Association of physical activity and the risk of COVID-19 hospitalization: a dose-response meta-analysis
et al., medRxiv, doi:10.1101/2022.06.22.22276789, Jun 2022
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
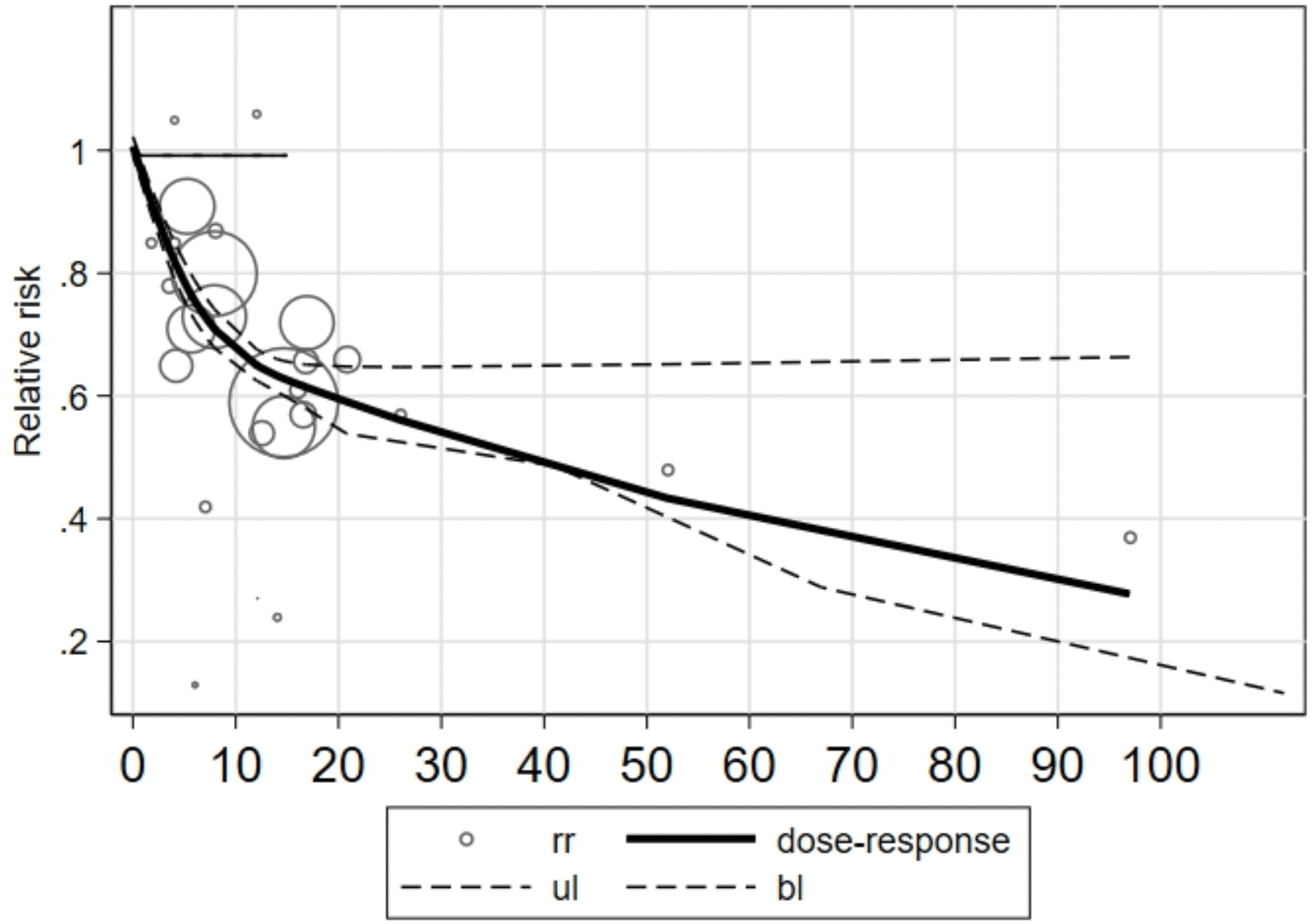
Meta analysis of 17 studies, showing a dose-response relationship with higher levels of physical activity reducing risk of COVID-19 hospitalization.
6 meta-analyses show significant improvements with exercise for mortality1-5,
ICU admission1,
hospitalization1,2,5,6 ,
severity2-4, and
cases2.
Currently there are 68 exercise for COVID-19 studies, showing 48% lower mortality [38‑57%], 46% lower ventilation [32‑57%], 41% lower ICU admission [35‑47%], 33% lower hospitalization [25‑40%], and 23% fewer cases [14‑31%].
|
risk of hospitalization, 40.0% lower, RR 0.60, p < 0.001.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Rahmati et al., Baseline physical activity is associated with reduced mortality and disease outcomes in COVID-19: A systematic review and meta-analysis, Reviews in Medical Virology, doi:10.1002/rmv.2349.
2.
Ezzatvar et al., Physical activity and risk of infection, severity and mortality of COVID-19: a systematic review and non-linear dose–response meta-analysis of data from 1 853 610 adults, British Journal of Sports Medicine, doi:10.1136/bjsports-2022-105733.
3.
Sittichai et al., Effects of physical activity on the severity of illness and mortality in COVID-19 patients: A systematic review and meta-analysis, Frontiers in Physiology, doi:10.3389/fphys.2022.1030568.
4.
Liu et al., Baseline physical activity and the risk of severe illness and mortality from COVID-19: A dose–response meta-analysis, Preventive Medicine Reports, doi:10.1016/j.pmedr.2023.102130.
Li et al., 23 Jun 2022, preprint, 3 authors.
Contact: lidanscerlett@126.com, whtyjinsz@163.com, songtaozhenzhenl@sina.com.
Association of physical activity and the risk of COVID-19 hospitalization: a dose–response meta-analysis
doi:10.1101/2022.06.22.22276789
Background Many people have experienced a high burden due to the spread of the coronavirus disease (COVID-19) and its serious consequences for health and everyday life. Prior studies have reported that physical activity (PA) may lower the risk of COVID-19 hospitalization. The present meta-analysis (PROSPERO registration number: CRD42022339672) explored the doseresponse relationship between PA and the risk of COVID-19 hospitalization.
Methods Epidemiological observational studies on the relationship between PA and the risk of COVID-19 hospitalization were included. Categorical dose-response relationships between PA and the risk of COVID-19 hospitalization were assessed using random effect models. Robust error meta-regression models assessed the continuous relationship between PA (metabolic equivalent [MET]-h/week) and COVID-19 hospitalization risk across studies reporting quantitative PA estimates.
Results Seventeen observational studies (cohort\case-control\cross-section) met the criteria for inclusion in the meta-analysis. Categorical dose-relationship analysis showed a 40% (risk ratio (RR) 0.60, 95% confidence intervals (CI): 0.48-0.71) reduction in the risk of COVID-19 hospitalization compared to the lowest dose of PA. The results of the continuous dose-response . NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice.
/ 14 relationship showed a non-linear inverse relationship (Pnon-linearity < 0.05) between PA and the risk of COVID-19 hospitalization. When total PA was less than or greater than 10 Met-h/week, an increase of 4 Met-h/week was associated with a 14% (RR = 0.83, 95%CI: 0.85-0.87) and 11% (RR = 0.89, 95%CI: 0.87-0.90) reduction in the risk of COVID-19 hospitalization, respectively.
Conclusions There was an inverse non-linear dose-response relationship between PA level and the risk of COVID-19 hospitalization. Doses of the guideline-recommended minimum PA levels by WTO may be required for more substantial reductions in the COVID-19 hospitalization risk.
Author Contributions
References
Ainsworth, Haskell, Herrmann, Meckes, Bassett et al., Compendium of Physical Activities: a second update of codes and MET values. Medicine and science in sports and exercise, doi:10.1249/MSS.0b013e31821ece12
Alketbi, Nagelkerke, Abdelbaqi, Al, Alsaedi et al., Risk Factors for SARS-CoV-2 Infection Severity in Abu Dhabi, Journal of epidemiology and global health, doi:10.1007/s44197-021-00006-4
Baik, Curhan, Rimm, Bendich, Willett et al., A prospective study of age and lifestyle factors in relation to community-acquired pneumonia in US men and women, Arch Intern Med, doi:10.1001/archinte.160.20.3082
Bielik, Grendar, Kolisek, A Possible Preventive Role of Physically Active Lifestyle during the SARS-CoV-2 Pandemic; Might Regular Cold-Water Swimming and Exercise Reduce the Symptom Severity of COVID-19?, Int J Environ Res Public Health, doi:10.3390/ijerph18137158
Brandenburg, Lesser, Thomson, Giles, Does Higher Self-Reported Cardiorespiratory Fitness Reduce the Odds of Hospitalization From COVID-19?, J Phys Act Health, doi:10.1123/jpah.2020-0817
Brawner, Ehrman, Bole, Kerrigan, Parikh et al., Inverse Relationship of Maximal Exercise Capacity to Hospitalization Secondary to Coronavirus Disease 2019, Mayo Clin Proc, doi:10.1016/j.mayocp.2020.10.003
Chastin, Abaraogu, Bourgois, Dall, Darnborough et al., Effects of Regular Physical Activity on the Immune System, Vaccination and Risk of Community-Acquired Infectious Disease in the General Population: Systematic Review and Meta-Analysis, Sports medicine, doi:10.1007/s40279-021-01466-1
Chen, Qi, Liu, Ling, Qian et al., Clinical progression of patients with COVID-19 in Shanghai, China. The, Journal of infection, doi:10.1016/j.jinf.2020.03.004
Collaborators, Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study, Lancet, doi:10.1016/s0140-6736(20)30752-2
Colpani, Baena, Jaspers, Van Dijk, Farajzadegan et al., Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: a systematic review and meta-analysis, Eur J Epidemiol, doi:10.1007/s10654-018-0374-z
De Souza, Motta-Santos, Santos Soares, De Lima, Cardozo et al., Association of physical activity levels and the prevalence of COVID-19-associated hospitalization, Journal of science and medicine in sport, doi:10.1016/j.jsams.2021.05.011
Duggal, Niemiro, Harridge, Simpson, Lord, Can physical activity ameliorate immunosenescence and thereby reduce age-related multi-morbidity?, Nature reviews Immunology, doi:10.1038/s41577-019-0177-9
Ekblom-Bak, Vaisanen, Ekblom, Blom, Kallings et al., Cardiorespiratory fitness and lifestyle on severe COVID-19 risk in 279,455 adults: a case control study. The international journal of behavioral nutrition and physical activity, doi:10.1186/s12966-021-01198-5
Halabchi, Mazaheri, Sabeti, Yunesian, Alizadeh et al., Regular Sports Participation as a Potential Predictor of Better Clinical Outcome in Adult Patients With COVID-19: A Large Cross-Sectional Study, J Phys Act Health, doi:10.1123/jpah.2020-0392
Hamdan, Badrasawi, Zidan, Sayarah, Zahra et al., Risk factors associated with hospitalization owing to COVID-19: a cross-sectional study in Palestine, The Journal of international medical research, doi:10.1177/03000605211064405
Hamer, Kivimaki, Gale, Batty, Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK. Brain, behavior, and immunity, doi:10.1016/j.bbi.2020.05.059
Higgins, Thompson, Quantifying heterogeneity in a meta-analysis, Statistics in medicine, doi:10.1002/sim.1186
Inoue, Koizumi, Wada, Iso, Watanabe et al., Risk and protective factors related to mortality from pneumonia among middleaged and elderly community residents: the JACC Study, J Epidemiol, doi:10.2188/jea.17.194
Katsoulis, Pasea, Lai, Dobson, Denaxas et al., Obesity during the COVID-19 pandemic: both cause of high risk and potential effect of lockdown? A population-based electronic health record study, Public health, doi:10.1016/j.puhe.2020.12.003
Latorre-Roman, Guzman-Guzman, Delgado-Floody, Sanchez, Aragon-Vela et al., Protective role of physical activity patterns prior to COVID-19 confinement with the severity/duration of respiratory pathologies consistent with COVID-19 symptoms in Spanish populations, Research in sports medicine, doi:10.1080/15438627.2021.1937166
Lee, Lee, Moon, Jin, Yang et al., Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study, Br J Sports Med, doi:10.1136/bjsports-2021-104203
Malisoux, Backes, Fischer, Aguayo, Ollert et al., Associations between physical activity prior to infection and COVID-19 disease severity and symptoms: results from the prospective Predi-COVID cohort study, BMJ open, doi:10.1136/bmjopen-2021-057863
Maltagliati, Sieber, Sarrazin, Cullati, Chalabaev et al., Muscle Strength Explains the Protective Effect of Physical Activity against COVID-19 Hospitalization among Adults aged 50 Years and Older, journal of sports medicile medRxiv, doi:10.1101/2021.02.25.21252451
Nieman, Wentz, The compelling link between physical activity and the body's defense system, J Sport Health Sci, doi:10.1016/j.jshs.2018.09.009
Rahmati, Shamsi, Khoramipour, Malakoutinia, Woo et al., Baseline physical activity is associated with reduced mortality and disease outcomes in COVID-19: A systematic review and meta-analysis, Reviews in medical virology, doi:10.1002/rmv.2349
Sallis, Young, Tartof, Sallis, Sall et al., Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients, Br J Sports Med, doi:10.1136/bjsports-2021-104080
Schlesinger, Neuenschwander, Ballon, Nothlings, Barbaresko, Adherence to healthy lifestyles and incidence of diabetes and mortality among individuals with diabetes: a systematic review and meta-analysis of prospective studies, Journal of epidemiology and community health, doi:10.1136/jech-2019-213415
Shephard, Shek, Potential impact of physical activity and sport on the immune system--a brief review, British journal of sports medicine, doi:10.1136/bjsm.28.4.247
Simpson, Kunz, Agha, Graff, Exercise and the Regulation of Immune Functions, Progress, doi:10.1016/bs.pmbts.2015.08.001
Stamatakis, Ding, Ekelund, Bauman, Sliding down the risk factor rankings: reasons for and consequences of the dramatic downgrading of physical activity in the Global Burden of Disease 2019, British journal of sports medicine, doi:10.1136/bjsports-2021-104064
Steenkamp, Saggers, Bandini, Stranges, Choi et al., Small steps, strong shield: directly measured, moderate physical activity in 65 361 adults is associated with significant protective effects from severe COVID-19 outcomes, British journal of sports medicine, doi:10.1136/bjsports-2021-105159
Tavakol, Ghannadi, Tabesh, Halabchi, Noormohammadpour et al., Relationship between physical activity, healthy lifestyle and COVID-19 disease severity; a cross-sectional study, Zeitschrift fur Gesundheitswissenschaften = Journal of public health, doi:10.1007/s10389-020-01468-9
Team, Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19) -United States, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm6912e2
Tiansong, Shengjie, Zhirui, The Advanced meta-Analysis Method-Based on stata
Wells, Peterson, Welch, The Newcastle-Ottawa scale (NOS) for assessing the quality in nonrandomized studies in meta-analyses
Wunsch, Kienberger, Niessner, Changes in Physical Activity Patterns Due to the Covid-19 Pandemic: A Systematic Review and Meta-Analysis, Int J Environ Res Public Health, doi:10.3390/ijerph19042250
Xu, Doi, The robust error meta-regression method for dose-response meta-analysis. International journal of evidence-based healthcare, doi:10.1097/xeb.0000000000000132
Yuan, Huang, Chen, Chen, Zhang et al., Does pre-existent physical inactivity have a role in the severity of COVID-19? Therapeutic advances in respiratory disease, doi:10.1177/17534666211025221
DOI record:
{
"DOI": "10.1101/2022.06.22.22276789",
"URL": "http://dx.doi.org/10.1101/2022.06.22.22276789",
"abstract": "<jats:p>Background: Many people have experienced a high burden due to the spread of the coronavirus disease (COVID-19) and its serious consequences for health and everyday life. Prior studies have reported that physical activity (PA) may lower the risk of COVID-19 hospitalization. The present meta-analysis (PROSPERO registration number: CRD42022339672) explored the dose–response relationship between PA and the risk of COVID-19 hospitalization.\nMethods: Epidemiological observational studies on the relationship between PA and the risk of COVID-19 hospitalization were included. Categorical dose–response relationships between PA and the risk of COVID-19 hospitalization were assessed using random effect models. Robust error meta-regression models assessed the continuous relationship between PA (metabolic equivalent [MET]–h/week) and COVID-19 hospitalization risk across studies reporting quantitative PA estimates.\nResults: Seventeen observational studies (cohort\\case–control\\cross-section) met the criteria for inclusion in the meta-analysis. Categorical dose-relationship analysis showed a 40% (risk ratio (RR) 0.60, 95% confidence intervals (CI): 0.48–0.71) reduction in the risk of COVID-19 hospitalization compared to the lowest dose of PA. The results of the continuous dose–response relationship showed a non-linear inverse relationship (Pnon-linearity < 0.05) between PA and the risk of COVID-19 hospitalization. When total PA was less than or greater than 10 Met-h/week, an increase of 4 Met-h/week was associated with a 14% (RR = 0.83, 95%CI: 0.85–0.87) and 11% (RR = 0.89, 95%CI: 0.87–0.90) reduction in the risk of COVID-19 hospitalization, respectively.\nConclusions: There was an inverse non-linear dose–response relationship between PA level and the risk of COVID-19 hospitalization. Doses of the guideline-recommended minimum PA levels by WTO may be required for more substantial reductions in the COVID-19 hospitalization risk.</jats:p>",
"accepted": {
"date-parts": [
[
2022,
6,
23
]
]
},
"author": [
{
"affiliation": [],
"family": "Li",
"given": "Dan",
"sequence": "first"
},
{
"affiliation": [],
"family": "Jin",
"given": "Shengzhen",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4549-9496",
"affiliation": [],
"authenticated-orcid": false,
"family": "Lu",
"given": "Songtao",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
6,
24
]
],
"date-time": "2022-06-24T02:05:10Z",
"timestamp": 1656036310000
},
"deposited": {
"date-parts": [
[
2022,
6,
24
]
],
"date-time": "2022-06-24T02:05:12Z",
"timestamp": 1656036312000
},
"group-title": "Sports Medicine",
"indexed": {
"date-parts": [
[
2022,
6,
24
]
],
"date-time": "2022-06-24T02:41:18Z",
"timestamp": 1656038478024
},
"institution": [
{
"name": "medRxiv"
}
],
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
6,
23
]
]
},
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1101/2022.06.22.22276789",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "246",
"original-title": [],
"posted": {
"date-parts": [
[
2022,
6,
23
]
]
},
"prefix": "10.1101",
"published": {
"date-parts": [
[
2022,
6,
23
]
]
},
"publisher": "Cold Spring Harbor Laboratory",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "http://medrxiv.org/lookup/doi/10.1101/2022.06.22.22276789"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"subtype": "preprint",
"title": "Association of physical activity and the risk of COVID-19 hospitalization: a dose-response meta-analysis",
"type": "posted-content"
}
