Protective role of physical activity patterns prior to COVID-19 confinement with the severity/duration of respiratory pathologies consistent with COVID-19 symptoms in Spanish populations
et al., Research in Sports Medicine, doi:10.1080/15438627.2021.1937166, Jun 2021
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
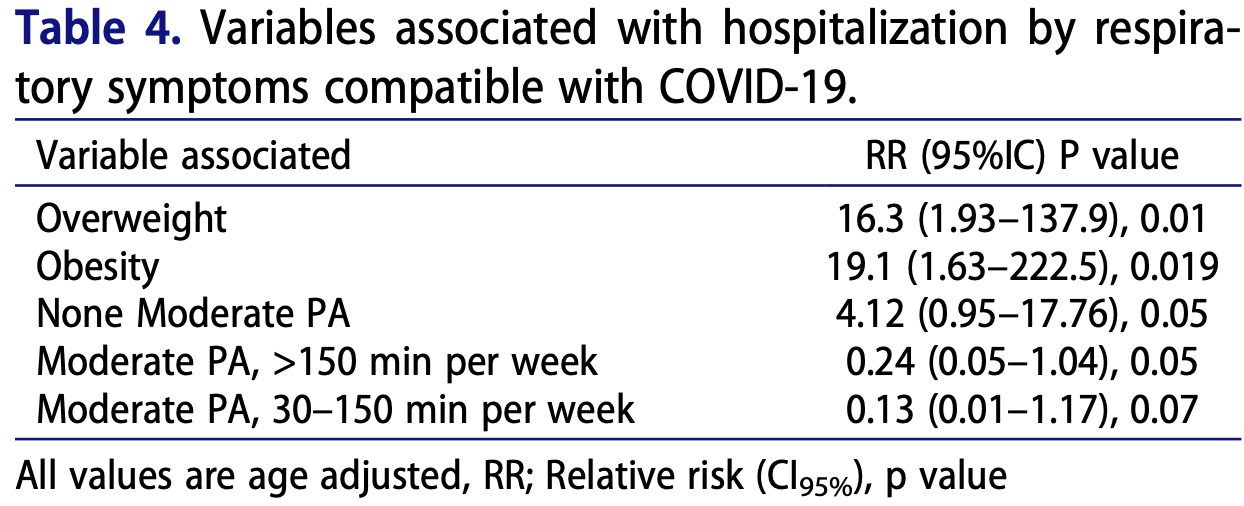
Retrospective 420 people in Spain, showing lower risk of COVID-19 hospitalization with a history of physical activity.
|
risk of hospitalization, 76.0% lower, OR 0.24, p = 0.05, moderate physical activity, >150 min per week, RR approximated with OR.
|
|
risk of hospitalization, 87.0% lower, OR 0.13, p = 0.07, moderate physical activity, 30-150 min per week, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Latorre-Román et al., 15 Jun 2021, retrospective, Spain, peer-reviewed, survey, 7 authors.
Protective role of physical activity patterns prior to COVID-19 confinement with the severity/duration of respiratory pathologies consistent with COVID-19 symptoms in Spanish populations
Research in Sports Medicine, doi:10.1080/15438627.2021.1937166
The main purpose of the present study was to determine the association of physical activity (PA) patterns prior to COVID-19 confinement with severe respiratory distress consistent with COVID-19 symptoms. Participants were recruited by sending a survey through various social network channels via the snowball method. A voluntary sample of 420 individuals consisting of 199 men and 221 women from the Spanish national territory participated in this study. Some factors, such as being overweight and obese were related to the presence of a greater number of symptoms associated with COVID-19. Interestingly, it was observed that not performing moderate or vigorous PA increased the risk of COVID-19 symptoms. Consequently, when the effect of the practise of PA was evaluated in terms of the number of practises per week and in minutes per practise per week, a protective effect was observed, where moderate PA >150 min per week reported an inverse association with hospitalization for respiratory symptoms (RR: 95%CI: 0.24, 0.05-1.04, P = 0.05). Likewise, overweight (RR: 16.3, 95%CI: 1.93-137.9, P = 0.01), obesity (RR: 19.1, 95%CI: 1.63-222.5, P = 0.019) and non-performance of moderate PA (RR: 4.12, 95%CI; 0.95-17.76, P = 0.05) reported positive associations with hospitalization for respiratory symptoms. Thus, the practise of moderate PA (>150 min per week) is a protective factor against hospitalization for respiratory symptoms consistent withCOVID-19 symptoms.
References
Adhikari, Meng, Wu, Mao, Ye et al., Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: A scoping review, Infectious Diseases of Poverty, doi:10.1186/s40249-020-00646-x
Baltar, Brunet, Social research 2.0: Virtual snowball sampling method using Facebook, Internet Research, doi:10.1108/10662241211199960
Brawner, Ehrman, Bole, Kerrigan, Parikh et al., Maximal exercise capacity is inversely related to hospitalization secondary to coronavirus disease 2019, Mayo Clinic Proceedings, doi:10.1016/j.mayocp.2020.10.003
Campbell, Turner, Debunking the myth of exercise-induced immune suppression: Redefining the impact of exercise on immunological health across the lifespan, Frontiers in Immunology, doi:10.3389/fimmu.2018.00648
Cancela, Ayán, Vila, Gutiérrez, Santiago, Validez de Constructo del Cuestionario Internacional de Actividad Física en Universitarios Españoles, Revista Iberoamericana de Diagnóstico y Evaluación Psicológica, doi:10.1007/10.21865/RIDEP52.3.01
Castañeda-Babarro, Arbillaga-Etxarri, Gutiérrez-Santamaría, Coca, Physical activity change during COVID-19 confinement, International Journal of Environmental Research and Public Health, doi:10.3390/ijerph17186878
Da Silveira, Da Silva Fagundes, Bizuti, Starck, Rossi et al., Physical exercise as a tool to help the immune system against COVID-19: An integrative review of the current literature, Clinical and Experimental Medicine, doi:10.1007/s10238-020-00650-3
Damiot, Pinto, Turner, Gualano, Immunological implications of physical inactivity among older adults during the COVID-19 pandemic, Gerontology, doi:10.1159/000509216
España, Fernández-Lázaro, González-Bernal, Sánchez-Serrano, Navascués et al., Physical exercise as a multimodal tool for COVID-19: Could it be used as a preventive strategy, International Journal of Environmental Research and Public Health, doi:10.3390/ijerph17228496
Goethals, Barth, Guyot, Hupin, Celarier et al., Impact of home quarantine on physical activity among older adults living at home during the COVID-19 pandemic: Qualitative interview study, JMIR Aging, doi:10.2196/19007
Hamer, Kivimäki, Gale, Batty, Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK, Brain, Behavior, and Immunity, doi:10.1016/j.bbi.2020.05.059
Heffernan, Ranadive, Jae, Exercise as medicine for COVID-19: On PPAR with emerging pharmacotherapy, Medical Hypotheses, doi:10.1016/j.mehy.2020.110197
Jans, Meyers, Fricker, Social science survey methodology training: Understanding the past and assessing the present to shape our future, Survey Practice, doi:10.29115/SP-2015-0007
Lau, Ng, Jones, Lee, Siu et al., A randomised controlled trial of the effectiveness of an exercise training program in patients recovering from severe acute respiratory syndrome, Australian Journal of Physiotherapy, doi:10.1016/S0004-9514(05)70002-7
Luzi, Radaelli, Influenza and obesity: Its odd relationship and the lessons for COVID-19 pandemic, Acta Diabetologica, doi:10.1007/s00592-020-01522-8
López-Bueno, Calatayud, Andersen, Balsalobre-Fernández, Casaña et al., Immediate impact of the COVID-19 confinement on physical activity levels in Spanish adults, Sustainability, doi:10.3390/su12145708
Magdy Beshbishy, Hetta, Hussein, Saati, Uba et al., Factors associated with increased morbidity and mortality of obese and overweight COVID-19 patients, Biology, doi:10.3390/biology9090280
Mattioli, Ballerini Puviani, Lifestyle at time of COVID-19: How could quarantine affect cardiovascular risk, American Journal of Lifestyle Medicine, doi:10.1177/1559827620918808
Nigro, Polito, Alfieri, Mancini, Imperlini et al., Molecular mechanisms involved in the positive effects of physical activity on coping with COVID-19, European Journal of Applied Physiology, doi:10.1007/s00421-020-04484-5
Rajkumar, COVID-19 and mental health: A review of the existing literature, Asian Journal of Psychiatry, doi:10.1016/j.ajp.2020.102066
Reyes-Olavarría, Latorre-Román, Guzmán-Guzmán, Jerez-Mayorga, Caamaño-Navarrete et al., Positive and negative changes in food habits, physical activity patterns, and weight status during COVID-19 confinement: Associated factors in the Chilean population, International Journal of Environmental Research and Public Health, doi:10.3390/ijerph17155431
Rooney, Webster, Paul, Systematic review of changes and recovery in physical function and fitness after severe acute respiratory syndrome-related coronavirus infection: Implications for COVID-19 rehabilitation, Physical Therapy, doi:10.1093/ptj/pzaa129
Salgado-Aranda, Pérez-Castellano, Núñez-Gil, Orozco, Torres-Esquivel et al., Influence of baseline physical activity as a modifying factor on COVID-19 mortality: A single-center, retrospective study, Infectious Diseases and Therapy, doi:10.1007/s40121-021-00418-6
Sallis, Young, Tartof, Sallis, Sall et al., Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: A study in 48 440 adult patients, British Journal of Sports Medicine, doi:10.1136/bjsports-2021-104080
Sanchis-Gomar, Lavie, Mehra, Henry, Lippi, Obesity and outcomes in COVID-19: When an epidemic and pandemic collide, Mayo Clinic Proceedings, doi:10.1016/j.mayocp.2020.05.006
Simpson, Campbell, Gleeson, Krüger, Nieman et al., Can exercise affect immune function to increase susceptibility to infection?, Exercise Immunology Review
Sánchez-Sánchez, Ramírez-Vargas, Avellaneda-López, Orellana-Pecino, García-Marín et al., Eating habits and physical activity of the Spanish population during the COVID-19 pandemic period, Nutrients, doi:10.3390/nu12092826
Vardavas, Nikitara, COVID-19 and smoking: A systematic review of the evidence, Tobacco Induced Diseases, doi:10.18332/tid/119324
Warburton, Nicol, Bredin, Health benefits of physical activity: The evidence, Canadian Medical Association Journal, doi:10.1503/cmaj.051351
Woods, Hutchinson, Powers, Roberts, Gomez-Cabrera et al., The COVID-19 pandemic and physical activity, Sports Medicine and Health Science, doi:10.1016/j.smhs.2020.05.006
Zachary, Brianna, Brianna, Garrett, Jade et al., Selfquarantine and weight gain related risk factors during the COVID-19 pandemic, Obesity Research & Clinical Practice, doi:10.1016/j.orcp.2020.05.004
Zbinden-Foncea, Francaux, Deldicque, Hawley, Does high cardiorespiratory fitness confer some protection against proinflammatory responses after infection by SARS-CoV-2?, Obesity, doi:10.1002/oby.22849
DOI record:
{
"DOI": "10.1080/15438627.2021.1937166",
"ISSN": [
"1543-8627",
"1543-8635"
],
"URL": "http://dx.doi.org/10.1080/15438627.2021.1937166",
"alternative-id": [
"10.1080/15438627.2021.1937166"
],
"assertion": [
{
"label": "Peer Review Statement",
"name": "peerreview_statement",
"order": 1,
"value": "The publishing and review policy for this title is described in its Aims & Scope."
},
{
"URL": "http://www.tandfonline.com/action/journalInformation?show=aimsScope&journalCode=gspm20",
"label": "Aim & Scope",
"name": "aims_and_scope_url",
"order": 2,
"value": "http://www.tandfonline.com/action/journalInformation?show=aimsScope&journalCode=gspm20"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2021-01-19"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "2021-05-11"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 3,
"value": "2021-06-15"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-0517-3627",
"affiliation": [
{
"name": "Department of Didactics of Corporal Expression, University of Jaen, Spain"
}
],
"authenticated-orcid": false,
"family": "Latorre-Román",
"given": "Pedro Ángel",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0003-1535-4226",
"affiliation": [
{
"name": "Faculty of Chemical-Biological Sciences, Universidad Autónoma De Guerrero, Guerrero, México"
}
],
"authenticated-orcid": false,
"family": "Guzmán-Guzmán",
"given": "Iris Paola",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9952-993X",
"affiliation": [
{
"name": "Department of Physical Education, Sports and Recreation. Universidad De La Frontera, Temuco, Chile"
}
],
"authenticated-orcid": false,
"family": "Delgado-Floody",
"given": "Pedro",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7465-8345",
"affiliation": [
{
"name": "Department of Didactics of Corporal Expression, University of Jaen, Spain"
}
],
"authenticated-orcid": false,
"family": "Herrador Sanchez",
"given": "Julio",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2550-6695",
"affiliation": [
{
"name": "Department of Nutrition, Exercise and Sports (NEXS), University of Copenhagen, Copenhagen, Denmark"
}
],
"authenticated-orcid": false,
"family": "Aragón-Vela",
"given": "Jerónimo",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7518-8234",
"affiliation": [
{
"name": "Department of Physical Education, Sports and Recreation. Universidad De La Frontera, Temuco, Chile"
},
{
"name": "Department of Physical Education and Sports, University of Granada, Spain"
}
],
"authenticated-orcid": false,
"family": "García Pinillos",
"given": "Felipe",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0250-0717",
"affiliation": [
{
"name": "Department of Didactics of Corporal Expression, University of Jaen, Spain"
}
],
"authenticated-orcid": false,
"family": "Párraga Montilla",
"given": "Juan A.",
"sequence": "additional"
}
],
"container-title": [
"Research in Sports Medicine"
],
"content-domain": {
"crossmark-restriction": true,
"domain": [
"www.tandfonline.com"
]
},
"created": {
"date-parts": [
[
2021,
6,
15
]
],
"date-time": "2021-06-15T11:56:39Z",
"timestamp": 1623758199000
},
"deposited": {
"date-parts": [
[
2021,
6,
15
]
],
"date-time": "2021-06-15T11:56:53Z",
"timestamp": 1623758213000
},
"indexed": {
"date-parts": [
[
2022,
3,
30
]
],
"date-time": "2022-03-30T06:28:01Z",
"timestamp": 1648621681028
},
"is-referenced-by-count": 3,
"issn-type": [
{
"type": "print",
"value": "1543-8627"
},
{
"type": "electronic",
"value": "1543-8635"
}
],
"issued": {
"date-parts": [
[
2021,
6,
15
]
]
},
"language": "en",
"link": [
{
"URL": "https://www.tandfonline.com/doi/pdf/10.1080/15438627.2021.1937166",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "301",
"original-title": [],
"page": "1-12",
"prefix": "10.1080",
"published": {
"date-parts": [
[
2021,
6,
15
]
]
},
"published-online": {
"date-parts": [
[
2021,
6,
15
]
]
},
"publisher": "Informa UK Limited",
"reference": [
{
"DOI": "10.1186/s40249-020-00646-x",
"doi-asserted-by": "publisher",
"key": "cit0001"
},
{
"DOI": "10.1108/10662241211199960",
"doi-asserted-by": "publisher",
"key": "cit0002"
},
{
"author": "Brawner C. A.",
"journal-title": "Mayo Clinic Proceedings",
"key": "cit0003",
"year": "2020"
},
{
"author": "Campbell J. P.",
"journal-title": "Frontiers in Immunology",
"key": "cit0004",
"volume": "9",
"year": "2018"
},
{
"author": "Cancela J. M.",
"first-page": "5",
"issue": "52",
"journal-title": "Revista Iberoamericana de Diagnóstico y Evaluación Psicológica",
"key": "cit0005",
"volume": "3",
"year": "2019"
},
{
"DOI": "10.3390/ijerph17186878",
"doi-asserted-by": "publisher",
"key": "cit0006"
},
{
"author": "Da Silveira M. P.",
"journal-title": "Clinical and Experimental Medicine",
"key": "cit0007",
"year": "2020"
},
{
"DOI": "10.1159/000509216",
"author": "Damiot A.",
"doi-asserted-by": "crossref",
"first-page": "431",
"issue": "5",
"journal-title": "Gerontology",
"key": "cit0008",
"volume": "66",
"year": "2020"
},
{
"key": "cit0009",
"unstructured": "España, E. C. (2020). Informe sobre la situación de COVID-19 en España."
},
{
"DOI": "10.3390/ijerph17228496",
"doi-asserted-by": "publisher",
"key": "cit0010"
},
{
"DOI": "10.2196/19007",
"doi-asserted-by": "publisher",
"key": "cit0011"
},
{
"DOI": "10.1016/j.bbi.2020.05.059",
"doi-asserted-by": "publisher",
"key": "cit0012"
},
{
"DOI": "10.1016/j.mehy.2020.110197",
"author": "Heffernan K. S.",
"doi-asserted-by": "crossref",
"first-page": "110197",
"journal-title": "Medical Hypotheses",
"key": "cit0013",
"volume": "143",
"year": "2020"
},
{
"DOI": "10.29115/SP-2015-0007",
"author": "Jans M.",
"doi-asserted-by": "crossref",
"first-page": "1",
"issue": "2",
"journal-title": "Survey Practice",
"key": "cit0014",
"volume": "8",
"year": "2015"
},
{
"DOI": "10.1016/S0004-9514(05)70002-7",
"doi-asserted-by": "publisher",
"key": "cit0015"
},
{
"DOI": "10.3390/su12145708",
"doi-asserted-by": "publisher",
"key": "cit0016"
},
{
"DOI": "10.1007/s00592-020-01522-8",
"doi-asserted-by": "publisher",
"key": "cit0017"
},
{
"DOI": "10.3390/biology9090280",
"author": "Magdy Beshbishy A.",
"doi-asserted-by": "crossref",
"first-page": "280",
"issue": "9",
"journal-title": "Biology",
"key": "cit0018",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1177/1559827620918808",
"author": "Mattioli A. V.",
"doi-asserted-by": "crossref",
"first-page": "240",
"issue": "3",
"journal-title": "American Journal of Lifestyle Medicine",
"key": "cit0019",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1007/s00421-020-04484-5",
"author": "Nigro E.",
"doi-asserted-by": "crossref",
"issue": "12",
"journal-title": "European Journal of Applied Physiology",
"key": "cit0020",
"volume": "120",
"year": "2020"
},
{
"DOI": "10.1016/j.ajp.2020.102066",
"doi-asserted-by": "publisher",
"key": "cit0021"
},
{
"DOI": "10.3390/ijerph17155431",
"doi-asserted-by": "publisher",
"key": "cit0022"
},
{
"DOI": "10.1093/ptj/pzaa129",
"doi-asserted-by": "publisher",
"key": "cit0023"
},
{
"DOI": "10.1007/s40121-021-00418-6",
"author": "Salgado-Aranda R.",
"doi-asserted-by": "crossref",
"issue": "2",
"journal-title": "Infectious Diseases and Therapy",
"key": "cit0024",
"volume": "10",
"year": "2021"
},
{
"author": "Sallis R.",
"journal-title": "British Journal of Sports Medicine",
"key": "cit0025",
"year": "2021"
},
{
"DOI": "10.3390/nu12092826",
"doi-asserted-by": "publisher",
"key": "cit0026"
},
{
"DOI": "10.1016/j.mayocp.2020.05.006",
"doi-asserted-by": "publisher",
"key": "cit0027"
},
{
"author": "Simpson R. J.",
"first-page": "8",
"journal-title": "Exercise Immunology Review",
"key": "cit0028",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.18332/tid/119324",
"doi-asserted-by": "publisher",
"key": "cit0029"
},
{
"DOI": "10.1503/cmaj.051351",
"doi-asserted-by": "publisher",
"key": "cit0030"
},
{
"DOI": "10.1016/j.smhs.2020.05.006",
"doi-asserted-by": "publisher",
"key": "cit0031"
},
{
"author": "World Health Organisation",
"key": "cit0032",
"volume-title": "Coronavirus disease (COVID-2019) situation reports",
"year": "2020"
},
{
"key": "cit0033",
"unstructured": "World Health Organization. (2003). Diet, nutrition and the prevention of chronic diseases. World Health Organization Technical Report Series, 916, i-viii-1-149-backcover. https://doi.org/ISBN.92.4.120916.X 0512-3054 (NLM classification: QU 145)"
},
{
"author": "World Health Organization",
"key": "cit0034",
"volume-title": "Recomendaciones Mundiales sobre Actividad Física para la Salud",
"year": "2010"
},
{
"DOI": "10.1016/j.orcp.2020.05.004",
"author": "Zachary Z.",
"doi-asserted-by": "crossref",
"first-page": "210",
"issue": "3",
"journal-title": "Obesity Research & Clinical Practice",
"key": "cit0035",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1002/oby.22849",
"doi-asserted-by": "publisher",
"key": "cit0036"
}
],
"reference-count": 36,
"references-count": 36,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.tandfonline.com/doi/full/10.1080/15438627.2021.1937166"
}
},
"score": 1,
"short-container-title": [
"Research in Sports Medicine"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Physical Therapy, Sports Therapy and Rehabilitation",
"Orthopedics and Sports Medicine"
],
"subtitle": [],
"title": [
"Protective role of physical activity patterns prior to COVID-19 confinement with the severity/duration of respiratory pathologies consistent with COVID-19 symptoms in Spanish populations"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1080/tandf_crossmark_01"
}
