Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study
et al., British Journal of Sports Medicine, doi:10.1136/bjsports-2021-104203, Jul 2021
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
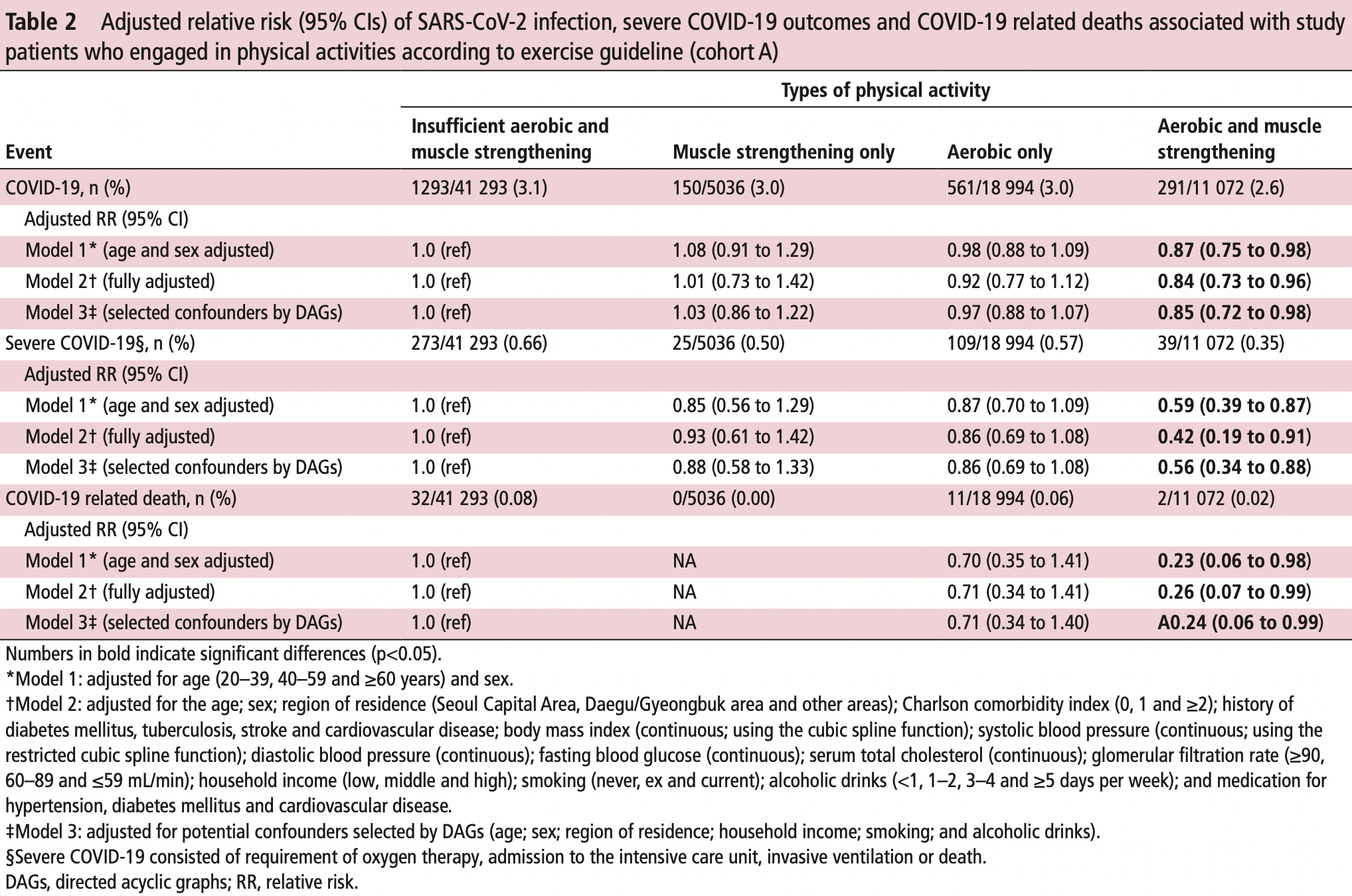
Retrospective 212,768 adults in South Korea, showing lower risk of COVID-19 cases, severity, and mortality with physical activity. Notably, results for aerobic and muscle strengthening activities combined were much better than results for either one in isolation.
|
risk of death, 74.0% lower, RR 0.26, p = 0.046, high activity levels 2 of 11,072 (0.0%), low activity levels 32 of 41,293 (0.1%), NNT 1683, adjusted per study, odds ratio converted to relative risk, model 2,aerobic and muscle strengthening vs. insufficient aerobic and muscle strengthening, multivariable.
|
|
risk of severe case, 57.8% lower, RR 0.42, p = 0.03, high activity levels 39 of 11,072 (0.4%), low activity levels 273 of 41,293 (0.7%), adjusted per study, odds ratio converted to relative risk, model 2,aerobic and muscle strengthening vs. insufficient aerobic and muscle strengthening, multivariable.
|
|
risk of case, 15.6% lower, RR 0.84, p = 0.03, high activity levels 291 of 11,072 (2.6%), low activity levels 1,293 of 41,293 (3.1%), NNT 199, adjusted per study, odds ratio converted to relative risk, model 2,aerobic and muscle strengthening vs. insufficient aerobic and muscle strengthening, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Lee et al., 22 Jul 2021, retrospective, South Korea, peer-reviewed, 25 authors, study period 1 January, 2020 - 31 July, 2020.
Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study
British Journal of Sports Medicine, doi:10.1136/bjsports-2021-104203
Purpose To determine the potential associations between physical activity and risk of SARS-CoV-2 infection, severe illness from COVID-19 and COVID-19 related death using a nationwide cohort from South Korea. Methods Data regarding 212 768 Korean adults (age ≥20 years), who tested for SARS-CoV-2, from 1 January 2020 to 30 May 2020, were obtained from the National Health Insurance Service of South Korea and further linked with the national general health examination from 1 January 2018 to 31 December 2019 to assess physical activity levels. SARS-CoV-2 positivity, severe COVID-19 illness and COVID-19 related death were the main outcomes. The observation period was between 1 January 2020 and 31 July 2020. Results Out of 76 395 participants who completed the general health examination and were tested for SARS-CoV-2, 2295 (3.0%) were positive for SARS-CoV-2, 446 (0.58%) had severe illness from COVID-19 and 45 (0.059%) died from COVID-19. Adults who engaged in both aerobic and muscle strengthening activities according to the 2018 physical activity guidelines had a lower risk of SARS-CoV-2 infection (2.6% vs 3.1%; adjusted relative risk (aRR), 0.85; 95% CI 0.72 to 0.96), severe COVID-19 illness (0.35% vs 0.66%; aRR 0.42; 95% CI 0.19 to 0.91) and COVID-19 related death (0.02% vs 0.08%; aRR 0.24; 95% CI 0.05 to 0.99) than those who engaged in insufficient aerobic and muscle strengthening activities. Furthermore, the recommended range of metabolic equivalent task (MET; 500-1000 MET min/week) was associated with the maximum beneficial effect size for reduced risk of SARS-CoV-2 infection (aRR 0.78; 95% CI 0.66 to 0.92), severe COVID-19 illness (aRR 0.62; 95% CI 0.43 to 0.90) and COVID-19 related death (aRR 0.17; 95% CI 0.07 to 0.98). Similar patterns of association were observed in different sensitivity analyses. Conclusion Adults who engaged in the recommended levels of physical activity were associated with a decreased likelihood of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related death. Our findings suggest that engaging in physical activity has substantial public health value and demonstrates potential benefits to combat COVID-19.
Competing interests None declared. Patient consent for publication Not required.
Ethics approval The National Health Insurance Service-National Sample Cohort has ethical approval form the Institutional Review Board of Sejong University (SJU-HR-E-2020-003). Provenance and peer review Not commissioned; externally peer reviewed. Data availability statement Data are available on reasonable request. Study protocol, statistical code: available from DKYon (email: yonkkang@ gmail. com). Data set: available from the National Health Insurance Service of Korea (NHIS-COVID-19 data) through a data use agreement.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise. This article is made freely available for use in accordance with BMJ's website terms and conditions for the duration of the covid-19 pandemic or until otherwise determined by..
References
Ainsworth, Haskell, Whitt, Compendium of physical activities: an update of activity codes and Met intensities, Med Sci Sports Exerc, doi:10.1097/00005768-200009001-00009
Autenrieth, Baumert, Baumeister, Association between domains of physical activity and all-cause, cardiovascular and cancer mortality, Eur J Epidemiol, doi:10.1007/s10654-010-9517-6
Baik, Curhan, Rimm, A prospective study of age and lifestyle factors in relation to community-acquired pneumonia in US men and women, Arch Intern Med, doi:10.1001/archinte.160.20.3082
Brawner, Ehrman, Bole, Inverse relationship of maximal exercise capacity to hospitalization secondary to coronavirus disease 2019, Mayo Clin Proc, doi:10.1016/j.mayocp.2020.10.003
Chastin, Abaraogu, Bourgois, Physical activity, immune function and risk of community acquired infectious disease in the general population: systematic review and meta-analysis, doi:10.2139/ssrn.3673184
Chesnut, Macdonald, Wambier, Could diet and exercise reduce risk of COVID-19 syndemic?, Med Hypotheses, doi:10.1016/j.mehy.2021.110502
Comorbidity, index
Craig, Marshall, Sjöström, International physical activity questionnaire: 12-country reliability and validity, Med Sci Sports Exerc, doi:10.1249/01.MSS.0000078924.61453.FB
Ekelund, Tarp, Steene-Johannessen, Dose-Response associations between accelerometry measured physical activity and sedentary time and all cause mortality: systematic review and harmonised meta-analysis, BMJ, doi:10.1136/bmj.l4570
Elliott, Martin, Heron, Infographic. graduated return to play guidance following COVID-19 infection, Br J Sports Med, doi:10.1136/bjsports-2020-102637
Ghilotti, Pesonen, Raposo, Physical activity, sleep and risk of respiratory infections: a Swedish cohort study, PLoS One, doi:10.1371/journal.pone.0190270
Grande, Keogh, Silva, Exercise versus no exercise for the occurrence, severity, and duration of acute respiratory infections, Cochrane Database Syst Rev, doi:10.1002/14651858.CD010596.pub3
Greenland, Mansournia, Altman, Sparse data bias: a problem hiding in plain sight, Female, doi:10.1136/bmj.i1981
Grubic, Jain, Mihajlovic, Competing against COVID-19: have we forgotten about student-athletes' mental health?, Br J Sports Med, doi:10.1136/bjsports-2021-104218
Ha, Lee, Yon, Ten-Year trends and prevalence of asthma, allergic rhinitis, and atopic dermatitis among the Korean population, 2008-2017, Clin Exp Pediatr, doi:10.3345/cep.2019.01291
Haas, Angulo, Mclaughlin, Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data, Lancet, doi:10.1016/S0140-6736(21)00947-8
Hamer, Kivimäki, Gale, Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: a community-based cohort study of 387,109 adults in UK, Brain Behav Immun, doi:10.1016/j.bbi.2020.05.059
Jedrychowski, Maugeri, Flak, Cohort study on low physical activity level and recurrent acute respiratory infections in schoolchildren, Cent Eur J Public Health
Jordan, Adab, Cheng, Covid-19: risk factors for severe disease and death, BMJ, doi:10.1136/bmj.m1198
Keon, Sw, Yang, Yoo, Proton pump inhibitors and the risk of severe COVID-19: a post-hoc analysis from the Korean nationwide cohort, Gut, doi:10.1136/gutjnl-2020-323672
Klöting, Ristow, Blüher, Effects of exercise on ACE2, Obesity, doi:10.1002/oby.23041
Kyu, Bachman, Alexander, Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the global burden of disease study 2013, BMJ, doi:10.1136/bmj.i3857
Lee, Ha, Abdullah Özgür, Severe clinical outcomes of COVID-19 associated with proton pump inhibitors: a nationwide cohort study with propensity score matching, Gut, doi:10.1136/gutjnl-2020-322248
Lee, Kim, Moon, Estimating COVID-19 infection and severity risks in patients with chronic rhinosinusitis: a Korean nationwide cohort study, J Allergy Clin Immunol Pract, doi:10.1016/j.jaip.2021.03.044
Lee, None
Lee, Shiroma, Lobelo, Effect of physical inactivity on major noncommunicable diseases worldwide: an analysis of burden of disease and life expectancy, Lancet, doi:10.1016/S0140-6736(12)61031-9
Lee, Yang, Moon, Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: a nationwide cohort study, Lancet Psychiatry, doi:10.1016/S2215-0366(20)30421-1
Lee, Yon, James, Short-Term effects of multiple outdoor environmental factors on risk of asthma exacerbations: age-stratified time-series analysis, J Allergy Clin Immunol, doi:10.1016/j.jaci.2019.08.037
Lee, Yuh, Yang, Nationwide results of COVID-19 contact tracing in South Korea: individual participant data from an epidemiological survey, JMIR Med Inform, doi:10.2196/20992
Mansournia, Etminan, Danaei, Handling time varying confounding in observational research, BMJ, doi:10.1136/bmj.j4587
Neuman, Willett, Curhan, Physical activity and the risk of communityacquired pneumonia in US women, Am J Med, doi:10.1016/j.amjmed.2009.07.028
Pape, Ryttergaard, Rotevatn, Leisure-Time physical activity and the risk of suspected bacterial infections, Med Sci Sports Exerc, doi:10.1249/MSS.0000000000000953
Piercy, Troiano, Ballard, The physical activity guidelines for Americans, JAMA, doi:10.1001/jama.2018.14854
Rowlands, Kloecker, Chudasama, Association of timing and balance of physical activity and Rest/Sleep with risk of COVID-19: a UK Biobank study, Mayo Clin Proc, doi:10.1016/j.mayocp.2020.10.032
Sallis, Young, Tartof, Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients, Br J Sports Med, doi:10.1136/bjsports-2021-104080
Seo, None
Serling-Boyd, Silva, Hsu, Coronavirus disease 2019 outcomes among patients with rheumatic diseases 6 months into the pandemic, Ann Rheum Dis, doi:10.1136/annrheumdis-2020-219279
Shin, Shin, Moon, Autoimmune inflammatory rheumatic diseases and COVID-19 outcomes in South Korea: a nationwide cohort study, Lancet Rheumatol, doi:10.1016/S2665-9913(21)00151-X
Simpson, Kunz, Agha, Exercise and the regulation of immune functions, Prog Mol Biol Transl Sci
Stockwell, Trott, Tully, Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review, BMJ Open Sport Exerc Med, doi:10.1136/bmjsem-2020-000960
Stravinskas Durigon, Mackenzie, Oliveira-Junior, Aerobic exercise protects from Pseudomonas aeruginosa-induced pneumonia in elderly mice, J Innate Immun, doi:10.1159/000488953
Tison, Avram, Kuhar, Worldwide effect of COVID-19 on physical activity: a descriptive study, Ann Intern Med, doi:10.7326/M20-2665
Woo, Lee, Koh, Incidence of cancer after asthma development: 2 independent population-based cohort studies, J Allergy Clin Immunol, doi:10.1016/j.jaci.2020.04.041
Yang, Koh, Moon, Allergic disorders and susceptibility to and severity of COVID-19: A nationwide cohort study, J Allergy Clin Immunol, doi:10.1016/j.jaci.2020.08.008
Zhao, Veeranki, Magnussen, Recommended physical activity and all cause and cause specific mortality in US adults: prospective cohort study, BMJ, doi:10.1136/bmj.m2031
DOI record:
{
"DOI": "10.1136/bjsports-2021-104203",
"ISSN": [
"0306-3674",
"1473-0480"
],
"URL": "http://dx.doi.org/10.1136/bjsports-2021-104203",
"abstract": "<jats:sec><jats:title>Purpose</jats:title><jats:p>To determine the potential associations between physical activity and risk of SARS-CoV-2 infection, severe illness from COVID-19 and COVID-19 related death using a nationwide cohort from South Korea.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>Data regarding 212 768 Korean adults (age ≥20 years), who tested for SARS-CoV-2, from 1 January 2020 to 30 May 2020, were obtained from the National Health Insurance Service of South Korea and further linked with the national general health examination from 1 January 2018 to 31 December 2019 to assess physical activity levels. SARS-CoV-2 positivity, severe COVID-19 illness and COVID-19 related death were the main outcomes. The observation period was between 1 January 2020 and 31 July 2020.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>Out of 76 395 participants who completed the general health examination and were tested for SARS-CoV-2, 2295 (3.0%) were positive for SARS-CoV-2, 446 (0.58%) had severe illness from COVID-19 and 45 (0.059%) died from COVID-19. Adults who engaged in both aerobic and muscle strengthening activities according to the 2018 physical activity guidelines had a lower risk of SARS-CoV-2 infection (2.6% vs 3.1%; adjusted relative risk (aRR), 0.85; 95% CI 0.72 to 0.96), severe COVID-19 illness (0.35% vs 0.66%; aRR 0.42; 95% CI 0.19 to 0.91) and COVID-19 related death (0.02% vs 0.08%; aRR 0.24; 95% CI 0.05 to 0.99) than those who engaged in insufficient aerobic and muscle strengthening activities. Furthermore, the recommended range of metabolic equivalent task (MET; 500–1000 MET min/week) was associated with the maximum beneficial effect size for reduced risk of SARS-CoV-2 infection (aRR 0.78; 95% CI 0.66 to 0.92), severe COVID-19 illness (aRR 0.62; 95% CI 0.43 to 0.90) and COVID-19 related death (aRR 0.17; 95% CI 0.07 to 0.98). Similar patterns of association were observed in different sensitivity analyses.</jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p>Adults who engaged in the recommended levels of physical activity were associated with a decreased likelihood of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related death. Our findings suggest that engaging in physical activity has substantial public health value and demonstrates potential benefits to combat COVID-19.</jats:p></jats:sec>",
"alternative-id": [
"10.1136/bjsports-2021-104203"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-5632-5208",
"affiliation": [],
"authenticated-orcid": false,
"family": "Lee",
"given": "Seung Won",
"sequence": "first"
},
{
"affiliation": [],
"family": "Lee",
"given": "Jinhee",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Moon",
"given": "Sung Yong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jin",
"given": "Hyun Young",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yang",
"given": "Jee Myung",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ogino",
"given": "Shuji",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Song",
"given": "Mingyang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hong",
"given": "Sung Hwi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Abou Ghayda",
"given": "Ramy",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kronbichler",
"given": "Andreas",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Koyanagi",
"given": "Ai",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jacob",
"given": "Louis",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dragioti",
"given": "Elena",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Smith",
"given": "Lee",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Giovannucci",
"given": "Edward",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1083-6907",
"affiliation": [],
"authenticated-orcid": false,
"family": "Lee",
"given": "I-Min",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lee",
"given": "Dong Hoon",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lee",
"given": "Keum Hwa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shin",
"given": "Youn Ho",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kim",
"given": "So Young",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2115-7835",
"affiliation": [],
"authenticated-orcid": false,
"family": "Kim",
"given": "Min Seo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Won",
"given": "Hong-Hee",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ekelund",
"given": "Ulf",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shin",
"given": "Jae Il",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1628-9948",
"affiliation": [],
"authenticated-orcid": false,
"family": "Yon",
"given": "Dong Keon",
"sequence": "additional"
}
],
"container-title": [
"British Journal of Sports Medicine"
],
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2021,
7,
22
]
],
"date-time": "2021-07-22T17:25:40Z",
"timestamp": 1626974740000
},
"deposited": {
"date-parts": [
[
2021,
7,
22
]
],
"date-time": "2021-07-22T17:25:55Z",
"timestamp": 1626974755000
},
"funder": [
{
"DOI": "10.13039/501100003725",
"award": [
"NRF2019R1G1A109977913"
],
"doi-asserted-by": "crossref",
"name": "National Research Foundation of Korea"
}
],
"indexed": {
"date-parts": [
[
2022,
4,
4
]
],
"date-time": "2022-04-04T15:07:56Z",
"timestamp": 1649084876522
},
"is-referenced-by-count": 24,
"issn-type": [
{
"type": "print",
"value": "0306-3674"
},
{
"type": "electronic",
"value": "1473-0480"
}
],
"issued": {
"date-parts": [
[
2021,
7,
22
]
]
},
"language": "en",
"license": [
{
"URL": "https://bmj.com/coronavirus/usage",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
7,
22
]
],
"date-time": "2021-07-22T00:00:00Z",
"timestamp": 1626912000000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/bjsports-2021-104203",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "bjsports-2021-104203",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2021,
7,
22
]
]
},
"published-online": {
"date-parts": [
[
2021,
7,
22
]
]
},
"publisher": "BMJ",
"reference": [
{
"DOI": "10.1136/gutjnl-2020-323672",
"article-title": "Proton pump inhibitors and the risk of severe COVID-19: a post-hoc analysis from the Korean nationwide cohort",
"author": "Lee",
"doi-asserted-by": "crossref",
"journal-title": "Gut",
"key": "2021072210252106000_bjsports-2021-104203v1.1",
"year": "2020"
},
{
"DOI": "10.1016/S2215-0366(20)30421-1",
"article-title": "Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: a nationwide cohort study",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "1025",
"journal-title": "Lancet Psychiatry",
"key": "2021072210252106000_bjsports-2021-104203v1.2",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1136/gutjnl-2020-322248",
"doi-asserted-by": "publisher",
"key": "2021072210252106000_bjsports-2021-104203v1.3"
},
{
"DOI": "10.1016/s0140-6736(21)00947-8",
"doi-asserted-by": "publisher",
"key": "2021072210252106000_bjsports-2021-104203v1.4"
},
{
"DOI": "10.1016/j.jaci.2020.08.008",
"article-title": "Allergic disorders and susceptibility to and severity of COVID-19: A nationwide cohort study",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "790",
"journal-title": "J Allergy Clin Immunol",
"key": "2021072210252106000_bjsports-2021-104203v1.5",
"volume": "146",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m1198",
"doi-asserted-by": "publisher",
"key": "2021072210252106000_bjsports-2021-104203v1.6"
},
{
"DOI": "10.1016/S0140-6736(12)61031-9",
"doi-asserted-by": "publisher",
"key": "2021072210252106000_bjsports-2021-104203v1.7"
},
{
"DOI": "10.1136/bmj.l4570",
"doi-asserted-by": "publisher",
"key": "2021072210252106000_bjsports-2021-104203v1.8"
},
{
"DOI": "10.1136/bmj.i3857",
"doi-asserted-by": "publisher",
"key": "2021072210252106000_bjsports-2021-104203v1.9"
},
{
"DOI": "10.1001/jama.2018.14854",
"doi-asserted-by": "publisher",
"key": "2021072210252106000_bjsports-2021-104203v1.10"
},
{
"DOI": "10.1001/archinte.160.20.3082",
"doi-asserted-by": "publisher",
"key": "2021072210252106000_bjsports-2021-104203v1.11"
},
{
"DOI": "10.2139/ssrn.3673184",
"doi-asserted-by": "crossref",
"key": "2021072210252106000_bjsports-2021-104203v1.12",
"unstructured": "Chastin S , Abaraogu U , Bourgois J , et al . Physical activity, immune function and risk of community acquired infectious disease in the general population: systematic review and meta-analysis. SSRN 2020.doi:10.2139/ssrn.3673184"
},
{
"article-title": "Cohort study on low physical activity level and recurrent acute respiratory infections in schoolchildren",
"author": "Jedrychowski",
"first-page": "126",
"journal-title": "Cent Eur J Public Health",
"key": "2021072210252106000_bjsports-2021-104203v1.13",
"volume": "9",
"year": "2001"
},
{
"DOI": "10.1136/bmjsem-2020-000960",
"doi-asserted-by": "crossref",
"key": "2021072210252106000_bjsports-2021-104203v1.14",
"unstructured": "Stockwell S , Trott M , Tully M , et al . Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ Open Sport Exerc Med 2021;7:e000960. doi:10.1136/bmjsem-2020-000960"
},
{
"DOI": "10.2196/20992",
"article-title": "Nationwide results of COVID-19 contact tracing in South Korea: individual participant data from an epidemiological survey",
"author": "Lee",
"doi-asserted-by": "crossref",
"journal-title": "JMIR Med Inform",
"key": "2021072210252106000_bjsports-2021-104203v1.15",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1136/bjsports-2020-102637",
"doi-asserted-by": "publisher",
"key": "2021072210252106000_bjsports-2021-104203v1.16"
},
{
"DOI": "10.7326/M20-2665",
"article-title": "Worldwide effect of COVID-19 on physical activity: a descriptive study",
"author": "Tison",
"doi-asserted-by": "crossref",
"first-page": "767",
"journal-title": "Ann Intern Med",
"key": "2021072210252106000_bjsports-2021-104203v1.17",
"volume": "173",
"year": "2020"
},
{
"DOI": "10.1016/j.mayocp.2020.10.032",
"article-title": "Association of timing and balance of physical activity and Rest/Sleep with risk of COVID-19: a UK Biobank study",
"author": "Rowlands",
"doi-asserted-by": "crossref",
"first-page": "156",
"journal-title": "Mayo Clin Proc",
"key": "2021072210252106000_bjsports-2021-104203v1.18",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1016/j.mayocp.2020.10.003",
"article-title": "Inverse relationship of maximal exercise capacity to hospitalization secondary to coronavirus disease 2019",
"author": "Brawner",
"doi-asserted-by": "crossref",
"first-page": "32",
"journal-title": "Mayo Clin Proc",
"key": "2021072210252106000_bjsports-2021-104203v1.19",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1016/j.bbi.2020.05.059",
"doi-asserted-by": "publisher",
"key": "2021072210252106000_bjsports-2021-104203v1.20"
},
{
"DOI": "10.1136/bjsports-2021-104080",
"article-title": "Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients",
"author": "Sallis",
"doi-asserted-by": "crossref",
"journal-title": "Br J Sports Med",
"key": "2021072210252106000_bjsports-2021-104203v1.21",
"year": "2021"
},
{
"DOI": "10.1136/bmj.m2031",
"doi-asserted-by": "publisher",
"key": "2021072210252106000_bjsports-2021-104203v1.22"
},
{
"DOI": "10.1016/j.jaci.2020.04.041",
"article-title": "Incidence of cancer after asthma development: 2 independent population-based cohort studies",
"author": "Woo",
"doi-asserted-by": "crossref",
"first-page": "135",
"journal-title": "J Allergy Clin Immunol",
"key": "2021072210252106000_bjsports-2021-104203v1.23",
"volume": "147",
"year": "2021"
},
{
"DOI": "10.1249/01.MSS.0000078924.61453.FB",
"doi-asserted-by": "publisher",
"key": "2021072210252106000_bjsports-2021-104203v1.24"
},
{
"DOI": "10.1097/00005768-200009001-00009",
"doi-asserted-by": "publisher",
"key": "2021072210252106000_bjsports-2021-104203v1.25"
},
{
"DOI": "10.1016/S2665-9913(21)00151-X",
"article-title": "Autoimmune inflammatory rheumatic diseases and COVID-19 outcomes in South Korea: a nationwide cohort study",
"author": "Shin",
"doi-asserted-by": "crossref",
"journal-title": "Lancet Rheumatol",
"key": "2021072210252106000_bjsports-2021-104203v1.26",
"year": "2021"
},
{
"DOI": "10.1016/j.jaci.2019.08.037",
"article-title": "Short-Term effects of multiple outdoor environmental factors on risk of asthma exacerbations: age-stratified time-series analysis",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "1542",
"journal-title": "J Allergy Clin Immunol",
"key": "2021072210252106000_bjsports-2021-104203v1.27",
"volume": "144",
"year": "2019"
},
{
"DOI": "10.1016/j.jaip.2021.03.044",
"article-title": "Estimating COVID-19 infection and severity risks in patients with chronic rhinosinusitis: a Korean nationwide cohort study",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "2262",
"journal-title": "J Allergy Clin Immunol Pract",
"key": "2021072210252106000_bjsports-2021-104203v1.28",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.3345/cep.2019.01291",
"article-title": "Ten-Year trends and prevalence of asthma, allergic rhinitis, and atopic dermatitis among the Korean population, 2008–2017",
"author": "Ha",
"doi-asserted-by": "crossref",
"first-page": "278",
"journal-title": "Clin Exp Pediatr",
"key": "2021072210252106000_bjsports-2021-104203v1.29",
"volume": "63",
"year": "2020"
},
{
"DOI": "10.1249/MSS.0000000000000953",
"article-title": "Leisure-Time physical activity and the risk of suspected bacterial infections",
"author": "Pape",
"doi-asserted-by": "crossref",
"first-page": "1737",
"journal-title": "Med Sci Sports Exerc",
"key": "2021072210252106000_bjsports-2021-104203v1.30",
"volume": "48",
"year": "2016"
},
{
"DOI": "10.1371/journal.pone.0190270",
"article-title": "Physical activity, sleep and risk of respiratory infections: a Swedish cohort study",
"author": "Ghilotti",
"doi-asserted-by": "crossref",
"journal-title": "PLoS One",
"key": "2021072210252106000_bjsports-2021-104203v1.31",
"volume": "13",
"year": "2018"
},
{
"DOI": "10.1016/j.amjmed.2009.07.028",
"doi-asserted-by": "publisher",
"key": "2021072210252106000_bjsports-2021-104203v1.32"
},
{
"article-title": "Exercise versus no exercise for the occurrence, severity, and duration of acute respiratory infections",
"author": "Grande",
"first-page": "Cd010596",
"journal-title": "Cochrane Database Syst Rev",
"key": "2021072210252106000_bjsports-2021-104203v1.33",
"volume": "4",
"year": "2020"
},
{
"DOI": "10.1016/bs.pmbts.2015.08.001",
"doi-asserted-by": "publisher",
"key": "2021072210252106000_bjsports-2021-104203v1.34"
},
{
"DOI": "10.1159/000488953",
"article-title": "Aerobic exercise protects from Pseudomonas aeruginosa-induced pneumonia in elderly mice",
"author": "Stravinskas Durigon",
"doi-asserted-by": "crossref",
"first-page": "279",
"journal-title": "J Innate Immun",
"key": "2021072210252106000_bjsports-2021-104203v1.35",
"volume": "10",
"year": "2018"
},
{
"DOI": "10.1002/oby.23041",
"article-title": "Effects of exercise on ACE2",
"author": "Klöting",
"doi-asserted-by": "crossref",
"first-page": "2266",
"journal-title": "Obesity",
"key": "2021072210252106000_bjsports-2021-104203v1.36",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1016/j.mehy.2021.110502",
"article-title": "Could diet and exercise reduce risk of COVID-19 syndemic?",
"author": "Chesnut",
"doi-asserted-by": "crossref",
"journal-title": "Med Hypotheses",
"key": "2021072210252106000_bjsports-2021-104203v1.37",
"volume": "148",
"year": "2021"
},
{
"DOI": "10.1136/bjsports-2021-104218",
"article-title": "Competing against COVID-19: have we forgotten about student-athletes' mental health?",
"author": "Grubic",
"doi-asserted-by": "crossref",
"journal-title": "Br J Sports Med",
"key": "2021072210252106000_bjsports-2021-104203v1.38",
"year": "2021"
},
{
"DOI": "10.1007/s10654-010-9517-6",
"doi-asserted-by": "publisher",
"key": "2021072210252106000_bjsports-2021-104203v1.39"
},
{
"article-title": "Coronavirus disease 2019 outcomes among patients with rheumatic diseases 6 months into the pandemic",
"author": "Serling-Boyd",
"journal-title": "Ann Rheum Dis",
"key": "2021072210252106000_bjsports-2021-104203v1.40",
"year": "2020"
},
{
"DOI": "10.1136/bmj.j4587",
"doi-asserted-by": "publisher",
"key": "2021072210252106000_bjsports-2021-104203v1.41"
},
{
"DOI": "10.1136/bmj.i1981",
"doi-asserted-by": "crossref",
"key": "2021072210252106000_bjsports-2021-104203v1.42",
"unstructured": "Greenland S , Mansournia MA , Altman DG . Sparse data bias: a problem hiding in plain sight. BMJ 2016;352:i1981. doi:10.1136/bmj.i1981"
}
],
"reference-count": 42,
"references-count": 42,
"relation": {},
"resource": {
"primary": {
"URL": "https://bjsm.bmj.com/lookup/doi/10.1136/bjsports-2021-104203"
}
},
"score": 1,
"short-container-title": [
"Br J Sports Med"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Physical Therapy, Sports Therapy and Rehabilitation",
"Orthopedics and Sports Medicine",
"General Medicine"
],
"subtitle": [],
"title": [
"Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy"
}
