Baseline physical activity and the risk of severe illness and mortality from COVID-19: A dose–response meta-analysis
et al., Preventive Medicine Reports, doi:10.1016/j.pmedr.2023.102130, Feb 2023
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
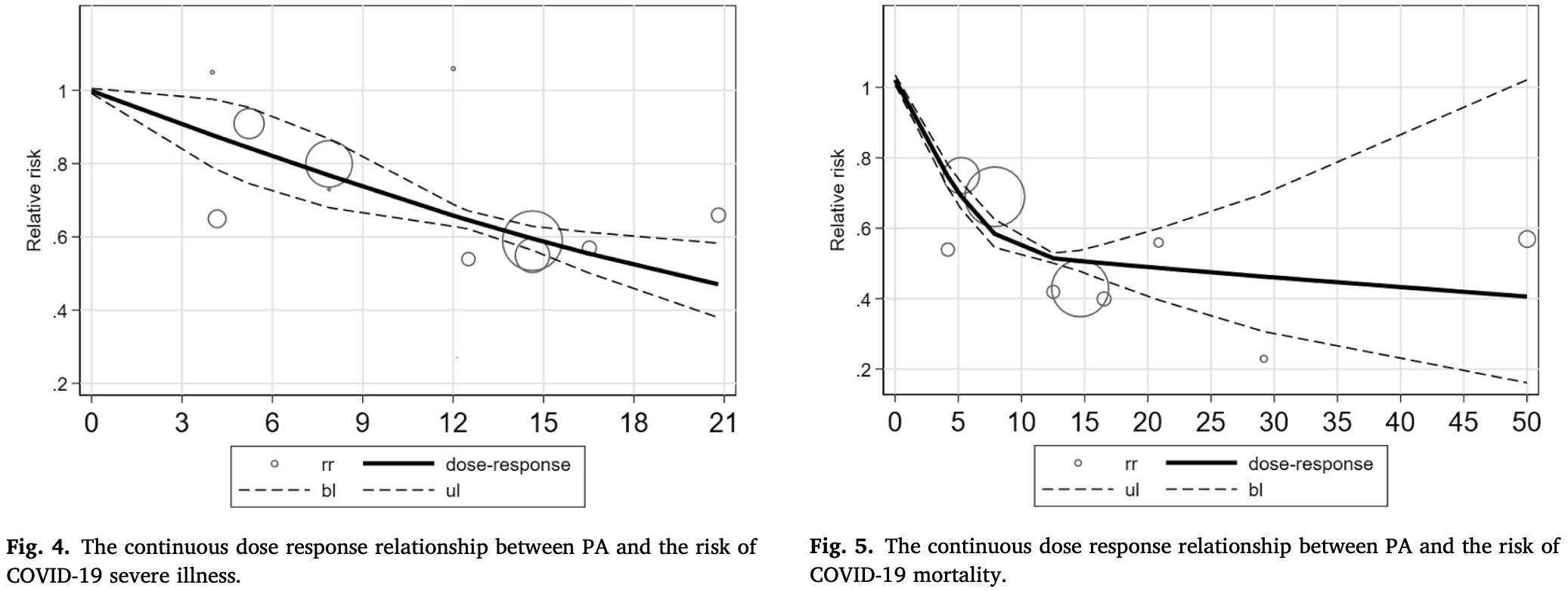
Meta analysis of 14 studies showing a negative dose-response relationship between the level of physical activity and COVID-19 severity and mortality.
6 meta-analyses show significant improvements with exercise for mortality1-5,
ICU admission1,
hospitalization1,2,5,6 ,
severity2-4, and
cases2.
Currently there are 68 exercise for COVID-19 studies, showing 48% lower mortality [38‑57%], 46% lower ventilation [32‑57%], 41% lower ICU admission [35‑47%], 33% lower hospitalization [25‑40%], and 23% fewer cases [14‑31%].
1.
Rahmati et al., Baseline physical activity is associated with reduced mortality and disease outcomes in COVID-19: A systematic review and meta-analysis, Reviews in Medical Virology, doi:10.1002/rmv.2349.
2.
Ezzatvar et al., Physical activity and risk of infection, severity and mortality of COVID-19: a systematic review and non-linear dose–response meta-analysis of data from 1 853 610 adults, British Journal of Sports Medicine, doi:10.1136/bjsports-2022-105733.
3.
Sittichai et al., Effects of physical activity on the severity of illness and mortality in COVID-19 patients: A systematic review and meta-analysis, Frontiers in Physiology, doi:10.3389/fphys.2022.1030568.
4.
Liu et al., Baseline physical activity and the risk of severe illness and mortality from COVID-19: A dose–response meta-analysis, Preventive Medicine Reports, doi:10.1016/j.pmedr.2023.102130.
Liu et al., 11 Feb 2023, peer-reviewed, 3 authors.
Contact: songtaozhenzhen@sina.com.
Baseline physical activity and the risk of severe illness and mortality from COVID-19: A dose–response meta-analysis
Preventive Medicine Reports, doi:10.1016/j.pmedr.2023.102130
To provide a scientific basis for improved exercise-based immunity, a meta-analysis was used to explore the dose-response relationship between physical activity (PA) and the risk of severe illness and mortality related to COVID-19 (coronavirus disease 2019). To this end, we searched PubMed, Web of Science databases from January 2020 through April 2022. 14 observational studies met the criteria for inclusion in the meta-analysis, including 2840 cases of severe illness and death from COVID-19. Categorical dose-relationship analysis showed that the risks of severe illness and mortality from COVID-19 were, respectively, 46% (risk ratio (RR): 0.54; confidence intervals (CIs): 0.41-0.68) and 59% (RR = 0.41; 95%CI: 0.23-0.58) lower for the highest dose of PA compared with the lowest dose of PA. The results of the continuous dose-response analysis show an inverse nonlinear relationship (P non-linearity < 0.05) between PA and both the risk of severe illness and mortality from COVID-19. For PA below 10 MET-h/week (MET-h/week: metabolic equivalent of task-hours/week), an increase of 4 MET-h/ week (1 h of moderate-intensity or 0.5 h of high-intensity PA) was associated with 8% and 11% reductions in the risk of severe illness and mortality from COVID-19. PA above 10 MET-h/week lowered the risk of severe illness and mortality from COVID-19 by 7% and 9%, respectively, for each 4 MET-h/week increase. Doses of WHOrecommended PA levels (10 MET-h/week) may be required for more substantial reductions in the risk of severe illness and mortality from COVID-19.
Appendix A. Supplementary data Supplementary data to this article can be found online at https://doi. org/10.1016/j.pmedr.2023.102130.
References
Ahmadi, Huang, Inan-Eroglu, Lifestyle risk factors and infectious disease mortality, including COVID-19, among middle aged and older adults: Evidence from a community-based cohort study in the United Kingdom, Brain Behav. Immun
Ainsworth, Haskell, Herrmann, Compendium of Physical Activities: a second update of codes and MET values, Med. Sci. Sports Exerc
Bakker, Lee, Hopman, Oymans, Watson et al., Dose-response association between moderate to vigorous physical activity and incident morbidity and mortality for individuals with a different cardiovascular health status: A cohort study among 142,493 adults from the Netherlands, PLoS Med, doi:10.1371/journal.pmed.1003845
Baynouna Alketbi, Nagelkerke, Abdelbaqi, Risk Factors for SARS-CoV-2 Infection Severity in Abu Dhabi, J Epidemiol Glob Health
Benson, Akbarian, Adler, Hemodynamic effects of pneumonia. I. Normal and hypodynamic responses, J. Clin. Invest
Bizuti, Starck, Da Silva Fagundes, Influence of exercise and vitamin D on the immune system against Covid-19: an integrative review of current literature, Mol. Cell. Biochem
Brandenburg, Lesser, Thomson, Does higher self-reported cardiorespiratory fitness reduce the odds of hospitalization from COVID-19?, J. Phys. Act. Health, doi:10.1123/jpah.2020-0817
Chastin, Abaraogu, Bourgois, disease in the general population: systematic review and meta-analysis, doi:10.2139/ssrn.3673184
Cho, Lee, Jae, Physical activity and the risk of COVID-19 infection and mortality: a nationwide population-based case-control study, J. Clin. Med
Collaborators, Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study, Lancet
Corrales-Medina, Musher, Wells, Cardiac complications in patients with community-acquired pneumonia: incidence, timing, risk factors, and association with short-term mortality, Circulation
Corrales-Medina, Suh, Rose, Cardiac complications in patients with community-acquired pneumonia: a systematic review and meta-analysis of observational studies, PLoS Med
Da Silveira, Da Silva Fagundes, Bizuti, Physical exercise as a tool to help the immune system against COVID-19: an integrative review of the current literature, Clin. Exp. Med
Ekblom-Bak, Väisänen, Ekblom, Blom, Kallings et al., Cardiorespiratory fitness and lifestyle on severe COVID-19 risk in 279,455 adults: a case control study, Int. J. Behav. Nutr. Phys. Act, doi:10.1186/s12966-021-01198-5
Ekelund, Tarp, Steene-Johannessen, Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: systematic review and harmonised meta-analysis, BMJ, doi:10.1136/bmj.l4570
Geidl, Schlesinger, Mino, Miranda, Pfeifer, Dose-response relationship between physical activity and mortality in adults with noncommunicable diseases: a systematic review and meta-analysis of prospective observational studies, Int. J. Behav. Nutr. Phys. Act, doi:10.1186/s12966-020-01007-5
Haas, Angulo, Mclaughlin, Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalizations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data, Lancet, doi:10.1016/s0140-6736(21)00947-8
Halabchi, Mazaheri, Sabeti, Yunesian, Alizadeh et al., Regular sports participation as a potential predictor of better clinical outcome in adult patients with COVID-19: A large cross-sectional study, J. Phys. Act. Health
Hamrouni, Roberts, Thackray, Stensel, Bishop, Associations of obesity, physical activity level, inflammation and cardiometabolic health with COVID-19 mortality: a prospective analysis of the UK Biobank cohort, BMJ Open
Higgins, Green, Cochrane handbook for systematic reviews of interventions
Katsoulis, Pasea, Lai, Dobson, Denaxas et al., Obesity during the COVID-19 pandemic: both cause of high risk and potential effect of lockdown? A population-based electronic health record study, Public Health
Kimura, Shimizu, Akama, Akimoto, Kuno et al., The effects of walking exercise training on immune response in elderly subjects, Internat. J. Sport Health Sci
Kunutsor, Seidu, Laukkanen, Physical activity reduces the risk of pneumonia: systematic review and meta-analysis of 10 prospective studies involving 1,044,492 participants, Geroscience, doi:10.1007/s11357-021-00491-2
Kyu, Bachman, Alexander, Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the Global Burden of Disease Study, BMJ, doi:10.1136/bmj.i3857
Lee, Lee, Moon, Jin, Yang et al., Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study, Br. J. Sports Med
Lee, Shiroma, Lobelo, Puska, Blair et al., Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy, Lancet
Lu, Liu, Li, Leisure time physical activity and risk of pneumonia mortality: a dose-response meta-analysis, J. Sports Med. Phys. Fitness, doi:10.23736/s0022-4707.21.12017-1
Nieman, Nehlsen-Cannarella, Markoff, Balk-Lamberton, Yang et al., The effects of moderate exercise training on natural killer cells and acute upper respiratory tract infections, Int. J. Sports Med
Page, Mckenzie, Bossuyt, The PRISMA 2020 statement: An updated guideline for reporting systematic reviews, J. Clin. Epidemiol
Piercy, Troiano, Ballard, The physical activity guidelines for Americans, J. Am. Med. Assoc
Pinto, Goessler, Fernandes, Murai, Sales et al., No independent associations between physical activity and clinical outcomes among hospitalized patients with moderate to severe COVID-19, J. Sport Health Sci
Rahmati, Shamsi, Khoramipour, Malakoutinia, Woo et al., Baseline physical activity is associated with reduced mortality and disease outcomes in COVID-19: A systematic review and meta-analysis, Rev. Med. Virol, doi:10.1002/rmv.2349
Rowlands, Kloecker, Chudasama, Association of timing and balance of physical activity and rest/sleep with risk of COVID-19: A UK Biobank Study, Mayo Clin. Proc
Salgado-Aranda, Pérez-Castellano, Núñez-Gil, Influence of Baseline Physical Activity as a Modifying Factor on COVID-19 Mortality: A Single-Center. Retrospective Study, Infect Dis Ther
Sallis, Young, Tartof, Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients, Br. J. Sports Med
Shephard, Rhind, Shek, The impact of exercise on the immune system: NK cells, interleukins 1 and 2, and related responses, Exerc. Sport Sci. Rev
Shephard, Shek, Cancer, immune function, and physical activity, Can. J. Appl. Physiol. = Revue canadienne de physiologie appliquee
Stamatakis, Ding, Ekelund, Bauman, Sliding down the risk factor rankings: reasons for and consequences of the dramatic downgrading of physical activity in the Global Burden of Disease 2019, Br. J. Sports Med
Steenkamp, Saggers, Bandini, Small steps, strong shield: directly measured, moderate physical activity in 65 361 adults is associated with significant protective effects from severe COVID-19 outcomes, Br. J. Sports Med
Tavakol, Ghannadi, Tabesh, Halabchi, Noormohammadpour et al., Relationship between physical activity, healthy lifestyle and COVID-19 disease severity; a cross-sectional study, Z Gesundh Wiss
Wells, Peterson, Welch, The Newcastle-Ottawa scale (NOS) for assessing the quality in nonrandomized studies in meta-analyses
Williams, Dose-response relationship between exercise and respiratory disease mortality, Med. Sci. Sports Exerc, doi:10.1249/mss.0000000000000142
Wunsch, Kienberger, Niessner, Changes in Physical Activity Patterns Due to the Covid-19 Pandemic: A Systematic Review and Meta-Analysis, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph19042250
Xu, Doi, The robust error meta-regression method for dose-response metaanalysis, Int. J. Evid. Based Healthc, doi:10.1097/xeb.0000000000000132
Yuan, Huang, Chen, Chen, Zhang et al., Does pre-existent physical inactivity have a role in the severity of COVID-19?, Ther. Adv. Respir. Dis, doi:10.1177/17534666211025221
Zbinden-Foncea, Francaux, Deldicque, Hawley, Does high cardiorespiratory fitness confer some protection against proinflammatory responses after infection by SARS-CoV-2?, Obesity
Zhang, Dong, Zhou, The advanced meta-analysis method-based on stata
DOI record:
{
"DOI": "10.1016/j.pmedr.2023.102130",
"ISSN": [
"2211-3355"
],
"URL": "http://dx.doi.org/10.1016/j.pmedr.2023.102130",
"alternative-id": [
"S2211335523000219"
],
"article-number": "102130",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Baseline physical activity and the risk of severe illness and mortality from COVID-19: A dose–response meta-analysis"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Preventive Medicine Reports"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.pmedr.2023.102130"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2023 The Author(s). Published by Elsevier Inc."
}
],
"author": [
{
"affiliation": [],
"family": "Liu",
"given": "Junjie",
"sequence": "first"
},
{
"affiliation": [],
"family": "Guo",
"given": "Zhiguang",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4549-9496",
"affiliation": [],
"authenticated-orcid": false,
"family": "Lu",
"given": "Songtao",
"sequence": "additional"
}
],
"container-title": "Preventive Medicine Reports",
"container-title-short": "Preventive Medicine Reports",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2023,
2,
8
]
],
"date-time": "2023-02-08T07:48:13Z",
"timestamp": 1675842493000
},
"deposited": {
"date-parts": [
[
2023,
2,
11
]
],
"date-time": "2023-02-11T22:52:00Z",
"timestamp": 1676155920000
},
"indexed": {
"date-parts": [
[
2023,
2,
12
]
],
"date-time": "2023-02-12T05:30:02Z",
"timestamp": 1676179802354
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
4
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
4,
1
]
],
"date-time": "2023-04-01T00:00:00Z",
"timestamp": 1680307200000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
2,
6
]
],
"date-time": "2023-02-06T00:00:00Z",
"timestamp": 1675641600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S2211335523000219?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S2211335523000219?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "102130",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2023,
4
]
]
},
"published-print": {
"date-parts": [
[
2023,
4
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1016/j.bbi.2021.04.022",
"article-title": "Lifestyle risk factors and infectious disease mortality, including COVID-19, among middle aged and older adults: Evidence from a community-based cohort study in the United Kingdom",
"author": "Ahmadi",
"doi-asserted-by": "crossref",
"first-page": "18",
"journal-title": "Brain Behav. Immun.",
"key": "10.1016/j.pmedr.2023.102130_b0005",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1249/MSS.0b013e31821ece12",
"article-title": "2011 Compendium of Physical Activities: a second update of codes and MET values",
"author": "Ainsworth",
"doi-asserted-by": "crossref",
"first-page": "1575",
"issue": "8",
"journal-title": "Med. Sci. Sports Exerc.",
"key": "10.1016/j.pmedr.2023.102130_b0010",
"volume": "43",
"year": "2011"
},
{
"DOI": "10.1371/journal.pmed.1003845",
"article-title": "Dose-response association between moderate to vigorous physical activity and incident morbidity and mortality for individuals with a different cardiovascular health status: A cohort study among 142,493 adults from the Netherlands",
"author": "Bakker",
"doi-asserted-by": "crossref",
"issue": "12",
"journal-title": "PLoS Med.",
"key": "10.1016/j.pmedr.2023.102130_b0015",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1007/s44197-021-00006-4",
"article-title": "Risk Factors for SARS-CoV-2 Infection Severity in Abu Dhabi",
"author": "Baynouna AlKetbi",
"doi-asserted-by": "crossref",
"first-page": "344",
"issue": "4",
"journal-title": "J Epidemiol Glob Health",
"key": "10.1016/j.pmedr.2023.102130_b0020",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1172/JCI106292",
"article-title": "Hemodynamic effects of pneumonia. I. Normal and hypodynamic responses",
"author": "Benson",
"doi-asserted-by": "crossref",
"first-page": "791",
"issue": "4",
"journal-title": "J. Clin. Invest.",
"key": "10.1016/j.pmedr.2023.102130_b0025",
"volume": "49",
"year": "1970"
},
{
"DOI": "10.1007/s11010-022-04402-7",
"article-title": "Influence of exercise and vitamin D on the immune system against Covid-19: an integrative review of current literature",
"author": "Bizuti",
"doi-asserted-by": "crossref",
"first-page": "1725",
"issue": "6",
"journal-title": "Mol. Cell. Biochem.",
"key": "10.1016/j.pmedr.2023.102130_b0030",
"volume": "477",
"year": "2022"
},
{
"DOI": "10.1123/jpah.2020-0817",
"article-title": "Does higher self-reported cardiorespiratory fitness reduce the odds of hospitalization from COVID-19?",
"author": "Brandenburg",
"doi-asserted-by": "crossref",
"first-page": "782",
"issue": "7",
"journal-title": "J. Phys. Act. Health",
"key": "10.1016/j.pmedr.2023.102130_b0035",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.2139/ssrn.3673184",
"article-title": "Physical activity, immune function and risk of community acquired infectious disease in the general population: systematic review and meta-analysis",
"author": "Chastin",
"doi-asserted-by": "crossref",
"journal-title": "SSRN Electron. J.",
"key": "10.1016/j.pmedr.2023.102130_b0040",
"year": "2020"
},
{
"DOI": "10.3390/jcm10071539",
"article-title": "Physical activity and the risk of COVID-19 infection and mortality: a nationwide population-based case-control study",
"author": "Cho",
"doi-asserted-by": "crossref",
"first-page": "1539",
"issue": "7",
"journal-title": "J. Clin. Med.",
"key": "10.1016/j.pmedr.2023.102130_b0045",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(20)30752-2",
"article-title": "Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019",
"author": "Collaborators",
"doi-asserted-by": "crossref",
"first-page": "1223",
"issue": "10258",
"journal-title": "Lancet (London, England)",
"key": "10.1016/j.pmedr.2023.102130_b0050",
"volume": "396",
"year": "2020"
},
{
"DOI": "10.1371/journal.pmed.1001048",
"article-title": "Cardiac complications in patients with community-acquired pneumonia: a systematic review and meta-analysis of observational studies",
"author": "Corrales-Medina",
"doi-asserted-by": "crossref",
"first-page": "e1001048",
"issue": "6",
"journal-title": "PLoS Med.",
"key": "10.1016/j.pmedr.2023.102130_b0055",
"volume": "8",
"year": "2011"
},
{
"DOI": "10.1161/CIRCULATIONAHA.111.040766",
"article-title": "Cardiac complications in patients with community-acquired pneumonia: incidence, timing, risk factors, and association with short-term mortality",
"author": "Corrales-Medina",
"doi-asserted-by": "crossref",
"first-page": "773",
"issue": "6",
"journal-title": "Circulation",
"key": "10.1016/j.pmedr.2023.102130_b0060",
"volume": "125",
"year": "2012"
},
{
"DOI": "10.1007/s10238-020-00650-3",
"article-title": "Physical exercise as a tool to help the immune system against COVID-19: an integrative review of the current literature",
"author": "da Silveira",
"doi-asserted-by": "crossref",
"first-page": "15",
"issue": "1",
"journal-title": "Clin. Exp. Med.",
"key": "10.1016/j.pmedr.2023.102130_b0065",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1186/s12966-021-01198-5",
"article-title": "Cardiorespiratory fitness and lifestyle on severe COVID-19 risk in 279,455 adults: a case control study",
"author": "Ekblom-Bak",
"doi-asserted-by": "crossref",
"issue": "1",
"journal-title": "Int. J. Behav. Nutr. Phys. Act.",
"key": "10.1016/j.pmedr.2023.102130_b0070",
"volume": "18",
"year": "2021"
},
{
"article-title": "Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: systematic review and harmonised meta-analysis",
"author": "Ekelund",
"journal-title": "BMJ",
"key": "10.1016/j.pmedr.2023.102130_b0075",
"volume": "366",
"year": "2019"
},
{
"DOI": "10.1186/s12966-020-01007-5",
"article-title": "Dose-response relationship between physical activity and mortality in adults with noncommunicable diseases: a systematic review and meta-analysis of prospective observational studies",
"author": "Geidl",
"doi-asserted-by": "crossref",
"first-page": "109",
"issue": "1",
"journal-title": "Int. J. Behav. Nutr. Phys. Act.",
"key": "10.1016/j.pmedr.2023.102130_b0080",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(21)00947-8",
"article-title": "Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalizations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data",
"author": "Haas",
"doi-asserted-by": "crossref",
"first-page": "1819",
"issue": "10287",
"journal-title": "Lancet",
"key": "10.1016/j.pmedr.2023.102130_b0085",
"volume": "397",
"year": "2021"
},
{
"DOI": "10.1123/jpah.2020-0392",
"article-title": "Regular sports participation as a potential predictor of better clinical outcome in adult patients with COVID-19: A large cross-sectional study",
"author": "Halabchi",
"doi-asserted-by": "crossref",
"first-page": "8",
"issue": "1",
"journal-title": "J. Phys. Act. Health",
"key": "10.1016/j.pmedr.2023.102130_b0090",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1136/bmjopen-2021-055003",
"article-title": "Associations of obesity, physical activity level, inflammation and cardiometabolic health with COVID-19 mortality: a prospective analysis of the UK Biobank cohort",
"author": "Hamrouni",
"doi-asserted-by": "crossref",
"first-page": "e055003",
"issue": "11",
"journal-title": "BMJ Open",
"key": "10.1016/j.pmedr.2023.102130_b0095",
"volume": "11",
"year": "2021"
},
{
"article-title": "Cochrane handbook for systematic reviews of interventions",
"author": "Higgins",
"key": "10.1016/j.pmedr.2023.102130_b0100",
"series-title": "New Jerse: A Version 5.1.0",
"year": "2011"
},
{
"DOI": "10.1016/j.puhe.2020.12.003",
"article-title": "Obesity during the COVID-19 pandemic: both cause of high risk and potential effect of lockdown? A population-based electronic health record study",
"author": "Katsoulis",
"doi-asserted-by": "crossref",
"first-page": "41",
"journal-title": "Public Health",
"key": "10.1016/j.pmedr.2023.102130_b0105",
"volume": "191",
"year": "2021"
},
{
"DOI": "10.5432/ijshs.4.508",
"article-title": "The effects of walking exercise training on immune response in elderly subjects",
"author": "Kimura",
"doi-asserted-by": "crossref",
"first-page": "508",
"journal-title": "Internat. J. Sport Health Sci.",
"key": "10.1016/j.pmedr.2023.102130_b0115",
"volume": "4",
"year": "2006"
},
{
"DOI": "10.1007/s11357-021-00491-2",
"article-title": "Physical activity reduces the risk of pneumonia: systematic review and meta-analysis of 10 prospective studies involving 1,044,492 participants",
"author": "Kunutsor",
"doi-asserted-by": "crossref",
"first-page": "519",
"issue": "1",
"journal-title": "Geroscience",
"key": "10.1016/j.pmedr.2023.102130_b0120",
"volume": "44",
"year": "2022"
},
{
"article-title": "Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013",
"author": "Kyu",
"journal-title": "BMJ",
"key": "10.1016/j.pmedr.2023.102130_b0125",
"volume": "354",
"year": "2016"
},
{
"DOI": "10.1136/bjsports-2021-104203",
"article-title": "Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "901",
"issue": "16",
"journal-title": "Br. J. Sports Med.",
"key": "10.1016/j.pmedr.2023.102130_b0135",
"volume": "56",
"year": "2022"
},
{
"DOI": "10.1016/S0140-6736(12)61031-9",
"article-title": "Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "219",
"issue": "9838",
"journal-title": "Lancet",
"key": "10.1016/j.pmedr.2023.102130_b0140",
"volume": "380",
"year": "2012"
},
{
"DOI": "10.23736/S0022-4707.21.12017-1",
"article-title": "Leisure time physical activity and risk of pneumonia mortality: a dose-response meta-analysis",
"author": "Lu",
"doi-asserted-by": "crossref",
"first-page": "547",
"issue": "4",
"journal-title": "J. Sports Med. Phys. Fitness",
"key": "10.1016/j.pmedr.2023.102130_b0145",
"volume": "62",
"year": "2022"
},
{
"DOI": "10.1055/s-2007-1024839",
"article-title": "The effects of moderate exercise training on natural killer cells and acute upper respiratory tract infections",
"author": "Nieman",
"doi-asserted-by": "crossref",
"first-page": "467",
"issue": "06",
"journal-title": "Int. J. Sports Med.",
"key": "10.1016/j.pmedr.2023.102130_b0150",
"volume": "11",
"year": "1990"
},
{
"DOI": "10.1016/j.jclinepi.2021.03.001",
"article-title": "The PRISMA 2020 statement: An updated guideline for reporting systematic reviews",
"author": "Page",
"doi-asserted-by": "crossref",
"first-page": "178",
"journal-title": "J. Clin. Epidemiol.",
"key": "10.1016/j.pmedr.2023.102130_b0155",
"volume": "134",
"year": "2021"
},
{
"DOI": "10.1001/jama.2018.14854",
"article-title": "The physical activity guidelines for Americans",
"author": "Piercy",
"doi-asserted-by": "crossref",
"first-page": "2020",
"issue": "19",
"journal-title": "J. Am. Med. Assoc.",
"key": "10.1016/j.pmedr.2023.102130_b0160",
"volume": "320",
"year": "2020"
},
{
"DOI": "10.1016/j.jshs.2021.08.001",
"article-title": "No independent associations between physical activity and clinical outcomes among hospitalized patients with moderate to severe COVID-19",
"author": "Pinto",
"doi-asserted-by": "crossref",
"first-page": "690",
"issue": "6",
"journal-title": "J. Sport Health Sci.",
"key": "10.1016/j.pmedr.2023.102130_b0165",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1002/rmv.2349",
"article-title": "Baseline physical activity is associated with reduced mortality and disease outcomes in COVID-19: A systematic review and meta-analysis",
"author": "Rahmati",
"doi-asserted-by": "crossref",
"issue": "5",
"journal-title": "Rev. Med. Virol.",
"key": "10.1016/j.pmedr.2023.102130_b0170",
"volume": "32",
"year": "2022"
},
{
"DOI": "10.1016/j.mayocp.2020.10.032",
"article-title": "Association of timing and balance of physical activity and rest/sleep with risk of COVID-19: A UK Biobank Study",
"author": "Rowlands",
"doi-asserted-by": "crossref",
"first-page": "156",
"issue": "1",
"journal-title": "Mayo Clin. Proc.",
"key": "10.1016/j.pmedr.2023.102130_b0175",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1007/s40121-021-00418-6",
"article-title": "Influence of Baseline Physical Activity as a Modifying Factor on COVID-19 Mortality: A Single-Center",
"author": "Salgado-Aranda",
"doi-asserted-by": "crossref",
"first-page": "801",
"issue": "2",
"journal-title": "Retrospective Study. Infect Dis Ther",
"key": "10.1016/j.pmedr.2023.102130_b0180",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1136/bjsports-2021-104080",
"article-title": "Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients",
"author": "Sallis",
"doi-asserted-by": "crossref",
"first-page": "1099",
"issue": "19",
"journal-title": "Br. J. Sports Med.",
"key": "10.1016/j.pmedr.2023.102130_b0185",
"volume": "55",
"year": "2021"
},
{
"DOI": "10.1249/00003677-199500230-00009",
"article-title": "The impact of exercise on the immune system: NK cells, interleukins 1 and 2, and related responses",
"author": "Shephard",
"doi-asserted-by": "crossref",
"first-page": "215",
"journal-title": "Exerc. Sport Sci. Rev.",
"key": "10.1016/j.pmedr.2023.102130_b0190",
"volume": "23",
"year": "1995"
},
{
"article-title": "Cancer, immune function, and physical activity",
"author": "Shephard",
"first-page": "1",
"issue": "1",
"journal-title": "Can. J. Appl. Physiol. = Revue canadienne de physiologie appliquee",
"key": "10.1016/j.pmedr.2023.102130_b0195",
"volume": "20",
"year": "1995"
},
{
"DOI": "10.1136/bjsports-2021-104064",
"article-title": "Sliding down the risk factor rankings: reasons for and consequences of the dramatic downgrading of physical activity in the Global Burden of Disease 2019",
"author": "Stamatakis",
"doi-asserted-by": "crossref",
"first-page": "1222",
"issue": "21",
"journal-title": "Br. J. Sports Med.",
"key": "10.1016/j.pmedr.2023.102130_b0200",
"volume": "55",
"year": "2021"
},
{
"DOI": "10.1136/bjsports-2021-105159",
"article-title": "Small steps, strong shield: directly measured, moderate physical activity in 65 361 adults is associated with significant protective effects from severe COVID-19 outcomes",
"author": "Steenkamp",
"doi-asserted-by": "crossref",
"first-page": "568",
"issue": "10",
"journal-title": "Br. J. Sports Med.",
"key": "10.1016/j.pmedr.2023.102130_b0205",
"volume": "56",
"year": "2022"
},
{
"DOI": "10.1007/s10389-020-01468-9",
"article-title": "Relationship between physical activity, healthy lifestyle and COVID-19 disease severity; a cross-sectional study",
"author": "Tavakol",
"doi-asserted-by": "crossref",
"first-page": "267",
"issue": "2",
"journal-title": "Z Gesundh Wiss",
"key": "10.1016/j.pmedr.2023.102130_b0210",
"volume": "31",
"year": "2021"
},
{
"key": "10.1016/j.pmedr.2023.102130_b0215",
"unstructured": "Wells GA, Peterson J, Welch V, et al., 2009. The Newcastle-Ottawa scale (NOS) for assessing the quality in nonrandomized studies in meta-analyses, Ottawa, University of Ottawa. Available from: http://www. ohri. ca/ programs/ clinical_ epidemiology/ oxford. Asp."
},
{
"DOI": "10.1249/MSS.0000000000000142",
"article-title": "Dose-response relationship between exercise and respiratory disease mortality",
"author": "Williams",
"doi-asserted-by": "crossref",
"first-page": "711",
"issue": "4",
"journal-title": "Med. Sci. Sports Exerc.",
"key": "10.1016/j.pmedr.2023.102130_b0220",
"volume": "46",
"year": "2014"
},
{
"key": "10.1016/j.pmedr.2023.102130_b0225",
"unstructured": "World Health Organization, 2022. Global Recommendations on Physical Activity for Health. [2022-07-15]. https://www.who.int/publications/i/item/9789241599979."
},
{
"key": "10.1016/j.pmedr.2023.102130_b0230",
"unstructured": "World Health Organization, 2022. Coronavirus disease (COVID-19) Numbers at a glance[R/OL]. [2022-07-15]. https://www.who.int/emergencies/diseases/novel-coronavirus-2019."
},
{
"DOI": "10.3390/ijerph19042250",
"article-title": "Changes in Physical Activity Patterns Due to the Covid-19 Pandemic: A Systematic Review and Meta-Analysis",
"author": "Wunsch",
"doi-asserted-by": "crossref",
"issue": "4",
"journal-title": "Int. J. Environ. Res. Public Health",
"key": "10.1016/j.pmedr.2023.102130_b0235",
"volume": "19",
"year": "2022"
},
{
"DOI": "10.1097/XEB.0000000000000132",
"article-title": "The robust error meta-regression method for dose-response meta-analysis",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "138",
"issue": "3",
"journal-title": "Int. J. Evid. Based Healthc.",
"key": "10.1016/j.pmedr.2023.102130_b0240",
"volume": "16",
"year": "2018"
},
{
"DOI": "10.1177/17534666211025221",
"article-title": "Does pre-existent physical inactivity have a role in the severity of COVID-19?",
"author": "Yuan",
"doi-asserted-by": "crossref",
"journal-title": "Ther. Adv. Respir. Dis.",
"key": "10.1016/j.pmedr.2023.102130_b0245",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1002/oby.22849",
"article-title": "Does high cardiorespiratory fitness confer some protection against proinflammatory responses after infection by SARS‐CoV‐2?",
"author": "Zbinden‐Foncea",
"doi-asserted-by": "crossref",
"first-page": "1378",
"issue": "8",
"journal-title": "Obesity",
"key": "10.1016/j.pmedr.2023.102130_b0250",
"volume": "28",
"year": "2020"
},
{
"article-title": "The advanced meta-analysis method-based on stata",
"author": "Zhang",
"first-page": "220",
"journal-title": "Fudan Univ. Press",
"key": "10.1016/j.pmedr.2023.102130_b0255",
"year": "2015"
}
],
"reference-count": 49,
"references-count": 49,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S2211335523000219"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Public Health, Environmental and Occupational Health",
"Epidemiology"
],
"subtitle": [],
"title": "Baseline physical activity and the risk of severe illness and mortality from COVID-19: A dose–response meta-analysis",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "32"
}
