Bad Prognosis in Critical Ill Patients with COVID-19 during Short-Term ICU Stay regarding Vitamin D Levels
et al., Nutrients, doi:10.3390/nu13061988, Jun 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
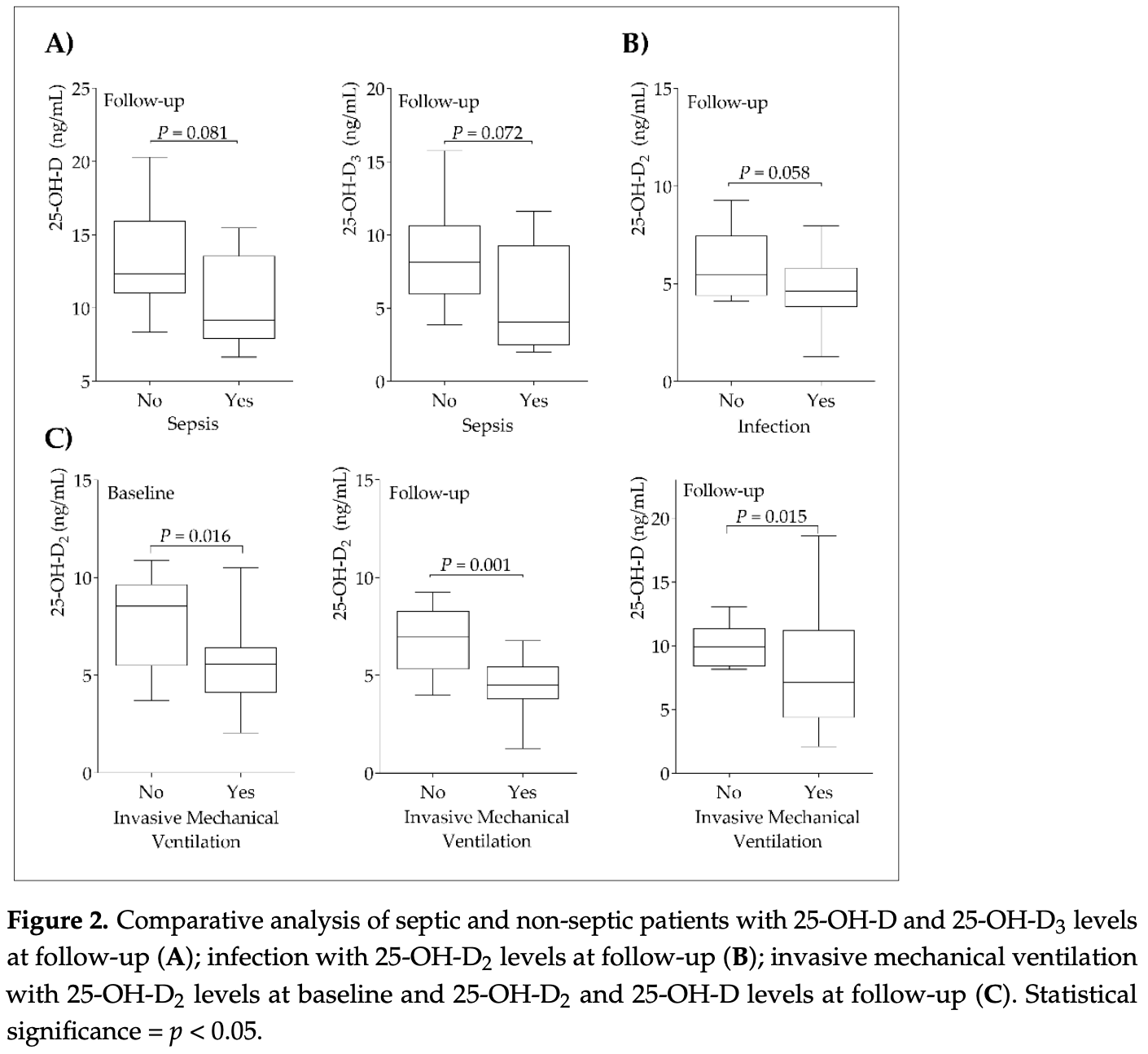
Prospective analysis of 37 critical COVID-19 patients, showing mechanical ventilation associated with lower vitamin D levels.
Herrera-Quintana et al., 9 Jun 2021, prospective, Spain, peer-reviewed, 9 authors, study period 1 March, 2020 - 1 June, 2020.
Contact: jorge.molina@ddi.uhu.es (corresponding author), lourdesherrera@ugr.es, jennifer_gamo@hotmail.com, hectorvazquez@ugr.es, jcastaoperez@yahoo.com, jmachc2@hotmail.com, ramon.coca.sspa@juntadeandalucia.es, josem.perez.villares.sspa@juntadeandalucia.es, elenamp@ugr.es.
Bad Prognosis in Critical Ill Patients with COVID-19 during Short-Term ICU Stay regarding Vitamin D Levels
Nutrients, doi:10.3390/nu13061988
Background and aims: Vitamin D inadequacy may be involved in the mechanisms of SARS-CoV-2 infection and in potential risk factors for disease propagation or control of coronavirus disease 2019 (COVID-19). This study assessed a short-term evolution of vitamin D status and its influence upon different clinical parameters in critically ill patients with COVID-19. Methods: A prospective analytical study in which 37 critically ill volunteers between 41 and 71 years of age with COVID-19 were evaluated at baseline and three days of intensive care unit (ICU) stay. 25-OH-D 3 and 25-OH-D 2 were analyzed by liquid chromatography-tandem mass spectrometry and total 25-OH-D levels were calculated as the sum of both. Results: All patients presented low 25-OH-D levels at baseline, decreasing total 25-OH-D (p = 0.011) mainly through 25-OH-D 2 (p = 0.006) levels during ICU stay. 25-OH-D 2 levels decreased a mean of 41.6% ± 89.6% versus 7.0% ± 23.4% for the 25-OH-D 3 form during the ICU stay. Patients who did not need invasive mechanical ventilation presented higher levels of 25-OH-D 2 at baseline and follow-up. Lower 25-OH-D and 25-OH-D 3 levels were associated with higher D-dimer at baseline (p = 0.003; p = 0.001) and at follow up (p = 0.029), higher procalcitonin levels (p = 0.002; p = 0.018) at follow up, and lower percentage lymphocyte counts (p = 0.044; p = 0.040) during ICU stay. Conclusions: Deficient vitamin D status in critical patients was established at the admission and further worsened after three days of stay. Lower vitamin D levels were related to key altered clinical and biochemical parameters on patients with SARS-CoV-2 infection. Given the different response of the 25-OH-D 3 and 25-OH-D 2 forms, it would be useful to monitor them on the evolution of the critically ill patient.
Conflicts of Interest: The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
Abilés, Aguayo, Moreno-Torres, Llopis, Aranda et al., Oxidative Stress Is Increased in Critically Ill Patients According to Antioxidant Vitamins Intake, Independent of Severity: A Cohort Study, Crit. Care, doi:10.1186/cc5068
Alexander, Tinkov, Strand, Alehagen, Skalny et al., Early Nutritional Interventions with Zinc, Selenium and Vitamin D for Raising Anti-Viral Resistance Against Progressive COVID-19, Nutrients, doi:10.3390/nu12082358
Ali, Role of Vitamin D in Preventing of COVID-19 Infection, Progression and Severity, J. Infect. Public Health, doi:10.1016/j.jiph.2020.06.021
Amrein, Zajic, Schnedl, Waltensdorfer, Fruhwald et al., Vitamin D Status and Its Association with Season, Hospital and Sepsis Mortality in Critical Illness, Crit. Care, doi:10.1186/cc13790
Annweiler, Hanotte, Grandin De L'eprevier, Sabatier, Lafaie et al., Vitamin D and Survival in COVID-19 Patients: A Quasi-Experimental Study, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2020.105771
Aygun, Vitamin D Can Prevent COVID-19 Infection-Induced Multiple Organ Damage, Naunyn. Schmiedebergs Arch. Pharmacol, doi:10.1007/s00210-020-01911-4
Barazzoni, Bischoff, Breda, Wickramasinghe, Krznaric et al., ESPEN Expert Statements and Practical Guidance for Nutritional Management of Individuals with SARS-CoV-2 Infection, Clin. Nutr, doi:10.1016/j.clnu.2020.03.022
Benskin, A Basic Review of the Preliminary Evidence That COVID-19 Risk and Severity Is Increased in Vitamin D Deficiency, Front. Public Health, doi:10.3389/fpubh.2020.00513
Berger, Reintam-Blaser, Calder, Casaer, Hiesmayr et al., Monitoring Nutrition in the ICU, Clin. Nutr, doi:10.1016/j.clnu.2018.07.009
Bigman, Vitamin D Metabolites, D3 and D2, and Their Independent Associations with Depression Symptoms among Adults in the United States, Nutr. Neurosci, doi:10.1080/1028415X.2020.1794422
Bilezikian, Bikle, Hewison, Lazaretti-Castro, Formenti et al., Mechanisms in endocrinology: Vitamin D and COVID-19, Eur. J. Endocrinol, doi:10.1530/EJE-20-0665
Buetti, Ruckly, De Montmollin, Reignier, Terzi et al., COVID-19 Increased the Risk of ICU-Acquired Bloodstream Infections: A Case-Cohort Study from the Multicentric OUTCOMEREA Network, Intensive Care Med, doi:10.1007/s00134-021-06346-w
Caccialanza, Laviano, Lobascio, Montagna, Bruno et al., Early Nutritional Supplementation in Non-Critically Ill Patients Hospitalized for the 2019 Novel Coronavirus Disease (COVID-19): Rationale and Feasibility of a Shared Pragmatic Protocol, Nutrition, doi:10.1016/j.nut.2020.110835
Cannell, Vieth, Umhau, Holick, Grant et al., Epidemic Influenza and Vitamin D, Epidemiol. Infect, doi:10.1017/S0950268806007175
Carpagnano, Di Lecce, Quaranta, Zito, Buonamico et al., Vitamin D Deficiency as a Predictor of Poor Prognosis in Patients with Acute Respiratory Failure Due to COVID-19, J. Endocrinol. Investig, doi:10.1007/s40618-020-01370-x
Castillo, Entrenas Costa, Vaquero Barrios, Alcalá Díaz, Miranda et al., Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2020.105751
Cereda, Bogliolo, Klersy, Lobascio, Masi et al., Vitamin D 25OH Deficiency in COVID-19 Patients Admitted to a Tertiary Referral Hospital, Clin. Nutr, doi:10.1016/j.clnu.2020.10.055
Chiappetta, Sharma, Bottino, Stier, COVID-19 and the Role of Chronic Inflammation in Patients with Obesity, Int. J. Obes, doi:10.1038/s41366-020-0597-4
Christopher, Vitamin D and Critical Illness Outcomes, Curr. Opin. Crit. Care, doi:10.1097/MCC.0000000000000328
Cohen, A Power Primer, Psychol. Bull, doi:10.1037/0033-2909.112.1.155
Daneshkhah, Agrawal, Eshein, Subramanian, Roy et al., Evidence for possible association of vitamin D status with cytokine storm and unregulated inflammation in COVID-19 patients, Aging Clin. Exp. Res, doi:10.1007/s40520-020-01677-y
De Las Heras, Martín Giménez, Ferder, Manucha, Lahera, Implications of Oxidative Stress and Potential Role of Mitochondrial Dysfunction in COVID-19: Therapeutic Effects of Vitamin D, Antioxidants, doi:10.3390/antiox9090897
Ebadi, Montano-Loza, Perspective: Improving Vitamin D Status in the Management of COVID-19, Eur. J. Clin. Nutr, doi:10.1038/s41430-020-0661-0
Feng, Li, Sun, Zhu, Chen et al., Immune-Inflammatory Parameters in COVID-19 Cases: A Systematic Review and Meta-Analysis, Front. Med, doi:10.3389/fmed.2020.00301
Gamarra, Santiago, Molina-López, Castaño, Herrera-Quintana et al., Pyroglutamic Acidosis by Glutathione Regeneration Blockage in Critical Patients with Septic Shock, Crit. Care, doi:10.1186/s13054-019-2450-5
Gottschlich, Mayes, Khoury, Kagan, Clinical Trial of Vitamin D 2 vs. D 3 Supplementation in Critically Ill Pediatric Burn Patients, J. Parenter. Enter. Nutr, doi:10.1177/0148607115587948
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence That Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients, doi:10.3390/nu12040988
Han, Ma, Li, Liu, Zhao et al., Profiling Serum Cytokines in COVID-19 Patients Reveals IL-6 and IL-10 Are Disease Severity Predictors, Emerg. Microbes Infect, doi:10.1080/22221751.2020.1770129
Heijboer, Blankenstein, Kema, Buijs, Accuracy of 6 Routine 25-Hydroxyvitamin D Assays: Influence of Vitamin D Binding Protein Concentration, Clin. Chem, doi:10.1373/clinchem.2011.176545
Higashi, Shimada, Toyo'oka, Advances in Determination of Vitamin D Related Compounds in Biological Samples Using Liquid Chromatography-Mass Spectrometry: A Review, J. Chromatogr. B, doi:10.1016/j.jchromb.2009.11.026
Holick, Binkley, Bischoff-Ferrari, Gordon, Hanley et al., Treatment, and Prevention of Vitamin D Deficiency: An Endocrine Society Clinical Practice Guideline, J. Clin. Endocrinol. Metab, doi:10.1210/jc.2011-0385
Holick, The D-Sparaging of Vitamin D2: How Physiologically and Pharmacologically Relevant Is It for the Clinician?, J. Clin. Endocrinol. Metab, doi:10.1210/clinem/dgz290
Holick, The Vitamin D Deficiency Pandemic: Approaches for Diagnosis, Treatment and Prevention, Rev. Endocr. Metab. Disord, doi:10.1007/s11154-017-9424-1
Houghton, Vieth, The Case against Ergocalciferol (Vitamin D2) as a Vitamin Supplement, Am. J. Clin. Nutr, doi:10.1093/ajcn/84.4.694
Ilie, Stefanescu, Smith, The Role of Vitamin D in the Prevention of Coronavirus Disease 2019 Infection and Mortality, Aging Clin. Exp. Res, doi:10.1007/s40520-020-01570-8
Infante, Buoso, Pieri, Lupisella, Nuccetelli et al., Low Vitamin D Status at Admission as a Risk Factor for Poor Survival in Hospitalized Patients with COVID-19: An Italian Retrospective Study, J. Am. Coll. Nutr, doi:10.1080/07315724.2021.1877580
Kaufman, Niles, Kroll, Bi, Holick, SARS-CoV-2 Positivity Rates Associated with Circulating 25-Hydroxyvitamin D Levels, PLoS ONE, doi:10.1371/journal.pone.0239252
Laviano, Koverech, Zanetti, Nutrition Support in the Time of SARS-CoV-2 (COVID-19), Nutrition, doi:10.1016/j.nut.2020.110834
Lips, Cashman, Lamberg-Allardt, Bischoff-Ferrari, Obermayer-Pietsch et al., Current vitamin D status in European and Middle East coun-tries and strategies to prevent vitamin D deficiency: A position statement of the European Calcified Tissue Society, Eur. J. Endocrinol, doi:10.1530/EJE-18-0736
Maghbooli, Sahraian, Ebrahimi, Pazoki, Kafan et al., Vitamin D Sufficiency, a Serum 25-Hydroxyvitamin D at Least 30 Ng/ML Reduced Risk for Adverse Clinical Outcomes in Patients with COVID-19 Infection, PLoS ONE, doi:10.1371/journal.pone.0239799
Mansur, Tajer, Mariani, Inserra, Ferder et al., Vitamin D high doses supplementation could represent a promising alternative to prevent or treat COVID-19 infection, Clín. Investig. Arterioscler, doi:10.1016/j.arteri.2020.05.003
Martín Giménez, Inserra, Tajer, Mariani, Ferder et al., Lungs as Target of COVID-19 Infection: Protective Common Molecular Mechanisms of Vitamin D and Melatonin as a New Potential Synergistic Treatment, Life Sci, doi:10.1016/j.lfs.2020.117808
Meltzer, Best, Zhang, Vokes, Arora et al., Association of Vitamin D Status and Other Clinical Characteristics With COVID-19 Test Results, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2020.19722
Parikh, Guo, Pollock, Petty, Bhagatwala et al., Circulating 25-Hydroxyvitamin D Concentrations Are Correlated with Cardiometabolic Risk Among American Black and White Adolescents Living in a Year-Round Sunny Climate, Diabetes Care, doi:10.2337/dc11-1944
Patel, Martindale, Mcclave, Relevant Nutrition Therapy in COVID-19 and the Constraints on Its Delivery by a Unique Disease Process, Nutr. Clin. Pract, doi:10.1002/ncp.10566
Ponti, Maccaferri, Ruini, Tomasi, Ozben, Biomarkers associated with COVID-19 disease progression, Crit. Rev. Clin. Lab. Sci, doi:10.1080/10408363.2020.1770685
Rapp, Lieberman-Cribbin, Tuminello, Taioli, Male, Sex, Severe Obesity, Older Age, and Chronic Kidney Disease Are Associated With COVID-19 Severity and Mortality in New York City, Chest, doi:10.1016/j.chest.2020.08.2065
Rousseau, Damas, Janssens, Kalin, Ledoux et al., Critical Care and Vitamin D Status Assessment: What about Immunoassays and Calculated Free 25OH-D?, Clin. Chim. Acta, doi:10.1016/j.cca.2014.07.007
Saghir Afifeh, Verdoia, Nardin, Negro, Viglione et al., Determinants of Vitamin D Activation in Patients with Acute Coronary Syndromes and Its Correlation with Inflammatory Markers, Nutr. Metab. Cardiovasc. Dis, doi:10.1016/j.numecd.2020.09.021
Swanson, Nielson, Shrestha, Lee, Barrett-Connor et al., Higher 25(OH)D2 Is Associated with Lower 25(OH)D3 and 1,25(OH)2D3, J. Clin. Endocrinol. Metab, doi:10.1210/jc.2014-1069
Tahsin-Swafiri, Blanco-Navarro, Pérez-Sacristán, Millán, Granado-Lorencio, The Prevalence of Vitamin Deficiency in Clinical Practice Is Assay-Dependent, Clin. Nutr, doi:10.1016/j.clnu.2012.04.009
Terpos, Ntanasis-Stathopoulos, Elalamy, Kastritis, Sergentanis et al., Hematological Findings and Complications of COVID -19, Am. J. Hematol, doi:10.1002/ajh.25829
Teymoori-Rad, Marashi, Vitamin D and Covid-19: From Potential Therapeutic Effects to Unanswered Questions, Rev. Med. Virol, doi:10.1002/rmv.2159
Van Den Ouweland, Analysis of Vitamin D Metabolites by Liquid Chromatography-Tandem Mass Spectrometry, TrAC Trends Anal. Chem, doi:10.1016/j.trac.2016.02.005
Vassiliou, Jahaj, Pratikaki, Orfanos, Dimopoulou et al., Low 25-Hydroxyvitamin D Levels on Admission to the Intensive Care Unit May Predispose COVID-19 Pneumonia Patients to a Higher 28-Day Mortality Risk: A Pilot Study on a Greek ICU Cohort, Nutrients, doi:10.3390/nu12123773
Vázquez-Lorente, Herrera-Quintana, Molina-López, Gamarra-Morales, López-González et al., Response of Vitamin D after Magnesium Intervention in a Postmenopausal Population from the Province of Granada, Spain, Nutrients, doi:10.3390/nu12082283
Vázquez-Lorente, Herrera-Quintana, Quintero-Osso, Molina-López, Planells, Current Trends in the Analytical Determination of Vitamin D, Nutr. Hosp
Waldron, Ashby, Cornes, Bechervaise, Razavi et al., A Negative Acute Phase Reactant, J. Clin. Pathol, doi:10.1136/jclinpath-2012-201301
Wang, Liu, Hou, Wei, Liu et al., Serum Vitamin D Affected Type 2 Diabetes Though Altering Lipid Profile and Modified the Effects of Testosterone on Diabetes Status, Nutrients
Weir, Thenappan, Bhargava, Chen, Does Vitamin D Deficiency Increase the Severity of COVID-19?, Clin. Med, doi:10.7861/clinmed.2020-0301
Xu, Baylink, Chen, Reeves, Xiao et al., The Importance of Vitamin d Metabolism as a Potential Prophylactic, Immunoregulatory and Neuroprotective Treatment for COVID-19, J. Transl. Med, doi:10.1186/s12967-020-02488-5
Zabetakis, Lordan, Norton, Tsoupras, COVID-19: The Inflammation Link and the Role of Nutrition in Potential Mitigation, Nutrients, doi:10.3390/nu12051466
Zhao, Li, Ge, Shi, Lv et al., Evaluation of Nutrition Risk and Its Association with Mortality Risk in Severely and Critically Ill COVID-19 Patients, J. Parenter. Enter. Nutr, doi:10.1002/jpen.1953
Zhao, Yan, Qu, Interpretations of "Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia (Trial Version 7), Chin. Med. J, doi:10.1097/CM9.0000000000000866
DOI record:
{
"DOI": "10.3390/nu13061988",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu13061988",
"abstract": "<jats:p>Background and aims: Vitamin D inadequacy may be involved in the mechanisms of SARS-CoV-2 infection and in potential risk factors for disease propagation or control of coronavirus disease 2019 (COVID-19). This study assessed a short-term evolution of vitamin D status and its influence upon different clinical parameters in critically ill patients with COVID-19. Methods: A prospective analytical study in which 37 critically ill volunteers between 41 and 71 years of age with COVID-19 were evaluated at baseline and three days of intensive care unit (ICU) stay. 25-OH-D3 and 25-OH-D2 were analyzed by liquid chromatography–tandem mass spectrometry and total 25-OH-D levels were calculated as the sum of both. Results: All patients presented low 25-OH-D levels at baseline, decreasing total 25-OH-D (p = 0.011) mainly through 25-OH-D2 (p = 0.006) levels during ICU stay. 25-OH-D2 levels decreased a mean of 41.6% ± 89.6% versus 7.0% ± 23.4% for the 25-OH-D3 form during the ICU stay. Patients who did not need invasive mechanical ventilation presented higher levels of 25-OH-D2 at baseline and follow-up. Lower 25-OH-D and 25-OH-D3 levels were associated with higher D-dimer at baseline (p = 0.003; p = 0.001) and at follow up (p = 0.029), higher procalcitonin levels (p = 0.002; p = 0.018) at follow up, and lower percentage lymphocyte counts (p = 0.044; p = 0.040) during ICU stay. Conclusions: Deficient vitamin D status in critical patients was established at the admission and further worsened after three days of stay. Lower vitamin D levels were related to key altered clinical and biochemical parameters on patients with SARS-CoV-2 infection. Given the different response of the 25-OH-D3 and 25-OH-D2 forms, it would be useful to monitor them on the evolution of the critically ill patient.</jats:p>",
"alternative-id": [
"nu13061988"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-1407-322X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Herrera-Quintana",
"given": "Lourdes",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0003-0921-2168",
"affiliation": [],
"authenticated-orcid": false,
"family": "Gamarra-Morales",
"given": "Yenifer",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0183-6902",
"affiliation": [],
"authenticated-orcid": false,
"family": "Vázquez-Lorente",
"given": "Héctor",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2516-5226",
"affiliation": [],
"authenticated-orcid": false,
"family": "Molina-López",
"given": "Jorge",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Castaño-Pérez",
"given": "José",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7852-6553",
"affiliation": [],
"authenticated-orcid": false,
"family": "Machado-Casas",
"given": "Juan Francisco",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5014-5644",
"affiliation": [],
"authenticated-orcid": false,
"family": "Coca-Zúñiga",
"given": "Ramón",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pérez-Villares",
"given": "José Miguel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Planells",
"given": "Elena",
"sequence": "additional"
}
],
"container-title": "Nutrients",
"container-title-short": "Nutrients",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
6,
9
]
],
"date-time": "2021-06-09T18:16:04Z",
"timestamp": 1623262564000
},
"deposited": {
"date-parts": [
[
2021,
6,
16
]
],
"date-time": "2021-06-16T01:33:37Z",
"timestamp": 1623807217000
},
"indexed": {
"date-parts": [
[
2022,
11,
7
]
],
"date-time": "2022-11-07T08:30:03Z",
"timestamp": 1667809803127
},
"is-referenced-by-count": 5,
"issue": "6",
"issued": {
"date-parts": [
[
2021,
6,
9
]
]
},
"journal-issue": {
"issue": "6",
"published-online": {
"date-parts": [
[
2021,
6
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
6,
9
]
],
"date-time": "2021-06-09T00:00:00Z",
"timestamp": 1623196800000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/13/6/1988/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1988",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2021,
6,
9
]
]
},
"published-online": {
"date-parts": [
[
2021,
6,
9
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1016/j.jiph.2020.06.021",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.3390/antiox9090897",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1080/22221751.2020.1770129",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1007/s00210-020-01911-4",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1186/cc5068",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1186/s13054-019-2450-5",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1002/jpen.1953",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1016/j.nut.2020.110834",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.1016/j.clnu.2020.03.022",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.3390/nu12051466",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1016/j.nut.2020.110835",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1002/ncp.10566",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.3390/nu12082358",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.1016/j.trac.2016.02.005",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1016/j.jchromb.2009.11.026",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1177/0148607115587948",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.3390/nu12040988",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1016/j.lfs.2020.117808",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1016/j.arteri.2020.05.003",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.7861/clinmed.2020-0301",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1136/jclinpath-2012-201301",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1373/clinchem.2011.176545",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1002/rmv.2159",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1530/EJE-20-0665",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1186/s12967-020-02488-5",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1007/s40618-020-01370-x",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1210/jc.2011-0385",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1097/CM9.0000000000000866",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1037/0033-2909.112.1.155",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1016/j.chest.2020.08.2065",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.1038/s41366-020-0597-4",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1080/10408363.2020.1770685",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.1097/MCC.0000000000000328",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1186/cc13790",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1007/s11154-017-9424-1",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.1371/journal.pone.0239252",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.3389/fpubh.2020.00513",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.1007/s40520-020-01570-8",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.1007/s40520-020-01677-y",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.1530/EJE-18-0736",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.1371/journal.pone.0239799",
"doi-asserted-by": "publisher",
"key": "ref42"
},
{
"DOI": "10.1016/j.clnu.2020.10.055",
"doi-asserted-by": "publisher",
"key": "ref43"
},
{
"DOI": "10.3390/nu12123773",
"doi-asserted-by": "publisher",
"key": "ref44"
},
{
"DOI": "10.3390/nu12082283",
"doi-asserted-by": "publisher",
"key": "ref45"
},
{
"DOI": "10.1210/jc.2014-1069",
"doi-asserted-by": "publisher",
"key": "ref46"
},
{
"DOI": "10.3390/nu13010090",
"doi-asserted-by": "publisher",
"key": "ref47"
},
{
"DOI": "10.1017/S0950268806007175",
"doi-asserted-by": "publisher",
"key": "ref48"
},
{
"DOI": "10.1007/s00134-021-06346-w",
"doi-asserted-by": "publisher",
"key": "ref49"
},
{
"DOI": "10.1080/07315724.2021.1877580",
"doi-asserted-by": "publisher",
"key": "ref50"
},
{
"DOI": "10.1093/ajcn/84.4.694",
"doi-asserted-by": "publisher",
"key": "ref51"
},
{
"DOI": "10.1210/clinem/dgz290",
"doi-asserted-by": "publisher",
"key": "ref52"
},
{
"DOI": "10.1080/1028415X.2020.1794422",
"doi-asserted-by": "publisher",
"key": "ref53"
},
{
"DOI": "10.3389/fmed.2020.00301",
"doi-asserted-by": "publisher",
"key": "ref54"
},
{
"DOI": "10.1002/ajh.25829",
"doi-asserted-by": "publisher",
"key": "ref55"
},
{
"DOI": "10.2337/dc11-1944",
"doi-asserted-by": "publisher",
"key": "ref56"
},
{
"DOI": "10.1016/j.numecd.2020.09.021",
"doi-asserted-by": "publisher",
"key": "ref57"
},
{
"DOI": "10.1016/j.clnu.2018.07.009",
"doi-asserted-by": "publisher",
"key": "ref58"
},
{
"article-title": "Current Trends in the Analytical Determination of Vitamin D",
"author": "Vázquez-Lorente",
"first-page": "1418",
"journal-title": "Nutr. Hosp.",
"key": "ref59",
"volume": "36",
"year": "2019"
},
{
"DOI": "10.1016/j.clnu.2012.04.009",
"doi-asserted-by": "publisher",
"key": "ref60"
},
{
"DOI": "10.1016/j.cca.2014.07.007",
"doi-asserted-by": "publisher",
"key": "ref61"
},
{
"DOI": "10.1016/j.jsbmb.2020.105771",
"doi-asserted-by": "publisher",
"key": "ref62"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"doi-asserted-by": "publisher",
"key": "ref63"
},
{
"DOI": "10.1038/s41430-020-0661-0",
"doi-asserted-by": "publisher",
"key": "ref64"
}
],
"reference-count": 64,
"references-count": 64,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2072-6643/13/6/1988"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "Bad Prognosis in Critical Ill Patients with COVID-19 during Short-Term ICU Stay regarding Vitamin D Levels",
"type": "journal-article",
"volume": "13"
}
