Inverse Relationship of Maximal Exercise Capacity to Hospitalization Secondary to Coronavirus Disease 2019
et al., Mayo Clinic Proceedings, doi:10.1016/j.mayocp.2020.10.003, Oct 2020
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
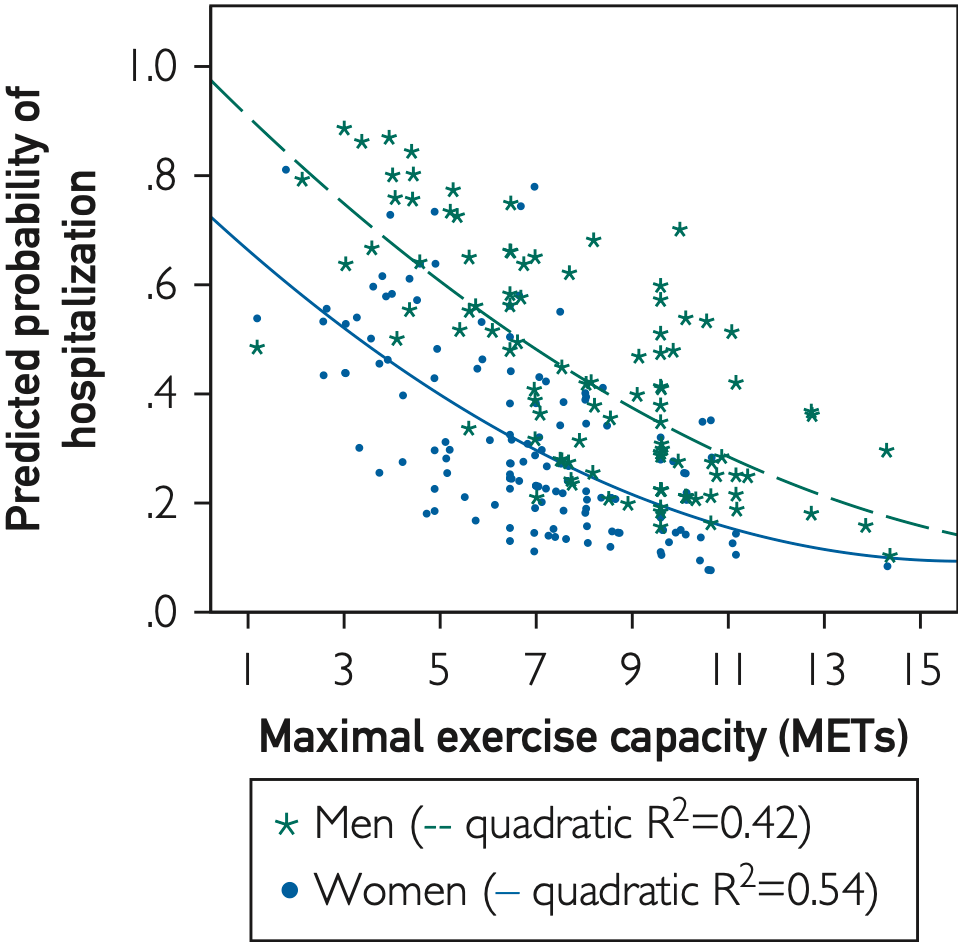
Retrospective 246 COVID-19 patients in the USA, showing the risk of hospitalization inversely associated with maximal exercise capacity. Adjusted results are only provided for MET as a continuous variable.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of hospitalization, 74.2% lower, OR 0.26, p = 0.001, unadjusted, inverted to make OR<1 favor high activity levels, highest fitness quartile vs. lowest fitness quartile, RR approximated with OR, excluded in exclusion analyses:
unadjusted results with no group details.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Brawner et al., 10 Oct 2020, retrospective, USA, peer-reviewed, 10 authors, study period 29 February, 2020 - 30 May, 2020.
Inverse Relationship of Maximal Exercise Capacity to Hospitalization Secondary to Coronavirus Disease 2019
Mayo Clinic Proceedings, doi:10.1016/j.mayocp.2020.10.003
Objective: To investigate the relationship between maximal exercise capacity measured before severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and hospitalization due to coronavirus disease 2019 (COVID-19). Methods: We identified patients (!18 years) who completed a clinically indicated exercise stress test between January 1, 2016, and February 29, 2020, and had a test for SARS-CoV-2 (ie, real-time reverse transcriptase polymerase chain reaction test) between February 29, 2020, and May 30, 2020. Maximal exercise capacity was quantified in metabolic equivalents of task (METs). Logistic regression was used to evaluate the likelihood that hospitalization secondary to COVID-19 is related to peak METs, with adjustment for 13 covariates previously identified as associated with higher risk for severe illness from COVID-19. Results: We identified 246 patients (age, 59AE12 years; 42% male; 75% black race) who had an exercise test and tested positive for SARS-CoV-2. Among these, 89 (36%) were hospitalized. Peak METs were significantly lower (P<.001) among patients who were hospitalized (6.7AE2.8) compared with those not hospitalized (8.0AE2.4). Peak METs were inversely associated with the likelihood of hospitalization in unadjusted (odds ratio, 0.83; 95% CI, 0.74-0.92) and adjusted models (odds ratio, 0.87; 95% CI, 0.76-0.99). Conclusion: Maximal exercise capacity is independently and inversely associated with the likelihood of hospitalization due to COVID-19. These data further support the important relationship between cardiorespiratory fitness and health outcomes. Future studies are needed to determine whether improving maximal exercise capacity is associated with lower risk of complications due to viral infections, such as COVID-19.
References
Blair, Kohl Hw 3rd, Paffenbarger, Jr, Clark et al., Physical fitness and all-cause mortality. A prospective study of healthy men and women, JAMA
Brawner, Al-Mallah, Ehrman, Qureshi, Blaha et al., Change in maximal exercise capacity is associated with survival in men and women, Mayo Clin Proc
Bruce, Kusumi, Hosmer, Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease, Am Heart J
Deoreo, Hemodialysis patient-assessed functional health status predicts continued survival, hospitalization, and dialysisattendance compliance, Am J Kidney Dis
Fleisher, Fleischmann, Auerbach, ACC/ AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines, J Am Coll Cardiol
Fletcher, Ades, Kligfield, Exercise standards for testing and training: a scientific statement from the American Heart Association, Circulation
Gleeson, Walsh, The BASES expert statement on exercise, immunity, and infection, J Sports Sci
Juraschek, Whelton, Sex Differences in cardiorespiratory fitness and all-cause mortality: the Henry Ford ExercIse Testing (FIT) Project, Mayo Clin Proc
Keteyian, Brawner, Savage, Peak aerobic capacity predicts prognosis in patients with coronary heart disease, Am Heart J
Keteyian, Patel, Kraus, Variables measured during cardiopulmonary exercise testing as predictors of mortality in chronic systolic heart failure, J Am Coll Cardiol
Myers, Prakash, Froelicher, Do, Partington et al., Exercise capacity and mortality among men referred for exercise testing, N Engl J Med
Nieman, Coronavirus disease-2019: a tocsin to our aging, unfit, corpulent, and immunodeficient society, J Sport Health Sci
Older, Levett, Cardiopulmonary exercise testing and surgery, Ann Am Thorac Soc
Richardson, Hirsch, Narasimhan, Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area, JAMA
Ross, Blair, Arena, Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association, Circulation
Sanchis-Gomar, Lavie, Mehra, Henry, Lippi, Obesity and outcomes in COVID-19: when an epidemic and pandemic collide, Mayo Clin Proc
Sharma, Garg, Rout, Lavie, Association of obesity with more critical illness in COVID-19, Mayo Clin Proc
DOI record:
{
"DOI": "10.1016/j.mayocp.2020.10.003",
"ISSN": [
"0025-6196"
],
"URL": "http://dx.doi.org/10.1016/j.mayocp.2020.10.003",
"alternative-id": [
"S0025619620311307"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Inverse Relationship of Maximal Exercise Capacity to Hospitalization Secondary to Coronavirus Disease 2019"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Mayo Clinic Proceedings"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.mayocp.2020.10.003"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2020 Mayo Foundation for Medical Education and Research"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-1705-6620",
"affiliation": [],
"authenticated-orcid": false,
"family": "Brawner",
"given": "Clinton A.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Ehrman",
"given": "Jonathan K.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bole",
"given": "Shane",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kerrigan",
"given": "Dennis J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Parikh",
"given": "Sachin S.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lewis",
"given": "Barry K.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gindi",
"given": "Ryan M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Keteyian",
"given": "Courtland",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Abdul-Nour",
"given": "Khaled",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Keteyian",
"given": "Steven J.",
"sequence": "additional"
}
],
"container-title": [
"Mayo Clinic Proceedings"
],
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.jp",
"mayoclinicproceedings.org",
"clinicalkey.com",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.fr",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2020,
10,
10
]
],
"date-time": "2020-10-10T15:09:01Z",
"timestamp": 1602342541000
},
"deposited": {
"date-parts": [
[
2021,
1,
21
]
],
"date-time": "2021-01-21T23:02:22Z",
"timestamp": 1611270142000
},
"indexed": {
"date-parts": [
[
2022,
4,
4
]
],
"date-time": "2022-04-04T21:12:58Z",
"timestamp": 1649106778118
},
"is-referenced-by-count": 63,
"issn-type": [
{
"type": "print",
"value": "0025-6196"
}
],
"issue": "1",
"issued": {
"date-parts": [
[
2021,
1
]
]
},
"journal-issue": {
"issue": "1",
"published-print": {
"date-parts": [
[
2021,
1
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
1,
1
]
],
"date-time": "2021-01-01T00:00:00Z",
"timestamp": 1609459200000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0025619620311307?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0025619620311307?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "32-39",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2021,
1
]
]
},
"published-print": {
"date-parts": [
[
2021,
1
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1016/S0272-6386(97)90053-6",
"article-title": "Hemodialysis patient-assessed functional health status predicts continued survival, hospitalization, and dialysis-attendance compliance",
"author": "DeOreo",
"doi-asserted-by": "crossref",
"first-page": "204",
"issue": "2",
"journal-title": "Am J Kidney Dis",
"key": "10.1016/j.mayocp.2020.10.003_bib1",
"volume": "30",
"year": "1997"
},
{
"DOI": "10.1016/j.jacc.2014.07.944",
"article-title": "2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines",
"author": "Fleisher",
"doi-asserted-by": "crossref",
"first-page": "e77",
"issue": "22",
"journal-title": "J Am Coll Cardiol",
"key": "10.1016/j.mayocp.2020.10.003_bib2",
"volume": "64",
"year": "2014"
},
{
"DOI": "10.1016/j.ahj.2008.03.017",
"article-title": "Peak aerobic capacity predicts prognosis in patients with coronary heart disease",
"author": "Keteyian",
"doi-asserted-by": "crossref",
"first-page": "292",
"issue": "2",
"journal-title": "Am Heart J",
"key": "10.1016/j.mayocp.2020.10.003_bib3",
"volume": "156",
"year": "2008"
},
{
"DOI": "10.1016/j.jacc.2015.11.050",
"article-title": "Variables measured during cardiopulmonary exercise testing as predictors of mortality in chronic systolic heart failure",
"author": "Keteyian",
"doi-asserted-by": "crossref",
"first-page": "780",
"issue": "7",
"journal-title": "J Am Coll Cardiol",
"key": "10.1016/j.mayocp.2020.10.003_bib4",
"volume": "67",
"year": "2016"
},
{
"DOI": "10.1513/AnnalsATS.201610-780FR",
"article-title": "Cardiopulmonary exercise testing and surgery",
"author": "Older",
"doi-asserted-by": "crossref",
"first-page": "S74",
"issue": "suppl 1",
"journal-title": "Ann Am Thorac Soc",
"key": "10.1016/j.mayocp.2020.10.003_bib5",
"volume": "14",
"year": "2017"
},
{
"DOI": "10.1161/CIR.0000000000000461",
"article-title": "Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association",
"author": "Ross",
"doi-asserted-by": "crossref",
"first-page": "e653",
"issue": "24",
"journal-title": "Circulation",
"key": "10.1016/j.mayocp.2020.10.003_bib6",
"volume": "134",
"year": "2016"
},
{
"DOI": "10.1001/jama.1989.03430170057028",
"article-title": "Physical fitness and all-cause mortality. A prospective study of healthy men and women",
"author": "Blair",
"doi-asserted-by": "crossref",
"first-page": "2395",
"issue": "17",
"journal-title": "JAMA",
"key": "10.1016/j.mayocp.2020.10.003_bib7",
"volume": "262",
"year": "1989"
},
{
"DOI": "10.1080/02640414.2011.627371",
"article-title": "The BASES expert statement on exercise, immunity, and infection",
"author": "Gleeson",
"doi-asserted-by": "crossref",
"first-page": "321",
"issue": "3",
"journal-title": "J Sports Sci",
"key": "10.1016/j.mayocp.2020.10.003_bib8",
"volume": "30",
"year": "2012"
},
{
"article-title": "Coronavirus disease-2019: a tocsin to our aging, unfit, corpulent, and immunodeficient society",
"author": "Nieman",
"first-page": "293",
"issue": "4",
"journal-title": "J Sport Health Sci",
"key": "10.1016/j.mayocp.2020.10.003_bib9",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.6775",
"article-title": "Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area",
"author": "Richardson",
"doi-asserted-by": "crossref",
"first-page": "2052",
"issue": "20",
"journal-title": "JAMA",
"key": "10.1016/j.mayocp.2020.10.003_bib10",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1016/j.mayocp.2020.05.006",
"article-title": "Obesity and outcomes in COVID-19: when an epidemic and pandemic collide",
"author": "Sanchis-Gomar",
"doi-asserted-by": "crossref",
"first-page": "1445",
"issue": "7",
"journal-title": "Mayo Clin Proc",
"key": "10.1016/j.mayocp.2020.10.003_bib11",
"volume": "95",
"year": "2020"
},
{
"DOI": "10.1016/j.mayocp.2020.06.046",
"article-title": "Association of obesity with more critical illness in COVID-19",
"author": "Sharma",
"doi-asserted-by": "crossref",
"first-page": "2040",
"issue": "9",
"journal-title": "Mayo Clin Proc",
"key": "10.1016/j.mayocp.2020.10.003_bib12",
"volume": "95",
"year": "2020"
},
{
"DOI": "10.1161/CIR.0b013e31829b5b44",
"article-title": "Exercise standards for testing and training: a scientific statement from the American Heart Association",
"author": "Fletcher",
"doi-asserted-by": "crossref",
"first-page": "873",
"issue": "8",
"journal-title": "Circulation",
"key": "10.1016/j.mayocp.2020.10.003_bib13",
"volume": "128",
"year": "2013"
},
{
"DOI": "10.1016/0002-8703(73)90502-4",
"article-title": "Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease",
"author": "Bruce",
"doi-asserted-by": "crossref",
"first-page": "546",
"issue": "4",
"journal-title": "Am Heart J",
"key": "10.1016/j.mayocp.2020.10.003_bib14",
"volume": "85",
"year": "1973"
},
{
"DOI": "10.1056/NEJMoa011858",
"article-title": "Exercise capacity and mortality among men referred for exercise testing",
"author": "Myers",
"doi-asserted-by": "crossref",
"first-page": "793",
"issue": "11",
"journal-title": "N Engl J Med",
"key": "10.1016/j.mayocp.2020.10.003_bib16",
"volume": "346",
"year": "2002"
},
{
"DOI": "10.1016/j.mayocp.2016.04.002",
"article-title": "Sex Differences in cardiorespiratory fitness and all-cause mortality: the Henry Ford ExercIse Testing (FIT) Project",
"author": "Al-Mallah",
"doi-asserted-by": "crossref",
"first-page": "755",
"issue": "6",
"journal-title": "Mayo Clin Proc",
"key": "10.1016/j.mayocp.2020.10.003_bib17",
"volume": "91",
"year": "2016"
},
{
"DOI": "10.1016/j.mayocp.2016.12.016",
"article-title": "Change in maximal exercise capacity is associated with survival in men and women",
"author": "Brawner",
"doi-asserted-by": "crossref",
"first-page": "383",
"issue": "3",
"journal-title": "Mayo Clin Proc",
"key": "10.1016/j.mayocp.2020.10.003_bib18",
"volume": "92",
"year": "2017"
},
{
"key": "10.1016/j.mayocp.2020.10.003_bib19",
"series-title": "2018 Physical Activity Guidelines for Americans",
"year": "2018"
}
],
"reference-count": 18,
"references-count": 18,
"relation": {
"has-review": [
{
"asserted-by": "object",
"id": "10.3410/f.739324710.793582658",
"id-type": "doi"
}
]
},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S0025619620311307"
}
},
"score": 1,
"short-container-title": [
"Mayo Clinic Proceedings"
],
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": [
"Inverse Relationship of Maximal Exercise Capacity to Hospitalization Secondary to Coronavirus Disease 2019"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "96"
}
