Comparative Effectiveness of Combination Therapy with Nirmatrelvir-Ritonavir and Molnupiravir versus Monotherapy with Molnupiravir or Nirmatrelvir-Ritonavir in Hospitalised COVID-19 Patients: A Target Trial Emulation Study
et al., Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1812, Jan 2026
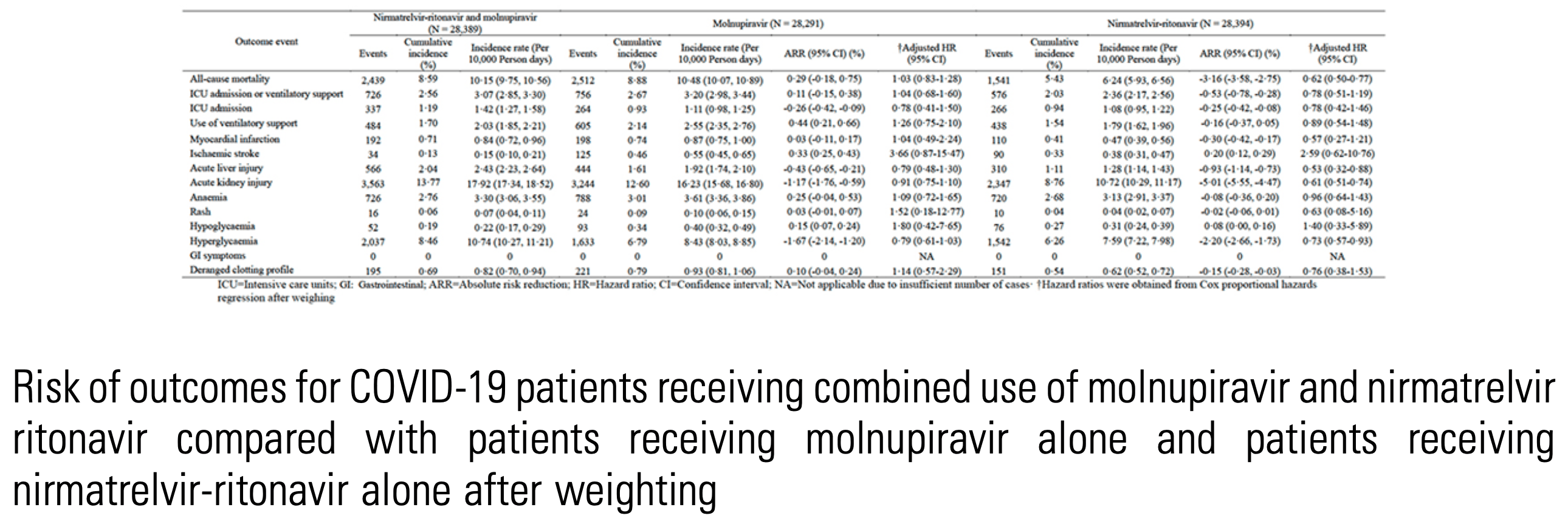
IPTW retrospective target trial emulation of 28,355 hospitalized COVID-19 patients in Hong Kong showing no benefit and potential harm (higher mortality) with combined nirmatrelvir-ritonavir and molnupiravir compared to nirmatrelvir-ritonavir monotherapy. Results are subject to potential unadjusted confounding by indication if combination therapy was preferentially given to patients at higher risk. Additive toxicity from the combined drugs may also be a factor.
Resistance. Variants may be resistant to paxlovid1-8. Use may promote the emergence of variants that weaken host immunity and potentially contribute to long COVID9. Confounding by contraindication. Hoertel et al. find that over 50% of patients that died had a contraindication for the use of Paxlovid10. Retrospective studies that do not exclude contraindicated patients may significantly overestimate efficacy. Black box warning. The FDA notes that severe, life-threatening, and/or fatal adverse reactions due to drug interactions have been reported in patients treated with paxlovid11. Kidney and liver injury. Studies show significantly increased risk of acute kidney injury12 and liver injury13,14. Viral rebound. Studies show significantly increased risk of replication-competent viral rebound15-17.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments18.
This study is excluded in the after exclusion results of meta-analysis:
substantial unadjusted confounding by indication possible.
Study covers molnupiravir and paxlovid.
|
risk of death, 2.9% lower, HR 0.97, p = 0.80, treatment 28,389, control 28,291, inverted to make HR<1 favor treatment, paxlovid+molnupiravir vs. molnupiravir, propensity score weighting.
|
|
risk of mechanical ventilation, 20.6% lower, HR 0.79, p = 0.39, treatment 28,389, control 28,291, inverted to make HR<1 favor treatment, paxlovid+molnupiravir vs. molnupiravir, propensity score weighting.
|
|
risk of ICU admission, 28.2% higher, HR 1.28, p = 0.46, treatment 28,389, control 28,291, inverted to make HR<1 favor treatment, paxlovid+molnupiravir vs. molnupiravir, propensity score weighting.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Zhou et al., Nirmatrelvir-resistant SARS-CoV-2 variants with high fitness in an infectious cell culture system, Science Advances, doi:10.1126/sciadv.add7197.
2.
Moghadasi et al., Rapid resistance profiling of SARS-CoV-2 protease inhibitors, npj Antimicrobials and Resistance, doi:10.1038/s44259-023-00009-0.
3.
Jochmans et al., The Substitutions L50F, E166A, and L167F in SARS-CoV-2 3CLpro Are Selected by a Protease Inhibitor In Vitro and Confer Resistance To Nirmatrelvir, mBio, doi:10.1128/mbio.02815-22.
4.
Lopez et al., SARS-CoV-2 Resistance to Small Molecule Inhibitors, Current Clinical Microbiology Reports, doi:10.1007/s40588-024-00229-6.
5.
Zvornicanin et al., Molecular Mechanisms of Drug Resistance and Compensation in SARS-CoV-2 Main Protease: The Interplay Between E166 and L50, bioRxiv, doi:10.1101/2025.01.24.634813.
6.
Vukovikj et al., Impact of SARS-CoV-2 variant mutations on susceptibility to monoclonal antibodies and antiviral drugs: a non-systematic review, April 2022 to October 2024, Eurosurveillance, doi:10.2807/1560-7917.ES.2025.30.10.2400252.
7.
Deschenes et al., Functional and structural characterization of treatment-emergent nirmatrelvir resistance mutations at low frequencies in the main protease (Mpro) reveals a unique evolutionary route for SARS-CoV-2 to gain resistance, The Journal of Infectious Diseases, doi:10.1093/infdis/jiaf294.
8.
Zhou (B) et al., SARS-CoV-2 Mpro inhibitor ensitrelvir: asymmetrical cross-resistance with nirmatrelvir and emerging resistance hotspots, Emerging Microbes & Infections, doi:10.1080/22221751.2025.2552716.
9.
Thomas et al., Nirmatrelvir-Resistant Mutations in SARS-CoV-2 Mpro Enhance Host Immune Evasion via Cleavage of NF-κB Essential Modulator, bioRxiv, doi:10.1101/2024.10.18.619137.
10.
Hoertel et al., Prevalence of Contraindications to Nirmatrelvir-Ritonavir Among Hospitalized Patients With COVID-19 at Risk for Progression to Severe Disease, JAMA Network Open, doi:10.1001/jamanetworkopen.2022.42140.
11.
FDA, Fact sheet for healthcare providers: emergency use authorization for paxlovid, www.fda.gov/media/155050/download.
12.
Kamo et al., Association of Antiviral Drugs for the Treatment of COVID-19 With Acute Renal Failure, In Vivo, doi:10.21873/invivo.13637.
13.
Wang et al., Development and validation of a nomogram to assess the occurrence of liver dysfunction in patients with COVID-19 pneumonia in the ICU, BMC Infectious Diseases, doi:10.1186/s12879-025-10684-1.
14.
Siby et al., Temporal Trends in Serious Adverse Events Associated with Oral Antivirals During the COVID-19 Pandemic: Insights from the FAERS Database (2020–2023), Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1825.
15.
Edelstein et al., SARS-CoV-2 virologic rebound with nirmatrelvir-ritonavir therapy, medRxiv, doi:10.1101/2023.06.23.23288598.
16.
Shah et al., SARS-CoV-2 infectious shedding and rebound among adults with and without oral antiviral use: two case-ascertained prospective household studies, The Lancet Microbe, doi:10.1016/j.lanmic.2025.101227.
Hong Choi et al., 11 Jan 2026, retrospective, China, peer-reviewed, 3 authors, study period 16 March, 2022 - 31 March, 2024.
Abstract: unclear. Preclinical studies and case reports suggest combining these antivirals may
reduce viral shedding and enhance survival.
1
1 1
Quinnipiac University
Risk of outcomes for COVID-19 patients receiving combined use of molnupiravir and nirmatrelvir
ritonavir compared with patients receiving molnupiravir alone and patients receiving
nirmatrelvir-ritonavir alone after weighting
Methods. This target trial emulation study evaluated the safety and efficacy of
combined molnupiravir and nirmatrelvir-ritonavir versus monotherapy in hospitalised COVID-19 adults in Hong Kong. Data were extracted from electronic health records of patients aged 18 and older treated within five days of hospital admission
between March 16, 2022, and March 31, 2024. Inverse probability of treatment weighting (IPTW) was used to balance baseline characteristics. Outcomes, including allcause mortality, Intensive Care Unit (ICU) admission, and ventilatory support,
were assessed using Cox proportional hazards models.
Abstract citation ID: ofaf695.1812
P-1636. Comparative Effectiveness of Combination Therapy with
Nirmatrelvir-Ritonavir and Molnupiravir versus Monotherapy with Molnupiravir
or Nirmatrelvir-Ritonavir in Hospitalised COVID-19 Patients: A Target Trial
Emulation Study
Ming Hong Choi, MBBS1; Eric Yuk Fai Wan, PhD2; Fan Ngai Ivan Hung, MD2;
1
Queen Mary Hospital, Hong Kong, Hong Kong; 2The University of Hong Kong,
Hong Kong, Not Applicable, Hong Kong
Session: 219. COVID-2019 and Co-Infections
Wednesday, October 22, 2025: 12:15 PM
Background. While molnupiravir and nirmatrelvir-ritonavir have demonstrated
efficacy in reducing hospitalisation and mortality among unvaccinated, high-risk
COVID-19 patients in outpatient settings, their impact on hospitalised adults remains
S1022 • OFID 2026:13 (Suppl 1) • Poster Abstracts
Study flow diagram
1
Frank H. Netter School of Medicine, Hamden, CT
Baseline characteristics of eligible COVID-19 patients after the inverse probability of treatment
weighting (IPTW)
SMD=Standardised mean difference; SD=Standard deviation; IQR = interquartile range;
CCI=Charlson Comorbidity Index; ICU=Intensive
care units;
†SMD<0.1 indicates balance between groups·
†† Level 1: Hospitalised patients with no oxygen therapy; Level 2: Hospitalised patients with
oxygen by mask, nasal prongs, non-invasive
ventilation or high flow; Level 3: Hospitalised patients with intubation and mechanical ventilation, vasopressors, dialysis, or extracorporeal
membrane oxygenation
90-day cumulative incidence of outcomes in recipients of combination treatment with
nirmatrelvir-ritonavir and molnupiravir compared to recipients of molnupiravir monotherapy
and recipients of nirmatrelvir-ritonavir
Shared area refers to the 95% confidence interval for the cumulative incidence. The P
values indicate the overall P values of the Log-rank test comparing the three treatment
groups for each outcome
1
2
1
2
3 1
3
3
Chang Gung University, Taoyuan, Taoyuan, Taiwan
(Republic of China) 2Chang gung university, Taoyuan, Taoyuan, Taiwan 3Chang
Gung Memorial Hospital, Taoyuan, Taoyuan, Taiwan
2
3
2
4 1
Yale School of
Medicine, West Hollywood, California 2Connecticut Department of Correction,
3
Wethersfield, Connecticut Yale School of Public Health/Oswaldo Cruz Foundation/
Brazilian Ministry of Health, New Haven, Connecticut 4Boston University School..
DOI record:
{
"DOI": "10.1093/ofid/ofaf695.1812",
"ISSN": [
"2328-8957"
],
"URL": "http://dx.doi.org/10.1093/ofid/ofaf695.1812",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:sec>\n <jats:title>Background</jats:title>\n <jats:p>While molnupiravir and nirmatrelvir-ritonavir have demonstrated efficacy in reducing hospitalisation and mortality among unvaccinated, high-risk COVID-19 patients in outpatient settings, their impact on hospitalised adults remains unclear. Preclinical studies and case reports suggest combining these antivirals may reduce viral shedding and enhance survival.Baseline characteristics of eligible COVID-19 patients after the inverse probability of treatment weighting (IPTW)SMD=Standardised mean difference; SD=Standard deviation; IQR = interquartile range; CCI=Charlson Comorbidity Index; ICU=Intensivecare units;†SMD&lt;0.1 indicates balance between groups·†† Level 1: Hospitalised patients with no oxygen therapy; Level 2: Hospitalised patients with oxygen by mask, nasal prongs, non-invasiveventilation or high flow; Level 3: Hospitalised patients with intubation and mechanical ventilation, vasopressors, dialysis, or extracorporealmembrane oxygenationRisk of outcomes for COVID-19 patients receiving combined use of molnupiravir and nirmatrelvir ritonavir compared with patients receiving molnupiravir alone and patients receiving nirmatrelvir-ritonavir alone after weighting</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>This target trial emulation study evaluated the safety and efficacy of combined molnupiravir and nirmatrelvir-ritonavir versus monotherapy in hospitalised COVID-19 adults in Hong Kong. Data were extracted from electronic health records of patients aged 18 and older treated within five days of hospital admission between March 16, 2022, and March 31, 2024. Inverse probability of treatment weighting (IPTW) was used to balance baseline characteristics. Outcomes, including all-cause mortality, Intensive Care Unit (ICU) admission, and ventilatory support, were assessed using Cox proportional hazards models.Study flow diagram90-day cumulative incidence of outcomes in recipients of combination treatment with nirmatrelvir-ritonavir and molnupiravir compared to recipients of molnupiravir monotherapy and recipients of nirmatrelvir-ritonavirShared area refers to the 95% confidence interval for the cumulative incidence. The P values indicate the overall P values of the Log-rank test comparing the three treatment groups for each outcome</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>Among 28,355 patients (combination: 1,081; molnupiravir: 8,416; nirmatrelvir-ritonavir: 18,858), IPTW-adjusted analyses showed that nirmatrelvir-ritonavir monotherapy was associated with a significantly lower risk of mortality (HR: 0.62; 95% CI 0.50-0.77; ARR: -3.16%) compared to combination therapy. Risks of ICU admission and ventilatory support were similar across all groups. Patients receiving nirmatrelvir-ritonavir monotherapy also showed lower risks of acute liver injury (HR: 0.53 [95% CI 0.32-0.88]), acute kidney injury (HR: 0.61 [95% CI 0.51-0.74]), and hyperglycaemia (HR 0·73 [95% CI 0.57- 0.93]).</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Conclusion</jats:title>\n <jats:p>Combining nirmatrelvir-ritonavir and molnupiravir does not significantly reduce mortality, ICU admissions, or ventilatory support needs in hospitalised COVID-19 adults. Further randomised controlled trials are needed to confirm these findings.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Disclosures</jats:title>\n <jats:p>All Authors: No reported disclosures</jats:p>\n </jats:sec>",
"article-number": "ofaf695.1812",
"author": [
{
"affiliation": [
{
"name": "Queen Mary Hospital , Hong Kong ,",
"place": [
"Hong Kong"
]
}
],
"family": "Hong Choi",
"given": "Ming",
"sequence": "first"
},
{
"affiliation": [
{
"name": "The University of Hong Kong , Hong Kong, Not Applicable ,",
"place": [
"Hong Kong"
]
}
],
"family": "Fai Wan",
"given": "Eric Yuk",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "The University of Hong Kong , Hong Kong, Not Applicable ,",
"place": [
"Hong Kong"
]
}
],
"family": "Ivan Hung",
"given": "Fan Ngai",
"sequence": "additional"
}
],
"container-title": "Open Forum Infectious Diseases",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2026,
1,
12
]
],
"date-time": "2026-01-12T07:29:12Z",
"timestamp": 1768202952000
},
"deposited": {
"date-parts": [
[
2026,
1,
12
]
],
"date-time": "2026-01-12T07:41:18Z",
"timestamp": 1768203678000
},
"indexed": {
"date-parts": [
[
2026,
1,
13
]
],
"date-time": "2026-01-13T10:46:32Z",
"timestamp": 1768301192693,
"version": "3.49.0"
},
"is-referenced-by-count": 0,
"issue": "Supplement_1",
"issued": {
"date-parts": [
[
2026,
1
]
]
},
"journal-issue": {
"issue": "Supplement_1",
"published-print": {
"date-parts": [
[
2026,
1,
11
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 11,
"start": {
"date-parts": [
[
2026,
1,
12
]
],
"date-time": "2026-01-12T00:00:00Z",
"timestamp": 1768176000000
}
}
],
"link": [
{
"URL": "https://academic.oup.com/ofid/article-pdf/13/Supplement_1/ofaf695.1812/66354845/ofaf695.1812.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "syndication"
},
{
"URL": "https://academic.oup.com/ofid/article-pdf/13/Supplement_1/ofaf695.1812/66354845/ofaf695.1812.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "286",
"original-title": [],
"prefix": "10.1093",
"published": {
"date-parts": [
[
2026,
1
]
]
},
"published-online": {
"date-parts": [
[
2026,
1,
11
]
]
},
"published-other": {
"date-parts": [
[
2026,
1
]
]
},
"published-print": {
"date-parts": [
[
2026,
1,
11
]
]
},
"publisher": "Oxford University Press (OUP)",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://academic.oup.com/ofid/article/doi/10.1093/ofid/ofaf695.1812/8422000"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "P-1636. Comparative Effectiveness of Combination Therapy with Nirmatrelvir-Ritonavir and Molnupiravir versus Monotherapy with Molnupiravir or Nirmatrelvir-Ritonavir in Hospitalised COVID-19 Patients: A Target Trial Emulation Study",
"type": "journal-article",
"volume": "13"
}
hongchoi