Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK
et al., Brain, Behavior, and Immunity, doi:10.1016/j.bbi.2020.05.059, Jul 2020
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
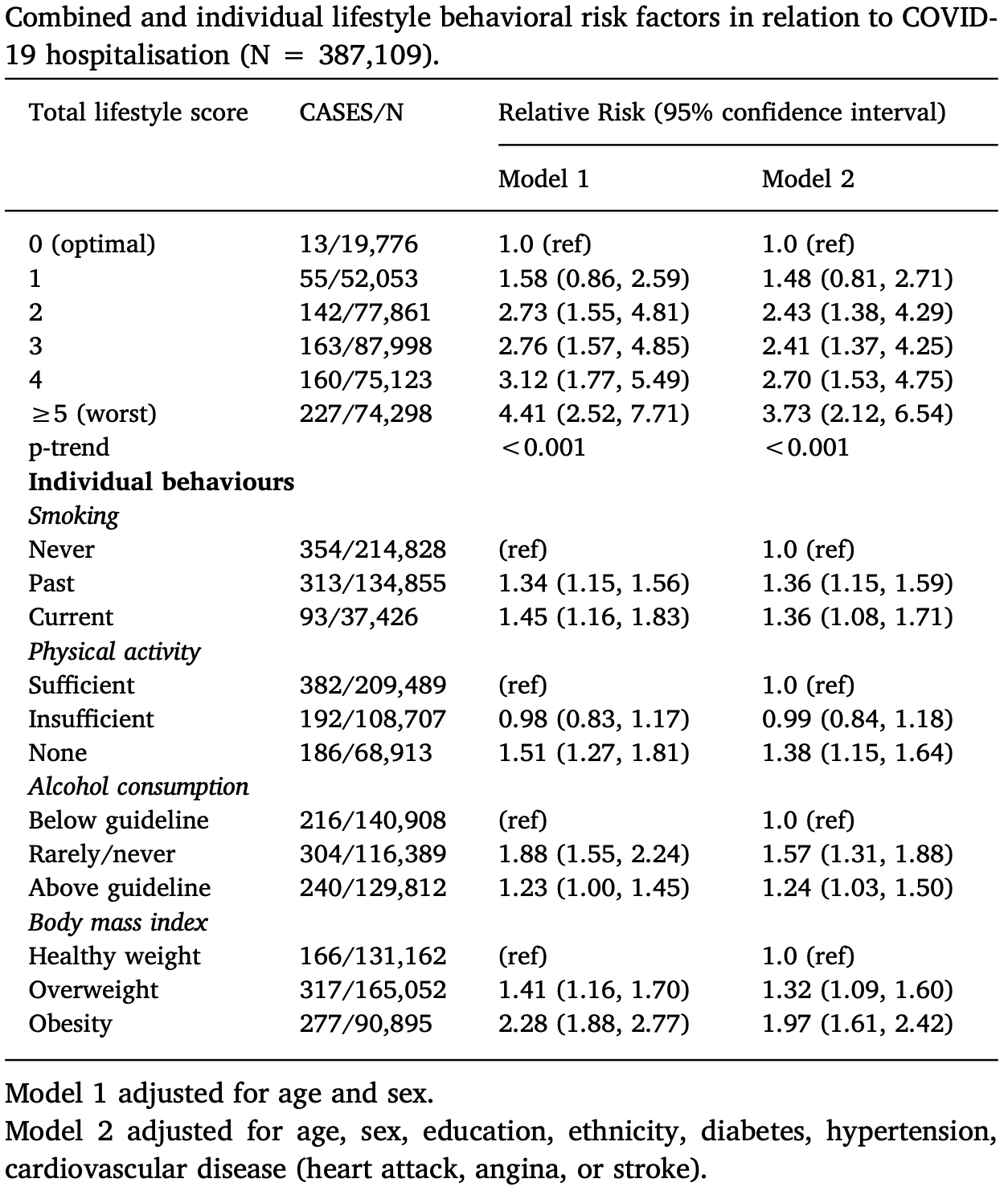
UK Biobank retrospective analysis of 387,109 people, showing lower risk of COVID-19 hospitalization with physical activity.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
|
risk of hospitalization, 27.5% lower, RR 0.72, p < 0.001, adjusted per study, inverted to make RR<1 favor high activity levels, model 2, sufficient vs. no activity, multivariable.
|
|
risk of hospitalization, 33.8% lower, RR 0.66, p < 0.001, adjusted per study, inverted to make RR<1 favor high activity levels, model 1, sufficient vs. no activity, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Hamer et al., 31 Jul 2020, retrospective, United Kingdom, peer-reviewed, 4 authors.
Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK
Brain, Behavior, and Immunity, doi:10.1016/j.bbi.2020.05.059
We conducted the first large-scale general population study on lifestyle risk factors (smoking, physical inactivity, obesity, and excessive alcohol intake) for COVID-19 using prospective cohort data with national registry linkage to hospitalisation. Participants were 387,109 men and women (56.4 ± 8.8 yr; 55.1% women) residing in England from UK Biobank study. Physical activity, smoking, and alcohol intake, were assessed by questionnaire at baseline (2006)(2007)(2008)(2009)(2010). Body mass index, from measured height and weight, was used as an indicator of overall obesity. Outcome was cases of COVID-19 serious enough to warrant a hospital admission from 16-March-2020 to 26-April-2020. There were 760 COVID-19 cases. After adjustment for age, sex and mutually for each lifestyle factor, physical inactivity (Relative risk, 1.32, 95% confidence interval, 1.10, 1.58), smoking (1.42;1.12, 1.79) and obesity (2.05 ;1.68, 2.49) but not heavy alcohol consumption (1.12; 0.93, 1.35) were all related to COVID-19. We also found a dose-dependent increase in risk of COVID-19 with less favourable lifestyle scores, such that participants in the most adverse category had 4-fold higher risk (4.41; 2.52-7.71) compared to people with the most optimal lifestyle. C-reactive protein levels were associated with elevated risk of COVID-19 in a dose-dependent manner, and partly (10-16%) explained associations between adverse lifestyle and COVID-19. Based on UK risk factor prevalence estimates, unhealthy behaviours in combination accounted for up to 51% of the population attributable fraction of severe COVID-19. Our findings suggest that an unhealthy lifestyle synonymous with an elevated risk of non-communicable disease is also a risk factor for COVID-19 hospital admission, which might be partly explained by low grade inflammation. Adopting simple lifestyle changes could lower the risk of severe infection.
Appendix A. Supplementary data Supplementary data to this article can be found online at https:// doi.org/10.1016/j.bbi.2020.05.059.
References
Baik, Curhan, Rimm, Bendich, Willett et al., A prospective study of age and lifestyle factors in relation to community-acquired pneumonia in US men and women, Arch. Intern. Med
Batty, Gale, Kivimäki, Deary, Bell, Comparison of risk factor associations in UK Biobank against representative, general population based studies with conventional response rates: prospective cohort study and individual participant meta-analysis, BMJ, doi:10.1136/bmj.m131
Colpani, Baena, Jaspers, Van Dijk, Farajzadegan et al., Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: a systematic review and meta-analysis, Eur. J. Epidemiol
Craig, Marshall, Sjorstrom, Bauman, Booth et al., International physical activity questionnaire: 12-country reliability and validity, Med. Sci. Sport Exerc
Del Giudice, Gangestad, Rethinking IL-6 and CRP: why they are more than inflammatory biomarkers, and why it matters, Brain Behav. Immun
Fry, Almond, Moffat, Gordon, Singh, UK Biobank Biomarker Project: Companion document to accompany serum biomarker data
Hamer, O'donovan, Stamatakis, Lifestyle risk factors, obesity and infectious disease mortality in the general population: linkage study of 97,844 adults from England and Scotland, Prev. Med
Harpsoe, Nielsen, Friis-Moller, Body mass index and risk of infections among women in the Danish national birth cohort, Am. J. Epidemiol
Inoue, Koizumi, Wada, Risk and protective factors related to mortality from pneumonia among middle aged and elderly community residents: the JACC Study, J Epidemiol
Li, Schoufour, Wang, Dhana, Pan et al., Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: prospective cohort study, BMJ, doi:10.1136/bmj.l6669
Matthews, Ockene, Freedson, Rosal, Merriam et al., Moderate to vigorous physical activity and risk of upper-respiratory tract infection, Med. Sci. Sports Exerc
Nieman, Henson, Austin, Sha, Upper respiratory tract infection is reduced in physically fit and active adults, Br. J. Sports Med
Nyberg, Singh-Manoux, Pentti, Madsen, Sabia et al., Association of healthy lifestyle with years lived without major chronic diseases, JAMA Int. Med, doi:10.1001/jamainternmed.2020.0618
Pascoe, Singh, Edwards, The effects of exercise on vaccination responses: a review of chronic and acute exercise interventions in humans, Brain Behav. Immun
Paulsen, Askim, Mohus, Associations of obesity and lifestyle with the risk and mortality of bloodstream infection in a general population: a 15-year follow-up of 64 027 individuals in the HUNT Study, Int. J. Epidemiol
Said, Verweij, Van Der Harst, Associations of combined genetic and lifestyle risks with incident cardiovascular disease and diabetes in the UK biobank study, JAMA Cardiol
Sattar, Mcinnes, Mcmurray, Obesity a risk factor for severe COVID-19 infection: multiple potential mechanisms, Circulation, doi:10.1161/CIRCULATIONAHA.120.047659
Schlesinger, Neuenschwander, Ballon, Nöthlings, Barbaresko, Adherence to healthy lifestyles and incidence of diabetes and mortality among individuals with diabetes: a systematic review and meta-analysis of prospective studies, J. Epidemiol. Community Health
Schwellnus, Soligard, Alonso, How much is too much? (Part 2) International Olympic Committee consensus statement on load in sport and risk of illness, Br. J. Sports Med
Spence, Brown, Pyne, Incidence, etiology, and symptomatology of upper respiratory illness in elite athletes, Med. Sci. Sports Exerc
Sudlow, Gallacher, Allen, UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age, PLoS Med
Wang, Baddley, Griffin, Physical inactivity and long-term rates of community-acquired sepsis, Prev. Med
DOI record:
{
"DOI": "10.1016/j.bbi.2020.05.059",
"ISSN": [
"0889-1591"
],
"URL": "http://dx.doi.org/10.1016/j.bbi.2020.05.059",
"alternative-id": [
"S088915912030996X"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Brain, Behavior, and Immunity"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.bbi.2020.05.059"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2020 Elsevier Inc. All rights reserved."
}
],
"author": [
{
"affiliation": [],
"family": "Hamer",
"given": "Mark",
"sequence": "first"
},
{
"affiliation": [],
"family": "Kivimäki",
"given": "Mika",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gale",
"given": "Catharine R.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Batty",
"given": "G. David",
"sequence": "additional"
}
],
"container-title": [
"Brain, Behavior, and Immunity"
],
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.jp",
"clinicalkey.com",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.fr",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2020,
5,
23
]
],
"date-time": "2020-05-23T06:33:16Z",
"timestamp": 1590215596000
},
"deposited": {
"date-parts": [
[
2021,
8,
16
]
],
"date-time": "2021-08-16T00:28:04Z",
"timestamp": 1629073684000
},
"indexed": {
"date-parts": [
[
2022,
4,
3
]
],
"date-time": "2022-04-03T05:49:07Z",
"timestamp": 1648964947884
},
"is-referenced-by-count": 226,
"issn-type": [
{
"type": "print",
"value": "0889-1591"
}
],
"issued": {
"date-parts": [
[
2020,
7
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
7,
1
]
],
"date-time": "2020-07-01T00:00:00Z",
"timestamp": 1593561600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S088915912030996X?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S088915912030996X?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "184-187",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2020,
7
]
]
},
"published-print": {
"date-parts": [
[
2020,
7
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1007/s10654-018-0374-z",
"article-title": "Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: a systematic review and meta-analysis",
"author": "Colpani",
"doi-asserted-by": "crossref",
"first-page": "831",
"issue": "9",
"journal-title": "Eur. J. Epidemiol.",
"key": "10.1016/j.bbi.2020.05.059_b0005",
"volume": "33",
"year": "2018"
},
{
"DOI": "10.1136/jech-2019-213415",
"article-title": "Adherence to healthy lifestyles and incidence of diabetes and mortality among individuals with diabetes: a systematic review and meta-analysis of prospective studies",
"author": "Schlesinger",
"doi-asserted-by": "crossref",
"first-page": "481",
"issue": "5",
"journal-title": "J. Epidemiol. Community Health",
"key": "10.1016/j.bbi.2020.05.059_b0010",
"volume": "74",
"year": "2020"
},
{
"DOI": "10.1001/jamainternmed.2020.0618",
"article-title": "Association of healthy lifestyle with years lived without major chronic diseases",
"author": "Nyberg",
"doi-asserted-by": "crossref",
"journal-title": "JAMA Int. Med.",
"key": "10.1016/j.bbi.2020.05.059_b0015",
"year": "2020"
},
{
"article-title": "Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: prospective cohort study",
"author": "Li",
"issue": "368",
"journal-title": "BMJ",
"key": "10.1016/j.bbi.2020.05.059_b0020",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/j.ypmed.2014.04.017",
"article-title": "Physical inactivity and long-term rates of community-acquired sepsis",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "58",
"journal-title": "Prev. Med.",
"key": "10.1016/j.bbi.2020.05.059_b0025",
"volume": "65",
"year": "2014"
},
{
"DOI": "10.1001/archinte.160.20.3082",
"article-title": "A prospective study of age and lifestyle factors in relation to community-acquired pneumonia in US men and women",
"author": "Baik",
"doi-asserted-by": "crossref",
"first-page": "3082",
"issue": "20",
"journal-title": "Arch. Intern. Med.",
"key": "10.1016/j.bbi.2020.05.059_b0030",
"volume": "160",
"year": "2000"
},
{
"DOI": "10.2188/jea.17.194",
"article-title": "Risk and protective factors related to mortality from pneumonia among middle aged and elderly community residents: the JACC Study",
"author": "Inoue",
"doi-asserted-by": "crossref",
"first-page": "194",
"issue": "6",
"journal-title": "J Epidemiol",
"key": "10.1016/j.bbi.2020.05.059_b0035",
"volume": "17",
"year": "2007"
},
{
"DOI": "10.1016/j.ypmed.2019.03.002",
"article-title": "Lifestyle risk factors, obesity and infectious disease mortality in the general population: linkage study of 97,844 adults from England and Scotland",
"author": "Hamer",
"doi-asserted-by": "crossref",
"first-page": "65",
"journal-title": "Prev. Med.",
"key": "10.1016/j.bbi.2020.05.059_b0040",
"volume": "123",
"year": "2019"
},
{
"DOI": "10.1093/ije/dyx091",
"article-title": "Associations of obesity and lifestyle with the risk and mortality of bloodstream infection in a general population: a 15-year follow-up of 64 027 individuals in the HUNT Study",
"author": "Paulsen",
"doi-asserted-by": "crossref",
"first-page": "1573",
"issue": "5",
"journal-title": "Int. J. Epidemiol.",
"key": "10.1016/j.bbi.2020.05.059_b0045",
"volume": "46",
"year": "2017"
},
{
"DOI": "10.1371/journal.pmed.1001779",
"article-title": "UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age",
"author": "Sudlow",
"doi-asserted-by": "crossref",
"issue": "3",
"journal-title": "PLoS Med.",
"key": "10.1016/j.bbi.2020.05.059_b0050",
"volume": "12",
"year": "2015"
},
{
"DOI": "10.1001/jamacardio.2018.1717",
"article-title": "Associations of combined genetic and lifestyle risks with incident cardiovascular disease and diabetes in the UK biobank study",
"author": "Said",
"doi-asserted-by": "crossref",
"first-page": "693",
"issue": "8",
"journal-title": "JAMA Cardiol.",
"key": "10.1016/j.bbi.2020.05.059_b0055",
"volume": "3",
"year": "2018"
},
{
"DOI": "10.1249/01.MSS.0000078924.61453.FB",
"article-title": "International physical activity questionnaire: 12-country reliability and validity",
"author": "Craig",
"doi-asserted-by": "crossref",
"first-page": "1381",
"issue": "8",
"journal-title": "Med. Sci. Sport Exerc.",
"key": "10.1016/j.bbi.2020.05.059_b0060",
"volume": "35",
"year": "2003"
},
{
"key": "10.1016/j.bbi.2020.05.059_b0065",
"unstructured": "NHS England and NHS Improvement. COVID-19 virus testing in NHS laboratories. Accessed 5/3/20 https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/guidance-and-sop-covid-19-virus-testing-in-nhs-laboratories-v1.pdf."
},
{
"key": "10.1016/j.bbi.2020.05.059_b0070",
"unstructured": "NHS Digital. Health Survey for England 2018 Overweight and obesity in adults and children. Accessed 5/5/20 https://files.digital.nhs.uk/52/FD7E18/HSE18-Adult-Child-Obesity-rep.pdf."
},
{
"key": "10.1016/j.bbi.2020.05.059_b0075",
"unstructured": "NHS Digital. Health Survey for England 2018 Adult’s health-related behaviours. Accessed 5/5/20 https://files.digital.nhs.uk/B5/771AC5/HSE18-Adult-Health-Related-Behaviours-rep-v3.pdf."
},
{
"key": "10.1016/j.bbi.2020.05.059_b0080",
"unstructured": "Fry, D., Almond, R., Moffat, S., Gordon, M., Singh, P. UK Biobank Biomarker Project: Companion document to accompany serum biomarker data Accessed 5/5/20 https://biobank.ndph.ox.ac.uk/showcase/showcase/docs/serum_biochemistry.pdf."
},
{
"DOI": "10.1136/bjsports-2016-096572",
"article-title": "How much is too much? (Part 2) International Olympic Committee consensus statement on load in sport and risk of illness",
"author": "Schwellnus",
"doi-asserted-by": "crossref",
"first-page": "1043",
"issue": "17",
"journal-title": "Br. J. Sports Med.",
"key": "10.1016/j.bbi.2020.05.059_b0085",
"volume": "50",
"year": "2016"
},
{
"DOI": "10.1249/mss.0b013e31802e851a",
"article-title": "Incidence, etiology, and symptomatology of upper respiratory illness in elite athletes",
"author": "Spence",
"doi-asserted-by": "crossref",
"first-page": "577",
"issue": "4",
"journal-title": "Med. Sci. Sports Exerc.",
"key": "10.1016/j.bbi.2020.05.059_b0090",
"volume": "39",
"year": "2007"
},
{
"DOI": "10.1097/00005768-200208000-00003",
"article-title": "Moderate to vigorous physical activity and risk of upper-respiratory tract infection",
"author": "Matthews",
"doi-asserted-by": "crossref",
"first-page": "1242",
"issue": "8",
"journal-title": "Med. Sci. Sports Exerc.",
"key": "10.1016/j.bbi.2020.05.059_b0095",
"volume": "34",
"year": "2002"
},
{
"DOI": "10.1136/bjsm.2010.077875",
"article-title": "Upper respiratory tract infection is reduced in physically fit and active adults",
"author": "Nieman",
"doi-asserted-by": "crossref",
"first-page": "987",
"issue": "12",
"journal-title": "Br. J. Sports Med.",
"key": "10.1016/j.bbi.2020.05.059_b0100",
"volume": "45",
"year": "2011"
},
{
"DOI": "10.1016/j.bbi.2013.10.003",
"article-title": "The effects of exercise on vaccination responses: a review of chronic and acute exercise interventions in humans",
"author": "Pascoe",
"doi-asserted-by": "crossref",
"first-page": "33",
"journal-title": "Brain Behav. Immun.",
"key": "10.1016/j.bbi.2020.05.059_b0105",
"volume": "39",
"year": "2014"
},
{
"DOI": "10.1093/aje/kwv300",
"article-title": "Body mass index and risk of infections among women in the Danish national birth cohort",
"author": "Harpsoe",
"doi-asserted-by": "crossref",
"first-page": "1008",
"issue": "11",
"journal-title": "Am. J. Epidemiol.",
"key": "10.1016/j.bbi.2020.05.059_b0110",
"volume": "183",
"year": "2016"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.047659",
"article-title": "Obesity a risk factor for severe COVID-19 infection: multiple potential mechanisms",
"author": "Sattar",
"doi-asserted-by": "crossref",
"journal-title": "Circulation",
"key": "10.1016/j.bbi.2020.05.059_b0115",
"year": "2020"
},
{
"DOI": "10.1016/j.bbi.2018.02.013",
"article-title": "Rethinking IL-6 and CRP: why they are more than inflammatory biomarkers, and why it matters",
"author": "Del Giudice",
"doi-asserted-by": "crossref",
"first-page": "61",
"journal-title": "Brain Behav. Immun.",
"key": "10.1016/j.bbi.2020.05.059_b0120",
"volume": "70",
"year": "2018"
},
{
"DOI": "10.1136/bmj.m131",
"article-title": "Comparison of risk factor associations in UK Biobank against representative, general population based studies with conventional response rates: prospective cohort study and individual participant meta-analysis",
"author": "Batty",
"doi-asserted-by": "crossref",
"first-page": "m131",
"journal-title": "BMJ",
"key": "10.1016/j.bbi.2020.05.059_b0125",
"volume": "368",
"year": "2020"
}
],
"reference-count": 25,
"references-count": 25,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S088915912030996X"
}
},
"score": 1,
"short-container-title": [
"Brain, Behavior, and Immunity"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Behavioral Neuroscience",
"Endocrine and Autonomic Systems",
"Immunology"
],
"subtitle": [],
"title": [
"Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "87"
}
