No independent associations between physical activity and clinical outcomes among hospitalized patients with moderate to severe COVID-19
et al., Journal of Sport and Health Science, doi:10.1016/j.jshs.2021.08.001, NCT04449718, Aug 2021
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
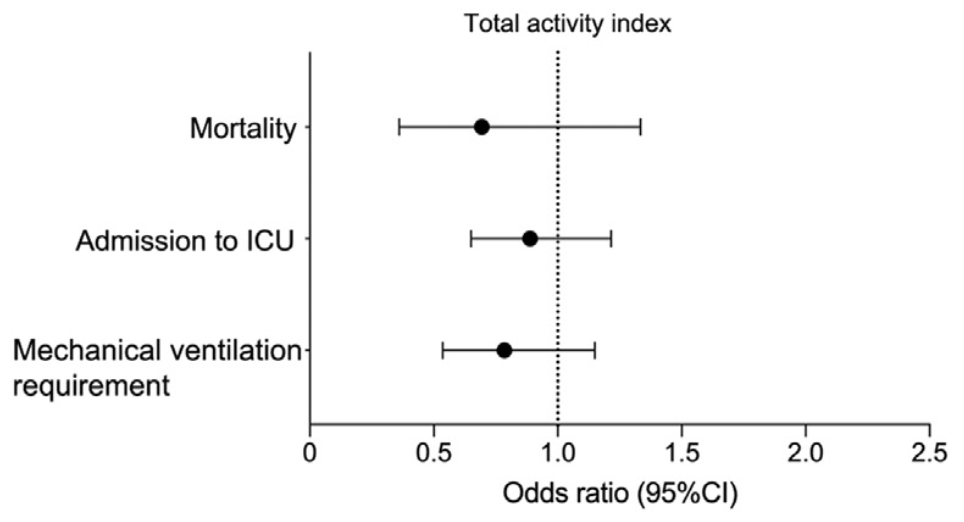
Prospective analysis of 209 hospitalized COVID-19 patients, showing no significant difference in COVID-19 outcomes with physical activity. Mortality, ventilation, and ICU results are only provided for activity as a continuous variable.
|
risk of death, 30.0% lower, OR 0.70, p = 0.27, RR approximated with OR.
|
|
risk of mechanical ventilation, 20.0% lower, OR 0.80, p = 0.21, RR approximated with OR.
|
|
risk of ICU admission, 10.0% lower, OR 0.90, p = 0.46, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Pinto et al., 12 Aug 2021, prospective, Brazil, peer-reviewed, survey, 10 authors, study period 2 June, 2020 - 7 October, 2020, trial NCT04449718 (history).
Contact: gualano@usp.br.
No independent associations between physical activity and clinical outcomes among hospitalized patients with moderate to severe COVID-19
Journal of Sport and Health Science, doi:10.1016/j.jshs.2021.08.001
Background: Regular physical activity (PA) has been postulated to improve, or at least maintain, immunity across the life span. However, the link between physical (in)activity and coronavirus disease 2019 (COVID-19) remains to be established. This small-scale prospective cohort study is nested within a randomized controlled trial aimed to investigate the possible associations between PA levels and clinical outcomes among hospitalized patients with moderate to severe COVID-19. Methods: Hospitalized patients with COVID-19 (mean age: 54.9 years) were recruited from the Clinical Hospital of the School of Medicine of the University of Sao Paulo (a quaternary referral teaching hospital) and from Ibirapuera Field Hospital, both located in Sao Paulo, Brazil. PA level was assessed using the Baecke Questionnaire of Habitual Physical Activity. The primary outcome was hospital length of stay. The secondary outcomes were mortality, admission to the intensive care unit (ICU), and mechanical ventilation requirement. Results: The median hospital length of stay was 7.0 § 4.0 days, median § IQR; 3.3% of patients died, 13.8% were admitted to the ICU, and 8.6% required mechanical ventilation. Adjusted linear regression models showed that PA indices were not associated with hospital length of stay (work index: b = À0.57 (95% confidence interval (95%CI): À1.80 to 0.65), p = 0.355; sport index: b = 0.43 (95%CI: À0.94 to 1.80), p = 0.536; leisure-time index: b = 1.18 (95%CI: À0.22 to 2.59), p = 0.099; and total activity index: b = 0.20 (95%CI: À0.48 to 0.87), p = 0.563). None of the PA indices were associated with mortality, admission to the ICU, or mechanical ventilation requirement (all p > 0.050). Conclusion: Among hospitalized patients with COVID-19, PA did not independently associate with hospital length of stay or any other clinically relevant outcomes. These findings should be interpreted as meaning that, among already hospitalized patients with more severe forms of COVID-19, being active is a potential protective factor likely outweighed by a cluster of comorbidities (e.g., type 2 diabetes, hypertension, weight excess) and older age, suggesting that the benefit of PA against the worsening of COVID-19 may vary across stages of the disease.
Authors' contributions AJP participated in conception and design, participants' recruitment, data collection, analysis and interpretation, statistical analysis, and manuscript writing; KFG participated in conception and design, participants' recruitment, data collection, analysis and interpretation, and manuscript revision; ALF, IHM, LPS, BZR, and MDS, participated in participants' recruitment, data collection, and manuscript revision; HR participated in data analysis and interpretation, statistical analysis, and manuscript revision; RMRP participated in data analysis and interpretation, obtaining funding, and manuscript revision; BG participated in conception and design, data analysis and interpretation, obtaining funding, and manuscript writing. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests The authors declare that they have no competing interests.
References
Damiot, Pinto, Turner, Gualano, Immunological implications of physical inactivity among older adults during the COVID-19 pandemic, Gerontology
De Souza, Motta-Santos, Soares, Association of physical activity levels and the prevalence of COVID-19-associated hospitalization, J Sci Med Sport
Ek, Kallings, Ekstrom, Borjesson, Ekblom, Subjective reports of physical activity levels and sedentary time prior to hospital admission can predict utilization of hospital care and all-cause mortality among patients with cardiovascular disease, Eur J Cardiovasc Nurs
Falagas, Kompoti, Obesity and infection, Lancet Infect Dis
Hamer, 'donovan, Stamatakis, Lifestyle risk factors, obesity and infectious disease mortality in the general population: Linkage study of 97,844 adults from England and Scotland, Prev Med
Hamer, Kivimaki, Gale, Batty, Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK, Brain Behav Immun
Joffe, Gambhir, Chadeau-Hyam, Vineis, Causal diagrams in systems epidemiology, Emerg Themes Epidemiol, doi:10.1186/1742-7622-9-1
Murai, Fernandes, Sales, Effect of a single high dose of vitamin d3 on hospital length of stay in patients with moderate to severe COVID-19: A randomized clinical trial, JAMA
Robins, Data, design, and background knowledge in etiologic inference, Epidemiology
Salgado-Aranda, Erez-Castellano, Uñez-Gil, Influence of baseline physical activity as a modifying factor on COVID-19 mortality: A single-center, retrospective study, Infect Dis Ther
Sallis, Young, Tartof, Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: A study in 48,440 adult patients, Br J Sports Med
Simpson, Campbell, Gleeson, Can exercise affect immune function to increase susceptibility to infection?, Exerc Immunol Rev
Woolcott, Ashe, Miller, Shi, Marra et al., Does physical activity reduce seniors' need for healthcare? A study of 24,281 Canadians, Br J Sports Med
DOI record:
{
"DOI": "10.1016/j.jshs.2021.08.001",
"ISSN": [
"2095-2546"
],
"URL": "http://dx.doi.org/10.1016/j.jshs.2021.08.001",
"alternative-id": [
"S2095254621000946"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "No independent associations between physical activity and clinical outcomes among hospitalized patients with moderate to severe COVID-19"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Journal of Sport and Health Science"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.jshs.2021.08.001"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2021 Published by Elsevier B.V. on behalf of Shanghai University of Sport."
}
],
"author": [
{
"affiliation": [],
"family": "Pinto",
"given": "Ana J.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Goessler",
"given": "Karla F.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fernandes",
"given": "Alan L.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Murai",
"given": "Igor H.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sales",
"given": "Lucas P.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Reis",
"given": "Bruna Z.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Santos",
"given": "Mayara Diniz",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Roschel",
"given": "Hamilton",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pereira",
"given": "Rosa M.R.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gualano",
"given": "Bruno",
"sequence": "additional"
}
],
"container-title": "Journal of Sport and Health Science",
"container-title-short": "Journal of Sport and Health Science",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2021,
8,
12
]
],
"date-time": "2021-08-12T08:21:59Z",
"timestamp": 1628756519000
},
"deposited": {
"date-parts": [
[
2022,
7,
18
]
],
"date-time": "2022-07-18T05:31:10Z",
"timestamp": 1658122270000
},
"funder": [
{
"DOI": "10.13039/501100003593",
"award": [
"301571/2017-1",
"301914/2017-6",
"305556/2017-7",
"2015/26937-4",
"2016/00006-7",
"2017/13552-2",
"2019/18039-7",
"2019/24782-4",
"2020/05752-4",
"2020/11102-2"
],
"doi-asserted-by": "publisher",
"name": "Conselho Nacional de Desenvolvimento Científico e Tecnológico"
},
{
"DOI": "10.13039/501100001807",
"award": [
"301571/2017-1",
"301914/2017-6",
"305556/2017-7",
"2015/26937-4",
"2016/00006-7",
"2017/13552-2",
"2019/18039-7",
"2019/24782-4",
"2020/05752-4",
"2020/11102-2"
],
"doi-asserted-by": "publisher",
"name": "Fundação de Amparo à Pesquisa do Estado de São Paulo"
}
],
"indexed": {
"date-parts": [
[
2022,
8,
22
]
],
"date-time": "2022-08-22T10:08:12Z",
"timestamp": 1661162892561
},
"is-referenced-by-count": 3,
"issue": "6",
"issued": {
"date-parts": [
[
2021,
12
]
]
},
"journal-issue": {
"issue": "6",
"published-print": {
"date-parts": [
[
2021,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
12,
1
]
],
"date-time": "2021-12-01T00:00:00Z",
"timestamp": 1638316800000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
8,
10
]
],
"date-time": "2021-08-10T00:00:00Z",
"timestamp": 1628553600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S2095254621000946?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S2095254621000946?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "690-696",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2021,
12
]
]
},
"published-print": {
"date-parts": [
[
2021,
12
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1016/j.ypmed.2019.03.002",
"article-title": "Lifestyle risk factors, obesity and infectious disease mortality in the general population: Linkage study of 97,844 adults from England and Scotland",
"author": "Hamer",
"doi-asserted-by": "crossref",
"first-page": "65",
"journal-title": "Prev Med",
"key": "10.1016/j.jshs.2021.08.001_bib0001",
"volume": "123",
"year": "2019"
},
{
"DOI": "10.1159/000509216",
"article-title": "Immunological implications of physical inactivity among older adults during the COVID-19 pandemic",
"author": "Damiot",
"doi-asserted-by": "crossref",
"first-page": "431",
"journal-title": "Gerontology",
"key": "10.1016/j.jshs.2021.08.001_bib0002",
"volume": "66",
"year": "2020"
},
{
"article-title": "Can exercise affect immune function to increase susceptibility to infection?",
"author": "Simpson",
"first-page": "8",
"journal-title": "Exerc Immunol Rev",
"key": "10.1016/j.jshs.2021.08.001_bib0003",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1016/j.bbi.2020.05.059",
"article-title": "Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK",
"author": "Hamer",
"doi-asserted-by": "crossref",
"first-page": "184",
"journal-title": "Brain Behav Immun",
"key": "10.1016/j.jshs.2021.08.001_bib0004",
"volume": "87",
"year": "2020"
},
{
"DOI": "10.1136/bjsports-2021-104080",
"article-title": "Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: A study in 48,440 adult patients",
"author": "Sallis",
"doi-asserted-by": "crossref",
"first-page": "1099",
"journal-title": "Br J Sports Med",
"key": "10.1016/j.jshs.2021.08.001_bib0005",
"volume": "55",
"year": "2021"
},
{
"DOI": "10.1007/s40121-021-00418-6",
"article-title": "Influence of baseline physical activity as a modifying factor on COVID-19 mortality: A single-center, retrospective study",
"author": "Salgado-Aranda",
"doi-asserted-by": "crossref",
"first-page": "801",
"journal-title": "Infect Dis Ther",
"key": "10.1016/j.jshs.2021.08.001_bib0006",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.26848",
"article-title": "Effect of a single high dose of vitamin d3 on hospital length of stay in patients with moderate to severe COVID-19: A randomized clinical trial",
"author": "Murai",
"doi-asserted-by": "crossref",
"first-page": "1053",
"journal-title": "JAMA",
"key": "10.1016/j.jshs.2021.08.001_bib0007",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.1186/1742-7622-9-1",
"article-title": "Causal diagrams in systems epidemiology",
"author": "Joffe",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Emerg Themes Epidemiol",
"key": "10.1016/j.jshs.2021.08.001_bib0008",
"volume": "9",
"year": "2012"
},
{
"DOI": "10.1097/00001648-200105000-00011",
"article-title": "Data, design, and background knowledge in etiologic inference",
"author": "Robins",
"doi-asserted-by": "crossref",
"first-page": "313",
"journal-title": "Epidemiology",
"key": "10.1016/j.jshs.2021.08.001_bib0009",
"volume": "12",
"year": "2001"
},
{
"DOI": "10.1016/S1473-3099(06)70523-0",
"article-title": "Obesity and infection",
"author": "Falagas",
"doi-asserted-by": "crossref",
"first-page": "438",
"journal-title": "Lancet Infect Dis",
"key": "10.1016/j.jshs.2021.08.001_bib0010",
"volume": "6",
"year": "2006"
},
{
"DOI": "10.1016/j.jsams.2021.05.011",
"article-title": "Association of physical activity levels and the prevalence of COVID-19-associated hospitalization",
"author": "de Souza",
"doi-asserted-by": "crossref",
"first-page": "913",
"journal-title": "J Sci Med Sport",
"key": "10.1016/j.jshs.2021.08.001_bib0011",
"volume": "24",
"year": "2021"
},
{
"DOI": "10.1177/1474515120921986",
"article-title": "Subjective reports of physical activity levels and sedentary time prior to hospital admission can predict utilization of hospital care and all-cause mortality among patients with cardiovascular disease",
"author": "Ek",
"doi-asserted-by": "crossref",
"first-page": "697",
"journal-title": "Eur J Cardiovasc Nurs",
"key": "10.1016/j.jshs.2021.08.001_bib0012",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1136/bjsm.2008.057216",
"article-title": "Does physical activity reduce seniors' need for healthcare? A study of 24,281 Canadians",
"author": "Woolcott",
"doi-asserted-by": "crossref",
"first-page": "902",
"journal-title": "Br J Sports Med",
"key": "10.1016/j.jshs.2021.08.001_bib0013",
"volume": "44",
"year": "2010"
}
],
"reference-count": 13,
"references-count": 13,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S2095254621000946"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Physical Therapy, Sports Therapy and Rehabilitation",
"Orthopedics and Sports Medicine"
],
"subtitle": [],
"title": "No independent associations between physical activity and clinical outcomes among hospitalized patients with moderate to severe COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "10"
}
