status remained low. Plasma levels of vitamins A and E, zinc, and selenium improved. No significant differences in micronutrient levels were found between patient groups. Negative correlations were identified between the CRP level and levels of vitamins A and E, iron, transferrin, zinc, and selenium. SOFA scores negatively correlated with vitamin D and selenium levels. Our findings reveal high micronutrient deficiency rates at ICU admission. Additional micronutrient administration did not enhance levels or expedite their increase. Spontaneous increases in vitamins A and E, zinc, and selenium levels were associated with inflammation resolution, suggesting that observed low levels may be attributed, at least in part, to redistribution rather than true deficiencies.</jats:p>",
"alternative-id": [
"nu16030385"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-1185-4373",
"affiliation": [
{
"name": "Department of Intensive Care Medicine, Research VUmc Intensive Care (REVIVE), Amsterdam Cardiovascular Science (ACS), Amsterdam Infection and Immunity Institute (AI&II), Amsterdam Medical Data Science (AMDS), Amsterdam UMC, Location VUmc, Vrije Universiteit Amsterdam, De Boelelaan 1117, 1081 HV Amsterdam, The Netherlands"
},
{
"name": "Department of Anesthesiology, Amsterdam UMC, Location VUmc, Vrije Universiteit Amsterdam, De Boelelaan 1117, 1081 HV Amsterdam, The Netherlands"
}
],
"authenticated-orcid": false,
"family": "Rozemeijer",
"given": "Sander",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Laboratory Medicine, Laboratory Specialized Techniques and Research, Amsterdam Gastroenterology Endocrinology and Metabolism, 1105 AZ Amsterdam, The Netherlands"
}
],
"family": "Hamer",
"given": "Henrike M.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6712-9955",
"affiliation": [
{
"name": "Department of Laboratory Medicine, Endocrine Laboratory, Amsterdam Gastroenterology Endocrinology and Metabolism, 1105 AZ Amsterdam, The Netherlands"
}
],
"authenticated-orcid": false,
"family": "Heijboer",
"given": "Annemieke C.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Laboratory Medicine, Amsterdam Gastroenterology Endocrinology and Metabolism, 1105 AZ Amsterdam, The Netherlands"
}
],
"family": "de Jonge",
"given": "Robert",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "OncoProteomics Laboratory, Department Laboratory Medical Oncology, Amsterdam UMC, 1081 HV Amsterdam, The Netherlands"
}
],
"family": "Jimenez",
"given": "Connie R.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Intensive Care and Laboratory of Translational Intensive Care, Erasmus Medical Center, 3015 GD Rotterdam, The Netherlands"
}
],
"family": "Juffermans",
"given": "Nicole P.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1095-3502",
"affiliation": [
{
"name": "Department of Anesthesiology, Amsterdam UMC, Location VUmc, Vrije Universiteit Amsterdam, De Boelelaan 1117, 1081 HV Amsterdam, The Netherlands"
}
],
"authenticated-orcid": false,
"family": "Dujardin",
"given": "Romein W. G.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Intensive Care Medicine, Research VUmc Intensive Care (REVIVE), Amsterdam Cardiovascular Science (ACS), Amsterdam Infection and Immunity Institute (AI&II), Amsterdam Medical Data Science (AMDS), Amsterdam UMC, Location VUmc, Vrije Universiteit Amsterdam, De Boelelaan 1117, 1081 HV Amsterdam, The Netherlands"
}
],
"family": "Girbes",
"given": "Armand R. J.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Intensive Care Medicine, Research VUmc Intensive Care (REVIVE), Amsterdam Cardiovascular Science (ACS), Amsterdam Infection and Immunity Institute (AI&II), Amsterdam Medical Data Science (AMDS), Amsterdam UMC, Location VUmc, Vrije Universiteit Amsterdam, De Boelelaan 1117, 1081 HV Amsterdam, The Netherlands"
}
],
"family": "de Man",
"given": "Angélique M. E.",
"sequence": "additional"
}
],
"container-title": "Nutrients",
"container-title-short": "Nutrients",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
1,
29
]
],
"date-time": "2024-01-29T13:54:03Z",
"timestamp": 1706536443000
},
"deposited": {
"date-parts": [
[
2024,
1,
30
]
],
"date-time": "2024-01-30T09:21:53Z",
"timestamp": 1706606513000
},
"indexed": {
"date-parts": [
[
2024,
1,
31
]
],
"date-time": "2024-01-31T00:42:14Z",
"timestamp": 1706661734101
},
"is-referenced-by-count": 0,
"issue": "3",
"issued": {
"date-parts": [
[
2024,
1,
29
]
]
},
"journal-issue": {
"issue": "3",
"published-online": {
"date-parts": [
[
2024,
2
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
1,
29
]
],
"date-time": "2024-01-29T00:00:00Z",
"timestamp": 1706486400000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/16/3/385/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "385",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2024,
1,
29
]
]
},
"published-online": {
"date-parts": [
[
2024,
1,
29
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"article-title": "Short Report—Medical nutrition therapy for critically ill patients with COVID-19",
"author": "Romano",
"first-page": "4035",
"journal-title": "Eur. Rev. Med. Pharmacol. Sci.",
"key": "ref_1",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1002/jmv.25707",
"article-title": "Potential interventions for novel coronavirus in China: A systematic review",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "479",
"journal-title": "J. Med. Virol.",
"key": "ref_2",
"volume": "92",
"year": "2020"
},
{
"DOI": "10.3390/nu12041181",
"doi-asserted-by": "crossref",
"key": "ref_3",
"unstructured": "Calder, P.C., Carr, A.C., Gombart, A.F., and Eggersdorfer, M. (2020). Optimal Nutritional Status for a Well-Functioning Immune System Is an Important Factor to Protect against Viral Infections. Nutrients, 12."
},
{
"DOI": "10.3390/jcm9082589",
"doi-asserted-by": "crossref",
"key": "ref_4",
"unstructured": "Fernandez-Quintela, A., Milton-Laskibar, I., Trepiana, J., Gomez-Zorita, S., Kajarabille, N., Leniz, A., Gonzalez, M., and Portillo, M.P. (2020). Key Aspects in Nutritional Management of COVID-19 Patients. J. Clin. Med., 9."
},
{
"DOI": "10.3390/metabo11090565",
"doi-asserted-by": "crossref",
"key": "ref_5",
"unstructured": "Tomasa-Irriguible, T.M., Bielsa-Berrocal, L., Bordeje-Laguna, L., Tural-Llacher, C., Barallat, J., Manresa-Dominguez, J.M., and Toran-Monserrat, P. (2021). Low Levels of Few Micronutrients May Impact COVID-19 Disease Progression: An Observational Study on the First Wave. Metabolites, 11."
},
{
"DOI": "10.1111/cen.14276",
"article-title": "Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalized with COVID-19 are associated with greater disease severity",
"author": "Panagiotou",
"doi-asserted-by": "crossref",
"first-page": "508",
"journal-title": "Clin. Endocrinol.",
"key": "ref_6",
"volume": "93",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.08.018",
"article-title": "Nutritional status of patients with COVID-19",
"author": "Im",
"doi-asserted-by": "crossref",
"first-page": "390",
"journal-title": "Int. J. Infect. Dis.",
"key": "ref_7",
"volume": "100",
"year": "2020"
},
{
"DOI": "10.1093/jn/nxaa332",
"article-title": "Vitamin D Deficiency Is Associated with COVID-19 Incidence and Disease Severity in Chinese People",
"author": "Luo",
"doi-asserted-by": "crossref",
"first-page": "98",
"journal-title": "J. Nutr.",
"key": "ref_8",
"volume": "151",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.26848",
"article-title": "Effect of a Single High Dose of Vitamin D3 on Hospital Length of Stay in Patients With Moderate to Severe COVID-19: A Randomized Clinical Trial",
"author": "Murai",
"doi-asserted-by": "crossref",
"first-page": "1053",
"journal-title": "JAMA",
"key": "ref_9",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.3390/nu13061988",
"doi-asserted-by": "crossref",
"key": "ref_10",
"unstructured": "Herrera-Quintana, L., Gamarra-Morales, Y., Vázquez-Lorente, H., Molina-López, J., Castaño-Pérez, J., Machado-Casas, J.F., Coca-Zúñiga, R., Pérez-Villares, J.M., and Planells, E. (2021). Bad Prognosis in Critical Ill Patients with COVID-19 during Short-Term ICU Stay regarding Vitamin D Levels. Nutrients, 13."
},
{
"DOI": "10.1038/s41598-020-77093-z",
"article-title": "Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers",
"author": "Jain",
"doi-asserted-by": "crossref",
"first-page": "20191",
"journal-title": "Sci. Rep.",
"key": "ref_11",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1038/s41598-021-97017-9",
"article-title": "The relationship between serum 25-hydroxyvitamin D levels and the severity of COVID-19 disease and its mortality",
"author": "Vasheghani",
"doi-asserted-by": "crossref",
"first-page": "17594",
"journal-title": "Sci. Rep.",
"key": "ref_12",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1186/s13054-020-03051-w",
"article-title": "Systemic hypoferremia and severity of hypoxemic respiratory failure in COVID-19",
"author": "Shah",
"doi-asserted-by": "crossref",
"first-page": "320",
"journal-title": "Crit. Care",
"key": "ref_13",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1186/s13017-020-00323-2",
"article-title": "Iron metabolism and lymphocyte characterisation during COVID-19 infection in ICU patients: An observational cohort study",
"author": "Bolondi",
"doi-asserted-by": "crossref",
"first-page": "41",
"journal-title": "World J. Emerg. Surg.",
"key": "ref_14",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1097/HS9.0000000000000492",
"article-title": "ypoferremia is Associated With Increased Hospitalization and Oxygen Demand in COVID-19 Patients",
"author": "Hippchen",
"doi-asserted-by": "crossref",
"first-page": "e492",
"journal-title": "Hemasphere",
"key": "ref_15",
"volume": "4",
"year": "2020"
},
{
"DOI": "10.1093/ofid/ofaa250",
"article-title": "Serum Iron Level as a Potential Predictor of Coronavirus Disease 2019 Severity and Mortality: A Retrospective Study",
"author": "Zhao",
"doi-asserted-by": "crossref",
"first-page": "ofaa250",
"journal-title": "Open Forum. Infect. Dis.",
"key": "ref_16",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26895",
"article-title": "A pilot double-blind safety and feasibility randomized controlled trial of high-dose intravenous zinc in hospitalized COVID-19 patients",
"author": "Patel",
"doi-asserted-by": "crossref",
"first-page": "3261",
"journal-title": "J. Med. Virol.",
"key": "ref_17",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.3390/nu13062113",
"doi-asserted-by": "crossref",
"key": "ref_18",
"unstructured": "Notz, Q., Herrmann, J., Schlesinger, T., Helmer, P., Sudowe, S., Sun, Q., Hackler, J., Roeder, D., Lotz, C., and Meybohm, P. (2021). Clinical Significance of Micronutrient Supplementation in Critically Ill COVID-19 Patients with Severe ARDS. Nutrients, 13."
},
{
"DOI": "10.20944/preprints202007.0113.v1",
"doi-asserted-by": "crossref",
"key": "ref_19",
"unstructured": "Moghaddam, A., Heller, R.A., Sun, Q., Seelig, J., Cherkezov, A., Seibert, L., Hackler, J., Seemann, P., Diegmann, J., and Pilz, M. (2020). Selenium Deficiency Is Associated with Mortality Risk from COVID-19. Nutrients, 12."
},
{
"DOI": "10.3945/ajcn.111.023812",
"article-title": "Quantitative data on the magnitude of the systemic inflammatory response and its effect on micronutrient status based on plasma measurements",
"author": "Duncan",
"doi-asserted-by": "crossref",
"first-page": "64",
"journal-title": "Am. J. Clin. Nutr.",
"key": "ref_20",
"volume": "95",
"year": "2012"
},
{
"DOI": "10.1016/j.clnu.2022.02.015",
"article-title": "ESPEN micronutrient guideline",
"author": "Berger",
"doi-asserted-by": "crossref",
"first-page": "1357",
"journal-title": "Clin. Nutr.",
"key": "ref_21",
"volume": "41",
"year": "2022"
},
{
"DOI": "10.1515/cclm-2018-1096",
"article-title": "Reference values for 24,25-dihydroxyvitamin D and the 25-hydroxyvitamin D/24,25-dihydroxyvitamin D ratio",
"author": "Dirks",
"doi-asserted-by": "crossref",
"first-page": "e259",
"journal-title": "Clin. Chem. Lab. Med. (CCLM)",
"key": "ref_22",
"volume": "57",
"year": "2019"
},
{
"DOI": "10.1016/S0378-4347(00)81869-1",
"article-title": "Measurement of vitamin A and vitamin E in human serum by high-performance liquid chromatography",
"author": "Driskell",
"doi-asserted-by": "crossref",
"first-page": "439",
"journal-title": "J. Chromatogr.",
"key": "ref_23",
"volume": "231",
"year": "1982"
},
{
"DOI": "10.1016/S1570-0232(03)00320-9",
"article-title": "Optimisation and validation of a sensitive high-performance liquid chromatography assay for routine measurement of pyridoxal 5-phosphate in human plasma and red cells using pre-column semicarbazide derivatisation",
"author": "Talwar",
"doi-asserted-by": "crossref",
"first-page": "333",
"journal-title": "J. Chromatogr. B Analyt. Technol. Biomed. Life Sci.",
"key": "ref_24",
"volume": "792",
"year": "2003"
},
{
"key": "ref_25",
"unstructured": "Stichting-NICE (2020, November 19). Sequential Organ Failure Assessment (SOFA). Available online: https://www.stichting-nice.nl/download/?Groep=Data%20Dictionary&Taal=Engels."
},
{
"article-title": "Limitations of Serum Ferritin in Diagnosing Iron Deficiency in Inflammatory Conditions",
"author": "Dignass",
"first-page": "9394060",
"journal-title": "Int. J. Chronic. Dis.",
"key": "ref_26",
"volume": "2018",
"year": "2018"
},
{
"DOI": "10.1016/j.metabol.2020.154434",
"article-title": "Letter to the Editor: Vitamin D deficiency in COVID-19: Mixing up cause and consequence",
"author": "Smolders",
"doi-asserted-by": "crossref",
"first-page": "154434",
"journal-title": "Metabolism",
"key": "ref_27",
"volume": "115",
"year": "2021"
},
{
"DOI": "10.1093/advances/nmab012",
"article-title": "Association of Vitamin D Status with SARS-CoV-2 Infection or COVID-19 Severity: A Systematic Review and Meta-analysis",
"author": "Kazemi",
"doi-asserted-by": "crossref",
"first-page": "1636",
"journal-title": "Adv. Nutr.",
"key": "ref_28",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1210/clinem/dgac719",
"article-title": "Consensus and Controversial Aspects of Vitamin D and COVID-19",
"author": "Bilezikian",
"doi-asserted-by": "crossref",
"first-page": "1034",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "ref_29",
"volume": "108",
"year": "2023"
},
{
"DOI": "10.3390/nu13072173",
"doi-asserted-by": "crossref",
"key": "ref_30",
"unstructured": "Tepasse, P.R., Vollenberg, R., Fobker, M., Kabar, I., Schmidt, H., Meier, J.A., Nowacki, T., and Husing-Kabar, A. (2021). Vitamin A Plasma Levels in COVID-19 Patients: A Prospective Multicenter Study and Hypothesis. Nutrients, 13."
},
{
"DOI": "10.1007/s12011-021-02997-4",
"article-title": "COVID-19 and Selenium Deficiency: A Systematic Review",
"author": "Fakhrolmobasheri",
"doi-asserted-by": "crossref",
"first-page": "3945",
"journal-title": "Biol. Trace Elem. Res.",
"key": "ref_31",
"volume": "200",
"year": "2022"
},
{
"DOI": "10.1016/j.nut.2021.111400",
"article-title": "The association between serum levels of micronutrients and the severity of disease in patients with COVID-19",
"author": "Beigmohammadi",
"doi-asserted-by": "crossref",
"first-page": "111400",
"journal-title": "Nutrition",
"key": "ref_32",
"volume": "91–92",
"year": "2021"
},
{
"DOI": "10.1186/s13063-021-05795-4",
"article-title": "The effect of supplementation with vitamins A, B, C, D, and E on disease severity and inflammatory responses in patients with COVID-19: A randomized clinical trial",
"author": "Beigmohammadi",
"doi-asserted-by": "crossref",
"first-page": "802",
"journal-title": "Trials",
"key": "ref_33",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.0369",
"article-title": "Effect of High-Dose Zinc and Ascorbic Acid Supplementation vs Usual Care on Symptom Length and Reduction Among Ambulatory Patients With SARS-CoV-2 Infection: The COVID A to Z Randomized Clinical Trial",
"author": "Thomas",
"doi-asserted-by": "crossref",
"first-page": "e210369",
"journal-title": "JAMA Netw. Open",
"key": "ref_34",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1186/s13054-016-1529-5",
"article-title": "High-dose intravenous selenium does not improve clinical outcomes in the critically ill: A systematic review and meta-analysis",
"author": "Manzanares",
"doi-asserted-by": "crossref",
"first-page": "356",
"journal-title": "Crit. Care",
"key": "ref_35",
"volume": "20",
"year": "2016"
},
{
"DOI": "10.1016/j.clnesp.2020.11.026",
"article-title": "Daily parenteral selenium therapy in critically ill patients: An updated systematic review and meta-analysis of randomized controlled trials",
"author": "Mousavi",
"doi-asserted-by": "crossref",
"first-page": "49",
"journal-title": "Clin. Nutr. ESPEN",
"key": "ref_36",
"volume": "41",
"year": "2021"
},
{
"DOI": "10.3390/ph16010130",
"doi-asserted-by": "crossref",
"key": "ref_37",
"unstructured": "Argano, C., Mallaci Bocchio, R., Natoli, G., Scibetta, S., Lo Monaco, M., and Corrao, S. (2023). Protective Effect of Vitamin D Supplementation on COVID-19-Related Intensive Care Hospitalization and Mortality: Definitive Evidence from Meta-Analysis and Trial Sequential Analysis. Pharmaceuticals, 16."
},
{
"DOI": "10.1016/j.nut.2020.110989",
"article-title": "Pharmaconutrition revisited for critically ill patients with coronavirus disease 2019 (COVID-19): Does selenium have a place?",
"author": "Manzanares",
"doi-asserted-by": "crossref",
"first-page": "110989",
"journal-title": "Nutrition",
"key": "ref_38",
"volume": "81",
"year": "2021"
}
],
"reference-count": 38,
"references-count": 38,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2072-6643/16/3/385"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "Micronutrient Status of Critically Ill Patients with COVID-19 Pneumonia",
"type": "journal-article",
"volume": "16"
}
rozemeijer
