Effects of physical activity on the severity of illness and mortality in COVID-19 patients: A systematic review and meta-analysis
et al., Frontiers in Physiology, doi:10.3389/fphys.2022.1030568, Nov 2022
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
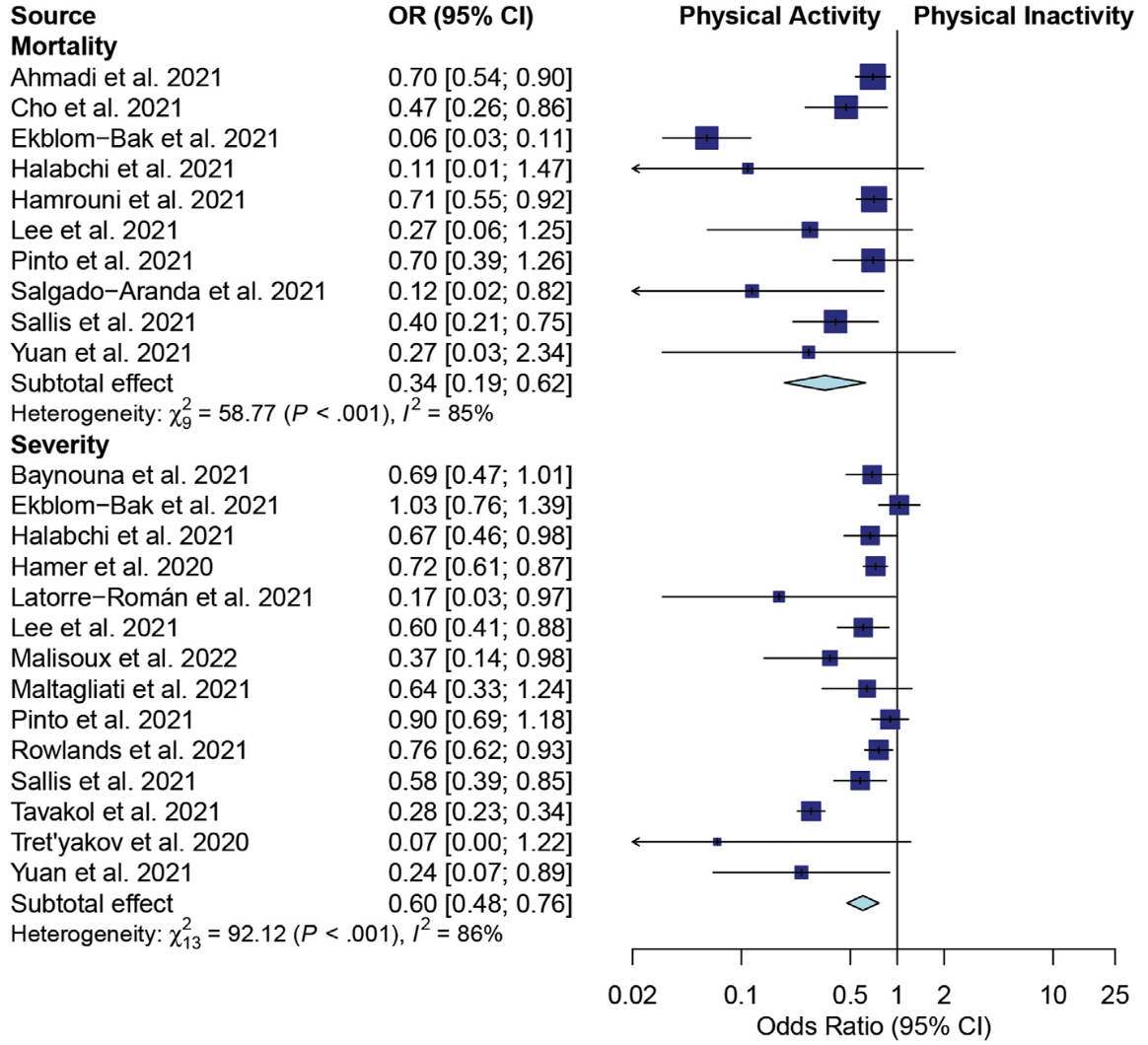
Systematic review and meta analysis of 18 studies, showing significantly lower COVID-19 severity and mortality with physical activity.
6 meta-analyses show significant improvements with exercise for mortality1-5,
ICU admission1,
hospitalization1,2,5,6 ,
severity2-4, and
cases2.
Currently there are 68 exercise for COVID-19 studies, showing 48% lower mortality [38‑57%], 46% lower ventilation [32‑57%], 41% lower ICU admission [35‑47%], 33% lower hospitalization [25‑40%], and 23% fewer cases [14‑31%].
1.
Rahmati et al., Baseline physical activity is associated with reduced mortality and disease outcomes in COVID-19: A systematic review and meta-analysis, Reviews in Medical Virology, doi:10.1002/rmv.2349.
2.
Ezzatvar et al., Physical activity and risk of infection, severity and mortality of COVID-19: a systematic review and non-linear dose–response meta-analysis of data from 1 853 610 adults, British Journal of Sports Medicine, doi:10.1136/bjsports-2022-105733.
3.
Sittichai et al., Effects of physical activity on the severity of illness and mortality in COVID-19 patients: A systematic review and meta-analysis, Frontiers in Physiology, doi:10.3389/fphys.2022.1030568.
4.
Liu et al., Baseline physical activity and the risk of severe illness and mortality from COVID-19: A dose–response meta-analysis, Preventive Medicine Reports, doi:10.1016/j.pmedr.2023.102130.
Sittichai et al., 8 Nov 2022, peer-reviewed, 8 authors.
Contact: mujalinp@gmail.com, coco_a105@hotmail.com.
Effects of physical activity on the severity of illness and mortality in COVID-19 patients: A systematic review and meta-analysis
Frontiers in Physiology, doi:10.3389/fphys.2022.1030568
Purpose: This systematic review and meta-analysis investigated the association between Physical activity (PA) before Coronavirus Disease 2019 (COVID-19) infection and the severity of illness and mortality in COVID-19 patients. Methods: A comprehensive search was undertaken to identify retrospective and nonrandomized controlled trial studies comparing the severity and mortality of COVID-19 infection among COVID-19 patients who had previously reported their participation in PA with those who had not. The databases searched were PubMed, Cochrane Library, Scopus, Science Direct, EMBASE, OPENGREY.EU, and ClinicalTrials.gov. The risk of bias was assessed using the Newcastle-Ottawa Scale. A random-effects model was used for determining pairwise meta-analyses. The protocol was registered with PROSPERO (CRD42021262548). Results: Eighteen studies met the inclusion criteria (5 cross-sectional, 12 cohort, and 1 case-control studies). All 1 618 680 subjects were adults. PA significantly decreased the risk of death in COVID-19 patients (odds ratio [OR] 0.34; 95% confidence interval [CI], 0.19-0.62; p < 0.001) and the risk of severe outcomes (OR 0.60; 95% CI, 0.48-0.76; p < 0.001). Subgroup analysis showed that PA for ≥150 min/wk at a moderate intensity or ≥75 min/wk at a vigorous intensity reduced the risks of severity and mortality. Vigorous PA reduced mortality risk, whereas moderate to vigorous PA reduced the risks of severity and mortality.
Conclusion: PA before infection might reduce severity and mortality in COVID-19 patients, especially PA ≥ 150 min/wk of moderate activity or ≥75 min/wk of
Author contributions NS, NP, SS, NK, KP, MP, and PP took part in designing the study, the selection process, and the writing of the first manuscript draft; NS, NP, SS, and MP took part in designing the study; NS, NP, SS, SK, NK, KP, and MP took part in the selection process and statistical analyses; NS, NP, NK, KP, MP, and PP wrote sections of the manuscript; all authors read and approved the final version of the manuscript and agreed with the order of presentation of the authors.
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys. 2022.1030568/full#supplementary-material
SUPPLEMENTARY FIGURE S1 Assessing publication bias by funnel plot: (A) effects of physical activity on mortality; (B) effects of physical activity on severity.
SUPPLEMENTARY FIGURE S2 Assessing publication bias by Egger's test: (A) effects of physical activity..
References
Ad Hagiu, Moderate exercise may prevent the development of severe forms of COVID-19, whereas high-intensity exercise may result in the opposite, Med. Hypotheses, doi:10.1016/j.mehy.2021.110705
Agarwal, Welsch, Keller, Francis, Chronic exercise modulates RAS components and improves balance between pro-and antiinflammatory cytokines in the brain of SHR, Basic Res. Cardiol, doi:10.1007/s00395-011-0231-7
Ahmadi, Huang, Inan-Eroglu, Hamer, Stamatakis, None
Ahmed, COVID-19 -does exercise prescription and maximal oxygen uptake (VO2 max) have a role in risk-stratifying patients?, Clin. Med, doi:10.7861/clinmed.2020-0111
Baynouna Alketbi, Nagelkerke, Abdelbaqi, Alblooshi, Alsaedi et al., Risk factors for SARS-CoV-2 infection severity in Abu Dhabi, J. Epidemiol. Glob. Health, doi:10.1007/s44197-021-00006-4
Cai, Chen, Wang, Luo, Liu et al., Obesity and COVID-19 severity in a designated hospital in Shenzhen, China, Diabetes Care
Caspersen, Powell, Christenson, Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research, doi:10.2307/20056429
Chandrasekaran, Ganesan, Sedentarism and chronic disease risk in COVID 19 lockdown -A scoping review, Scott. Med. J, doi:10.1177/0036933020946336
Cho, Lee, Jae, Kim, Ha et al., Physical exercise as a tool to help the immune system against COVID-19: An integrative review of the current literature, Clin. Exp. Med, doi:10.1007/s10238-020-00650-3
Da Tavakol, Ghannadi, Tabesh, Halabchi, Noormohammadpour et al., Relationship between physical activity, healthy lifestyle and COVID-19 disease severity; a cross-sectional study, J. Public Health, doi:10.1007/s10389-020-01468-9
Ekblom-Bak, Väisänen, Ekblom, Blom, Kallings et al., Cardiorespiratory fitness and lifestyle on severe COVID-19 risk in 279, 455 adults: A case control study, Int. J. Behav. Nutr. Phys. Act, doi:10.1186/s12966-021-01198-5
Fahriani, Ilmawan, Fajar, Maliga, Frediansyah et al., Persistence of long COVID symptoms in COVID-19 survivors worldwide and its potential pathogenesis -a systematic review and metaanalysis, Narra J, doi:10.52225/narraj.v1i2.36
Fajar, Ilmawan, Mamada, Mutiawati, Husnah et al., Global prevalence of persistent neuromuscular symptoms and the possible pathomechanisms in COVID-19 recovered individuals: A systematic review and meta-analysis, Narra J, doi:10.52225/narra.v1i3.48
Foster, Ravikumar, Bellotto, Unger, Hsia, Fatty diabetic lung: Altered alveolar structure and surfactant protein expression, Am. J. Physiol. Lung Cell. Mol. Physiol, doi:10.1152/ajplung.00041.2009
Guyatt, Oxman, Vist, Kunz, Falck-Ytter et al., None
Halabchi, Mazaheri, Sabeti, Yunesian, Alizadeh et al., Regular sports participation as a potential predictor of better clinical outcome in adult patients with COVID-19: A large cross-sectional study, J. Phys. Act. Health, doi:10.1123/jpah.2020-0392
Halperin, Prevalence of asymptomatic SARS-CoV-2 infection
Hamer, Kivimäki, Gale, Batty, Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A communitybased cohort study of 387, 109 adults in UK, Brain Behav. Immun, doi:10.1016/j.bbi.2020.05.059
Hamrouni, Roberts, Thackray, Stensel, Bishop, None
Kai, Kai, Interactions of coronaviruses with ACE2, angiotensin II, and RAS inhibitors-Lessons from available evidence and insights into COVID-19, Hypertens. Res, doi:10.1038/s41440-020-0455-8
Kharroubi, Saleh, Are lockdown measures effective against COVID-19? Front, Public Health, doi:10.3389/fpubh.2020.549692
Lai, Shih, Ko, Tang, Hsueh, Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges, Int. J. Antimicrob. Agents, doi:10.1016/j.ijantimicag.2020.105924
Latorre-Román, Guzmán-Guzmán, Delgado-Floody, Herrador, None
Lee, Lee, Moon, Jin, Yang et al., Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: A nationwide cohort study, Br. J. Sports Med, doi:10.1136/bjsports-2021-104203
Lowder, Padgett, Woods, Moderate exercise early after influenza virus infection reduces the Th1 inflammatory response in lungs of mice, Exerc. Immunol. Rev
Malisoux, Backes, Fischer, Aguayo, Ollert et al., Associations between physical activity prior to infection and COVID-19 disease severity and symptoms: Results from the prospective predi-COVID cohort study, BMJ Open, doi:10.1136/bmjopen-2021-057863
Maltagliati, Sieber, Sarrazin, Cullati, Chalabaev et al., Muscle strength explains the protective effect of physical activity against COVID-19 hospitalization among adults aged 50 Years and older, medRxiv, doi:10.1101/2021.02.25.21252451
Marino, Vargas, Skein, Hartmann, Mcfarlin et al., Metabolic and inflammatory health in SARS-CoV-2 and the potential role for habitual exercise in reducing disease severity, Inflamm. Res, doi:10.1007/s00011-021-01517-3
Mayer, Exercise stress increases susceptibility to influenza infection, Brain Behav. Immun, doi:10.1016/j.bbi.2008.06.004
Murphy, Davis, Carmichael, Gangemi, Ghaffar, None
Nieman, Nehlsen-Cannarella, Fagoaga, Henson, Shannonm et al., Immune function in female elite rowers and non-athletes, Br. J. Sports Med, doi:10.1136/bjsm.34.3.181
Nieman, Nehlsen-Cannarella, Markoff, Balk-Lamberton, Yang et al., The effects of moderate exercise training on natural killer cells and acute upper respiratory tract infections, Int. J. Sports Med
Nieman, Wentz, The compelling link between physical activity and the body's defense system, J. Sport Health Sci, doi:10.1016/j.jshs.2018.09.009
Page, Mckenzie, Bossuyt, Boutron, Hoffmann et al., The PRISMA 2020 statement: An updated guideline for reporting systematic reviews, Br. Med. J, doi:10.1136/bmj.n71
Pinto, Goessler, Fernandes, Murai, Sales et al., No independent associations between physical activity and clinical outcomes among hospitalized patients with moderate to severe COVID-19, J. Sport Health Sci, doi:10.1016/j.jshs.2021.08.001
Popkin, Du, Green, Beck, Algaith et al., Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships, Obes. Rev, doi:10.1111/obr.13128
Rahmati, Shamsi, Khoramipour, Malakoutinia, Woo et al., Baseline physical activity is associated with reduced mortality and disease outcomes in COVID-19: A systematic review and meta-analysis, Rev. Med. Virol, doi:10.1002/rmv.2349
Rowlands, Dempsey, Gillies, Kloecker, Razieh et al., Association between accelerometer-assessed physical activity and severity of COVID-19 in UK biobank, Mayo Clin. Proc. Innov. Qual. Outcomes, doi:10.1016/j.mayocpiqo.2021.08.011
Salgado-Aranda, Pérez-Castellano, Núñez-Gil, Orozco, Torres-Esquivel et al., Influence of baseline physical activity as a modifying factor on COVID-19 mortality: A single-center, retrospective study, Infect. Dis. Ther, doi:10.1007/s40121-021-00418-6
Sallis, Young, Tartof, Sallis, Sall et al., Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: A study in Frontiers in Physiology frontiersin
Sanchez, Aragón-Vela, García Pinillos, Protective role of physical activity patterns prior to COVID-19 confinement with the severity/ duration of respiratory pathologies consistent with COVID-19 symptoms in Spanish populations, Res. Sports Med, doi:10.1080/15438627.2021.1937166
Sim, Yu, Yoon, Loiacono, Kohut, Chronic exercise reduces illness severity, decreases viral load, and results in greater antiinflammatory effects than acute exercise during influenza infection, J. Infect. Dis, doi:10.1086/606014
Stang, Stockwell, Trott, Tully, Shin et al., Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses, Eur. J. Epidemiol, doi:10.1007/s10654-010-9491-z
Strath, Kaminsky, Ainsworth, Ekelund, Freedson et al., Guide to the assessment of physical activity: Clinical and research applications: A scientific statement from the American heart association, Circulation, doi:10.1161/01.cir.0000435708.67487.da
Timmons, Cieslak, Human natural killer cell subsets and acute exercise: A brief review, Exerc. Immunol. Rev
Toledo, Magalhaes, Hizume, Vieira, Biselli et al., Aerobic exercise attenuates pulmonary injury induced by exposure to cigarette smoke, Eur. Respir. J, doi:10.1183/09031936.00003411
Tracey, Reflex control of immunity, Nat. Rev. Immunol, doi:10.1038/nri2566
Tret'yakov, Zakharchenko, Romasenko, Dyatlova, Zhabskaya et al., COVID-19 in individuals adapted to aerobic exercise, Pulʹmonologia, doi:10.18093/0869-0189-2020-30-5-553-560
Verity, Okell, Dorigatti, Winskill, Whittaker et al., Estimates of the severity of coronavirus disease 2019: A modelbased analysis, Lancet. Infect. Dis, doi:10.1016/s1473-3099(20)30243-7
Warren, Olson, Thompson, Cahill, Wyatt et al., None
Yan, Xiao, Lin, Angiotensin-converting enzyme 2 in severe acute respiratory syndrome coronavirus and SARS-CoV-2: A double-edged sword?, FASEB J, doi:10.1096/fj.202000782
Yuan, Huang, Chen, Chen, Zhang et al., Does pre-existent physical inactivity have a role in the severity of COVID-19?, Ther. Adv. Respir. Dis, doi:10.1177/17534666211025221
Zhang, Zhu, Cai, Lei, Qin et al., Association of inpatient use of angiotensin converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19, Circ. Res, doi:10.1161/circresaha.120.317134
DOI record:
{
"DOI": "10.3389/fphys.2022.1030568",
"ISSN": [
"1664-042X"
],
"URL": "http://dx.doi.org/10.3389/fphys.2022.1030568",
"abstract": "<jats:p><jats:bold>Purpose:</jats:bold> This systematic review and meta-analysis investigated the association between Physical activity (PA) before Coronavirus Disease 2019 (COVID-19) infection and the severity of illness and mortality in COVID-19 patients.</jats:p><jats:p><jats:bold>Methods:</jats:bold> A comprehensive search was undertaken to identify retrospective and nonrandomized controlled trial studies comparing the severity and mortality of COVID-19 infection among COVID-19 patients who had previously reported their participation in PA with those who had not. The databases searched were PubMed, Cochrane Library, Scopus, Science Direct, EMBASE, OPENGREY.EU, and <jats:ext-link>ClinicalTrials.gov</jats:ext-link>. The risk of bias was assessed using the Newcastle-Ottawa Scale. A random-effects model was used for determining pairwise meta-analyses. The protocol was registered with PROSPERO (CRD42021262548).</jats:p><jats:p><jats:bold>Results:</jats:bold> Eighteen studies met the inclusion criteria (5 cross-sectional, 12 cohort, and 1 case-control studies). All 1 618 680 subjects were adults. PA significantly decreased the risk of death in COVID-19 patients (odds ratio [OR] 0.34; 95% confidence interval [CI], 0.19–0.62; <jats:italic>p</jats:italic> &lt; 0.001) and the risk of severe outcomes (OR 0.60; 95% CI, 0.48–0.76; <jats:italic>p</jats:italic> &lt; 0.001). Subgroup analysis showed that PA for ≥150 min/wk at a moderate intensity or ≥75 min/wk at a vigorous intensity reduced the risks of severity and mortality. Vigorous PA reduced mortality risk, whereas moderate to vigorous PA reduced the risks of severity and mortality.</jats:p><jats:p><jats:bold>Conclusion:</jats:bold> PA before infection might reduce severity and mortality in COVID-19 patients, especially PA ≥ 150 min/wk of moderate activity or ≥75 min/wk of vigorous activity. However, careful interpretations should be considered due to the difference in PA patterns and severity definitions among included studies. This finding implies that engaging in regular PA, even in different patterns, has beneficial effects on the severity and mortality of COVID-19 patients.</jats:p>",
"alternative-id": [
"10.3389/fphys.2022.1030568"
],
"author": [
{
"affiliation": [],
"family": "Sittichai",
"given": "Nuttawut",
"sequence": "first"
},
{
"affiliation": [],
"family": "Parasin",
"given": "Nichapa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Saokaew",
"given": "Surasak",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kanchanasurakit",
"given": "Sukrit",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kayod",
"given": "Nuttawan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Praikaew",
"given": "Ketnapa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Phisalprapa",
"given": "Pochamana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Prasannarong",
"given": "Mujalin",
"sequence": "additional"
}
],
"container-title": "Frontiers in Physiology",
"container-title-short": "Front. Physiol.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2022,
11,
8
]
],
"date-time": "2022-11-08T07:33:08Z",
"timestamp": 1667892788000
},
"deposited": {
"date-parts": [
[
2022,
11,
8
]
],
"date-time": "2022-11-08T07:33:16Z",
"timestamp": 1667892796000
},
"indexed": {
"date-parts": [
[
2022,
11,
9
]
],
"date-time": "2022-11-09T06:01:19Z",
"timestamp": 1667973679704
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
11,
8
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
11,
8
]
],
"date-time": "2022-11-08T00:00:00Z",
"timestamp": 1667865600000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fphys.2022.1030568/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2022,
11,
8
]
]
},
"published-online": {
"date-parts": [
[
2022,
11,
8
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.1007/s00395-011-0231-7",
"article-title": "Chronic exercise modulates RAS components and improves balance between pro- and anti-inflammatory cytokines in the brain of SHR",
"author": "Agarwal",
"doi-asserted-by": "publisher",
"first-page": "1069",
"journal-title": "Basic Res. Cardiol.",
"key": "B1",
"volume": "106",
"year": "2011"
},
{
"DOI": "10.1016/j.bbi.2021.04.022",
"article-title": "Lifestyle risk factors and infectious disease mortality, including COVID-19, among middle aged and older adults: Evidence from a community-based cohort study in the United Kingdom",
"author": "Ahmadi",
"doi-asserted-by": "publisher",
"first-page": "18",
"journal-title": "Brain Behav. Immun.",
"key": "B2",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.7861/clinmed.2020-0111",
"article-title": "COVID-19 – does exercise prescription and maximal oxygen uptake (VO2 max) have a role in risk-stratifying patients?",
"author": "Ahmed",
"doi-asserted-by": "publisher",
"first-page": "282",
"journal-title": "Clin. Med.",
"key": "B3",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1007/s44197-021-00006-4",
"article-title": "Risk factors for SARS-CoV-2 infection severity in Abu Dhabi",
"author": "Baynouna AlKetbi",
"doi-asserted-by": "publisher",
"first-page": "344",
"journal-title": "J. Epidemiol. Glob. Health",
"key": "B4",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.2337/dc20-0576",
"article-title": "Obesity and COVID-19 severity in a designated hospital in Shenzhen, China",
"author": "Cai",
"doi-asserted-by": "publisher",
"first-page": "1392",
"journal-title": "Diabetes Care",
"key": "B5",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.2307/20056429",
"article-title": "Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research",
"author": "Caspersen",
"doi-asserted-by": "publisher",
"first-page": "126",
"journal-title": "Public Health Rep.",
"key": "B6",
"volume": "100",
"year": "1985"
},
{
"key": "B7",
"unstructured": "People with certain medical conditions centers for disease control and prevention2020"
},
{
"DOI": "10.1177/0036933020946336",
"article-title": "Sedentarism and chronic disease risk in COVID 19 lockdown – A scoping review",
"author": "Chandrasekaran",
"doi-asserted-by": "publisher",
"first-page": "3",
"journal-title": "Scott. Med. J.",
"key": "B8",
"volume": "66",
"year": "2020"
},
{
"DOI": "10.3390/jcm10071539",
"article-title": "Physical activity and the risk of COVID-19 infection and mortality: A nationwide population-based case-control study",
"author": "Cho",
"doi-asserted-by": "publisher",
"first-page": "1539",
"journal-title": "J. Clin. Med.",
"key": "B9",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1007/s10238-020-00650-3",
"article-title": "Physical exercise as a tool to help the immune system against COVID-19: An integrative review of the current literature",
"author": "da Silveira",
"doi-asserted-by": "publisher",
"first-page": "15",
"journal-title": "Clin. Exp. Med.",
"key": "B10",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1186/s12966-021-01198-5",
"article-title": "Cardiorespiratory fitness and lifestyle on severe COVID-19 risk in 279, 455 adults: A case control study",
"author": "Ekblom-Bak",
"doi-asserted-by": "publisher",
"first-page": "135",
"journal-title": "Int. J. Behav. Nutr. Phys. Act.",
"key": "B11",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.52225/narraj.v1i2.36",
"article-title": "Persistence of long COVID symptoms in COVID-19 survivors worldwide and its potential pathogenesis - a systematic review and meta-analysis",
"author": "Fahriani",
"doi-asserted-by": "publisher",
"first-page": "36",
"journal-title": "Narra J.",
"key": "B12",
"volume": "1",
"year": "2021"
},
{
"DOI": "10.52225/narra.v1i3.48",
"article-title": "Global prevalence of persistent neuromuscular symptoms and the possible pathomechanisms in COVID-19 recovered individuals: A systematic review and meta-analysis",
"author": "Fajar",
"doi-asserted-by": "publisher",
"first-page": "48",
"journal-title": "Narra J.",
"key": "B13",
"volume": "1",
"year": "2021"
},
{
"DOI": "10.1152/ajplung.00041.2009",
"article-title": "Fatty diabetic lung: Altered alveolar structure and surfactant protein expression",
"author": "Foster",
"doi-asserted-by": "publisher",
"first-page": "L392",
"journal-title": "Am. J. Physiol. Lung Cell. Mol. Physiol.",
"key": "B14",
"volume": "298",
"year": "2010"
},
{
"DOI": "10.1136/bmj.39489.470347.AD",
"article-title": "Grade: An emerging consensus on rating quality of evidence and strength of recommendations",
"author": "Guyatt",
"doi-asserted-by": "publisher",
"first-page": "924",
"journal-title": "BMJ",
"key": "B15",
"volume": "336",
"year": "2008"
},
{
"DOI": "10.1016/j.mehy.2021.110705",
"article-title": "Moderate exercise may prevent the development of severe forms of COVID-19, whereas high-intensity exercise may result in the opposite",
"author": "Hagiu",
"doi-asserted-by": "publisher",
"first-page": "110705",
"journal-title": "Med. Hypotheses",
"key": "B16",
"volume": "157",
"year": "2021"
},
{
"DOI": "10.1123/jpah.2020-0392",
"article-title": "Regular sports participation as a potential predictor of better clinical outcome in adult patients with COVID-19: A large cross-sectional study",
"author": "Halabchi",
"doi-asserted-by": "publisher",
"first-page": "8",
"journal-title": "J. Phys. Act. Health",
"key": "B17",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.7326/l20-1282",
"article-title": "Prevalence of asymptomatic SARS-CoV-2 infection",
"author": "Halperin",
"doi-asserted-by": "publisher",
"first-page": "283",
"journal-title": "Ann. Intern. Med.",
"key": "B18",
"volume": "174",
"year": "2021"
},
{
"DOI": "10.1016/j.bbi.2020.05.059",
"article-title": "Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387, 109 adults in UK",
"author": "Hamer",
"doi-asserted-by": "publisher",
"first-page": "184",
"journal-title": "Brain Behav. Immun.",
"key": "B19",
"volume": "87",
"year": "2020"
},
{
"DOI": "10.1136/bmjopen-2021-055003",
"article-title": "Associations of obesity, physical activity level, inflammation and cardiometabolic health with COVID-19 mortality: A prospective analysis of the UK biobank cohort",
"author": "Hamrouni",
"doi-asserted-by": "publisher",
"first-page": "e055003",
"journal-title": "BMJ Open",
"key": "B20",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1038/s41440-020-0455-8",
"article-title": "Interactions of coronaviruses with ACE2, angiotensin II, and RAS inhibitors—Lessons from available evidence and insights into COVID-19",
"author": "Kai",
"doi-asserted-by": "publisher",
"first-page": "648",
"journal-title": "Hypertens. Res.",
"key": "B21",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.3389/fpubh.2020.549692",
"article-title": "Are lockdown measures effective against COVID-19?",
"author": "Kharroubi",
"doi-asserted-by": "publisher",
"first-page": "549692",
"journal-title": "Front. Public Health",
"key": "B22",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/j.ijantimicag.2020.105924",
"article-title": "Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges",
"author": "Lai",
"doi-asserted-by": "publisher",
"first-page": "105924",
"journal-title": "Int. J. Antimicrob. Agents",
"key": "B23",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.1080/15438627.2021.1937166",
"article-title": "Protective role of physical activity patterns prior to COVID-19 confinement with the severity/duration of respiratory pathologies consistent with COVID-19 symptoms in Spanish populations",
"author": "Latorre-Román",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Res. Sports Med.",
"key": "B24",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1136/bjsports-2021-104203",
"article-title": "Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: A nationwide cohort study",
"author": "Lee",
"doi-asserted-by": "publisher",
"first-page": "901",
"journal-title": "Br. J. Sports Med.",
"key": "B25",
"volume": "56",
"year": "2021"
},
{
"article-title": "Moderate exercise early after influenza virus infection reduces the Th1 inflammatory response in lungs of mice",
"author": "Lowder",
"first-page": "97",
"journal-title": "Exerc. Immunol. Rev.",
"key": "B26",
"volume": "12",
"year": "2006"
},
{
"DOI": "10.1136/bmjopen-2021-057863",
"article-title": "Associations between physical activity prior to infection and COVID-19 disease severity and symptoms: Results from the prospective predi-COVID cohort study",
"author": "Malisoux",
"doi-asserted-by": "publisher",
"first-page": "e057863",
"journal-title": "BMJ Open",
"key": "B27",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1101/2021.02.25.21252451",
"article-title": "Muscle strength explains the protective effect of physical activity against COVID-19 hospitalization among adults aged 50 Years and older",
"author": "Maltagliati",
"doi-asserted-by": "publisher",
"first-page": "21252451",
"journal-title": "medRxiv.",
"key": "B28",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.1007/s00011-021-01517-3",
"article-title": "Metabolic and inflammatory health in SARS-CoV-2 and the potential role for habitual exercise in reducing disease severity",
"author": "Marino",
"doi-asserted-by": "publisher",
"first-page": "27",
"journal-title": "Inflamm. Res.",
"key": "B29",
"volume": "71",
"year": "2022"
},
{
"DOI": "10.1093/gerona/60.10.1315",
"article-title": "Chronic resistance exercise training improves natural killer cell activity in older women",
"author": "McFarlin",
"doi-asserted-by": "publisher",
"first-page": "1315",
"journal-title": "J. Gerontol. A Biol. Sci. Med. Sci.",
"key": "B30",
"volume": "60",
"year": "2005"
},
{
"DOI": "10.1016/j.bbi.2008.06.004",
"article-title": "Exercise stress increases susceptibility to influenza infection",
"author": "Murphy",
"doi-asserted-by": "publisher",
"first-page": "1152",
"journal-title": "Brain Behav. Immun.",
"key": "B31",
"volume": "22",
"year": "2008"
},
{
"DOI": "10.1136/bjsm.34.3.181",
"article-title": "Immune function in female elite rowers and non-athletes",
"author": "Nieman",
"doi-asserted-by": "publisher",
"first-page": "181",
"journal-title": "Br. J. Sports Med.",
"key": "B32",
"volume": "34",
"year": "2000"
},
{
"DOI": "10.1055/s-2007-1024839",
"article-title": "The effects of moderate exercise training on natural killer cells and acute upper respiratory tract infections",
"author": "Nieman",
"doi-asserted-by": "publisher",
"first-page": "467",
"journal-title": "Int. J. Sports Med.",
"key": "B33",
"volume": "11",
"year": "1990"
},
{
"DOI": "10.1016/j.jshs.2018.09.009",
"article-title": "The compelling link between physical activity and the body’s defense system",
"author": "Nieman",
"doi-asserted-by": "publisher",
"first-page": "201",
"journal-title": "J. Sport Health Sci.",
"key": "B34",
"volume": "8",
"year": "2019"
},
{
"DOI": "10.1136/bmj.n71",
"article-title": "The PRISMA 2020 statement: An updated guideline for reporting systematic reviews",
"author": "Page",
"doi-asserted-by": "publisher",
"first-page": "n71",
"journal-title": "Br. Med. J.",
"key": "B35",
"volume": "372",
"year": "2021"
},
{
"DOI": "10.1001/jama.2018.14854",
"article-title": "The physical activity guidelines for americans",
"author": "Piercy",
"doi-asserted-by": "publisher",
"first-page": "2020",
"journal-title": "JAMA",
"key": "B36",
"volume": "320",
"year": "2018"
},
{
"DOI": "10.1016/j.jshs.2021.08.001",
"article-title": "No independent associations between physical activity and clinical outcomes among hospitalized patients with moderate to severe COVID-19",
"author": "Pinto",
"doi-asserted-by": "publisher",
"first-page": "690",
"journal-title": "J. Sport Health Sci.",
"key": "B37",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1111/obr.13128",
"article-title": "Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships",
"author": "Popkin",
"doi-asserted-by": "publisher",
"first-page": "e13128",
"journal-title": "Obes. Rev.",
"key": "B38",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1002/rmv.2349",
"article-title": "Baseline physical activity is associated with reduced mortality and disease outcomes in COVID-19: A systematic review and meta-analysis",
"author": "Rahmati",
"doi-asserted-by": "publisher",
"first-page": "e2349",
"journal-title": "Rev. Med. Virol.",
"key": "B39",
"volume": "32",
"year": "2022"
},
{
"DOI": "10.1016/j.mayocpiqo.2021.08.011",
"article-title": "Association between accelerometer-assessed physical activity and severity of COVID-19 in UK biobank",
"author": "Rowlands",
"doi-asserted-by": "publisher",
"first-page": "997",
"journal-title": "Mayo Clin. Proc. Innov. Qual. Outcomes",
"key": "B40",
"volume": "5",
"year": "2021"
},
{
"DOI": "10.1007/s40121-021-00418-6",
"article-title": "Influence of baseline physical activity as a modifying factor on COVID-19 mortality: A single-center, retrospective study",
"author": "Salgado-Aranda",
"doi-asserted-by": "publisher",
"first-page": "801",
"journal-title": "Infect. Dis. Ther.",
"key": "B41",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1136/bjsports-2021-104080",
"article-title": "Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: A study in 48 440 adult patients",
"author": "Sallis",
"doi-asserted-by": "publisher",
"first-page": "1099",
"journal-title": "Br. J. Sports Med.",
"key": "B42",
"volume": "55",
"year": "2021"
},
{
"DOI": "10.1086/606014",
"article-title": "Chronic exercise reduces illness severity, decreases viral load, and results in greater anti-inflammatory effects than acute exercise during influenza infection",
"author": "Sim",
"doi-asserted-by": "publisher",
"first-page": "1434",
"journal-title": "J. Infect. Dis.",
"key": "B43",
"volume": "200",
"year": "2009"
},
{
"DOI": "10.1007/s10654-010-9491-z",
"article-title": "Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses",
"author": "Stang",
"doi-asserted-by": "publisher",
"first-page": "603",
"journal-title": "Eur. J. Epidemiol.",
"key": "B44",
"volume": "25",
"year": "2010"
},
{
"DOI": "10.1136/bmjsem-2020-000960",
"article-title": "Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review",
"author": "Stockwell",
"doi-asserted-by": "publisher",
"first-page": "e000960",
"journal-title": "BMJ Open Sport Exerc. Med.",
"key": "B45",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1161/01.cir.0000435708.67487.da",
"article-title": "Guide to the assessment of physical activity: Clinical and research applications: A scientific statement from the American heart association",
"author": "Strath",
"doi-asserted-by": "publisher",
"first-page": "2259",
"journal-title": "Circulation",
"key": "B46",
"volume": "128",
"year": "2013"
},
{
"DOI": "10.1007/s10389-020-01468-9",
"article-title": "Relationship between physical activity, healthy lifestyle and COVID-19 disease severity; a cross-sectional study",
"author": "Tavakol",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J. Public Health",
"key": "B47",
"volume": "4",
"year": "2021"
},
{
"article-title": "Human natural killer cell subsets and acute exercise: A brief review",
"author": "Timmons",
"first-page": "8",
"journal-title": "Exerc. Immunol. Rev.",
"key": "B48",
"volume": "14",
"year": "2008"
},
{
"DOI": "10.1183/09031936.00003411",
"article-title": "Aerobic exercise attenuates pulmonary injury induced by exposure to cigarette smoke",
"author": "Toledo",
"doi-asserted-by": "publisher",
"first-page": "254",
"journal-title": "Eur. Respir. J.",
"key": "B49",
"volume": "39",
"year": "2012"
},
{
"DOI": "10.1038/nri2566",
"article-title": "Reflex control of immunity",
"author": "Tracey",
"doi-asserted-by": "publisher",
"first-page": "418",
"journal-title": "Nat. Rev. Immunol.",
"key": "B50",
"volume": "9",
"year": "2009"
},
{
"DOI": "10.18093/0869-0189-2020-30-5-553-560",
"article-title": "COVID-19 in individuals adapted to aerobic exercise",
"author": "Tret’yakov",
"doi-asserted-by": "publisher",
"first-page": "553",
"journal-title": "Pulʹmonologia.",
"key": "B51",
"volume": "30",
"year": "2020"
},
{
"DOI": "10.1016/s1473-3099(20)30243-7",
"article-title": "Estimates of the severity of coronavirus disease 2019: A model-based analysis",
"author": "Verity",
"doi-asserted-by": "publisher",
"first-page": "669",
"journal-title": "Lancet. Infect. Dis.",
"key": "B52",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0129713",
"article-title": "Exercise improves host response to influenza viral infection in obese and non-obese mice through different mechanisms",
"author": "Warren",
"doi-asserted-by": "publisher",
"first-page": "e0129713",
"journal-title": "PLOS ONE",
"key": "B53",
"volume": "10",
"year": "2015"
},
{
"key": "B54",
"volume-title": "Clinical management of COVID-19: Living guideline",
"year": ""
},
{
"key": "B55",
"unstructured": "Physical activity. [online] world health organization"
},
{
"key": "B56",
"unstructured": "WHO COVID-19 dashboard. [online] world health organization"
},
{
"key": "B57",
"unstructured": "WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020 World Health Organization2020"
},
{
"DOI": "10.1096/fj.202000782",
"article-title": "Angiotensin-converting enzyme 2 in severe acute respiratory syndrome coronavirus and SARS-CoV-2: A double-edged sword?",
"author": "Yan",
"doi-asserted-by": "publisher",
"first-page": "6017",
"journal-title": "FASEB J.",
"key": "B58",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.1177/17534666211025221",
"article-title": "Does pre-existent physical inactivity have a role in the severity of COVID-19?",
"author": "Yuan",
"doi-asserted-by": "publisher",
"first-page": "17534666211025221",
"journal-title": "Ther. Adv. Respir. Dis.",
"key": "B59",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1161/circresaha.120.317134",
"article-title": "Association of inpatient use of angiotensin converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "1671",
"journal-title": "Circ. Res.",
"key": "B60",
"volume": "126",
"year": "2020"
}
],
"reference-count": 60,
"references-count": 60,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fphys.2022.1030568/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Physiology (medical)",
"Physiology"
],
"subtitle": [],
"title": "Effects of physical activity on the severity of illness and mortality in COVID-19 patients: A systematic review and meta-analysis",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "13"
}
