Small steps, strong shield: directly measured, moderate physical activity in 65 361 adults is associated with significant protective effects from severe COVID-19 outcomes
et al., British Journal of Sports Medicine, doi:10.1136/bjsports-2021-105159, Feb 2022
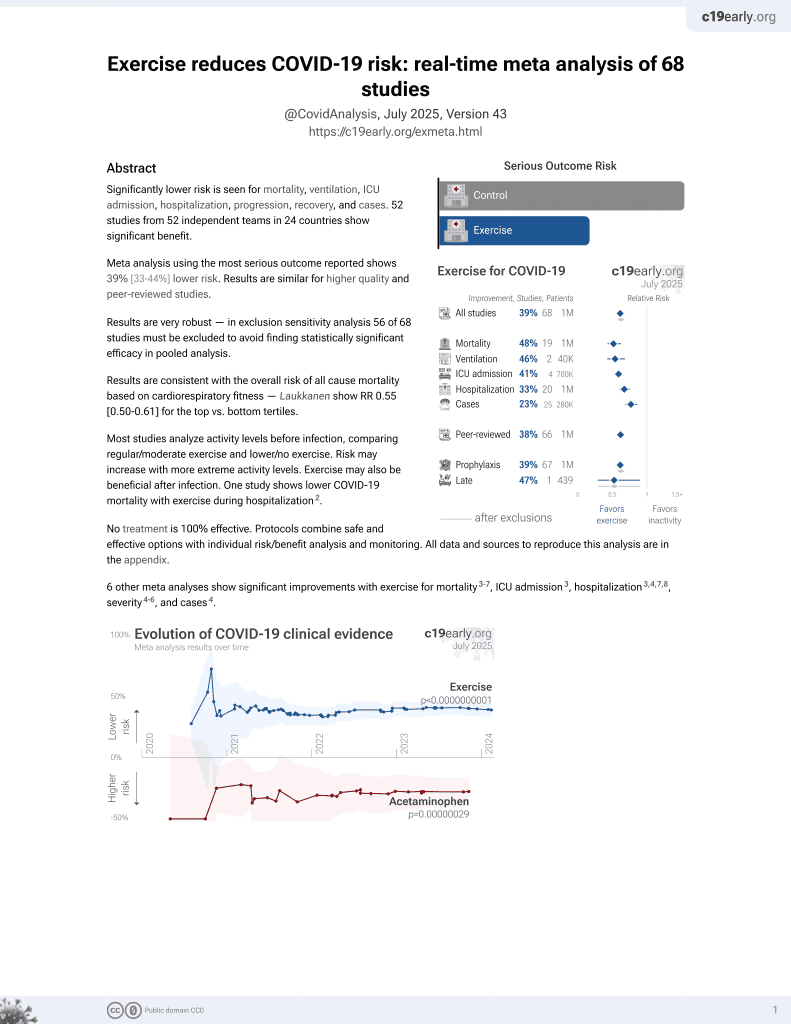
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 65,361 COVID-19 patients in South Africa, showing significantly lower hospitalization, ICU admission, ventilation, and mortality with exercise.
|
risk of death, 42.0% lower, RR 0.58, p < 0.001, high activity levels 29,469, low activity levels 13,366, adjusted per study, high activity vs. low activity, poisson regression, multivariable.
|
|
risk of mechanical ventilation, 45.0% lower, RR 0.55, p < 0.001, high activity levels 29,469, low activity levels 13,366, adjusted per study, high activity vs. low activity, poisson regression, multivariable.
|
|
risk of ICU admission, 41.0% lower, RR 0.59, p < 0.001, high activity levels 29,469, low activity levels 13,366, adjusted per study, high activity vs. low activity, poisson regression, multivariable.
|
|
risk of hospitalization, 34.0% lower, RR 0.66, p < 0.001, high activity levels 29,469, low activity levels 13,366, adjusted per study, high activity vs. low activity, poisson regression, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Steenkamp et al., 9 Feb 2022, retrospective, South Africa, peer-reviewed, 10 authors, study period 19 March, 2020 - 30 June, 2021.
Small steps, strong shield: directly measured, moderate physical activity in 65 361 adults is associated with significant protective effects from severe COVID-19 outcomes
British Journal of Sports Medicine, doi:10.1136/bjsports-2021-105159
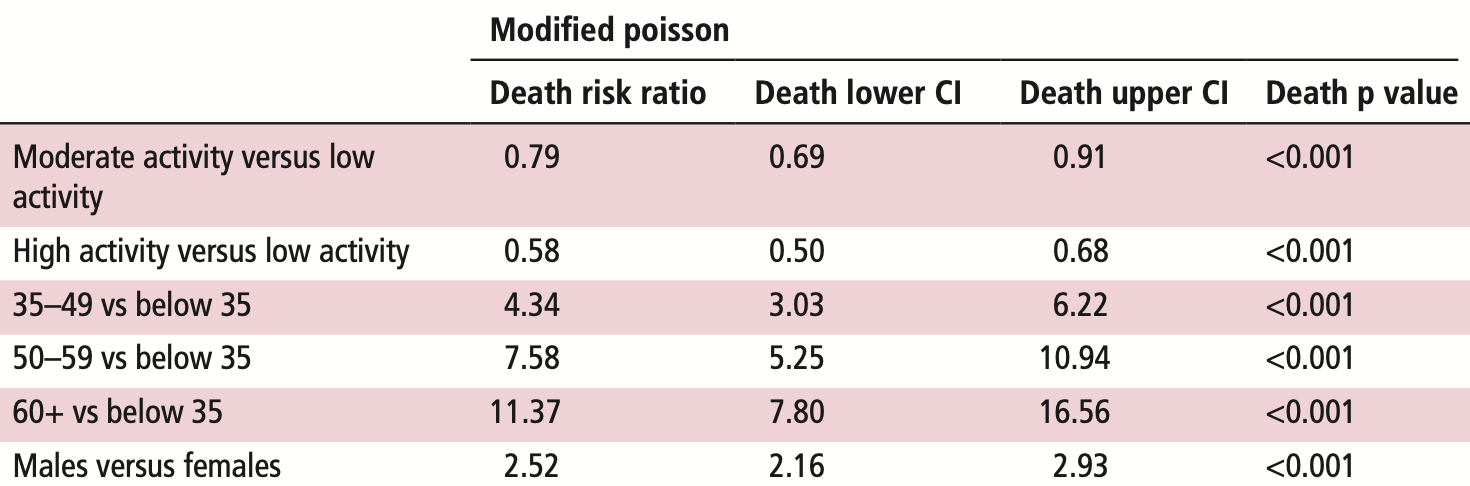
Objective To determine the association between directly measured physical activity and hospitalisation, intensive care unit (ICU) admission, ventilation and mortality rates in patients with a confirmed diagnosis of COVID-19. Methods Directly measured physical activity data from 65 361 adult patients with a COVID-19 diagnosis from 19 March 2020 to 30 June 2021, were grouped by activity level: low (<60 min/week), moderate (60-149 min/week) and high activity (≥150 min/week). The association of physical activity levels and the risk of adverse outcomes was analysed using modified Poisson regression. We accounted for demographics and comorbidities including conditions known to influence COVID-19 outcomes, as well as patient complexity as measured by the Johns Hopkins Adjusted Clinical Group system. The regression approach was further validated with a Bayesian network model built off a directed acyclic graph. Results High physical activity was associated with lower rates of hospitalisation (risk ratio, RR 0.66, 95% CI 0.63 to 0.70), ICU admission (RR 0.59, 95% CI 0.52 to 0.66), ventilation (RR 0.55, 95% CI 0.47 to 0.64) and death (RR 0.58, 95% CI 0.50 to 0.68) due to COVID-19 than those who engaged in low physical activity. Moderate physical activity also was associated with lower rates of hospitalisation (RR 0.87, 95% CI 0.82 to 0.91), admission to ICU (RR 0.80, 95% CI 0.71 to 0.89), ventilation (RR 0.73, 95% CI 0.62 to 0.84) and death (RR 0.79, 95% CI 0.69 to 0.91). Conclusions Adults with high and moderate physical activity levels had significantly better outcomes than those with low activity when contracting COVID-19. The apparent protective effects of regular physical activity extended to those with concomitant chronic medical conditions.
Competing interests LS, DP, SR and SH are employed by Discovery Health; JP and JST are editors of BJSM.
Patient consent for publication Not applicable. Ethics approval Permission for use of DHMS anonymised medical and physical activity data was obtained from the Research Governance Committee of Discovery Health. Ethical approval was obtained from the Human Research Ethics Committee of the University of the Witwatersrand, Johannesburg (clearance certificate number M210725.) Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement No data are available. Not applicable.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Open access This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits..
References
Brandenburg, Lesser, Thomson, Does higher self-reported cardiorespiratory fitness reduce the odds of hospitalization from COVID-19?, J Phys Act Health, doi:10.1123/jpah.2020-0817
Cho, Lee, Physical activity and the risk of COVID-19 infection and mortality: a nationwide population-based case-control study, J Clin Med, doi:10.3390/jcm10071539
Christensen, Arneja, Cyr, The association of estimated cardiorespiratory fitness with COVID-19 incidence and mortality: a cohort study, PLoS One, doi:10.1371/journal.pone.0250508
Cunningham, Physical activity and its relationship with COVID-19 cases and deaths: analysis of U.S. counties, J Sport Health Sci, doi:10.1016/j.jshs.2021.03.008
De Souza, Motta-Santos, Soares, Association of physical activity levels and the prevalence of COVID-19-associated hospitalization, J Sci Med Sport, doi:10.1016/j.jsams.2021.05.011
Dunton, Do, Wang, Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U, S. BMC Public Health, doi:10.1186/s12889-020-09429-3
Gimati, Alrasheed, Bashir, Effect of a COVID-19 on social, psychological, economic and health conditions in Libya, J App Sci Eng Tech Ed
Greenland, Mansournia, Altman, Sparse data bias: a problem hiding in plain sight, BMJ, doi:10.1136/bmj.i1981
Hoeger, Bond, Ransdell, One-mile step count at walking and running speeds, ACSMs Health Fit J, doi:10.1249/01.FIT.0000298459.30006.8d
Joyner, Green, Exercise protects the cardiovascular system: effects beyond traditional risk factors, J Physiol, doi:10.1113/jphysiol.2009.179432
Ledo, Schub, Ziller, Elite athletes on regular training show more pronounced induction of vaccine-specific T-cells and antibodies after tetravalent influenza vaccination than controls, Brain Behav Immun, doi:10.1016/j.bbi.2019.09.024
Lee, Lee, Moon, Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study, Br J Sports Med, doi:10.1136/bjsports-2021-104203
Mansournia, Etminan, Danaei, Handling time varying confounding in observational research, BMJ, doi:10.1136/bmj.j4587
Nextstrain, Genomic epidemiology of novel coronavirus -Global subsampling
Nieman, Wentz, The compelling link between physical activity and the body's defense system, J Sport Health Sci, doi:10.1016/j.jshs.2018.09.009
Patel, Nossel, Patricios, Bright spots, physical activity investments that work: vitality active Rewards-a smartphone APP that incentivises programme members to be physically active, Br J Sports Med, doi:10.1136/bjsports-2018-099271
Pinckard, Baskin, Stanford, Effects of exercise to improve cardiovascular health, Front Cardiovasc Med, doi:10.3389/fcvm.2019.00069
Sallis, Young, Tartof, Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients, Br J Sports Med, doi:10.1136/bjsports-2021-104080
Simpson, Hussain, Baker, Cardiorespiratory fitness is associated with better control of latent herpesvirus infections in a large ethnically diverse community sample: evidence from the Texas City stress and health study, Brain Behav Immun, doi:10.1016/j.bbi.2017.07.128
Simpson, Katsanis, The immunological case for staying active during the COVID-19 pandemic, Brain Behav Immun, doi:10.1016/j.bbi.2020.04.041
Simpson, Kunz, Agha, Exercise and the regulation of immune functions
Stalsberg, Pedersen, Are differences in physical activity across socioeconomic groups associated with choice of physical activity variables to report?, Int J Environ Res Public Health, doi:10.3390/ijerph15050922
Steenkamp, None, Br J Med
Tavakol, Ghannadi, Tabesh, Relationship between physical activity, healthy lifestyle and COVID-19 disease severity; a cross-sectional study, Z Gesundh Wiss, doi:10.1007/s10389-020-01468-9
Tison, Avram, Kuhar, Worldwide effect of COVID-19 on physical activity: a descriptive study, Ann Intern Med, doi:10.7326/M20-2665
Woods, Hutchinson, Powers, The COVID-19 pandemic and physical activity, Sports Med Health Sci, doi:10.1016/j.smhs.2020.05.006
Zbinden-Foncea, Francaux, Deldicque, Does high cardiorespiratory fitness confer some protection against proinflammatory responses after infection by SARS-CoV-2?, Obesity, doi:10.1002/oby.22849
DOI record:
{
"DOI": "10.1136/bjsports-2021-105159",
"ISSN": [
"0306-3674",
"1473-0480"
],
"URL": "http://dx.doi.org/10.1136/bjsports-2021-105159",
"abstract": "<jats:sec><jats:title>Objective</jats:title><jats:p>To determine the association between directly measured physical activity and hospitalisation, intensive care unit (ICU) admission, ventilation and mortality rates in patients with a confirmed diagnosis of COVID-19.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>Directly measured physical activity data from 65 361 adult patients with a COVID-19 diagnosis from 19 March 2020 to 30 June 2021, were grouped by activity level: low (<60 min/week), moderate (60–149 min/week) and high activity (≥150 min/week). The association of physical activity levels and the risk of adverse outcomes was analysed using modified Poisson regression. We accounted for demographics and comorbidities including conditions known to influence COVID-19 outcomes, as well as patient complexity as measured by the Johns Hopkins Adjusted Clinical Group system. The regression approach was further validated with a Bayesian network model built off a directed acyclic graph.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>High physical activity was associated with lower rates of hospitalisation (risk ratio, RR 0.66, 95% CI 0.63 to 0.70), ICU admission (RR 0.59, 95% CI 0.52 to 0.66), ventilation (RR 0.55, 95% CI 0.47 to 0.64) and death (RR 0.58, 95% CI 0.50 to 0.68) due to COVID-19 than those who engaged in low physical activity. Moderate physical activity also was associated with lower rates of hospitalisation (RR 0.87, 95% CI 0.82 to 0.91), admission to ICU (RR 0.80, 95% CI 0.71 to 0.89), ventilation (RR 0.73, 95% CI 0.62 to 0.84) and death (RR 0.79, 95% CI 0.69 to 0.91).</jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p>Adults with high and moderate physical activity levels had significantly better outcomes than those with low activity when contracting COVID-19. The apparent protective effects of regular physical activity extended to those with concomitant chronic medical conditions.</jats:p></jats:sec>",
"alternative-id": [
"10.1136/bjsports-2021-105159"
],
"author": [
{
"affiliation": [],
"family": "Steenkamp",
"given": "Lizelle",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-6593-8049",
"affiliation": [],
"authenticated-orcid": false,
"family": "Saggers",
"given": "Robin Terence",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bandini",
"given": "Rossella",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Stranges",
"given": "Saverio",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Choi",
"given": "Yun-Hee",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3519-7101",
"affiliation": [],
"authenticated-orcid": false,
"family": "Thornton",
"given": "Jane S",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hendrie",
"given": "Simon",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Patel",
"given": "Deepak",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rabinowitz",
"given": "Shannon",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6829-4098",
"affiliation": [],
"authenticated-orcid": false,
"family": "Patricios",
"given": "Jon",
"sequence": "additional"
}
],
"container-title": [
"British Journal of Sports Medicine"
],
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2022,
2,
9
]
],
"date-time": "2022-02-09T18:20:59Z",
"timestamp": 1644430859000
},
"deposited": {
"date-parts": [
[
2022,
2,
9
]
],
"date-time": "2022-02-09T18:21:20Z",
"timestamp": 1644430880000
},
"indexed": {
"date-parts": [
[
2022,
2,
9
]
],
"date-time": "2022-02-09T18:42:47Z",
"timestamp": 1644432167495
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "print",
"value": "0306-3674"
},
{
"type": "electronic",
"value": "1473-0480"
}
],
"issued": {
"date-parts": [
[
2022,
2,
9
]
]
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
2,
8
]
],
"date-time": "2022-02-08T00:00:00Z",
"timestamp": 1644278400000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/bjsports-2021-105159",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "bjsports-2021-105159",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2022,
2,
9
]
]
},
"published-online": {
"date-parts": [
[
2022,
2,
9
]
]
},
"publisher": "BMJ",
"reference": [
{
"DOI": "10.1161/01.CIR.0000048890.59383.8D",
"doi-asserted-by": "publisher",
"key": "2022020910201015000_bjsports-2021-105159v1.1"
},
{
"DOI": "10.1113/jphysiol.2009.179432",
"doi-asserted-by": "publisher",
"key": "2022020910201015000_bjsports-2021-105159v1.2"
},
{
"DOI": "10.3389/fcvm.2019.00069",
"article-title": "Effects of exercise to improve cardiovascular health",
"author": "Pinckard",
"doi-asserted-by": "crossref",
"journal-title": "Front Cardiovasc Med",
"key": "2022020910201015000_bjsports-2021-105159v1.3",
"volume": "6",
"year": "2019"
},
{
"DOI": "10.1016/j.smhs.2020.05.006",
"article-title": "The COVID-19 pandemic and physical activity",
"author": "Woods",
"doi-asserted-by": "crossref",
"first-page": "55",
"journal-title": "Sports Med Health Sci",
"key": "2022020910201015000_bjsports-2021-105159v1.4",
"volume": "2",
"year": "2020"
},
{
"DOI": "10.3390/jcm10071539",
"article-title": "Physical activity and the risk of COVID-19 infection and mortality: a nationwide population-based case-control study",
"author": "Cho",
"doi-asserted-by": "crossref",
"first-page": "1539",
"journal-title": "J Clin Med",
"key": "2022020910201015000_bjsports-2021-105159v1.5",
"volume": "10",
"year": "2021"
},
{
"author": "Simpson",
"first-page": "355",
"key": "2022020910201015000_bjsports-2021-105159v1.6",
"volume": "135",
"volume-title": "Progress in molecular biology and translational science",
"year": "2015"
},
{
"DOI": "10.1016/j.bbi.2020.04.041",
"article-title": "The immunological case for staying active during the COVID-19 pandemic",
"author": "Simpson",
"doi-asserted-by": "crossref",
"first-page": "6",
"journal-title": "Brain Behav Immun",
"key": "2022020910201015000_bjsports-2021-105159v1.7",
"volume": "87",
"year": "2020"
},
{
"DOI": "10.1002/oby.22849",
"article-title": "Does high cardiorespiratory fitness confer some protection against proinflammatory responses after infection by SARS-CoV-2?",
"author": "Zbinden-Foncea",
"doi-asserted-by": "crossref",
"first-page": "1378",
"journal-title": "Obesity",
"key": "2022020910201015000_bjsports-2021-105159v1.8",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1016/j.bbi.2017.07.128",
"doi-asserted-by": "crossref",
"key": "2022020910201015000_bjsports-2021-105159v1.9",
"unstructured": "Simpson RJ , Hussain M , Baker F , et al . Cardiorespiratory fitness is associated with better control of latent herpesvirus infections in a large ethnically diverse community sample: evidence from the Texas City stress and health study. Brain Behav Immun 2017;66:e35. doi:10.1016/j.bbi.2017.07.128"
},
{
"DOI": "10.1016/j.jshs.2018.09.009",
"article-title": "The compelling link between physical activity and the body’s defense system",
"author": "Nieman",
"doi-asserted-by": "crossref",
"first-page": "201",
"journal-title": "J Sport Health Sci",
"key": "2022020910201015000_bjsports-2021-105159v1.10",
"volume": "8",
"year": "2019"
},
{
"DOI": "10.1136/bjsports-2021-104080",
"doi-asserted-by": "publisher",
"key": "2022020910201015000_bjsports-2021-105159v1.11"
},
{
"DOI": "10.1136/bjsports-2021-104203",
"article-title": "Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study",
"author": "Lee",
"doi-asserted-by": "crossref",
"journal-title": "Br J Sports Med",
"key": "2022020910201015000_bjsports-2021-105159v1.12",
"year": "2021"
},
{
"article-title": "Relationship between physical activity, healthy lifestyle and COVID-19 disease severity; a cross-sectional study",
"author": "Tavakol",
"first-page": "1",
"journal-title": "Z Gesundh Wiss",
"key": "2022020910201015000_bjsports-2021-105159v1.13",
"year": "2021"
},
{
"DOI": "10.1123/jpah.2020-0817",
"article-title": "Does higher self-reported cardiorespiratory fitness reduce the odds of hospitalization from COVID-19?",
"author": "Brandenburg",
"doi-asserted-by": "crossref",
"first-page": "782",
"journal-title": "J Phys Act Health",
"key": "2022020910201015000_bjsports-2021-105159v1.14",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1016/j.jshs.2021.03.008",
"article-title": "Physical activity and its relationship with COVID-19 cases and deaths: analysis of U.S. counties",
"author": "Cunningham",
"doi-asserted-by": "crossref",
"first-page": "570",
"journal-title": "J Sport Health Sci",
"key": "2022020910201015000_bjsports-2021-105159v1.15",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0250508",
"article-title": "The association of estimated cardiorespiratory fitness with COVID-19 incidence and mortality: a cohort study",
"author": "Christensen",
"doi-asserted-by": "crossref",
"journal-title": "PLoS One",
"key": "2022020910201015000_bjsports-2021-105159v1.16",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1016/j.jsams.2021.05.011",
"article-title": "Association of physical activity levels and the prevalence of COVID-19-associated hospitalization",
"author": "de Souza",
"doi-asserted-by": "crossref",
"first-page": "913",
"journal-title": "J Sci Med Sport",
"key": "2022020910201015000_bjsports-2021-105159v1.17",
"volume": "24",
"year": "2021"
},
{
"DOI": "10.1136/bjsports-2018-099271",
"doi-asserted-by": "publisher",
"key": "2022020910201015000_bjsports-2021-105159v1.18"
},
{
"key": "2022020910201015000_bjsports-2021-105159v1.19",
"unstructured": "National Institute for Communicable Diseases . Available: https://www.nicd.ac.za/wp-content/uploads/2020/05/COVID_Recovered-Definition.pdf [Accessed 10 Oct 2021]."
},
{
"DOI": "10.1249/01.FIT.0000298459.30006.8d",
"article-title": "One-mile step count at walking and running speeds",
"author": "Hoeger",
"doi-asserted-by": "crossref",
"first-page": "14",
"journal-title": "ACSMs Health Fit J",
"key": "2022020910201015000_bjsports-2021-105159v1.20",
"volume": "12",
"year": "2008"
},
{
"key": "2022020910201015000_bjsports-2021-105159v1.21",
"unstructured": "Pedometer Conversion Chart . Gundersen health system. Available: https://www.gundersenhealth.org/health-wellness/move/physical-activity/minutes-in-motion/pedometer-conversion-chart/ [Accessed 13 Jan 2022]."
},
{
"key": "2022020910201015000_bjsports-2021-105159v1.22",
"unstructured": "Johns Hopkins ACG® system. Available: https://www.hopkinsacg.org [Accessed 10 October 2021]."
},
{
"key": "2022020910201015000_bjsports-2021-105159v1.23",
"unstructured": "Nextstrain . Genomic epidemiology of novel coronavirus - Global subsampling. Available: https://nextstrain.org/ncov/gisaid/global?c=clade_membership&dmax [Accessed 23 October 2021]."
},
{
"key": "2022020910201015000_bjsports-2021-105159v1.24",
"unstructured": "World Health Organization . Currently designated variants of concern. Available: https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/ [Accessed 23 October 2021]."
},
{
"DOI": "10.35877/454RI.asci136",
"article-title": "Effect of a COVID-19 on social, psychological, economic and health conditions in Libya",
"author": "Gimati",
"doi-asserted-by": "crossref",
"first-page": "160",
"journal-title": "J App Sci Eng Tech Ed",
"key": "2022020910201015000_bjsports-2021-105159v1.25",
"volume": "3",
"year": "2021"
},
{
"DOI": "10.1186/s12889-020-09429-3",
"doi-asserted-by": "publisher",
"key": "2022020910201015000_bjsports-2021-105159v1.26"
},
{
"key": "2022020910201015000_bjsports-2021-105159v1.27",
"unstructured": "Johns Hopkins University of Medicine . Coronavirus Resource Center. Available: https://coronavirus.jhu.edu/map.html [Accessed 8 Jan 2022]."
},
{
"key": "2022020910201015000_bjsports-2021-105159v1.28",
"unstructured": "Department of Health and Social Care, Office for National Statistics, Government Actuary’s Department and Home Office . Direct and indirect impacts of COVID-19 on excess deaths and morbidity: Executive summary, 2020. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/918738/S0650_Direct_and_Indirect_Impacts_of_COVID-19_on_Excess_Deaths_and_Morbidity.pdf [Accessed 26 Aug 2021]."
},
{
"DOI": "10.7326/m20-2665",
"doi-asserted-by": "publisher",
"key": "2022020910201015000_bjsports-2021-105159v1.29"
},
{
"key": "2022020910201015000_bjsports-2021-105159v1.30",
"unstructured": "World Health Organization . WHO guidelines on physical activity and sedentary behaviour. Available: https://www.who.int/publications/i/item/9789240015128 [Accessed 10 Oct 2021]."
},
{
"key": "2022020910201015000_bjsports-2021-105159v1.31",
"unstructured": "US Department of Health and Human Services . Physical activity guidelines for Americans. 2nd edn, 2021. https://health.gov/sites/default/files/2019-09/Physical_Activity_Guidelines_2nd_edition.pdf"
},
{
"DOI": "10.1016/j.bbi.2019.09.024",
"article-title": "Elite athletes on regular training show more pronounced induction of vaccine-specific T-cells and antibodies after tetravalent influenza vaccination than controls",
"author": "Ledo",
"doi-asserted-by": "crossref",
"first-page": "135",
"journal-title": "Brain Behav Immun",
"key": "2022020910201015000_bjsports-2021-105159v1.32",
"volume": "83",
"year": "2020"
},
{
"DOI": "10.3390/ijerph15050922",
"article-title": "Are differences in physical activity across socioeconomic groups associated with choice of physical activity variables to report?",
"author": "Stalsberg",
"doi-asserted-by": "crossref",
"journal-title": "Int J Environ Res Public Health",
"key": "2022020910201015000_bjsports-2021-105159v1.33",
"volume": "15",
"year": "2018"
},
{
"DOI": "10.1136/bmj.j4587",
"doi-asserted-by": "publisher",
"key": "2022020910201015000_bjsports-2021-105159v1.34"
},
{
"DOI": "10.1136/bmj.i1981",
"doi-asserted-by": "publisher",
"key": "2022020910201015000_bjsports-2021-105159v1.35"
}
],
"reference-count": 35,
"references-count": 35,
"relation": {},
"score": 1,
"short-container-title": [
"Br J Sports Med"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Physical Therapy, Sports Therapy and Rehabilitation",
"Orthopedics and Sports Medicine",
"General Medicine"
],
"subtitle": [],
"title": [
"Small steps, strong shield: directly measured, moderate physical activity in 65 361 adults is associated with significant protective effects from severe COVID-19 outcomes"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy"
}