Association of physical activity levels and the prevalence of COVID-19-associated hospitalization
et al., Journal of Science and Medicine in Sport, doi:10.1016/j.jsams.2021.05.011, NCT04396353, Sep 2021
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective survey of 938 COVID-19 recovered patients in Brazil, showing lower hospitalization with physical activity. NCT04396353 (history).
|
risk of mechanical ventilation, 73.2% lower, RR 0.27, p = 0.07, high activity levels 3 of 611 (0.5%), low activity levels 6 of 327 (1.8%), NNT 74, unadjusted, excluded in exclusion analyses:
unadjusted results with no group details.
|
|
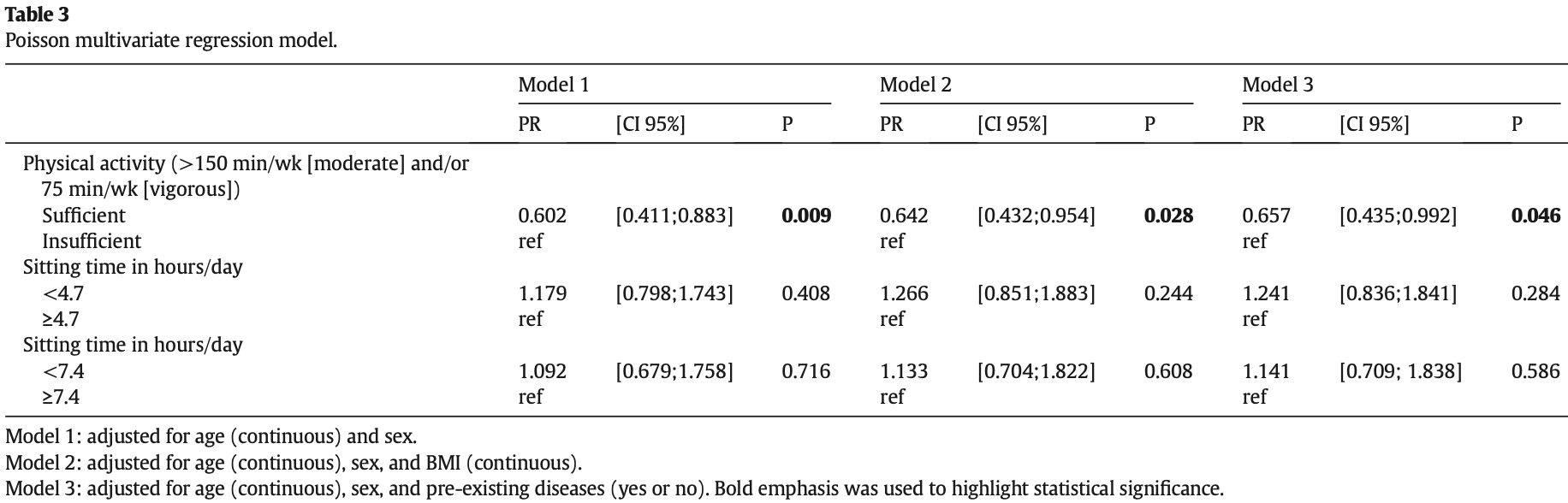
risk of hospitalization, 34.3% lower, RR 0.66, p = 0.046, high activity levels 49 of 611 (8.0%), low activity levels 42 of 327 (12.8%), NNT 21, adjusted per study, sufficient vs. insufficient, model 3, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
de Souza et al., 30 Sep 2021, retrospective, Brazil, peer-reviewed, 8 authors, study period June 2020 - August 2020, trial NCT04396353 (history).
Association of physical activity levels and the prevalence of COVID-19-associated hospitalization
Journal of Science and Medicine in Sport, doi:10.1016/j.jsams.2021.05.011
Objectives: We compared physical activity levels before the outbreak and quarantine measures with COVID-19associated hospitalization prevalence in surviving patients infected with SARS-CoV-2. Additionally, we investigated the association of physical activity levels with symptoms of the disease, length of hospital stay, and mechanical ventilation. Design: Observational, cross-sectional. Methods: Between June 2020 and August 2020, we invited Brazilian survivors and fully recovered patients infected with SARS-CoV-2 to respond to an online questionnaire. We shared the electronic link to the questionnaire on the internet. We collected data about clinical outcomes (symptoms, medications, hospitalization, and length of hospital stay) and cofactors, such as age, sex, ethnicity, preexisting diseases, socioeconomic and educational, and physical activity levels using the International Physical Activity Questionnaire (IPAQ short version). Results: Out of 938 patients, 91 (9.7%) were hospitalized due to COVID-19. In a univariate analysis, sex, age, and BMI were all associated with hospitalizations due to COVID-19. Men had a higher prevalence of hospitalization (66.6%, p = 0.013). Patients older than 65 years, obese, and with preexisting disease had a higher prevalence of COVID-19-related hospitalizations. In a multivariate regression model, performance of at least 150 min/wk (moderate) and/or 75 min/wk (vigorous) physical activity was associated with a lower prevalence of hospitalizations after adjustment for age, sex, BMI, and preexisting diseases (PR = 0.657; p = 0.046). Conclusions: Sufficient physical activity levels were associated with a lower prevalence of COVID-19-related hospitalizations. Performing at least 150 min a week of moderate-intensity, or 75 min a week of vigorous-intensity physical activity was associated with 34.3% reduction in prevalence.
Declaration of interest statement The authors declare that there is no conflict of interest.
Confirmation of ethical compliance This study was approved by the local Human Subject Protection Committee at the Hospital das Clinicas da Faculdade de Medicina da Universidade de São Paulo (CAPPesq 5044-20-073), and all participants provided an online written informed consent. This study is registered on ClinicalTrials.gov (NCT04396353), and its protocol has been published previously (https://osf.io/crv6t).
Data sharing All data are shared publicly through the tool Open Science Framework (https://osf.io/crv6t).
References
Biddle, Bengoechea, Pedisic, Screen time, other sedentary behaviours, and obesity risk in adults: a review of reviews, Curr Obes Rep
Booth, Roberts, Thyfault, Role of inactivity in chronic diseases: evolutionary insight and pathophysiological mechanisms, Physiol Rev
Brawner, Ehrman, Bole, Inverse relationship of maximal exercise capacity to hospitalization secondary to coronavirus disease 2019, Mayo Clin Proc
Burton, Fort, Hospitalization and mortality among black patients and white patients with Covid-19, N Engl J Med
Craig, Marshall, Sjöström, International physical activity questionnaire: 12-country reliability and validity, Med Sci Sports Exerc
De Souza, Motta-Santos, Dos, Soares, None, Journal of Science and Medicine in Sport
Donnelly, Blair, Jakicic, American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults, Med Sci Sports Exerc
Du, Liang, Yang, Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study, Eur Respir J
Franceschi, Campisi, Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases, J Gerontol A Biol Sci Med Sci
Franssen, Donnell, Goossens, Obesity and the lung: 5. Obesity and COPD, Thorax
Frantz, Prodel, Braz, Modulation of the renin-angiotensin system in white adipose tissue and skeletal muscle: focus on exercise training, Clin Sci (Lond)
Gleeson, Bishop, Stensel, The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease, Nat Rev Immunol
Goncalves, Dantas, Santos, Effect of acute and chronic aerobic exercise on immunological markers: a systematic review, Front Physiol
Guthold, Stevens, Riley, Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1.9 million participants, Lancet Glob Health
Health, Advice on the Use of Masks in the Context of COVID-19: Interim Guidance
Heymsfield, Wadden, Mechanisms, pathophysiology, and management of obesity, N Engl J Med
Kassir, Risk of COVID-19 for patients with obesity, Obes Rev
Kujala, Evidence on the effects of exercise therapy in the treatment of chronic disease, Br J Sports Med
Levitt, Schwartz, Lopez, Estimated cost of treating the uninsured hospitalized with COVID-19
Maki-Nunes, Toschi-Dias, Cepeda, Diet and exercise improve chemoreflex sensitivity in patients with metabolic syndrome and obstructive sleep apnea, Silver Spring)
Mauvais-Jarvis, Aging, male sex, obesity, and metabolic inflammation create the perfect storm for COVID-19, Diabetes
Negrão, Middlekauff, Exercise training in heart failure: reduction in angiotensin II, sympathetic nerve activity, and baroreflex control, J Appl Physiol
Nieman, Wentz, The compelling link between physical activity and the body's defense system, J Sport Health Sci
Piercy, Troiano, Ballard, The physical activity guidelines for Americans, JAMA
Ranzani, Bastos, Gelli, Characterisation of the first 250,000 hospital admissions for COVID-19 in Brazil: a retrospective analysis of nationwide data, Lancet Respir Med
Richardson, Hirsch, Narasimhan, Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area, JAMA
Rosa, Neves, Deus, Sprint and endurance training in relation to redox balance, inflammatory status and biomarkers of aging in master athletes, Nitric Oxide
Rush, Aultman, Vascular biology of angiotensin and the impact of physical activity, Appl Physiol Nutr Metab
Sanchis-Gomar, Lavie, Mehra, Obesity and outcomes in COVID-19: when an epidemic and pandemic collide, Mayo Clin Proc
Silsbury, Goldsmith, Rushton, Systematic review of the measurement properties of self-report physical activity questionnaires in healthy adult populations, BMJ Open
Souza, Motta-Santos, Soares, The Impact of EXercise TRAining, Physical Activity and Sedentary Lifestyle on Clinical Outcomes in Surviving Patients Infected With the SARS-CoV-2 Virus (EXTRA SARS-CoV-2 Study): A Protocol
Vandenbroucke, Elm, Altman, Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration, Int J Surg
Villareal, Aguirre, Gurney, Aerobic or resistance exercise, or both, in dieting obese older adults, N Engl J Med
Villareal, Chode, Parimi, Weight loss, exercise, or both and physical function in obese older adults, N Engl J Med
Yates, Razieh, Zaccardi, Obesity, walking pace and risk of severe COVID-19 and mortality: analysis of UK Biobank, Int J Obes
Zbinden-Foncea, Francaux, Deldicque, Does high cardiorespiratory fitness confer some protection against proinflammatory responses after infection by SARS-CoV-2? Obesity, Silver Spring
Zhu, Zhang, A novel coronavirus from patients with pneumonia in China, 2019, N Engl J Med
DOI record:
{
"DOI": "10.1016/j.jsams.2021.05.011",
"ISSN": [
"1440-2440"
],
"URL": "http://dx.doi.org/10.1016/j.jsams.2021.05.011",
"alternative-id": [
"S1440244021001365"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Association of physical activity levels and the prevalence of COVID-19-associated hospitalization"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Journal of Science and Medicine in Sport"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.jsams.2021.05.011"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2021 Sports Medicine Australia. Published by Elsevier Ltd. All rights reserved."
}
],
"author": [
{
"affiliation": [],
"family": "de Souza",
"given": "Francis Ribeiro",
"sequence": "first"
},
{
"affiliation": [],
"family": "Motta-Santos",
"given": "Daisy",
"sequence": "additional"
},
{
"affiliation": [],
"family": "dos Santos Soares",
"given": "Douglas",
"sequence": "additional"
},
{
"affiliation": [],
"family": "de Lima",
"given": "Juliana Beust",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cardozo",
"given": "Gustavo Gonçalves",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Guimarães",
"given": "Luciano Santos Pinto",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Negrão",
"given": "Carlos Eduardo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "dos Santos",
"given": "Marcelo Rodrigues",
"sequence": "additional"
}
],
"container-title": [
"Journal of Science and Medicine in Sport"
],
"content-domain": {
"crossmark-restriction": true,
"domain": [
"jsams.org",
"clinicalkey.jp",
"clinicalkey.com",
"clinicalkey.es",
"clinicalkey.fr",
"clinicalkey.com.au",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2021,
5,
23
]
],
"date-time": "2021-05-23T15:59:49Z",
"timestamp": 1621785589000
},
"deposited": {
"date-parts": [
[
2022,
2,
28
]
],
"date-time": "2022-02-28T20:39:40Z",
"timestamp": 1646080780000
},
"funder": [
{
"DOI": "10.13039/501100002322",
"doi-asserted-by": "publisher",
"name": "Coordenação de Aperfeiçoamento de Pessoal de Nível Superior"
},
{
"DOI": "10.13039/501100001807",
"doi-asserted-by": "publisher",
"name": "Fundacao de Amparo a Pesquisa do Estado de Sao Paulo"
},
{
"DOI": "10.13039/501100003593",
"doi-asserted-by": "publisher",
"name": "Conselho Nacional de Desenvolvimento Científico e Tecnológico"
}
],
"indexed": {
"date-parts": [
[
2022,
3,
29
]
],
"date-time": "2022-03-29T19:39:59Z",
"timestamp": 1648582799256
},
"is-referenced-by-count": 5,
"issn-type": [
{
"type": "print",
"value": "1440-2440"
}
],
"issue": "9",
"issued": {
"date-parts": [
[
2021,
9
]
]
},
"journal-issue": {
"issue": "9",
"published-print": {
"date-parts": [
[
2021,
9
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
9,
1
]
],
"date-time": "2021-09-01T00:00:00Z",
"timestamp": 1630454400000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S1440244021001365?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S1440244021001365?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "913-918",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2021,
9
]
]
},
"published-print": {
"date-parts": [
[
2021,
9
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1056/NEJMoa2001017",
"article-title": "A novel coronavirus from patients with pneumonia in China, 2019",
"author": "Zhu",
"doi-asserted-by": "crossref",
"first-page": "727",
"issue": "8",
"journal-title": "N Engl J Med",
"key": "10.1016/j.jsams.2021.05.011_bb0005",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1183/13993003.00524-2020",
"article-title": "Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study",
"author": "Du",
"doi-asserted-by": "crossref",
"issue": "5",
"journal-title": "Eur Respir J",
"key": "10.1016/j.jsams.2021.05.011_bb0010",
"volume": "55",
"year": "2020"
},
{
"author": "World Health O",
"key": "10.1016/j.jsams.2021.05.011_bb0015",
"series-title": "Advice on the Use of Masks in the Context of COVID-19: Interim Guidance, 5 June 2020",
"year": "2020"
},
{
"DOI": "10.1016/j.jshs.2018.09.009",
"article-title": "The compelling link between physical activity and the body’s defense system",
"author": "Nieman",
"doi-asserted-by": "crossref",
"first-page": "201",
"issue": "3",
"journal-title": "J Sport Health Sci",
"key": "10.1016/j.jsams.2021.05.011_bb0020",
"volume": "8",
"year": "2019"
},
{
"DOI": "10.1002/oby.22849",
"article-title": "Does high cardiorespiratory fitness confer some protection against proinflammatory responses after infection by SARS-CoV-2?",
"author": "Zbinden-Foncea",
"doi-asserted-by": "crossref",
"first-page": "1378",
"journal-title": "Obesity (Silver Spring)",
"key": "10.1016/j.jsams.2021.05.011_bb0025",
"volume": "28",
"year": "2020"
},
{
"author": "Souza",
"key": "10.1016/j.jsams.2021.05.011_bb0030",
"series-title": "The Impact of EXercise TRAining, Physical Activity and Sedentary Lifestyle on Clinical Outcomes in Surviving Patients Infected With the SARS-CoV-2 Virus (EXTRA SARS-CoV-2 Study): A Protocol. Web: OSF",
"year": "2020"
},
{
"DOI": "10.1016/j.ijsu.2014.07.014",
"article-title": "Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration",
"author": "Vandenbroucke",
"doi-asserted-by": "crossref",
"first-page": "1500",
"issue": "12",
"journal-title": "Int J Surg",
"key": "10.1016/j.jsams.2021.05.011_bb0035",
"volume": "12",
"year": "2014"
},
{
"DOI": "10.1249/01.MSS.0000078924.61453.FB",
"article-title": "International physical activity questionnaire: 12-country reliability and validity",
"author": "Craig",
"doi-asserted-by": "crossref",
"first-page": "1381",
"issue": "8",
"journal-title": "Med Sci Sports Exerc",
"key": "10.1016/j.jsams.2021.05.011_bb0040",
"volume": "35",
"year": "2003"
},
{
"DOI": "10.1001/jama.2018.14854",
"article-title": "The physical activity guidelines for Americans",
"author": "Piercy",
"doi-asserted-by": "crossref",
"first-page": "2020",
"issue": "19",
"journal-title": "JAMA",
"key": "10.1016/j.jsams.2021.05.011_bb0045",
"volume": "320",
"year": "2018"
},
{
"DOI": "10.1016/j.mayocp.2020.10.003",
"article-title": "Inverse relationship of maximal exercise capacity to hospitalization secondary to coronavirus disease 2019",
"author": "Brawner",
"doi-asserted-by": "crossref",
"first-page": "32",
"issue": "1",
"journal-title": "Mayo Clin Proc",
"key": "10.1016/j.jsams.2021.05.011_bb0050",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1038/s41366-021-00771-z",
"article-title": "Obesity, walking pace and risk of severe COVID-19 and mortality: analysis of UK Biobank",
"author": "Yates",
"doi-asserted-by": "crossref",
"first-page": "1155",
"journal-title": "Int J Obes",
"key": "10.1016/j.jsams.2021.05.011_bb0055",
"volume": "45",
"year": "2021"
},
{
"author": "Levitt",
"key": "10.1016/j.jsams.2021.05.011_bb0060"
},
{
"DOI": "10.1001/jama.2020.6775",
"article-title": "Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area",
"author": "Richardson",
"doi-asserted-by": "crossref",
"first-page": "2052",
"issue": "20",
"journal-title": "JAMA",
"key": "10.1016/j.jsams.2021.05.011_bb0065",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1016/S2214-109X(18)30357-7",
"article-title": "Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1.9 million participants",
"author": "Guthold",
"doi-asserted-by": "crossref",
"first-page": "e1077",
"issue": "10",
"journal-title": "Lancet Glob Health",
"key": "10.1016/j.jsams.2021.05.011_bb0070",
"volume": "6",
"year": "2018"
},
{
"DOI": "10.1016/S2213-2600(20)30560-9",
"article-title": "Characterisation of the first 250,000 hospital admissions for COVID-19 in Brazil: a retrospective analysis of nationwide data",
"author": "Ranzani",
"doi-asserted-by": "crossref",
"first-page": "407",
"issue": "4",
"journal-title": "Lancet Respir Med",
"key": "10.1016/j.jsams.2021.05.011_bb0075",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1056/NEJMsa2011686",
"article-title": "Hospitalization and mortality among black patients and white patients with Covid-19",
"author": "Price-Haywood",
"doi-asserted-by": "crossref",
"first-page": "2534",
"issue": "26",
"journal-title": "N Engl J Med",
"key": "10.1016/j.jsams.2021.05.011_bb0080",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1093/gerona/glu057",
"article-title": "Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases",
"author": "Franceschi",
"doi-asserted-by": "crossref",
"first-page": "S4",
"issue": "Suppl 1",
"journal-title": "J Gerontol A Biol Sci Med Sci",
"key": "10.1016/j.jsams.2021.05.011_bb0085",
"volume": "69",
"year": "2014"
},
{
"DOI": "10.1016/j.niox.2020.05.004",
"article-title": "Sprint and endurance training in relation to redox balance, inflammatory status and biomarkers of aging in master athletes",
"author": "Rosa",
"doi-asserted-by": "crossref",
"first-page": "42",
"journal-title": "Nitric Oxide",
"key": "10.1016/j.jsams.2021.05.011_bb0090",
"volume": "102",
"year": "2020"
},
{
"article-title": "Mechanisms, pathophysiology, and management of obesity",
"author": "Heymsfield",
"first-page": "1492",
"issue": "15",
"journal-title": "N Engl J Med",
"key": "10.1016/j.jsams.2021.05.011_bb0095",
"volume": "376",
"year": "2017"
},
{
"DOI": "10.1056/NEJMoa1616338",
"article-title": "Aerobic or resistance exercise, or both, in dieting obese older adults",
"author": "Villareal",
"doi-asserted-by": "crossref",
"first-page": "1943",
"issue": "20",
"journal-title": "N Engl J Med",
"key": "10.1016/j.jsams.2021.05.011_bb0100",
"volume": "376",
"year": "2017"
},
{
"DOI": "10.1007/s13679-017-0256-9",
"article-title": "Screen time, other sedentary behaviours, and obesity risk in adults: a review of reviews",
"author": "Biddle",
"doi-asserted-by": "crossref",
"first-page": "134",
"issue": "2",
"journal-title": "Curr Obes Rep",
"key": "10.1016/j.jsams.2021.05.011_bb0105",
"volume": "6",
"year": "2017"
},
{
"DOI": "10.1152/physrev.00019.2016",
"article-title": "Role of inactivity in chronic diseases: evolutionary insight and pathophysiological mechanisms",
"author": "Booth",
"doi-asserted-by": "crossref",
"first-page": "1351",
"issue": "4",
"journal-title": "Physiol Rev",
"key": "10.1016/j.jsams.2021.05.011_bb0110",
"volume": "97",
"year": "2017"
},
{
"DOI": "10.1111/obr.13034",
"article-title": "Risk of COVID-19 for patients with obesity",
"author": "Kassir",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Obes Rev",
"key": "10.1016/j.jsams.2021.05.011_bb0115",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.2337/dbi19-0023",
"article-title": "Aging, male sex, obesity, and metabolic inflammation create the perfect storm for COVID-19",
"author": "Mauvais-Jarvis",
"doi-asserted-by": "crossref",
"first-page": "1857",
"issue": "9",
"journal-title": "Diabetes",
"key": "10.1016/j.jsams.2021.05.011_bb0120",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa1008234",
"article-title": "Weight loss, exercise, or both and physical function in obese older adults",
"author": "Villareal",
"doi-asserted-by": "crossref",
"first-page": "1218",
"issue": "13",
"journal-title": "N Engl J Med",
"key": "10.1016/j.jsams.2021.05.011_bb0125",
"volume": "364",
"year": "2011"
},
{
"DOI": "10.1249/MSS.0b013e3181949333",
"article-title": "American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults",
"author": "Donnelly",
"doi-asserted-by": "crossref",
"first-page": "459",
"issue": "2",
"journal-title": "Med Sci Sports Exerc",
"key": "10.1016/j.jsams.2021.05.011_bb0130",
"volume": "41",
"year": "2009"
},
{
"DOI": "10.1038/nri3041",
"article-title": "The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease",
"author": "Gleeson",
"doi-asserted-by": "crossref",
"first-page": "607",
"issue": "9",
"journal-title": "Nat Rev Immunol",
"key": "10.1016/j.jsams.2021.05.011_bb0135",
"volume": "11",
"year": "2011"
},
{
"DOI": "10.1136/thx.2007.086827",
"article-title": "Obesity and the lung: 5. Obesity and COPD",
"author": "Franssen",
"doi-asserted-by": "crossref",
"first-page": "1110",
"issue": "12",
"journal-title": "Thorax",
"key": "10.1016/j.jsams.2021.05.011_bb0140",
"volume": "63",
"year": "2008"
},
{
"DOI": "10.1016/j.mayocp.2020.05.006",
"article-title": "Obesity and outcomes in COVID-19: when an epidemic and pandemic collide",
"author": "Sanchis-Gomar",
"doi-asserted-by": "crossref",
"first-page": "1445",
"issue": "7",
"journal-title": "Mayo Clin Proc",
"key": "10.1016/j.jsams.2021.05.011_bb0145",
"volume": "95",
"year": "2020"
},
{
"DOI": "10.1002/oby.21126",
"article-title": "Diet and exercise improve chemoreflex sensitivity in patients with metabolic syndrome and obstructive sleep apnea",
"author": "Maki-Nunes",
"doi-asserted-by": "crossref",
"first-page": "1582",
"issue": "8",
"journal-title": "Obesity (Silver Spring)",
"key": "10.1016/j.jsams.2021.05.011_bb0150",
"volume": "23",
"year": "2015"
},
{
"DOI": "10.1136/bjsm.2009.059808",
"article-title": "Evidence on the effects of exercise therapy in the treatment of chronic disease",
"author": "Kujala",
"doi-asserted-by": "crossref",
"first-page": "550",
"issue": "8",
"journal-title": "Br J Sports Med",
"key": "10.1016/j.jsams.2021.05.011_bb0155",
"volume": "43",
"year": "2009"
},
{
"DOI": "10.1152/japplphysiol.01368.2007",
"article-title": "Exercise training in heart failure: reduction in angiotensin II, sympathetic nerve activity, and baroreflex control",
"author": "Negrão",
"doi-asserted-by": "crossref",
"first-page": "577",
"issue": "3",
"journal-title": "J Appl Physiol",
"key": "10.1016/j.jsams.2021.05.011_bb0160",
"volume": "104",
"year": "2008"
},
{
"DOI": "10.1042/CS20180276",
"article-title": "Modulation of the renin-angiotensin system in white adipose tissue and skeletal muscle: focus on exercise training",
"author": "Frantz",
"doi-asserted-by": "crossref",
"first-page": "1487",
"issue": "14",
"journal-title": "Clin Sci (Lond)",
"key": "10.1016/j.jsams.2021.05.011_bb0165",
"volume": "132",
"year": "2018"
},
{
"DOI": "10.1139/H07-147",
"article-title": "Vascular biology of angiotensin and the impact of physical activity",
"author": "Rush",
"doi-asserted-by": "crossref",
"first-page": "162",
"issue": "1",
"journal-title": "Appl Physiol Nutr Metab",
"key": "10.1016/j.jsams.2021.05.011_bb0170",
"volume": "33",
"year": "2008"
},
{
"DOI": "10.3389/fphys.2019.01602",
"article-title": "Effect of acute and chronic aerobic exercise on immunological markers: a systematic review",
"author": "Goncalves",
"doi-asserted-by": "crossref",
"first-page": "1602",
"journal-title": "Front Physiol",
"key": "10.1016/j.jsams.2021.05.011_bb0175",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1136/bmjopen-2015-008430",
"article-title": "Systematic review of the measurement properties of self-report physical activity questionnaires in healthy adult populations",
"author": "Silsbury",
"doi-asserted-by": "crossref",
"issue": "9",
"journal-title": "BMJ Open",
"key": "10.1016/j.jsams.2021.05.011_bb0180",
"volume": "5",
"year": "2015"
}
],
"reference-count": 36,
"references-count": 36,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S1440244021001365"
}
},
"score": 1,
"short-container-title": [
"Journal of Science and Medicine in Sport"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Physical Therapy, Sports Therapy and Rehabilitation",
"Orthopedics and Sports Medicine"
],
"subtitle": [],
"title": [
"Association of physical activity levels and the prevalence of COVID-19-associated hospitalization"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "24"
}
