Risk factors associated with hospitalization owing to COVID-19: a cross-sectional study in Palestine
et al., Journal of International Medical Research, doi:10.1177/03000605211064405, Dec 2021
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
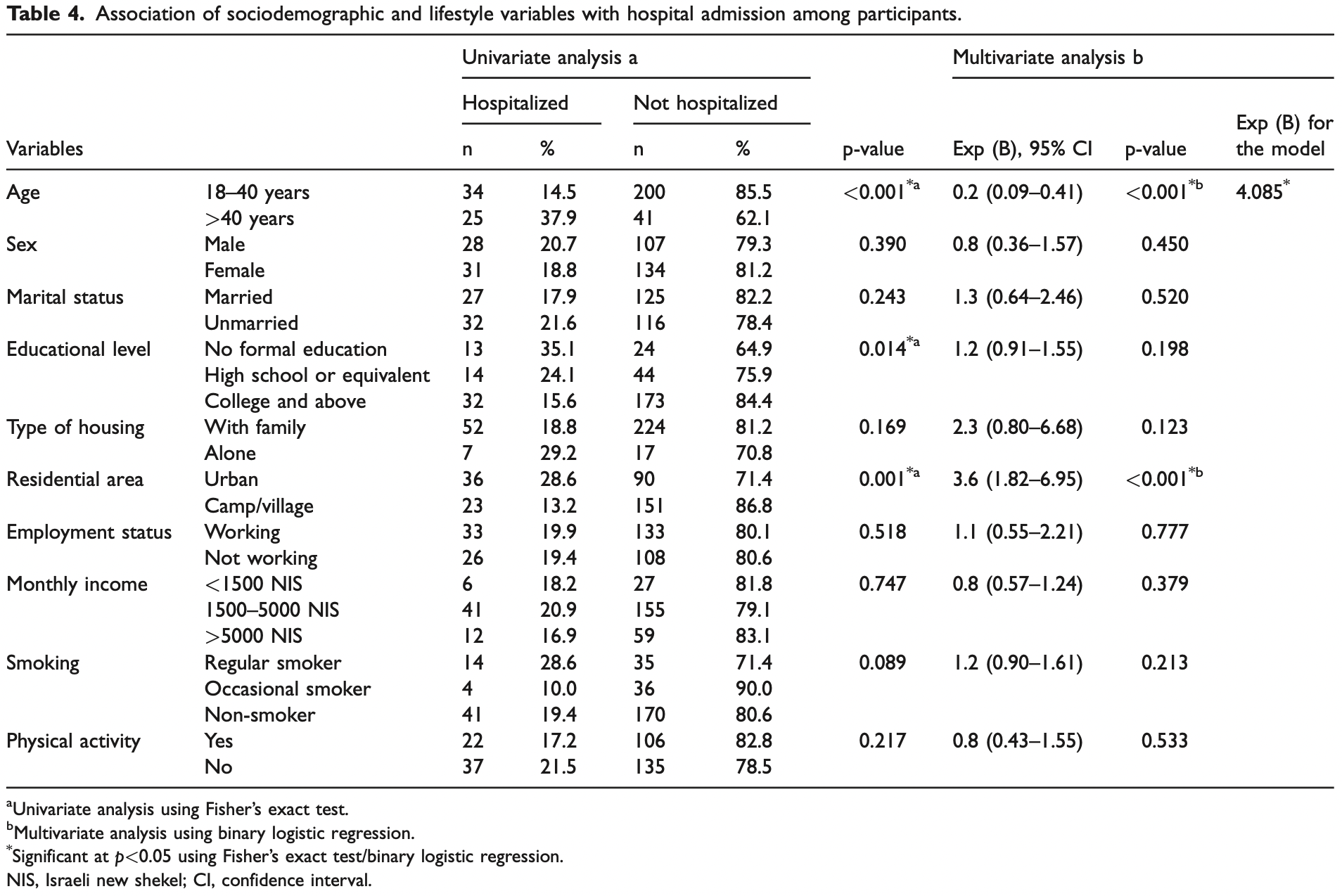
Retrospective 300 participants in Palestine, showing lower risk of hospitalization with physical activity, without statistical significance.
|
risk of hospitalization, 16.4% lower, RR 0.84, p = 0.53, high activity levels 22 of 128 (17.2%), low activity levels 37 of 172 (21.5%), NNT 23, adjusted per study, odds ratio converted to relative risk, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Hamdan et al., 23 Dec 2021, retrospective, Palestine, peer-reviewed, survey, mean age 30.5, 7 authors.
Contact: mayhamdan@ppu.edu.
Risk factors associated with hospitalization owing to COVID-19: a cross-sectional study in Palestine
Journal of International Medical Research, doi:10.1177/03000605211064405
Objectives: We aimed to identify the risk factors for coronavirus disease 2019 (COVID-19)associated hospitalization to provide evidence for improved clinical care of patients with COVID-19 infection. Methods: We conducted a cross-sectional study among 300 participants. The collected data comprised sociodemographic data, lifestyle habits, physical activity, medical history, anthropometric measurements, COVID-19-related symptoms, dietary habits prior to and after COVID-19 infection, and psychological status. Results: Fifty-nine participants were hospitalized. Fever, dry cough, joint pain, chills, diarrhea, and shortness of breath were significantly associated with hospitalization owing to COVID-19. Adults with obesity, diabetes mellitus, hypertension, respiratory diseases, and cardiovascular diseases had higher rates of hospitalization. The findings also showed that residential area and age were related to COVID-19 hospitalization. Furthermore, our analysis revealed that certain dietary habits were associated with hospitalization rates. Conclusion: Our study confirmed that older age, urban residence, illiteracy, obesity, hypertension, diabetes mellitus, respiratory diseases, cardiovascular diseases, and symptoms of loss of smell and sneezing elevated the risk of hospitalization among patients with COVID-19 infection.
Authors' contributions May Hamdan supervised the project and data collection. Manal Badrasawi was responsible for proposal revision and methodology optimization, supervision of data collection, and data analysis. Souzan Zidan was responsible for proposal revision and methodology optimization, supervision of data collection, data analysis, and writing the first draft. Asma Sayarah, Lamia Abu Zahra, Shahd Dana, and Tasneem Almasry were responsible for writing the review, drafting the proposal, collecting data, and data entry, and assisting in writing the proposal. All authors have read and approved the final manuscript.
Declaration of conflicting interest The authors declare that there is no conflict of interest.
ORCID iD
References
Afshin, Forouzanfar, Health Effects of Overweight and Obesity in 195 Countries over 25 Years, N Engl J Med
Alamri, Alsofayan, Alruthia, Predictors of Hospitalization Among Older Adults with COVID-19 in Saudi Arabia: A Cross-Sectional Study of a Nationally Representative Sample, Risk Manag
Azarpazhooh, Morovatdar, Avan, COVID-19 pandemic and burden of non-communicable diseases: an ecological study on data of 185 countries, J Stroke Cerebrovasc Dis
Caci, Albini, Malerba, COVID-19 and obesity: dangerous liaisons, J Clin Med
Casas, Sacanella, Estruch, The immune protective effect of the Mediterranean diet against chronic low-grade inflammatory diseases, Endocr Metab Immune Disord Drug Targets
Ca€ Er, Rouault, Roy, Immune cell-derived cytokines contribute to obesityrelated inflammation, fibrogenesis and metabolic deregulation in human adipose tissue, Sci Rep
Chen, Liang, Jiang, Risk Factors of Fatal Outcome in Hospitalized Subjects with Coronavirus Disease 2019 From a Nationwide Analysis in China, Chest
Du, Liang, Yang, Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study, Eur Respir J
Flores-Ram Irez, Iguez, Inez-Castillo, A review of environmental risks and vulnerability factors of indigenous populations from Latin America and the Caribbean in the face of the COVID-19, Glob Public Health
Garg, Kim, Whitaker, Hospitalization rates and characteristics of patients hospitalized with laboratoryconfirmed coronavirus disease 2019-COVID-NET, 14 states, MMWR Morb Mortal Wkly Rep
Gorbalenya, Baker, Baric, The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2, Nat Microbiol
Gralinski, Vd, Return of the coronavirus: 2019-nCoV, Viruses
Hamer, Gale, Kivim€ Aki, Overweight, obesity, and risk of hospitalization for COVID-19: A community-based cohort study of adults in the United Kingdom, Proc Natl Acad Sci U S A
Han, Ran, Mak, Smoking and Influenza-Associated Morbidity and Mortality: A Systematic Review and Meta-Analysis, Epidemiology
Honce, Schultz-Cherry, Impact of Obesity on Influenza A Virus Pathogenesis, Immune Response, and Evolution, Front Immunol
Kant, Dietary patterns: biomarkers and chronic disease risk, Appl Physiol Nutr Metab
Ko, Danielson, Town, Risk Factors for COVID-19-Associated Hospitalization: COVID-19-Associated Hospitalization Surveillance Network and Behavioral Risk Factor Surveillance System, Clin Infect Dis
Laddu, Lavie, Phillips, Physical activity for immunity protection: Inoculating populations with healthy living medicine in preparation for the next pandemic, Prog Cardiovasc Dis
Le On-Mart Inez, De, Sierra-De, Vega, Irez, Critical review of social, environmental and health risk factors in the Mexican indigenous population and their capacity to respond to the COVID-19, Sci Total Environ
Lee, Nieman, Nutritional Assessment
Lee, Nieman, Nutritional Assessment
Morgan, Bramley, Fowlkes, Morbid obesity as a risk factor for hospitalization and death due to 2009 pandemic influenza A(H1N1) disease, PLoS One
Overexpression, Shedding, and Antibody-Dependent Enhancement (ADE), Clinics
Palaiodimos, Kokkinidis, Li, Severe obesity, increasing age and male sex are independently associated with worse inhospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York, Metabolism
Peron, Nakaya, Susceptibility of the Elderly to SARS-CoV-2 Infection: ACE-2
Petrilli, Jones, Yang, Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study, BMJ
Pietil€ Ainen, Kaprio, Borg, Physical Inactivity and Obesity: A Vicious Circle, Obesity
Ranganathan, Pramesh, Aggarwal, Common pitfalls in statistical analysis: Logistic regression, Perspect Clin Res
Richardson, Hirsch, Narasimhan, Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area, JAMA
Soares, Mattos, Raposo, Risk Factors for Hospitalization and Mortality due to COVID-19 in Esp ırito Santo State, Brazil, Am J Trop Med Hyg
Tavakol, Ghannadi, Tabesh, Relationship between physical activity, healthy lifestyle and COVID-19 disease severity; a cross-sectional study, J Public Health, doi:10.1007/s10389-020-01468-9
Tetro, Is COVID-19 receiving ADE from other coronaviruses?, Microbes Infect
Verdecchia, Cavallini, Spanevello, The pivotal link between ACE2 deficiency and SARS-CoV-2 infection, Eur J Intern Med
Wang, Hu, Hu, Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China, JAMA
Weber, Zimmermann, Kieseier, Bacteria and their cell wall components uniformly co-activate interleukin-17-producing thymocytes, Clin Exp Immunol
Who, Body Mass index -report
Wolff, Starfield, Prevalence, expenditures, and complications of multiple chronic conditions in the elderly, Arch Intern Med
Wu, Chen, Cai, Risk Factors Associated with Acute Respiratory Distress Syndrome and Death in Patients with Coronavirus Disease 2019 Pneumonia in Wuhan, China, JAMA Intern Med
DOI record:
{
"DOI": "10.1177/03000605211064405",
"ISSN": [
"0300-0605",
"1473-2300"
],
"URL": "http://dx.doi.org/10.1177/03000605211064405",
"abstract": "<jats:sec><jats:title>Objectives</jats:title><jats:p> We aimed to identify the risk factors for coronavirus disease 2019 (COVID-19)-associated hospitalization to provide evidence for improved clinical care of patients with COVID-19 infection. </jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p> We conducted a cross-sectional study among 300 participants. The collected data comprised sociodemographic data, lifestyle habits, physical activity, medical history, anthropometric measurements, COVID-19-related symptoms, dietary habits prior to and after COVID-19 infection, and psychological status. </jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p> Fifty-nine participants were hospitalized. Fever, dry cough, joint pain, chills, diarrhea, and shortness of breath were significantly associated with hospitalization owing to COVID-19. Adults with obesity, diabetes mellitus, hypertension, respiratory diseases, and cardiovascular diseases had higher rates of hospitalization. The findings also showed that residential area and age were related to COVID-19 hospitalization. Furthermore, our analysis revealed that certain dietary habits were associated with hospitalization rates. </jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p> Our study confirmed that older age, urban residence, illiteracy, obesity, hypertension, diabetes mellitus, respiratory diseases, cardiovascular diseases, and symptoms of loss of smell and sneezing elevated the risk of hospitalization among patients with COVID-19 infection. Patients with a higher risk of hospitalization may benefit from targeted therapeutic and preventive interventions. </jats:p></jats:sec>",
"alternative-id": [
"10.1177/03000605211064405"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-4922-852X",
"affiliation": [
{
"name": "Program of Health and Therapeutic Nutrition, College of Medicine and Health Sciences, Palestine Polytechnic University, Hebron, Palestine"
}
],
"authenticated-orcid": false,
"family": "Hamdan",
"given": "May",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Nutrition and Food Technology, Faculty of Agriculture and Veterinary Medicine, An-Najah National University, Nablus, West Bank, Palestine"
}
],
"family": "Badrasawi",
"given": "Manal",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Nutrition and Food Technology, Faculty of Agriculture, Hebron University, Hebron, West Bank, Palestine"
}
],
"family": "Zidan",
"given": "Souzan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Program of Health and Therapeutic Nutrition, College of Medicine and Health Sciences, Palestine Polytechnic University, Hebron, Palestine"
}
],
"family": "Sayarah",
"given": "Asma",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Program of Health and Therapeutic Nutrition, College of Medicine and Health Sciences, Palestine Polytechnic University, Hebron, Palestine"
}
],
"family": "Zahra",
"given": "Lamia Abu",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Program of Health and Therapeutic Nutrition, College of Medicine and Health Sciences, Palestine Polytechnic University, Hebron, Palestine"
}
],
"family": "Dana",
"given": "Shahd",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Program of Health and Therapeutic Nutrition, College of Medicine and Health Sciences, Palestine Polytechnic University, Hebron, Palestine"
}
],
"family": "Almasry",
"given": "Tasneem",
"sequence": "additional"
}
],
"container-title": "Journal of International Medical Research",
"container-title-short": "J Int Med Res",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"journals.sagepub.com"
]
},
"created": {
"date-parts": [
[
2021,
12,
23
]
],
"date-time": "2021-12-23T10:34:52Z",
"timestamp": 1640255692000
},
"deposited": {
"date-parts": [
[
2021,
12,
23
]
],
"date-time": "2021-12-23T10:35:00Z",
"timestamp": 1640255700000
},
"indexed": {
"date-parts": [
[
2022,
8,
23
]
],
"date-time": "2022-08-23T00:25:21Z",
"timestamp": 1661214321486
},
"is-referenced-by-count": 3,
"issue": "12",
"issued": {
"date-parts": [
[
2021,
12
]
]
},
"journal-issue": {
"issue": "12",
"published-print": {
"date-parts": [
[
2021,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
12,
1
]
],
"date-time": "2021-12-01T00:00:00Z",
"timestamp": 1638316800000
}
}
],
"link": [
{
"URL": "http://journals.sagepub.com/doi/pdf/10.1177/03000605211064405",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://journals.sagepub.com/doi/full-xml/10.1177/03000605211064405",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://journals.sagepub.com/doi/pdf/10.1177/03000605211064405",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "179",
"original-title": [],
"page": "030006052110644",
"prefix": "10.1177",
"published": {
"date-parts": [
[
2021,
12
]
]
},
"published-online": {
"date-parts": [
[
2021,
12,
23
]
]
},
"published-print": {
"date-parts": [
[
2021,
12
]
]
},
"publisher": "SAGE Publications",
"reference": [
{
"DOI": "10.1038/s41564-020-0695-z",
"doi-asserted-by": "publisher",
"key": "bibr1-03000605211064405"
},
{
"DOI": "10.3390/v12020135",
"doi-asserted-by": "publisher",
"key": "bibr2-03000605211064405"
},
{
"key": "bibr3-03000605211064405",
"unstructured": "World Health Organization, 2021. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. (Accessed 22 May 2021)"
},
{
"key": "bibr4-03000605211064405",
"unstructured": "Palestinian Ministry of Health. Coronavirus- Covid19 Surveillance System. Available at: المرصد الالكتروني لفايروس كورونا المستجد - كوفيد 19 (moh.ps). (Accessed 22 May 2021)"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"doi-asserted-by": "publisher",
"key": "bibr5-03000605211064405"
},
{
"DOI": "10.1053/j.gastro.2020.04.017",
"doi-asserted-by": "publisher",
"key": "bibr6-03000605211064405"
},
{
"DOI": "10.1016/j.jemermed.2020.04.004",
"doi-asserted-by": "publisher",
"key": "bibr7-03000605211064405"
},
{
"DOI": "10.1001/jama.2020.1585",
"doi-asserted-by": "publisher",
"key": "bibr8-03000605211064405"
},
{
"DOI": "10.1371/journal.pone.0009694",
"doi-asserted-by": "publisher",
"key": "bibr9-03000605211064405"
},
{
"DOI": "10.3390/jcm9082511",
"doi-asserted-by": "publisher",
"key": "bibr10-03000605211064405"
},
{
"key": "bibr11-03000605211064405",
"unstructured": "World Health Organization (WHO). Obesity and overweight n.d. Available at: https: //www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (Accessed 16 March 2021)."
},
{
"DOI": "10.1016/j.jstrokecerebrovasdis.2020.105089",
"doi-asserted-by": "publisher",
"key": "bibr12-03000605211064405"
},
{
"DOI": "10.1016/j.pcad.2020.04.006",
"doi-asserted-by": "publisher",
"key": "bibr13-03000605211064405"
},
{
"DOI": "10.1038/oby.2007.72",
"doi-asserted-by": "publisher",
"key": "bibr14-03000605211064405"
},
{
"DOI": "10.15585/mmwr.mm6915e3",
"doi-asserted-by": "publisher",
"key": "bibr15-03000605211064405"
},
{
"DOI": "10.1007/s10389-020-01468-9",
"doi-asserted-by": "publisher",
"key": "bibr16-03000605211064405"
},
{
"DOI": "10.1139/H10-005",
"doi-asserted-by": "publisher",
"key": "bibr17-03000605211064405"
},
{
"DOI": "10.2174/1871530314666140922153350",
"doi-asserted-by": "publisher",
"key": "bibr18-03000605211064405"
},
{
"DOI": "10.1111/cei.12414",
"doi-asserted-by": "publisher",
"key": "bibr19-03000605211064405"
},
{
"author": "Alamri F",
"first-page": "875",
"journal-title": "Risk Manag",
"key": "bibr20-03000605211064405",
"volume": "14",
"year": "2021"
},
{
"key": "bibr21-03000605211064405",
"unstructured": "Lee RD, andNieman DC. Nutritional Assessment. McGraw-Hill Higher Education, 2007."
},
{
"key": "bibr22-03000605211064405",
"unstructured": "WHO. Body Mass index – report. 2018. Available at: https://gateway.euro.who.int/en/indicators/mn_survey_19-cut-off-for-bmi-according-to-who-standards/. (Accessed 22 March 2021)."
},
{
"DOI": "10.1136/bmj.m1966",
"doi-asserted-by": "publisher",
"key": "bibr23-03000605211064405"
},
{
"key": "bibr24-03000605211064405",
"unstructured": "Lee RD, Nieman DC. Nutritional Assessment. McGraw-Hill, 2013."
},
{
"DOI": "10.4269/ajtmh.20-0483",
"doi-asserted-by": "publisher",
"key": "bibr25-03000605211064405"
},
{
"DOI": "10.1073/pnas.2011086117",
"doi-asserted-by": "publisher",
"key": "bibr26-03000605211064405"
},
{
"DOI": "10.1016/j.chest.2020.04.010",
"doi-asserted-by": "publisher",
"key": "bibr27-03000605211064405"
},
{
"DOI": "10.1016/j.micinf.2020.02.006",
"doi-asserted-by": "publisher",
"key": "bibr28-03000605211064405"
},
{
"DOI": "10.6061/clinics/2020/e1912",
"doi-asserted-by": "publisher",
"key": "bibr29-03000605211064405"
},
{
"DOI": "10.1001/archinte.162.20.2269",
"doi-asserted-by": "publisher",
"key": "bibr30-03000605211064405"
},
{
"DOI": "10.1016/j.ejim.2020.04.037",
"doi-asserted-by": "publisher",
"key": "bibr31-03000605211064405"
},
{
"DOI": "10.1001/jama.2020.6775",
"doi-asserted-by": "publisher",
"key": "bibr32-03000605211064405"
},
{
"DOI": "10.1016/j.metabol.2020.154262",
"doi-asserted-by": "publisher",
"key": "bibr33-03000605211064405"
},
{
"author": "Ko JY",
"first-page": "ciaa1419",
"journal-title": "Clin Infect Dis",
"key": "bibr34-03000605211064405",
"year": "2020"
},
{
"DOI": "10.1038/s41598-017-02660-w",
"doi-asserted-by": "publisher",
"key": "bibr35-03000605211064405"
},
{
"DOI": "10.1056/NEJMoa1614362",
"doi-asserted-by": "publisher",
"key": "bibr36-03000605211064405"
},
{
"DOI": "10.3389/fimmu.2019.01071",
"doi-asserted-by": "publisher",
"key": "bibr37-03000605211064405"
},
{
"DOI": "10.1097/EDE.0000000000000984",
"doi-asserted-by": "publisher",
"key": "bibr38-03000605211064405"
},
{
"DOI": "10.1183/13993003.00524-2020",
"doi-asserted-by": "publisher",
"key": "bibr39-03000605211064405"
},
{
"DOI": "10.1001/jamainternmed.2020.0994",
"doi-asserted-by": "publisher",
"key": "bibr40-03000605211064405"
},
{
"author": "Ranganathan P",
"first-page": "148",
"journal-title": "Perspect Clin Res",
"key": "bibr41-03000605211064405",
"volume": "8",
"year": "2007"
},
{
"DOI": "10.1016/j.scitotenv.2020.139357",
"doi-asserted-by": "publisher",
"key": "bibr42-03000605211064405"
},
{
"DOI": "10.1080/17441692.2021.1923777",
"doi-asserted-by": "publisher",
"key": "bibr43-03000605211064405"
}
],
"reference-count": 43,
"references-count": 43,
"relation": {},
"resource": {
"primary": {
"URL": "http://journals.sagepub.com/doi/10.1177/03000605211064405"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Biochemistry (medical)",
"Cell Biology",
"Biochemistry",
"General Medicine"
],
"subtitle": [],
"title": "Risk factors associated with hospitalization owing to COVID-19: a cross-sectional study in Palestine",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1177/sage-journals-update-policy",
"volume": "49"
}
