The association of estimated cardiorespiratory fitness with COVID-19 incidence and mortality: A cohort study
et al., PLOS ONE, doi:10.1371/journal.pone.0250508, May 2021
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Prospective study of 2,690 adults in the UK Biobank showing lower cardiorespiritory fitness associated with COVID-19 mortality.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
|
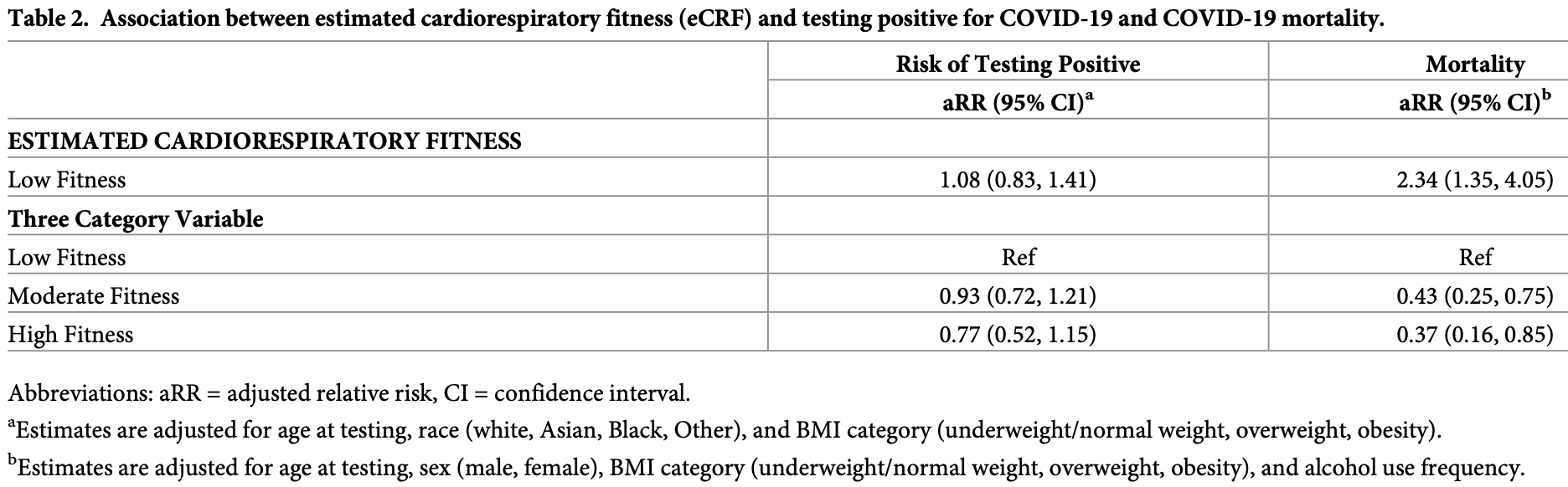
risk of death, 63.0% lower, RR 0.37, p = 0.02, high activity levels 543, low activity levels 529, adjusted per study, high fitness vs. low fitness, multivariable.
|
|
risk of case, 23.0% lower, RR 0.77, p = 0.20, high activity levels 55 of 543 (10.1%), low activity levels 77 of 529 (14.6%), NNT 23, adjusted per study, high fitness vs. low fitness, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Christensen et al., 5 May 2021, prospective, United Kingdom, peer-reviewed, 5 authors, study period 16 March, 2020 - 26 July, 2020.
The association of estimated cardiorespiratory fitness with COVID-19 incidence and mortality: A cohort study
PLOS ONE, doi:10.1371/journal.pone.0250508
Background It has been suggested that cardiorespiratory fitness (CRF) may be used to identify those at greatest risk for severe COVID-19 illness. However, no study to date has examined the association between CRF and COVID-19. The objectives of this study were to determine whether CRF is independently associated with testing positive with or dying from COVID-19.
Methods This is a prospective cohort study of 2,690 adults from the UK Biobank Study that were followed from March 16 th , 2020 to July 26 th , 2020. Participants who were tested for COVID-19 and had undergone CRF assessment were examined. CRF was estimated (eCRF) and categorized as low (<20 th percentile), moderate (20 th to 80 th percentile) and high (�80 th percentile) within sex and ten-year age groups (e.g. 50-60 years). Participants were classified as having COVID-19 if they tested positive (primarily PCR tests) at an in-patient or outpatient setting as of July 26, 2020. Participants were classified as having died from COVID-19 if the primary or underlying cause of death was listed ICD-10 codes U071 or U072 by June 30 th , 2020. Adjusted risk ratios (aRR) and 95% confidence intervals (CI) were estimated and a forward model building approach used to identify covariates.
Findings There was no significant association between eCRF and testing positive for COVID-19. Conversely, individuals with moderate (aRR = 0.43, 95% CI: 0.25, 0.75) and high fitness (aRR = 0.37, 95% CI: 0.16, 0.85) had a significantly lower risk of dying from COVID-19 than those with low fitness.
Conclusions While eCRF was not significantly associated with testing positive for COVID-19, we observed a significant dose-response between having higher eCRF and a decreased risk of
Author Contributions Conceptualization: Rebecca A. G. Christensen.
Formal analysis:
References
Ahmed, COVID-19 -does exercise prescription and maximal oxygen uptake (VO2 max) have a role in risk-stratifying patients?, Clin. Med. J. R. Coll. Physicians, doi:10.7861/clinmed.2020-0111
Blair, Kohl, Paffenbarger, Clark, Cooper et al., Physical Fitness and All-Cause Mortality: A Prospective Study of Healthy Men and Women, JAMA J. Am. Med. Assoc, doi:10.1001/jama.262.17.2395
Bouchard, Familial aggregation of VO2 max response to exercise training: Results from the HERITAGE family study and elite athletic performance, J. Appl. Physiol, doi:10.1152/jappl.1999.87.3.1003
Dipietro, Kohl, Barlow, Improvements in cardiorespiratory fitness attenuate age-related weight gain in healthy men and women: The aerobics center longitudinal study, Int. J. Obes, doi:10.1038/sj.ijo.0800543
Dong, Du, Gardner, An interactive web-based dashboard to track COVID-19 in real time, Lancet Infect. Dis
Duscha, Effects of exercise training amount and intensity on peak oxygen consumption in middle-age men and women at risk for cardiovascular disease, Chest, doi:10.1378/chest.128.4.2788
Edvardsen, Hansen, Holme, Dyrstad, Reference values for cardiorespiratory response and fitness on the treadmill in a 20-to 85-year-old population, Chest, doi:10.1378/chest.12-1458
Florido, Six-year changes in physical activity and the risk of incident heart failure ARIC study, Circulation, doi:10.1161/CIRCULATIONAHA.117.030226
Fondell, Physical activity, stress, and self-reported upper respiratory tract infection, Med. Sci. Sports Exerc, doi:10.1249/MSS.0b013e3181edf108
Fry, Comparison of Sociodemographic and Health-Related Characteristics of UK Biobank Participants with Those of the General Population, Am. J. Epidemiol, doi:10.1093/aje/kwx246
Garg, Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019-COVID-NET, 14 States, MMWR. Morb. Mortal. Wkly. Rep, doi:10.15585/mmwr.mm6915e3
Gortmaker, Hosmer, Applied Logistic Regression, Contemp. Sociol, doi:10.2307/2074954
Hall, Laddu, Phillips, Lavie, Arena, A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another?, Progress in Cardiovascular Diseases, doi:10.1016/j.pcad.2020.04.005
Hamer, Kivima, Gale, Batty, Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK, Brain. Behav. Immun, doi:10.1016/j.bbi.2020.05.059
Harber, Impact of Cardiorespiratory Fitness on All-Cause and Disease-Specific Mortality: Advances Since 2009, Progress in Cardiovascular Diseases, doi:10.1016/j.pcad.2017.03.001
Hung, Liao, Chang, Wang, Wu, Examining the relationship between cardiorespiratory fitness and body weight status: Empirical evidence from a population-based survey of adults in Taiwan, Sci. World J, doi:10.1155/2014/463736
Ingelsson, Heritability, linkage, and genetic associations of exercise treadmill test responses, Circulation, doi:10.1161/CIRCULATIONAHA.106.683821
Jackson, Sui, He, Church, Role of lifestyle and aging on the longitudinal change in cardiorespiratory fitness, Arch. Intern. Med, doi:10.1001/archinternmed.2009.312
Jurak, Physical activity recommendations during the coronavirus disease-2019 virus outbreak, Journal of Sport and Health Science, doi:10.1016/j.jshs.2020.05.003
Kaminsky, Imboden, Arena, Myers, Reference Standards for Cardiorespiratory Fitness Measured With Cardiopulmonary Exercise Testing Using Cycle Ergometry: Data From the Fitness Registry and the Importance of Exercise National Database (FRIEND) Registry, Mayo Clin. Proc, doi:10.1016/j.mayocp.2016.10.003
Kodama, Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis, JAMA-Journal of the American Medical Association, doi:10.1001/jama.2009.681
Laaksonen, Physical activity in the prevention of type 2 diabetes: The finnish diabetes prevention study, Diabetes, doi:10.2337/diabetes.54.1.158
Laddu, Lavie, Phillips, Arena, Physical activity for immunity protection: Inoculating populations with healthy living medicine in preparation for the next pandemic, Progress in Cardiovascular Diseases, doi:10.1016/j.pcad.2020.04.006
Loe, Rognmo, Saltin, Wisløff, Aerobic Capacity Reference Data in 3816 Healthy Men and Women 20-90 Years, PLoS One, doi:10.1371/journal.pone.0064319
Matthews, Ockene, Freedson, Rosal, Merriam et al., Moderate to vigorous physical activity and risk of upper-respiratory tract infection, Med. Sci. Sports Exerc, doi:10.1097/00005768-200208000-00003
Moholdt, Lavie, Sustained Physical Activity, Not Weight Loss, Associated With Improved Survival in Coronary Heart Disease, J. Am. Coll. Cardiol, doi:10.1016/j.jacc.2018.01.011
Nieman, Henson, Austin, Upper respiratory tract infection is reduced in physically fit and active adults, Br. J. Sports Med, doi:10.1136/bjsm.2010.077875
Peel, Sui, Adams, Hibert, Hardin, A prospective study of cardiorespiratory fitness and breast cancer mortality, Med. Sci. Sports Exerc, doi:10.1249/MSS.0b013e31818edac7
Rajagopal, Advanced Pulmonary and Cardiac Support of COVID-19 Patients: Emerging Recommendations from ASAIO-A 'living Working Document, ASAIO J, doi:10.1097/MAT.0000000000001180
Romeo, Wa, Pozo, Physical activity, immunity and infection, doi:10.1017/S0029665110001795
Schwendinger, Pocecco, Counteracting physical inactivity during the COVID-19 pandemic: Evidence-based recommendations for home-based exercise, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph17113909
Sui, Longitudinal analyses of physical activity and cardiorespiratory fitness on adiposity and glucose levels
Swain, Energy cost calculations for exercise prescription: An update, Sports Medicine, doi:10.2165/00007256-200030010-00002
Uk Biobank, Cardio Assessment Version 1.0
Wang, Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China, JAMA-J. Am. Med. Assoc, doi:10.1001/jama.2020.1585
Wei, Relationship between low cardiorespiratory fitness and mortality in normal-weight, overweight, and obese men, J. Am. Med. Assoc, doi:10.1001/jama.282.16.1547
Williams, Physical fitness and activity as separate heart disease risk factors: A meta-analysis, Med. Sci. Sports Exerc, doi:10.1097/00005768-200105000-00012
Williams, Self-selection Accounts for inverse association between weight and cardiorespiratory fitness, Obesity, doi:10.1038/oby.2007.5
Zbinden-Foncea, Francaux, Deldicque, Hawley, Does High Cardiorespiratory Fitness Confer Some Protection Against Proinflammatory Responses After Infection by SARS-CoV-2?, doi:10.1002/oby.22849
DOI record:
{
"DOI": "10.1371/journal.pone.0250508",
"ISSN": [
"1932-6203"
],
"URL": "http://dx.doi.org/10.1371/journal.pone.0250508",
"abstract": "<jats:sec id=\"sec001\">\n<jats:title>Background</jats:title>\n<jats:p>It has been suggested that cardiorespiratory fitness (CRF) may be used to identify those at greatest risk for severe COVID-19 illness. However, no study to date has examined the association between CRF and COVID-19. The objectives of this study were to determine whether CRF is independently associated with testing positive with or dying from COVID-19.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec002\">\n<jats:title>Methods</jats:title>\n<jats:p>This is a prospective cohort study of 2,690 adults from the UK Biobank Study that were followed from March 16<jats:sup>th</jats:sup>, 2020 to July 26<jats:sup>th</jats:sup>, 2020. Participants who were tested for COVID-19 and had undergone CRF assessment were examined. CRF was estimated (eCRF) and categorized as low (<20<jats:sup>th</jats:sup> percentile), moderate (20<jats:sup>th</jats:sup> to 80<jats:sup>th</jats:sup> percentile) and high (≥80<jats:sup>th</jats:sup> percentile) within sex and ten-year age groups (e.g. 50–60 years). Participants were classified as having COVID-19 if they tested positive (primarily PCR tests) at an in-patient or out-patient setting as of July 26, 2020. Participants were classified as having died from COVID-19 if the primary or underlying cause of death was listed ICD-10 codes U071 or U072 by June 30<jats:sup>th</jats:sup>, 2020. Adjusted risk ratios (aRR) and 95% confidence intervals (CI) were estimated and a forward model building approach used to identify covariates.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec003\">\n<jats:title>Findings</jats:title>\n<jats:p>There was no significant association between eCRF and testing positive for COVID-19. Conversely, individuals with moderate (aRR = 0.43, 95% CI: 0.25, 0.75) and high fitness (aRR = 0.37, 95% CI: 0.16, 0.85) had a significantly lower risk of dying from COVID-19 than those with low fitness.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec004\">\n<jats:title>Conclusions</jats:title>\n<jats:p>While eCRF was not significantly associated with testing positive for COVID-19, we observed a significant dose-response between having higher eCRF and a decreased risk of dying from COVID-19. This suggests that prior gains in CRF could be protective against dying from COVID-19 should someone develop the virus.</jats:p>\n</jats:sec>",
"author": [
{
"ORCID": "http://orcid.org/0000-0001-5212-8688",
"affiliation": [],
"authenticated-orcid": true,
"family": "Christensen",
"given": "Rebecca A. G.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Arneja",
"given": "Jasleen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "St. Cyr",
"given": "Kate",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sturrock",
"given": "Shelby L.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Brooks",
"given": "Jennifer D.",
"sequence": "additional"
}
],
"container-title": [
"PLOS ONE"
],
"content-domain": {
"crossmark-restriction": false,
"domain": [
"www.plosone.org"
]
},
"created": {
"date-parts": [
[
2021,
5,
5
]
],
"date-time": "2021-05-05T19:42:53Z",
"timestamp": 1620243773000
},
"deposited": {
"date-parts": [
[
2021,
5,
5
]
],
"date-time": "2021-05-05T19:43:37Z",
"timestamp": 1620243817000
},
"editor": [
{
"affiliation": [],
"family": "Siegel",
"given": "Robert",
"sequence": "first"
}
],
"indexed": {
"date-parts": [
[
2022,
4,
13
]
],
"date-time": "2022-04-13T08:17:08Z",
"timestamp": 1649837828702
},
"is-referenced-by-count": 11,
"issn-type": [
{
"type": "electronic",
"value": "1932-6203"
}
],
"issue": "5",
"issued": {
"date-parts": [
[
2021,
5,
5
]
]
},
"journal-issue": {
"issue": "5",
"published-online": {
"date-parts": [
[
2021,
5,
5
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
5,
5
]
],
"date-time": "2021-05-05T00:00:00Z",
"timestamp": 1620172800000
}
}
],
"link": [
{
"URL": "https://dx.plos.org/10.1371/journal.pone.0250508",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "340",
"original-title": [],
"page": "e0250508",
"prefix": "10.1371",
"published": {
"date-parts": [
[
2021,
5,
5
]
]
},
"published-online": {
"date-parts": [
[
2021,
5,
5
]
]
},
"publisher": "Public Library of Science (PLoS)",
"reference": [
{
"key": "pone.0250508.ref001",
"unstructured": "The World Health Organization, “Coronavirus disease 2019 (COVID-19) Situation Report-94 HIGHLIGHTS,” Geneva, 2020. Accessed: Nov. 16, 2020. [Online]. Available: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200423-sitrep-94-covid-19.pdf#:~:text=The first human cases of,%2C in December 2019."
},
{
"article-title": "An interactive web-based dashboard to track COVID-19 in real time",
"author": "E. Dong",
"journal-title": "Lancet Infect. Dis.",
"key": "pone.0250508.ref002",
"year": "2020"
},
{
"article-title": "Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK",
"author": "M. Hamer",
"journal-title": "Brain. Behav. Immun.",
"key": "pone.0250508.ref003",
"year": "2020"
},
{
"article-title": "Physical activity in the prevention of type 2 diabetes: The finnish diabetes prevention study",
"author": "D. E. Laaksonen",
"journal-title": "Diabetes",
"key": "pone.0250508.ref004",
"year": "2005"
},
{
"article-title": "Physical activity, immunity and infection",
"author": "J. Romeo",
"key": "pone.0250508.ref005",
"year": "2010"
},
{
"article-title": "Six-year changes in physical activity and the risk of incident heart failure ARIC study",
"author": "R. Florido",
"journal-title": "Circulation",
"key": "pone.0250508.ref006",
"year": "2018"
},
{
"article-title": "Upper respiratory tract infection is reduced in physically fit and active adults",
"author": "D. C. Nieman",
"journal-title": "Br. J. Sports Med.",
"key": "pone.0250508.ref007",
"year": "2011"
},
{
"article-title": "Moderate to vigorous physical activity and risk of upper-respiratory tract infection",
"author": "C. E. Matthews",
"journal-title": "Med. Sci. Sports Exerc.",
"key": "pone.0250508.ref008",
"year": "2002"
},
{
"article-title": "Physical activity, stress, and self-reported upper respiratory tract infection",
"author": "E. Fondell",
"journal-title": "Med. Sci. Sports Exerc.",
"key": "pone.0250508.ref009",
"year": "2011"
},
{
"article-title": "Sustained Physical Activity, Not Weight Loss, Associated With Improved Survival in Coronary Heart Disease",
"author": "T. Moholdt",
"journal-title": "J. Am. Coll. Cardiol.",
"key": "pone.0250508.ref010",
"year": "2018"
},
{
"DOI": "10.1378/chest.128.4.2788",
"article-title": "Effects of exercise training amount and intensity on peak oxygen consumption in middle-age men and women at risk for cardiovascular disease",
"author": "B. D. Duscha",
"doi-asserted-by": "crossref",
"first-page": "2788",
"issue": "4",
"journal-title": "Chest",
"key": "pone.0250508.ref011",
"volume": "128",
"year": "2005"
},
{
"article-title": "Heritability, linkage, and genetic associations of exercise treadmill test responses",
"author": "E. Ingelsson",
"journal-title": "Circulation",
"key": "pone.0250508.ref012",
"year": "2007"
},
{
"article-title": "Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis",
"author": "S. Kodama",
"journal-title": "JAMA—Journal of the American Medical Association",
"key": "pone.0250508.ref013",
"year": "2009"
},
{
"article-title": "Relationship between low cardiorespiratory fitness and mortality in normal-weight, overweight, and obese men",
"author": "M. Wei",
"journal-title": "J. Am. Med. Assoc.",
"key": "pone.0250508.ref014",
"year": "1999"
},
{
"article-title": "“Impact of Cardiorespiratory Fitness on All-Cause and Disease-Specific Mortality: Advances Since 2009",
"author": "M. P. Harber",
"journal-title": "Progress in Cardiovascular Diseases",
"key": "pone.0250508.ref015",
"year": "2017"
},
{
"article-title": "Physical fitness and activity as separate heart disease risk factors: A meta-analysis",
"author": "P. T. Williams",
"journal-title": "Med. Sci. Sports Exerc.",
"key": "pone.0250508.ref016",
"year": "2001"
},
{
"article-title": "COVID-19 –does exercise prescription and maximal oxygen uptake (VO2 max) have a role in risk-stratifying patients?",
"author": "I. Ahmed",
"journal-title": "Clin. Med. J. R. Coll. Physicians London",
"key": "pone.0250508.ref017",
"year": "2020"
},
{
"article-title": "Does High Cardiorespiratory Fitness Confer Some Protection Against Proinflammatory Responses After Infection by SARS-CoV-2?",
"author": "H. Zbinden-Foncea",
"journal-title": "Obesity",
"key": "pone.0250508.ref018",
"year": "2020"
},
{
"article-title": "UK Biobank: Protocol for a large-scale prospective epidemiological resource",
"author": "UK Biobank Coordinating Centre",
"key": "pone.0250508.ref019",
"year": "2007"
},
{
"article-title": "Comparison of Sociodemographic and Health-Related Characteristics of UK Biobank Participants with Those of the General Population",
"author": "A. Fry",
"journal-title": "Am. J. Epidemiol.",
"key": "pone.0250508.ref020",
"year": "2017"
},
{
"article-title": "UKB: External Info: COVID19_tests",
"author": "United Kingdom Biobank Study",
"key": "pone.0250508.ref021",
"year": "2020"
},
{
"article-title": "Cardio Assessment Version 1.0",
"author": "UK Biobank",
"key": "pone.0250508.ref022",
"year": "2011"
},
{
"article-title": "Energy cost calculations for exercise prescription: An update",
"author": "D. P. Swain",
"journal-title": "Sports Medicine",
"key": "pone.0250508.ref023",
"year": "2000"
},
{
"article-title": "Physical Fitness and All-Cause Mortality: A Prospective Study of Healthy Men and Women",
"author": "S. N. Blair",
"journal-title": "JAMA J. Am. Med. Assoc.",
"key": "pone.0250508.ref024",
"year": "1989"
},
{
"article-title": "A prospective study of cardiorespiratory fitness and breast cancer mortality",
"author": "J. B. Peel",
"journal-title": "Med. Sci. Sports Exerc.",
"key": "pone.0250508.ref025",
"year": "2009"
},
{
"article-title": "Applied Logistic Regression",
"author": "S. L. Gortmaker",
"journal-title": "Contemp. Sociol.",
"key": "pone.0250508.ref026",
"year": "1994"
},
{
"article-title": "Examining the relationship between cardiorespiratory fitness and body weight status: Empirical evidence from a population-based survey of adults in Taiwan",
"author": "T. H. Hung",
"journal-title": "Sci. World J.",
"key": "pone.0250508.ref027",
"year": "2014"
},
{
"article-title": "Improvements in cardiorespiratory fitness attenuate age-related weight gain in healthy men and women: The aerobics center longitudinal study",
"author": "L. DiPietro",
"journal-title": "Int. J. Obes.",
"key": "pone.0250508.ref028",
"year": "1998"
},
{
"article-title": "Longitudinal analyses of physical activity and cardiorespiratory fitness on adiposity and glucose levels",
"author": "X. Sui",
"key": "pone.0250508.ref029",
"year": "2012"
},
{
"article-title": "Self-selection Accounts for inverse association between weight and cardiorespiratory fitness",
"author": "P. T. Williams",
"journal-title": "Obesity",
"key": "pone.0250508.ref030",
"year": "2008"
},
{
"DOI": "10.1152/jappl.1999.87.3.1003",
"article-title": "Familial aggregation of VO2 max response to exercise training: Results from the HERITAGE family study and elite athletic performance",
"author": "C. Bouchard",
"doi-asserted-by": "crossref",
"first-page": "1003",
"issue": "3",
"journal-title": "J. Appl. Physiol.",
"key": "pone.0250508.ref031",
"volume": "87",
"year": "1999"
},
{
"article-title": "Physical activity for immunity protection: Inoculating populations with healthy living medicine in preparation for the next pandemic",
"author": "D. R. Laddu",
"journal-title": "Progress in Cardiovascular Diseases",
"key": "pone.0250508.ref032",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.1585",
"article-title": "Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China,",
"author": "D. Wang",
"doi-asserted-by": "crossref",
"first-page": "1061",
"issue": "11",
"journal-title": "JAMA—J. Am. Med. Assoc.",
"key": "pone.0250508.ref033",
"volume": "323",
"year": "2020"
},
{
"article-title": "Advanced Pulmonary and Cardiac Support of COVID-19 Patients: Emerging Recommendations from ASAIO—A ‘living Working Document,’",
"author": "K. Rajagopal",
"journal-title": "ASAIO J.",
"key": "pone.0250508.ref034",
"year": "2020"
},
{
"DOI": "10.15585/mmwr.mm6915e3",
"article-title": "Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019—COVID-NET, 14 States, March 1–30, 2020,”",
"author": "S. Garg",
"doi-asserted-by": "crossref",
"first-page": "458",
"issue": "15",
"journal-title": "MMWR. Morb. Mortal. Wkly. Rep.",
"key": "pone.0250508.ref035",
"volume": "69",
"year": "2020"
},
{
"article-title": "“Reference Standards for Cardiorespiratory Fitness Measured With Cardiopulmonary Exercise Testing Using Cycle Ergometry: Data From the Fitness Registry and the Importance of Exercise National Database (FRIEND) Registry",
"author": "L. A. Kaminsky",
"journal-title": "Mayo Clin. Proc.",
"key": "pone.0250508.ref036",
"year": "2017"
},
{
"article-title": "Aerobic Capacity Reference Data in 3816 Healthy Men and Women 20–90 Years",
"author": "H. Loe",
"journal-title": "PLoS One",
"key": "pone.0250508.ref037",
"year": "2013"
},
{
"DOI": "10.1378/chest.12-1458",
"article-title": "Reference values for cardiorespiratory response and fitness on the treadmill in a 20- to 85-year-old population",
"author": "E. Edvardsen",
"doi-asserted-by": "crossref",
"journal-title": "Chest",
"key": "pone.0250508.ref038",
"year": "2013"
},
{
"article-title": "Role of lifestyle and aging on the longitudinal change in cardiorespiratory fitness",
"author": "A. S. Jackson",
"journal-title": "Arch. Intern. Med.",
"key": "pone.0250508.ref039",
"year": "2009"
},
{
"article-title": "“Physical activity recommendations during the coronavirus disease-2019 virus outbreak",
"author": "G. Jurak",
"journal-title": "Journal of Sport and Health Science",
"key": "pone.0250508.ref040",
"year": "2020"
},
{
"article-title": "A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another?",
"author": "G. Hall",
"journal-title": "Progress in Cardiovascular Diseases",
"key": "pone.0250508.ref041",
"year": "2020"
},
{
"article-title": "Counteracting physical inactivity during the COVID-19 pandemic: Evidence-based recommendations for home-based exercise",
"author": "F. Schwendinger",
"journal-title": "Int. J. Environ. Res. Public Health",
"key": "pone.0250508.ref042",
"year": "2020"
}
],
"reference-count": 42,
"references-count": 42,
"relation": {},
"resource": {
"primary": {
"URL": "https://dx.plos.org/10.1371/journal.pone.0250508"
}
},
"score": 1,
"short-container-title": [
"PLoS ONE"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": [
"The association of estimated cardiorespiratory fitness with COVID-19 incidence and mortality: A cohort study"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1371/journal.pone.corrections_policy",
"volume": "16"
}
