Associations between physical activity prior to infection and COVID-19 disease severity and symptoms: results from the prospective Predi-COVID cohort study
et al., BMJ Open, doi:10.1136/bmjopen-2021-057863, NCT04380987, Apr 2022
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
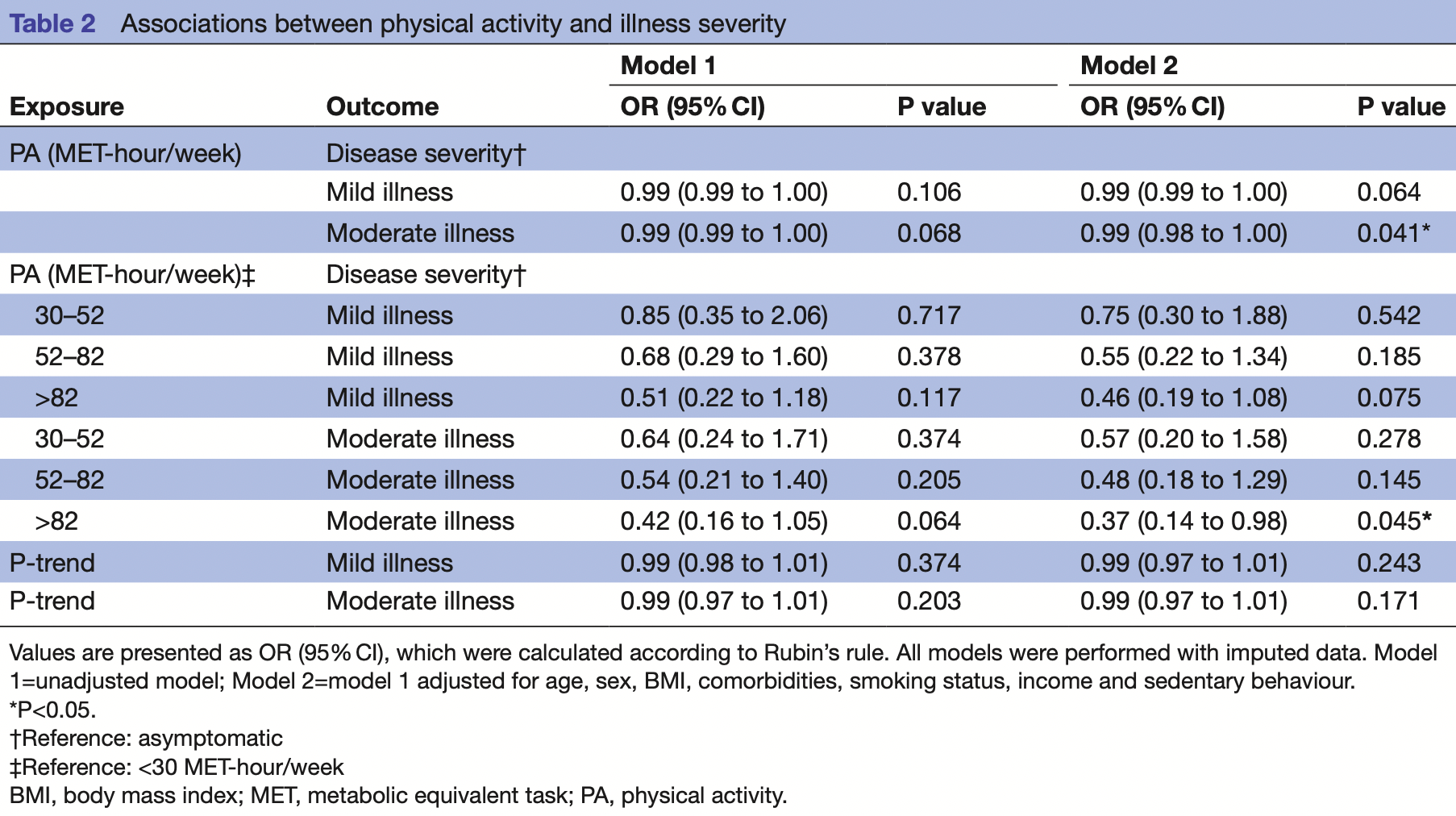
Retrospective 452 participants in Luxembourg, showing lower risk of moderate cases with higher physical activity.
|
risk of progression, 63.0% lower, OR 0.37, p = 0.045, high activity levels 115, low activity levels 108, moderate case, >82 vs. <30 MET-hour/week, RR approximated with OR.
|
|
risk of progression, 52.0% lower, OR 0.48, p = 0.14, high activity levels 116, low activity levels 108, moderate case, >52-82 vs. <30 MET-hour/week, RR approximated with OR.
|
|
risk of progression, 43.0% lower, OR 0.57, p = 0.28, high activity levels 113, low activity levels 108, moderate case, 30-52 vs. <30 MET-hour/week, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Malisoux et al., 29 Apr 2022, retrospective, Luxembourg, peer-reviewed, survey, median age 42.0, 6 authors, study period May 2020 - June 2021, trial NCT04380987 (history).
Associations between physical activity prior to infection and COVID-19 disease severity and symptoms: results from the prospective Predi-COVID cohort study
BMJ Open, doi:10.1136/bmjopen-2021-057863
Objective To investigate if the physical activity (PA) prior to infection is associated with the severity of the disease in patients positively tested for COVID-19, as well as with the most common symptoms. Design A cross-sectional study using baseline data from a prospective, hybrid cohort study (Predi-COVID) in Luxembourg. Data were collected from May 2020 to June 2021. Setting Real-life setting (at home) and hospitalised patients. Participants All volunteers aged >18 years with confirmed SARS-CoV-2 infection, as determined by reverse transcription-PCR, and having completed the PA questionnaire (n=452). Primary and secondary outcome measures The primary outcome was disease severity (asymptomatic, mild illness and moderate illness). The secondary outcomes were self-reported symptoms. Results From the 452 patients included, 216 (48%) were female, the median (IQR) age was 42 (31-51) years, 59 (13%) were classified as asymptomatic, 287 (63%) as mild illness and 106 (24%) as moderate illness. The most prevalent symptoms were fatigue (n=294; 65%), headache (n=281; 62%) and dry cough (n=241; 53%). After adjustment, the highest PA level was associated with a lower risk of moderate illness (OR 0.37; 95% CI 0.14 to 0.98, p=0.045), fatigue (OR 0.54; 95% CI 0.30 to 0.97, p=0.040), dry cough (OR 0.55; 95% CI 0.32 to 0.96, p=0.034) and chest pain (OR 0.32; 95% CI 0.14 to 0.77, p=0.010). Conclusions PA before COVID-19 infection was associated with a reduced risk of moderate illness severity and a reduced risk of experiencing fatigue, dry cough and chest pain, suggesting that engaging in PA may be an effective approach to minimise the severity of COVID-19. Trial registration number NCT04380987.
References
Ainsworth, Haskell, Whitt, Compendium of physical activities: an update of activity codes and Met intensities, Med Sci Sports Exerc, doi:10.1097/00005768-200009001-00009
Asano, Boisson, Onodi, X-linked recessive TLR7 deficiency in ~1% of men under 60 years old with life-threatening COVID-19, Sci Immunol, doi:10.1126/sciimmunol.abl4348
Bastard, Gervais, Voyer, Autoantibodies neutralizing type I IFNs are present in ~4% of uninfected individuals over 70 years old and account for ~20% of COVID-19 deaths, Sci Immunol, doi:10.1126/sciimmunol.abl4340
Bialek, Boundy, Bowen, Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19) -United States, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm6912e2
Brawner Ehrman, Bole, Inverse relationship of maximal exercise capacity to hospitalization secondary to coronavirus disease
Chastin, Abaraogu, Bourgois, Effects of regular physical activity on the immune system, vaccination and risk of community-acquired infectious disease in the general population: systematic review and meta-analysis, Sports Med, doi:10.1007/s40279-021-01466-1
Da, Mesquita, Silva Junior, Santana, Clinical manifestations of COVID-19 in the general population: systematic review, Wien Klin Wochenschr, doi:10.1007/s00508-020-01760-4
De Souza, Motta-Santos, Soares, Association of physical activity levels and the prevalence of COVID-19-associated hospitalization, J Sci Med Sport, doi:10.1016/j.jsams.2021.05.011
Fagherazzi, Fischer, Betsou, Protocol for a prospective, longitudinal cohort of people with COVID-19 and their household members to study factors associated with disease severity: the Predi-COVID study, BMJ Open, doi:10.1136/bmjopen-2020-041834
Fournier, Santos, Guillas, Recent recreational physical activity and breast cancer risk in postmenopausal women in the E3N cohort, Cancer Epidemiol Biomarkers Prev, doi:10.1158/1055-9965.EPI-14-0150
Gualano, Lemes, Silva, Association between physical activity and immunogenicity of an inactivated virus vaccine against SARS-CoV-2 in patients with autoimmune rheumatic diseases, Brain Behav Immun, doi:10.1016/j.bbi.2021.12.016
Hamer, Kivimäki, Gale, Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: a community-based cohort study of 387,109 adults in UK, Brain Behav Immun, doi:10.1016/j.bbi.2020.05.059
Hamer, Sabia, Batty, Physical activity and inflammatory markers over 10 years: follow-up in men and women from the Whitehall II cohort study, Circulation, doi:10.1161/CIRCULATIONAHA.112.103879
Izcovich, Ragusa, Tortosa, Prognostic factors for severity and mortality in patients infected with COVID-19: a systematic review, PLoS One, doi:10.1371/journal.pone.0241955
Jordan, Adab, Cheng, Covid-19: risk factors for severe disease and death
Lacombe, Armstrong, Wright, The impact of physical activity and an additional behavioural risk factor on cardiovascular disease, cancer and all-cause mortality: a systematic review, BMC Public Health, doi:10.1186/s12889-019-7030-8
Laddu, Lavie, Phillips, Physical activity for immunity protection: Inoculating populations with healthy living medicine in preparation for the next pandemic, Prog Cardiovasc Dis, doi:10.1016/j.pcad.2020.04.006
Lavie, Ozemek, Carbone, Sedentary behavior, exercise, and cardiovascular health, Circ Res, doi:10.1161/CIRCRESAHA.118.312669
Lee, Lee, Moon, Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study, Br J Sports Med, doi:10.1136/bjsports-2021-104203
Lee, Shiroma, Lobelo, Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy, Lancet, doi:10.1016/S0140-6736(12)61031-9
Liu, Kuo, Shih, COVID-19: the first documented coronavirus pandemic in history, Biomed J, doi:10.1016/j.bj.2020.04.007
Macdonald, Madika, Lajous, Associations between physical activity and incident hypertension across strata of body mass index: a prospective investigation in a large cohort of French women, J Am Heart Assoc, doi:10.1161/JAHA.119.015121
Monteiro, Immunoglobulin A as an anti-inflammatory agent, Clin Exp Immunol, doi:10.1111/cei.12531
Netea, Giamarellos-Bourboulis, Domínguez-Andrés, Trained immunity: a tool for reducing susceptibility to and the severity of SARS-CoV-2 infection, Cell, doi:10.1016/j.cell.2020.04.042
Nieman, Coronavirus disease-2019: a tocsin to our aging, unfit, corpulent, and immunodeficient Society, J Sport Health Sci, doi:10.1016/j.jshs.2020.05.001
Nieman, Wentz, The compelling link between physical activity and the body's defense system, J Sport Health Sci, doi:10.1016/j.jshs.2018.09.009
Pascoe, Singh, Edwards, The effects of exercise on vaccination responses: a review of chronic and acute exercise interventions in humans, Brain Behav Immun, doi:10.1016/j.bbi.2013.10.003
Piercy, Troiano, Ballard, The physical activity guidelines for Americans, JAMA, doi:10.1001/jama.2018.14854
Rubin, Multiple imputation for nonresponse in surveys
Sallis, Young, Tartof, Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients, Br J Sports Med, doi:10.1136/bjsports-2021-104080
Schwellnus, Soligard, Alonso, How much is too much? (Part 2) International Olympic Committee consensus statement on load in sport and risk of illness, Br J Sports Med, doi:10.1136/bjsports-2016-096572
Simpson, Kunz, Agha, Exercise and the regulation of immune functions, Prog Mol Biol Transl Sci, doi:10.1016/bs.pmbts.2015.08.001
Siu, Campitelli, Kwong, Physical activity and influenzacoded outpatient visits, a population-based cohort study, PLoS One, doi:10.1371/journal.pone.0039518
Stamatakis, Lee, Does strength-promoting exercise confer unique health benefits? A pooled analysis of data on 11 population cohorts with all-cause, cancer, and cardiovascular mortality endpoints, Am J Epidemiol, doi:10.1093/aje/kwx345
Svan, Groothuis-Oudshoorn, mice : Multivariate Imputation by Chained Equations in R, J Stat Softw, doi:10.18637/jss.v045.i03
Tavakol, Ghannadi, Tabesh, Relationship between physical activity, healthy lifestyle and COVID-19 disease severity; a cross-sectional study, Z Gesundh Wiss, doi:10.1007/s10389-020-01468-9
Von Elm, Altman, Egger, The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies, PLoS Med, doi:10.1371/journal.pmed.0040296
Wahid, Manek, Nichols, Quantifying the association between physical activity and cardiovascular disease and diabetes: a systematic review and meta-analysis, J Am Heart Assoc, doi:10.1161/JAHA.115.002495
Wong, Lai, Ou, Is exercise protective against influenza-associated mortality?, PLoS One, doi:10.1371/journal.pone.0002108
Yuan, Huang, Chen, Does pre-existent physical inactivity have a role in the severity of COVID-19?, Ther Adv Respir Dis, doi:10.1177/17534666211025221
Yuki, Fujiogi, Koutsogiannaki, COVID-19 pathophysiology: a review, Clin Immunol, doi:10.1016/j.clim.2020.108427
Zhang, Chen, Ren, Pre-Operative exercise therapy triggers anti-inflammatory trained immunity of Kupffer cells through metabolic reprogramming, Nat Metab, doi:10.1038/s42255-021-00402-x
Zhang, Li, Sun, Physical activity and COVID-19: an observational and Mendelian randomisation study, J Glob Health, doi:10.7189/jogh.10.020514
DOI record:
{
"DOI": "10.1136/bmjopen-2021-057863",
"ISSN": [
"2044-6055",
"2044-6055"
],
"URL": "http://dx.doi.org/10.1136/bmjopen-2021-057863",
"abstract": "<jats:sec><jats:title>Objective</jats:title><jats:p>To investigate if the physical activity (PA) prior to infection is associated with the severity of the disease in patients positively tested for COVID-19, as well as with the most common symptoms.</jats:p></jats:sec><jats:sec><jats:title>Design</jats:title><jats:p>A cross-sectional study using baseline data from a prospective, hybrid cohort study (Predi-COVID) in Luxembourg. Data were collected from May 2020 to June 2021.</jats:p></jats:sec><jats:sec><jats:title>Setting</jats:title><jats:p>Real-life setting (at home) and hospitalised patients.</jats:p></jats:sec><jats:sec><jats:title>Participants</jats:title><jats:p>All volunteers aged >18 years with confirmed SARS-CoV-2 infection, as determined by reverse transcription-PCR, and having completed the PA questionnaire (n=452).</jats:p></jats:sec><jats:sec><jats:title>Primary and secondary outcome measures</jats:title><jats:p>The primary outcome was disease severity (asymptomatic, mild illness and moderate illness). The secondary outcomes were self-reported symptoms.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>From the 452 patients included, 216 (48%) were female, the median (IQR) age was 42 (31–51) years, 59 (13%) were classified as asymptomatic, 287 (63%) as mild illness and 106 (24%) as moderate illness. The most prevalent symptoms were fatigue (n=294; 65%), headache (n=281; 62%) and dry cough (n=241; 53%). After adjustment, the highest PA level was associated with a lower risk of moderate illness (OR 0.37; 95% CI 0.14 to 0.98, p=0.045), fatigue (OR 0.54; 95% CI 0.30 to 0.97, p=0.040), dry cough (OR 0.55; 95% CI 0.32 to 0.96, p=0.034) and chest pain (OR 0.32; 95% CI 0.14 to 0.77, p=0.010).</jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p>PA before COVID-19 infection was associated with a reduced risk of moderate illness severity and a reduced risk of experiencing fatigue, dry cough and chest pain, suggesting that engaging in PA may be an effective approach to minimise the severity of COVID-19.</jats:p></jats:sec><jats:sec><jats:title>Trial registration number</jats:title><jats:p><jats:ext-link xmlns:xlink=\"http://www.w3.org/1999/xlink\" ext-link-type=\"clintrialgov\" xlink:href=\"NCT04380987\">NCT04380987</jats:ext-link>.</jats:p></jats:sec>",
"alternative-id": [
"10.1136/bmjopen-2021-057863"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-6601-5630",
"affiliation": [],
"authenticated-orcid": false,
"family": "Malisoux",
"given": "Laurent",
"sequence": "first"
},
{
"affiliation": [],
"family": "Backes",
"given": "Anne",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fischer",
"given": "Aurélie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Aguayo",
"given": "Gloria",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ollert",
"given": "Markus",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fagherazzi",
"given": "Guy",
"sequence": "additional"
}
],
"clinical-trial-number": [
{
"clinical-trial-number": "nct04380987",
"registry": "10.18810/clinical-trials-gov"
}
],
"container-title": "BMJ Open",
"container-title-short": "BMJ Open",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2022,
4,
30
]
],
"date-time": "2022-04-30T01:51:44Z",
"timestamp": 1651283504000
},
"deposited": {
"date-parts": [
[
2022,
6,
30
]
],
"date-time": "2022-06-30T18:06:53Z",
"timestamp": 1656612413000
},
"funder": [
{
"award": [
"N/A"
],
"name": "Luxembourg Institute of Health"
},
{
"DOI": "10.13039/501100001866",
"award": [
"14716273"
],
"doi-asserted-by": "publisher",
"name": "Fonds National de la Recherche Luxembourg"
},
{
"award": [
"N/A"
],
"name": "André Losch Fondation"
},
{
"DOI": "10.13039/501100008530",
"award": [
"Convention 2018-04-026-21"
],
"doi-asserted-by": "publisher",
"name": "European Regional Development Fund"
}
],
"indexed": {
"date-parts": [
[
2022,
6,
30
]
],
"date-time": "2022-06-30T18:40:47Z",
"timestamp": 1656614447883
},
"is-referenced-by-count": 1,
"issue": "4",
"issued": {
"date-parts": [
[
2022,
4
]
]
},
"journal-issue": {
"issue": "4",
"published-online": {
"date-parts": [
[
2022,
4,
29
]
]
},
"published-print": {
"date-parts": [
[
2022,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "unspecified",
"delay-in-days": 27,
"start": {
"date-parts": [
[
2022,
4,
28
]
],
"date-time": "2022-04-28T00:00:00Z",
"timestamp": 1651104000000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/bmjopen-2021-057863",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "e057863",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2022,
4
]
]
},
"published-online": {
"date-parts": [
[
2022,
4,
29
]
]
},
"published-print": {
"date-parts": [
[
2022,
4
]
]
},
"publisher": "BMJ",
"reference": [
{
"DOI": "10.1016/j.bj.2020.04.007",
"article-title": "COVID-19: the first documented coronavirus pandemic in history",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "328",
"journal-title": "Biomed J",
"key": "2022063010225462000_12.4.e057863.1",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1136/bmjopen-2020-041834",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.2"
},
{
"DOI": "10.1371/journal.pone.0241955",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.3"
},
{
"DOI": "10.1126/sciimmunol.abl4340",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.4"
},
{
"DOI": "10.1126/sciimmunol.abl4348",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.5"
},
{
"DOI": "10.1136/bmj.m1198",
"doi-asserted-by": "crossref",
"key": "2022063010225462000_12.4.e057863.6",
"unstructured": "Jordan RE , Adab P , Cheng K . Covid-19: risk factors for severe disease and death. British Medical Journal Publishing Group, 2020."
},
{
"DOI": "10.1016/S0140-6736(12)61031-9",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.7"
},
{
"DOI": "10.1186/s12889-019-7030-8",
"article-title": "The impact of physical activity and an additional behavioural risk factor on cardiovascular disease, cancer and all-cause mortality: a systematic review",
"author": "Lacombe",
"doi-asserted-by": "crossref",
"journal-title": "BMC Public Health",
"key": "2022063010225462000_12.4.e057863.8",
"volume": "19",
"year": "2019"
},
{
"DOI": "10.1161/JAHA.115.002495",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.9"
},
{
"DOI": "10.15585/mmwr.mm6912e2",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.10"
},
{
"DOI": "10.1161/CIRCRESAHA.118.312669",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.11"
},
{
"DOI": "10.1007/s40279-021-01466-1",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.12"
},
{
"DOI": "10.1016/j.clim.2020.108427",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.13"
},
{
"DOI": "10.1007/s00508-020-01760-4",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.14"
},
{
"DOI": "10.1136/bjsports-2021-104203",
"article-title": "Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study",
"author": "Lee",
"doi-asserted-by": "crossref",
"journal-title": "Br J Sports Med",
"key": "2022063010225462000_12.4.e057863.15",
"year": "2021"
},
{
"DOI": "10.1136/bjsports-2021-104080",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.16"
},
{
"DOI": "10.1371/journal.pmed.0040296",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.17"
},
{
"key": "2022063010225462000_12.4.e057863.18",
"unstructured": "National Institutes of Health (NIH) . Clinical spectrum of SARS-CoV-2 infection, 2021. Available: https://www.covid19treatmentguidelines.nih.gov/overview/clinical-spectrum/ [Accessed 23 Jul 2021]."
},
{
"DOI": "10.1161/JAHA.119.015121",
"article-title": "Associations between physical activity and incident hypertension across strata of body mass index: a prospective investigation in a large cohort of French women",
"author": "MacDonald",
"doi-asserted-by": "crossref",
"journal-title": "J Am Heart Assoc",
"key": "2022063010225462000_12.4.e057863.19",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1097/00005768-200009001-00009",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.20"
},
{
"key": "2022063010225462000_12.4.e057863.21"
},
{
"key": "2022063010225462000_12.4.e057863.22",
"unstructured": "Rubin DB . Multiple imputation for nonresponse in surveys. John Wiley & Sons, 2004."
},
{
"DOI": "10.1016/j.bbi.2020.05.059",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.23"
},
{
"DOI": "10.1177/17534666211025221",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.24"
},
{
"DOI": "10.1016/j.jsams.2021.05.011",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.25"
},
{
"DOI": "10.1001/jama.2018.14854",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.26"
},
{
"DOI": "10.7189/jogh.10.020514",
"article-title": "Physical activity and COVID-19: an observational and Mendelian randomisation study",
"author": "Zhang",
"doi-asserted-by": "crossref",
"journal-title": "J Glob Health",
"key": "2022063010225462000_12.4.e057863.27",
"volume": "10",
"year": "2020"
},
{
"article-title": "Relationship between physical activity, healthy lifestyle and COVID-19 disease severity; a cross-sectional study",
"author": "Tavakol",
"first-page": "1",
"journal-title": "Z Gesundh Wiss",
"key": "2022063010225462000_12.4.e057863.28",
"year": "2021"
},
{
"DOI": "10.1016/j.pcad.2020.04.006",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.29"
},
{
"DOI": "10.1371/journal.pone.0002108",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.30"
},
{
"DOI": "10.1371/journal.pone.0039518",
"article-title": "Physical activity and influenza-coded outpatient visits, a population-based cohort study",
"author": "Siu",
"doi-asserted-by": "crossref",
"journal-title": "PLoS One",
"key": "2022063010225462000_12.4.e057863.31",
"volume": "7",
"year": "2012"
},
{
"DOI": "10.1016/j.jshs.2020.05.001",
"article-title": "Coronavirus disease-2019: a tocsin to our aging, unfit, corpulent, and immunodeficient Society",
"author": "Nieman",
"doi-asserted-by": "crossref",
"first-page": "293",
"journal-title": "J Sport Health Sci",
"key": "2022063010225462000_12.4.e057863.32",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1016/j.mayocp.2020.10.003",
"doi-asserted-by": "crossref",
"key": "2022063010225462000_12.4.e057863.33",
"unstructured": "Brawner CA , Ehrman JK , Bole S , et al , eds. Inverse relationship of maximal exercise capacity to hospitalization secondary to coronavirus disease 2019. Mayo Clinic Proceedings. Elsevier, 2021."
},
{
"DOI": "10.1016/bs.pmbts.2015.08.001",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.34"
},
{
"DOI": "10.1016/j.jshs.2018.09.009",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.35"
},
{
"DOI": "10.1161/CIRCULATIONAHA.112.103879",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.36"
},
{
"DOI": "10.1111/cei.12531",
"article-title": "Immunoglobulin A as an anti-inflammatory agent",
"author": "Monteiro",
"doi-asserted-by": "crossref",
"first-page": "108",
"journal-title": "Clin Exp Immunol",
"key": "2022063010225462000_12.4.e057863.37",
"volume": "178 Suppl 1",
"year": "2014"
},
{
"DOI": "10.1016/j.bbi.2013.10.003",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.38"
},
{
"DOI": "10.1016/j.bbi.2021.12.016",
"article-title": "Association between physical activity and immunogenicity of an inactivated virus vaccine against SARS-CoV-2 in patients with autoimmune rheumatic diseases",
"author": "Gualano",
"doi-asserted-by": "crossref",
"first-page": "49",
"journal-title": "Brain Behav Immun",
"key": "2022063010225462000_12.4.e057863.39",
"volume": "101",
"year": "2022"
},
{
"DOI": "10.1038/s42255-021-00402-x",
"article-title": "Pre-Operative exercise therapy triggers anti-inflammatory trained immunity of Kupffer cells through metabolic reprogramming",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "843",
"journal-title": "Nat Metab",
"key": "2022063010225462000_12.4.e057863.40",
"volume": "3",
"year": "2021"
},
{
"DOI": "10.1016/j.cell.2020.04.042",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.41"
},
{
"DOI": "10.1136/bjsports-2016-096572",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.42"
},
{
"DOI": "10.1158/1055-9965.EPI-14-0150",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.43"
},
{
"DOI": "10.1093/aje/kwx345",
"doi-asserted-by": "publisher",
"key": "2022063010225462000_12.4.e057863.44"
}
],
"reference-count": 44,
"references-count": 44,
"relation": {},
"resource": {
"primary": {
"URL": "https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2021-057863"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Associations between physical activity prior to infection and COVID-19 disease severity and symptoms: results from the prospective Predi-COVID cohort study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy",
"volume": "12"
}
