Does Higher Self-Reported Cardiorespiratory Fitness Reduce the Odds of Hospitalization From COVID-19?
et al., Journal of Physical Activity and Health, doi:10.1123/jpah.2020-0817, Jul 2021
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
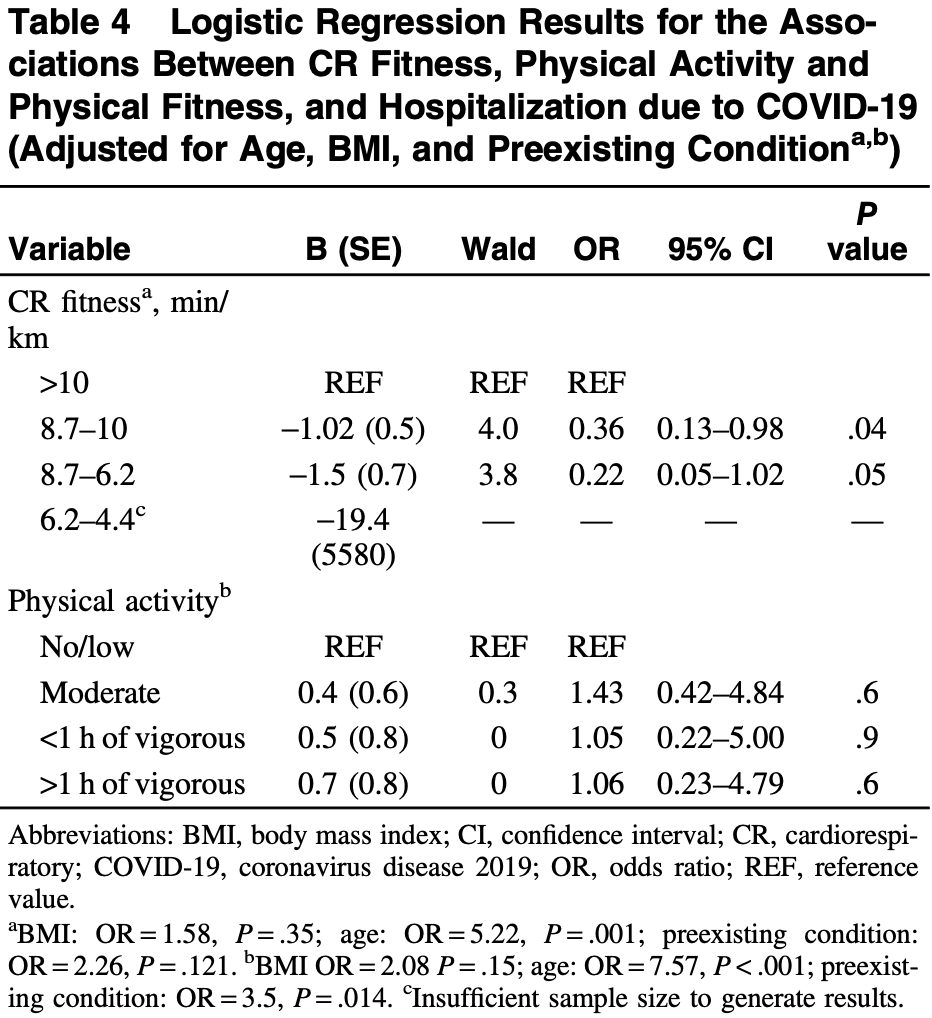
Retrospective 263 COVID+ patients, showing lower hospitalization with higher self-reported cardiorespiratory fitness, but no significant differences for physical activity. Participants in the study were healthier and more fit than the general population.
|
risk of hospitalization, 6.0% higher, OR 1.06, p = 0.60, high activity levels 102, low activity levels 39, adjusted per study, multivariable, PA, >1h vigorous vs. no/low, RR approximated with OR.
|
|
risk of hospitalization, 78.0% lower, OR 0.22, p = 0.05, high activity levels 177, low activity levels 34, adjusted per study, multivariable, CRF, 6.2-8.7 vs. >10, RR approximated with OR.
|
|
risk of hospitalization, 64.0% lower, OR 0.36, p = 0.04, high activity levels 97, low activity levels 34, adjusted per study, multivariable, CRF, 8.7-10 vs. >10, RR approximated with OR.
|
|
risk of severe case, 35.0% lower, OR 0.65, p = 0.30, high activity levels 102, low activity levels 39, adjusted per study, multivariable, PA, >1h vigorous vs. no/low, RR approximated with OR.
|
|
risk of severe case, 24.0% lower, OR 0.76, p = 0.60, high activity levels 52, low activity levels 34, adjusted per study, multivariable, CRF, 4.4-6.2 vs. >10, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Brandenburg et al., 1 Jul 2021, retrospective, multiple countries, peer-reviewed, survey, 4 authors.
Does Higher Self-Reported Cardiorespiratory Fitness Reduce the Odds of Hospitalization From COVID-19?
Journal of Physical Activity and Health, doi:10.1123/jpah.2020-0817
Background: Regular physical activity and higher cardiorespiratory (CR) fitness enhance immune function, possibly reducing coronavirus disease 2019 (COVID-19) infection severity. The aim was to assess the association between physical activity and self-reported CR fitness on COVID-19 infection characteristics. Methods: Participants formerly testing positive for COVID-19 completed an online questionnaire measuring COVID-19 infection characteristics and complications, self-reported CR fitness level, physical activity, and sociodemographic and health-related characteristics. Self-reported CR fitness was determined as the pace to cover 4.8 km without becoming overly fatigued (with slow walking, brisk walking, jogging, and running corresponding to low, moderate, good, and excellent levels of fitness, respectively). Results: A total of 263 individuals completed the survey. Compared with the lowest level of self-reported CR fitness, the odds of hospitalization significantly decreased by 64% (odds ratio = 0.36; 95% confidence interval, 0.13-0.98; P = .04) in individuals reporting the ability to maintain a brisk walk. In individuals reporting the ability to maintain a jogging pace, the further reduction in hospitalization was not significant (odds ratio = 0.22; 95% confidence interval, 0.05-1.04; P = .05). For COVID-19 symptom severity and number, there were no significant associations with self-reported CR fitness or physical activity levels. Conclusions: For individuals with low self-reported CR fitness, improving CR fitness represents a strategy to reduce the risk of hospitalization from COVID-19.
References
Ahmed, COVID-19-does exercise prescription and maximal oxygen uptake (VO 2 max) have a role in risk-stratifying patients?, Clin Med J R Coll Physicians Lond, doi:10.7861/clinmed.2020-0111
Bradshaw, George, Hyde, An accurate vo2max nonexercise regression model for 18-65-year-old adults, Res Q Exerc Sport, doi:10.1080/02701367.2005.10599315
Brawner, Ehrman, Bole, Maximal exercise capacity is inversely related to hospitalization secondary to coronavirus disease 2019, Mayo Clin Proc, doi:10.1016/j.mayocp.2020.10.003
Duggal, Niemiro, Harridge, Simpson, Lord, Can physical activity ameliorate immunosenescence and thereby reduce age-related multi-morbidity?, Nat Rev Immunol, doi:10.1038/s41577-019-0177-9
Hamer, Kivimäki, Gale, Batty, Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: a community-based cohort study of 387,109 adults in UK, Brain Behav Immun, doi:10.1016/j.bbi.2020.05.059
Hjelstuen, Anderssen, Holme, Seljeflot, Klemsdal, Markers of inflammation are inversely related to physical activity and fitness in sedentary men with treated hypertension, Am J Hypertens, doi:10.1016/j.amjhyper.2005.11.012
Krajewska, Krajewski, Zub, Zatoński, COVID-19 in otolaryngologist practice: a review of current knowledge, Eur Arch Oto-Rhino-Laryngology, doi:10.1007/s00405-020-05968-y
Lake, What we know so far: COVID-19 current clinical knowledge and research, Clin Med J R Coll Physicians Lond, doi:10.7861/clinmed.2019-coron
Lesser, Nienhuis, The impact of COVID-19 on physical activity behavior and well-being of Canadians, Int J Environ Res Public Health, doi:10.3390/ijerph17113899
Li, Xu, Yu, Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan, J Allergy Clin Immunol, doi:10.1016/j.jaci.2020.04.006
Long, Ward, Khorasani-Zadeh, The impact of obesity on COVID-19 disease severity, PRiMER, doi:10.22454/PRiMER.2020.104798
Matthews, Heil, Freedson, Pastides, Classification of cardiorespiratory fitness without exercise testing, Med Sci Sports Exerc, doi:10.1097/00005768-199903000-00019
Nieman, Coronavirus disease-2019: a tocsin to our aging, unfit, corpulent, and immunodeficient society, J Sport Heal Sci, doi:10.1016/j.jshs.2020.05.001
Nieman, Wentz, The compelling link between physical activity and the body's defense system, J Sport Heal Sci, doi:10.1016/j.jshs.2018.09.009
Razai, Doerholt, Ladhani, Oakeshott, Coronavirus disease 2019 (COVID-19): a guide for UK GPS, BMJ, doi:10.1136/bmj.m800
Reinholdsson, Palstam, Sunnerhagen, Prestroke physical activity could influence acute stroke severity (part of PAPSIGOT), Neurology, doi:10.1212/WNL.0000000000006354
Sallis, Adlakha, Oyeyemi, Salvo, An international physical activity and public health research agenda to inform coronavirus disease-2019 policies and practices, J Sport Heal Sci, doi:10.1016/j.jshs.2020.05.005
Schuler, Leblanc, Marzilli, Effect of physical activity on the production of specific antibody in response to the 1998-99 influenza virus vaccine in older adults, J Sports Med Phys Fitness
Sebastiano, Chulak-Bozzer, Vanderloo, Faulkner, Don't walk so close to me: physical distancing and adult physical activity in Canada, Front Psychol, doi:10.3389/fpsyg.2020.01895
Shatz, Fast, free, and targeted: reddit as a source for recruiting participants online, Soc Sci Comput Rev, doi:10.1177/0894439316650163
Simpson, Katsanis, The immunological case for staying active during the COVID-19 pandemic, Brain Behav Immun
Simpson, Kunz, Agha, Graff, Exercise and the regulation of immune functions, Prog Mol Biol Transl Sci
Sokolow, Naleway, Li, Severity of influenza and noninfluenza acute respiratory illness among pregnant women, 2010-2012, Am J Obstet Gynecol, doi:10.1016/j.ajog.2014.08.004
Wang, Li, Lu, Huang, Does comorbidity increase the risk of patients with covid-19: evidence from meta-analysis, Aging, doi:10.18632/aging.103000
Wong, Lai, Ou, Is exercise protective against influenza-associated mortality?, PLoS One, doi:10.1371/journal.pone.0002108
Wong, Narang, Lu, Hallmarks of improved immunological responses in the vaccination of more physically active elderly females, Exerc Immunol Rev
Zbinden-Foncea, Francaux, Deldicque, Hawley, Does high cardiorespiratory fitness confer some protection against proinflammatory responses after infection by SARS-CoV-2?, Obesity, doi:10.1002/oby.22849
Zheng, SARS-coV-2: an emerging coronavirus that causes a global threat, Int J Biol Sci, doi:10.7150/ijbs.45053
DOI record:
{
"DOI": "10.1123/jpah.2020-0817",
"ISSN": [
"1543-3080",
"1543-5474"
],
"URL": "http://dx.doi.org/10.1123/jpah.2020-0817",
"abstract": "<jats:p><jats:bold>Background</jats:bold>: Regular physical activity and higher cardiorespiratory (CR) fitness enhance immune function, possibly reducing coronavirus disease 2019 (COVID-19) infection severity. The aim was to assess the association between physical activity and self-reported CR fitness on COVID-19 infection characteristics. <jats:bold>Methods</jats:bold>: Participants formerly testing positive for COVID-19 completed an online questionnaire measuring COVID-19 infection characteristics and complications, self-reported CR fitness level, physical activity, and sociodemographic and health-related characteristics. Self-reported CR fitness was determined as the pace to cover 4.8 km without becoming overly fatigued (with slow walking, brisk walking, jogging, and running corresponding to low, moderate, good, and excellent levels of fitness, respectively). <jats:bold>Results</jats:bold>: A total of 263 individuals completed the survey. Compared with the lowest level of self-reported CR fitness, the odds of hospitalization significantly decreased by 64% (odds ratio = 0.36; 95% confidence interval, 0.13–0.98; <jats:italic>P</jats:italic> = .04) in individuals reporting the ability to maintain a brisk walk. In individuals reporting the ability to maintain a jogging pace, the further reduction in hospitalization was not significant (odds ratio = 0.22; 95% confidence interval, 0.05–1.04; <jats:italic>P</jats:italic> = .05). For COVID-19 symptom severity and number, there were no significant associations with self-reported CR fitness or physical activity levels. <jats:bold>Conclusions</jats:bold>: For individuals with low self-reported CR fitness, improving CR fitness represents a strategy to reduce the risk of hospitalization from COVID-19.</jats:p>",
"author": [
{
"affiliation": [],
"family": "Brandenburg",
"given": "Jason P.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Lesser",
"given": "Iris A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Thomson",
"given": "Cynthia J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Giles",
"given": "Luisa V.",
"sequence": "additional"
}
],
"container-title": [
"Journal of Physical Activity and Health"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
5,
13
]
],
"date-time": "2021-05-13T04:26:52Z",
"timestamp": 1620880012000
},
"deposited": {
"date-parts": [
[
2021,
7,
23
]
],
"date-time": "2021-07-23T09:13:36Z",
"timestamp": 1627031616000
},
"indexed": {
"date-parts": [
[
2022,
3,
30
]
],
"date-time": "2022-03-30T18:57:55Z",
"timestamp": 1648666675312
},
"is-referenced-by-count": 3,
"issn-type": [
{
"type": "print",
"value": "1543-3080"
},
{
"type": "electronic",
"value": "1543-5474"
}
],
"issue": "7",
"issued": {
"date-parts": [
[
2021,
7,
1
]
]
},
"journal-issue": {
"issue": "7"
},
"link": [
{
"URL": "https://journals.humankinetics.com/view/journals/jpah/18/7/article-p782.xml",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://journals.humankinetics.com/downloadpdf/journals/jpah/18/7/article-p782.xml",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "100",
"original-title": [],
"page": "782-788",
"prefix": "10.1123",
"published": {
"date-parts": [
[
2021,
7,
1
]
]
},
"published-print": {
"date-parts": [
[
2021,
7,
1
]
]
},
"publisher": "Human Kinetics",
"reference-count": 60,
"references-count": 60,
"relation": {},
"resource": {
"primary": {
"URL": "https://journals.humankinetics.com/view/journals/jpah/18/7/article-p782.xml"
}
},
"score": 1,
"short-container-title": [],
"short-title": [],
"source": "Crossref",
"subject": [
"Orthopedics and Sports Medicine"
],
"subtitle": [],
"title": [
"Does Higher Self-Reported Cardiorespiratory Fitness Reduce the Odds of Hospitalization From COVID-19?"
],
"type": "journal-article",
"volume": "18"
}
