Association between physical activity and risk of COVID-19 infection or clinical outcomes of the patients with COVID-19; A systematic review and meta-analysis
et al., Journal of Preventive Medicine and Hygiene, doi:10.15167/2421-4248/jpmh2023.64.2.2625, PROSPERO CRD42021291451, Aug 2023
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Systematic review and meta analysis showing significantly lower COVID-19 mortality and hospitalization with regular physical activity.
6 meta-analyses show significant improvements with exercise for mortality1-5,
ICU admission1,
hospitalization1,2,5,6 ,
severity2-4, and
cases2.
Currently there are 68 exercise for COVID-19 studies, showing 48% lower mortality [38‑57%], 46% lower ventilation [32‑57%], 41% lower ICU admission [35‑47%], 33% lower hospitalization [25‑40%], and 23% fewer cases [14‑31%].
|
risk of death, 39.0% lower, OR 0.61, p < 0.001, RR approximated with OR.
|
|
risk of hospitalization, 46.0% lower, OR 0.54, p < 0.001, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Rahmati et al., Baseline physical activity is associated with reduced mortality and disease outcomes in COVID-19: A systematic review and meta-analysis, Reviews in Medical Virology, doi:10.1002/rmv.2349.
2.
Ezzatvar et al., Physical activity and risk of infection, severity and mortality of COVID-19: a systematic review and non-linear dose–response meta-analysis of data from 1 853 610 adults, British Journal of Sports Medicine, doi:10.1136/bjsports-2022-105733.
3.
Sittichai et al., Effects of physical activity on the severity of illness and mortality in COVID-19 patients: A systematic review and meta-analysis, Frontiers in Physiology, doi:10.3389/fphys.2022.1030568.
4.
Liu et al., Baseline physical activity and the risk of severe illness and mortality from COVID-19: A dose–response meta-analysis, Preventive Medicine Reports, doi:10.1016/j.pmedr.2023.102130.
Halabchi et al., 1 Aug 2023, peer-reviewed, 5 authors, trial PROSPERO CRD42021291451.
Abstract: J PREV MED HYG 2023; 64: E123-E136
OPEN ACCESS
COVID-19
Association between physical activity
and risk of COVID‑19 infection or clinical outcomes
of the patients with COVID‑19:
A systematic review and meta-analysis
FARZIN HALABCHI1, BEHNAZ MAHDAVIANI2, BEHNAZ TAZESH2, SAKINEH SHAB-BIDAR3,
MARYAM SELK-GHAFFARI2*
1
Department of Sports and Exercise Medicine, Imam Khomeini Hospital Complex, Tehran University of Medical Sciences, Tehran, Iran;
2
Sports Medicine Research Center, Neuroscience Institute, Tehran University of Medical Sciences, Tehran, Iran;
3
Department of Community Nutrition, School of Nutritional Sciences and Dietetics, Tehran University of Medical Sciences, Tehran, Iran
Keywords
Exercise • COVID‑19 • SARS-CoV-2 • Systematic Review • Meta-analysis
Summary
Objective. The COVID‑19 pandemic has caused serious conse‑
quences for global health and economy. The important question
is whether the level of physical activity might influence the risk of
COVID‑19 incidence or clinical outcomes, including the severity
or mortality of infected patients. The objective of this systematic
review and meta-analysis is to evaluate the association between
sufficient physical activity and incidence, hospitalization, sever‑
ity, recovery, and mortality of COVID‑19.
Methods. A systematic search of Web of Sciences, PubMed, and
Scopus between December 2019 and November 2021 was con‑
ducted. Studies were screened based on the inclusion criteria, i.e.
observational studies (case-control, prospective or retrospective
longitudinal designs, and cross-sectional studies) which have
determined the association of physical activity, exercise, sports
participation, or sedentary behavior with COVID‑19 incidence
or outcomes, including mortality, severity, recovery and hospi‑
talization in healthy population or population with any specific
comorbidity.
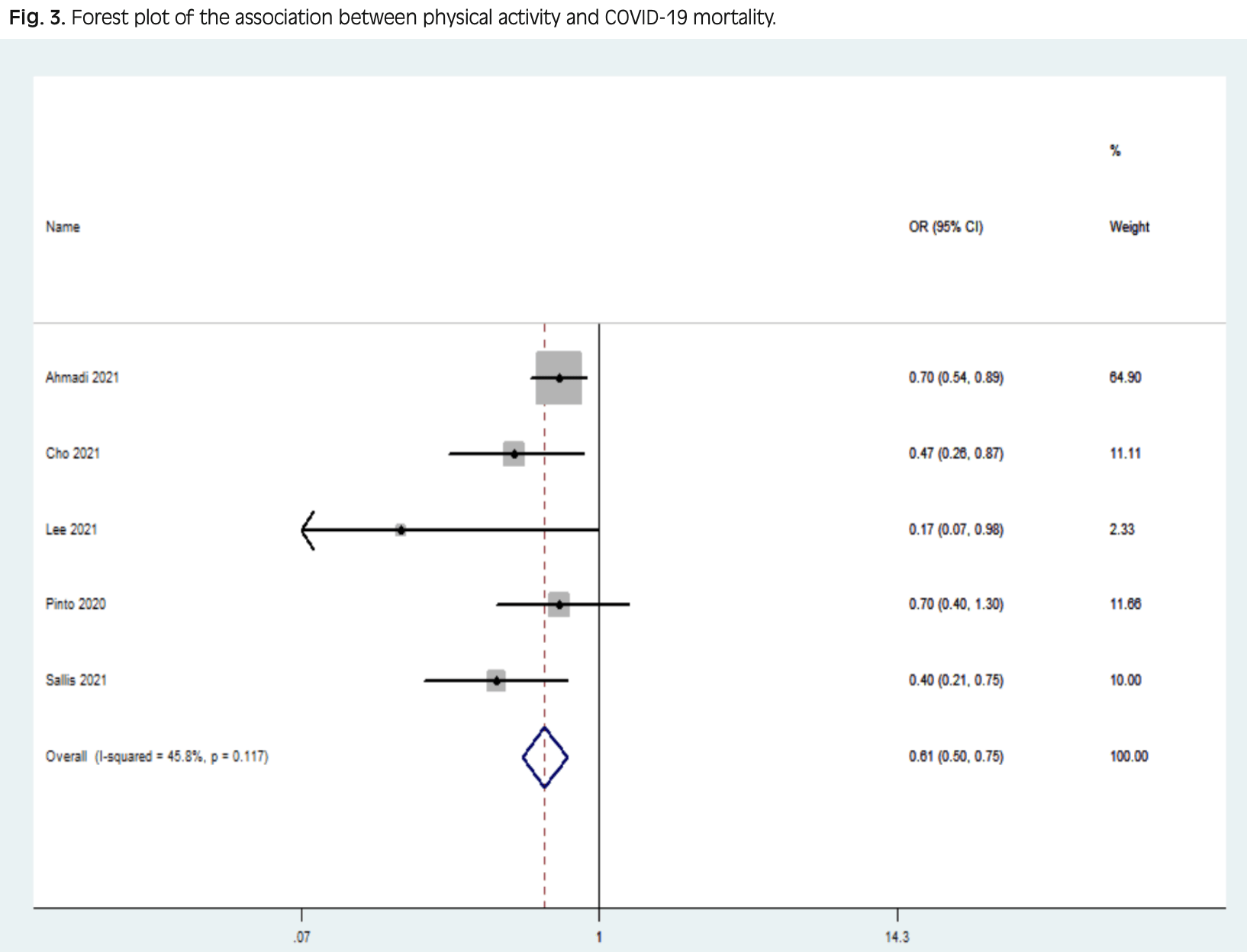
Results. Based on eligibility criteria, 27 articles were finally
included in the qualitative synthesis. The meta-analysis of
five studies evaluating the association of physical activity and
COVID‑19 mortality showed a weighted OR of OR of 0.61
(CI 95%: 0.50‑0.75) with heterogeneity (I2 = 45.8%, P < 0.001)
and in seven studies regarding physical activity and COVID‑19
hospitalization, weighted OR was 0.541 (CI 95%: 0.491-0.595)
with heterogeneity (I2 = 81.7%, P < 0.001).
Conclusion. Participating in sufficient physical activity might
decrease COVID‑19 related COVID‑19-related hospitalization
and mortality. Developing programs to increase physical activity
during the COVID‑19 pandemic might be an appropriate health
strategy.
DOI record:
{
"DOI": "10.15167/2421-4248/JPMH2023.64.2.2625",
"URL": "https://www.jpmh.org/index.php/jpmh/article/view/2625",
"abstract": "Objective: Nowadays, the COVID-19 pandemic has caused serious consequences for global health and economy. The important question is whether the level of physical activity might influence the risk of COVID-19 incidence or clinical outcomes, including the severity or mortality of infected patients. The objective of this systematic review and meta-analysis is to evaluate the association between sufficient physical activity and incidence, hospitalization, severity, recovery, and mortality of COVID-19. Methods: A systematic search of Web of Sciences, PubMed, and Scopus between December 2019 and November 2021 in English language was conducted. Studies were screened based on the inclusion criteria, i.e. observational studies (case-control, prospective or retrospective longitudinal designs, and cross-sectional studies) which have determined the association of physical activity, exercise, sports participation, or sedentary behavior with COVID-19 incidence or outcomes, including mortality, severity, recovery and hospitalization in healthy population or population with any specific comorbidity. Results: Based on eligibility criteria, 27 articles were finally included in the qualitative synthesis. The meta-analysis of five studies evaluating association of physical activity and COVID-19 mortality showed weighted OR of OR of 0.61 (CI 95%: 0.50- 0.75) with heterogeneity (I2= 45.8%, P<0.001) and in seven studies regarding physical activity and COVID-19 hospitalization, weighted OR was 0.541 (CI 95% :0.491 -0.595) with heterogeneity (I2=81.7%, P<0.001). Conclusion: Participating in sufficient physical activity might decrease COVID-19 related hospitalization and mortality. Developing programs to increase physical activity during the COVID-19 pandemic might be an appropriate health strategy.",
"author": [
{
"family": "Halabchi",
"given": "Farzin"
},
{
"family": "Mahdaviani",
"given": "Behnaz"
},
{
"family": "Tazesh",
"given": "Behnaz"
},
{
"family": "Shab-Bidar",
"given": "Sakineh"
},
{
"family": "Selk-Ghaffari",
"given": "Maryam"
}
],
"categories": [
"Exercise, COVID-19, SARS-CoV-2, Systematic Review, Meta-Analysis",
"A systematic review and meta-analysis"
],
"container-title": "Journal of Preventive Medicine and Hygiene",
"id": "https://doi.org/10.15167/2421-4248/jpmh2023.64.2.2625",
"issued": {
"date-parts": [
[
2023,
8,
1
]
]
},
"language": "en",
"page": "Vol. 64 No. 2 (2023): Vol. 64 No. 2 (2023)",
"publisher": "Journal of Preventive Medicine and Hygiene",
"title": "Association between physical activity and risk of COVID-19 infection or clinical outcomes of the patients with COVID-19; A systematic review and meta-analysis",
"type": "article-journal"
}
