Impact of SARS-CoV-2 variant mutations on susceptibility to monoclonal antibodies and antiviral drugs: a non-systematic review, April 2022 to October 2024
et al., Eurosurveillance, doi:10.2807/1560-7917.ES.2025.30.10.2400252, Mar 2025
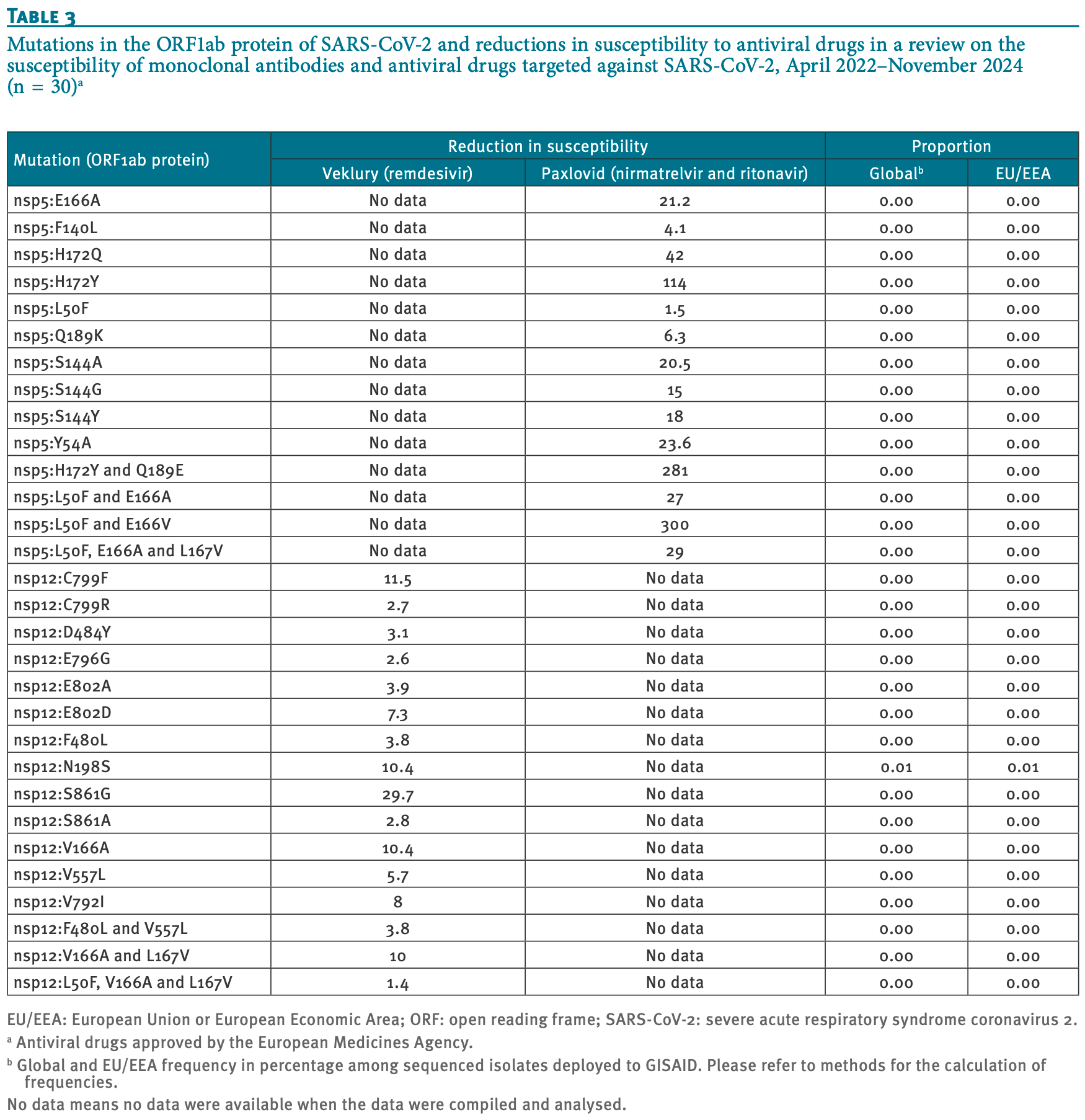
Review of SARS-CoV-2 variant mutations and their impact on susceptibility to monoclonal antibodies and antivirals. Mutations in the ORF1ab region led to decreased susceptibility to paxlovid, while nsp12 mutations reduced efficacy for remdesivir. Casirivimab/imdevimab showed highly reduced neutralization capacity against all Omicron sub-lineages, regdanvimab exhibited decreased effectiveness against BA.1, BA.2, and BA.5 sub-lineages, sotrovimab showed reduced efficacy against BA.2, BA.4, BQ.1.1, and BA.2.86, and tixagevimab/cilgavimab showed highly reduced neutralization activity against BQ.1, BQ.1.1, XBB, XBB.1.5, and BA.2.86 sub-lineages.
Review covers paxlovid, remdesivir, tixagevimab/cilgavimab, sotrovimab, casirivimab/imdevimab, and regdanvimab.
1.
Shen et al., Carboxylesterase Factors Influencing the Therapeutic Activity of Common Antiviral Medications Used for SARS-CoV-2 Infection, Pharmaceutics, doi:10.3390/pharmaceutics17070832.
2.
Vukovikj et al., Impact of SARS-CoV-2 variant mutations on susceptibility to monoclonal antibodies and antiviral drugs: a non-systematic review, April 2022 to October 2024, Eurosurveillance, doi:10.2807/1560-7917.ES.2025.30.10.2400252.
3.
Brewitz et al., Fixing the Achilles Heel of Pfizer’s Paxlovid for COVID-19 Treatment, Journal of Medicinal Chemistry, doi:10.1021/acs.jmedchem.4c01342.
4.
Lopez et al., SARS-CoV-2 Resistance to Small Molecule Inhibitors, Current Clinical Microbiology Reports, doi:10.1007/s40588-024-00229-6.
Vukovikj et al., 13 Mar 2025, peer-reviewed, 6 authors.
Contact: eeva.broberg@ecdc.europa.eu.
Impact of SARS-CoV-2 variant mutations on susceptibility to monoclonal antibodies and antiviral drugs: a non-systematic review, April 2022 to October 2024
Eurosurveillance, doi:10.2807/1560-7917.es.2025.30.10.2400252
Background: Monoclonal antibodies (mAbs) and antiviral drugs have emerged as additional tools for treatment of COVID-19. Aim: We aimed to review data on susceptibility of 14 SARS-CoV-2 variants to mAbs and antiviral drugs authorised in the European Union/European Economic Area (EU/EEA) countries. Methods: We constructed a literature review compiling 298 publications from four databases: PubMed, Science Direct, LitCovid and BioRxiv/MedRxiv preprint servers. We included publications on nirmatrelvir and ritonavir, remdesivir and tixagevimab and cilgavimab, regdanvimab, casirivimab and imdevimab, and sotrovimab approved by the European Medicines Agency (EMA) by 1 October 2024. Results: The mutations identified in the open reading frame (ORF)1ab, specifically nsp5:H172Y, nsp5:H172Y and Q189E, nsp5:L50F and E166V and nsp5:L50F, E166A and L167V, led to a decrease in susceptibility to nirmatrelvir and ritonavir, ranging from moderate (25-99) to high reductions (> 100). Casirivimab and imdevimab exhibited highly reduced neutralisation capacity across all Omicron sub-lineages. Sub-lineages BA.1, BA.2 and BA.5 had decreased susceptibility to regdanvimab, while sotrovimab showed decreased efficacy for BA.2, BA.4, BQ.1.1 and BA.2.86. Tixagevimab and cilgavimab exhibited highly reduced neutralisation activity against BQ.1, BQ.1.1, XBB, XBB.1.5 and BA.2.86 sublineages. Conclusions: The emergence of new variants, some with altered antigenic characteristics, may lead to resistance against mAbs and/or antiviral drugs and evasion of immunity induced naturally or by vaccination. This summary of mutations, combination of mutations and SARS-CoV-2 variants linked to reduced susceptibility to mAbs and antiviral drugs, should aid the selection of appropriate treatment strategies and/or phasing out therapies that have lost their effectiveness. N501Y Alpha Pseudovirus < 2 No data < 5 No data 97.33 98.29 Virus isolate No data No data 1.4 No data N501Y and P681H Alpha Pseudovirus No data < 5 96.58 97.25 Virus isolate No data < 5 K417N, E484K and N501Y Beta Pseudovirus < 2 No data < 5 184 80.4 83.36 Virus isolate No data No data < 5 19.7 P337H Delta Pseudovirus No data 5 No data 0.00 0.00 P337L Delta Pseudovirus No data 192 No data 0.01 0.01 P337R Delta Pseudovirus No data 192 No data 0.00 0.00 P337T Delta Pseudovirus No data 11 No data 0.00 0.00 E340A Delta Pseudovirus No data 100 No data 0.00 0.00 E340G Delta Pseudovirus No data 18 No data 0.00 0.00 E340K Delta Pseudovirus No data 297 No data 0.01 0.01 E340Q Delta Pseudovirus No data 50 No data 0.00 0.00 E340V Delta Pseudovirus No data 200 No data 0.00 0.00 K417N, L452R and T478K Delta Pseudovirus No data 27.7 0.18 0.04 Virus isolate No data 183 L452R and T478K Delta Pseudovirus < 2 No data < 5 No data 95.98 96.85 Virus isolate No data No data < 5 No data K417T, E484K and N501Y Gamma Pseudovirus < 2 < 5 < 5 61.4 90.22 92.09 Virus isolate No data No data < 5 137.9 E484A BA.1..
The combination of mutations in BQ.1 (G339D, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, L452R, S477N, T478K, E484A, F486V, Q498R, N501Y, Y505H, K444T and N460K) and the mutations in the BQ.1.1 sub-lineage (G339D, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, L452R, S477N, T478K, E484A, F486V, Q498R, N501Y, Y505H, R346T, K444T and N460K) resulted in > 2,000-fold decreases in susceptibility to Evusheld [11] . This set of mutations within the respective sub-lineages was present in > 75% of the isolates (Table 2 ). The set of mutations in the XBB and XBB.1.5 sub-lineages (G339H, R346T, L368I, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, V445P, G446S, N460K, S477N, T478K, E484A, F486P, F490S, Q498R, N501Y and Y505H) conferred 1,400 and > 5,000-fold reduction in susceptibility to Evusheld, respectively [24] . Further on, the unique sets of mutations in BA.2.86 and JN.1 shown in Table 2 correlated with high fold reductions (> 5,000) in neutralisation efficacy for Evusheld, however, their proportion was < 0.01%. The mutations identified in ORF1ab, specifically nsp5:H172Y, nsp5:H172Y and Q189E, nsp5:L50F and E166V and nsp5:L50F, E166A and L167V, led to a decrease in susceptibility to Paxlovid (nirmatrelvir and ritonavir), ranging from moderate (25-99) to high (> 100)
Conflict of interest None declared.
Authors' contributions MV, EKB: conceptualisation, methodology; MV: validation, data curation (lead), writing -original..
References
Bewley, Coombes, Gagnon, Mcinroy, Baker et al., Quantification of SARS-CoV-2 neutralizing antibody by wild-type plaque reduction neutralization, microneutralization and pseudotyped virus neutralization assays, Nat Protoc, doi:10.1038/s41596-021-00536-yPMID:33893470
Cao, Yisimayi, Jian, Song, Wang, 2.12.1, BA.4 and BA.5 escape antibodies elicited by Omicron infection, Nature, doi:10.1038/s41586-022-04980-yPMID:35714668
Case, Mackin, Errico, Chong, Madden et al., Resilience of S309 and AZD7442 monoclonal antibody treatments against infection by SARS-CoV-2 Omicron lineage strains, Nat Commun, doi:10.1038/s41467-022-31615-7PMID:35780162
Cathcart, Havenar-Daughton, Lempp, Ma, Schmid et al., The dual function monoclonal antibodies VIR-7831 and VIR-7832 demonstrate potent in vitro and in vivo activity against SARS-CoV-2, bioRxiv
Cheng, Reyes, Satram, Birch, Gibbons et al., Real-world effectiveness of sotrovimab for the early treatment of COVID-19 during SARS-CoV-2 Delta and Omicron waves in the USA, Infect Dis Ther, doi:10.1007/s40121-022-00755-0PMID:36629998
Clayton, De Oliveira, Ibrahim, Sun, Mahinthichaichan et al., Integrative approach to dissect the drug resistance mechanism of the H172Y mutation of SARS-CoV-2 main protease, J Chem Inf Model, doi:10.1021/acs.jcim.3c00344PMID:37199464
Cox, Peacock, Harvey, Hughes, Wright et al., SARS-CoV-2 variant evasion of monoclonal antibodies based on in vitro studies, Nat Rev Microbiol, doi:10.1038/s41579-022-00809-7PMID:36307535
Driouich, Bernadin, Touret, De Lamballerie, Nougairède, Activity of Sotrovimab against BQ.1.1 and XBB.1 Omicron sublineages in a hamster model, Antiviral Res, doi:10.1016/j.antiviral.2023.105638
Drożdżal, Rosik, Lechowicz, Machaj, Szostak et al., An update on drugs with therapeutic potential for SARS-CoV-2 (COVID-19) treatment, Drug Resist Updat, doi:10.1016/j.drup.2021.100794
Fenwick, Turelli, Ni, Perez, Lau, SARS-CoV-2 Omicron potently neutralized by a novel antibody with unique spike binding properties, bioRxiv, doi:10.1101/2022.03.18.484873v1
Hashemian, Sheida, Taghizadieh, Memar, Hamblin et al., Paxlovid (Nirmatrelvir/ Ritonavir): A new approach to Covid-19 therapy?, Biomed Pharmacother, doi:10.1016/j.biopha.2023.114367
Herman, Brien, Forleo-Neto, Sarkar, Isa et al., COVID-19 Phase 3 Prevention Trial Team. Efficacy and safety of a single dose of casirivimab and imdevimab for the prevention of COVID-19 over an 8-month period: a randomised, double-blind, placebo-controlled trial, Lancet Infect Dis, doi:10.1016/S1473-3099(22)00416-9PMID:35803290
Hu, Lewandowski, Tan, Zhang, Morgan et al., Naturally occurring mutations of SARS-CoV-2 main protease confer drug resistance to nirmatrelvir, ACS Cent Sci, doi:10.1021/acscentsci.3c00538PMID:37637734
Huang, Borisov, Kee, Carpp, Wrin et al., Calibration of two validated SARS-CoV-2 pseudovirus neutralization assays for COVID-19 vaccine evaluation, Sci Rep, doi:10.1038/s41598-021-03154-6PMID:34907214
Kristiansen, Page, Bernasconi, Mattiuzzo, Dull et al., WHO International Standard for anti-SARS-CoV-2 immunoglobulin, Lancet, doi:10.1016/S0140-6736(21)00527-4PMID:33770519
Lee, Lee, Lee, Kim, Lee et al., Regdanvimab in patients with mild-to-moderate SARS-CoV-2 infection: A propensity score-matched retrospective cohort study, Int Immunopharmacol, doi:10.1016/j.intimp.2022.108570
Malin, Suárez, Priesner, Fätkenheuer, Rybniker, Remdesivir against COVID-19 and other viral diseases, Clin Microbiol Rev, doi:10.1128/CMR.00162-20PMID:33055231
Martin-Blondel, Marcelin, Soulié, Kaisaridi, Lusivika-Nzinga et al., Sotrovimab to prevent severe COVID-19 in high-risk patients infected with Omicron BA.2, J Infect, doi:10.1016/j.jinf.2022.06.033
Meng, Abdullahi, Ferreira, Goonawardane, Saito et al., Altered TMPRSS2 usage by SARS-CoV-2 Omicron impacts infectivity and fusogenicity, Nature, doi:10.1038/s41586-022-04474-xPMID:35104837
Mlcochova, Kemp, Dhar, Papa, Meng et al., Indian SARS-CoV-2 Genomics Consortium (INSACOG), Genotype to Phenotype Japan (G2P-Japan) Consortium, CITIID-NIHR BioResource COVID-19 Collaboration. SARS-CoV-2 B.1.617.2 Delta variant replication and immune evasion, Nature, doi:10.1038/s41586-021-03944-yPMID:34488225
Moghadasi, Biswas, Harki, Harris, Rapid resistance profiling of SARS-CoV-2 protease inhibitors, NPJ Antimicrob Resist, doi:10.1038/s44259-023-00009-0PMID:39843958
Perera, Ko, Tsang, Hui, Kwan et al., Evaluation of a SARS-CoV-2 surrogate virus neutralization test for detection of antibody in human, canine, cat, and hamster sera, J Clin Microbiol, doi:10.1128/JCM.02504-20PMID:33139421
Perera, Mok, Tsang, Lv, Ko et al., Serological assays for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), March 2020, Euro Surveill, doi:10.2807/1560-7917.ES.2020.25.16.2000421
Sheward, Yang, Westerberg, Öling, Muschiol et al., Sensitivity of the SARS-CoV-2 BA.2.86 variant to prevailing neutralising antibody responses, Lancet Infect Dis, doi:10.1016/S1473-3099(23)00588-1PMID:37776877
Sholukh, Fiore-Gartland, Ford, Miner, Hou et al., Evaluation of cell-based and surrogate SARS-CoV-2 neutralization assays, J Clin Microbiol, doi:10.1128/JCM.00527-21PMID:34288726
Takashita, Kinoshita, Yamayoshi, Sakai-Tagawa, Fujisaki et al., Efficacy of antibodies and antiviral drugs against Covid-19 Omicron variant, N Engl J Med, doi:10.1056/NEJMc2119407PMID:35081300
Takashita, Yamayoshi, Simon, Van Bakel, Sordillo et al., Efficacy of antibodies and antiviral drugs against Omicron BA.2.12.1, BA.4, and BA.5 subvariants, N Engl J Med, doi:10.1056/NEJMc2207519PMID:35857646
Taylor, Adams, Hufford, De La Torre, Winthrop et al., Neutralizing monoclonal antibodies for treatment of COVID-19, Nat Rev Immunol, doi:10.1038/s41577-021-00542-xPMID:33875867
Tchesnokov, Gordon, Woolner, Kocinkova, Perry et al., Template-dependent inhibition of coronavirus RNA-dependent RNA polymerase by remdesivir reveals a second mechanism of action, J Biol Chem, doi:10.1074/jbc.AC120.015720
Tegally, Moir, Everatt, Giovanetti, Scheepers et al., Emergence of SARS-CoV-2 Omicron lineages BA.4 and BA.5 in South Africa, Nat Med, doi:10.1038/s41591-022-01911-2PMID:35760080
Tzou, Tao, Pond, Shafer, Coronavirus Resistance Database (CoV-RDB): SARS-CoV-2 susceptibility to monoclonal antibodies, convalescent plasma, and plasma from vaccinated persons, PLoS One, doi:10.1371/journal.pone.0261045
Uddin, Mustafa, Rizvi, Loney, Suwaidi et al., SARS-CoV-2/COVID-19: viral genomics, epidemiology, vaccines, and therapeutic interventions, Viruses, doi:10.3390/v12050526PMID:32397688
Uriu, Ito, Kosugi, Tanaka, Mugita et al., Transmissibility, infectivity, and immune evasion of the SARS-CoV-2 BA.2.86 variant, Lancet Infect Dis, doi:10.1016/S1473-3099(23)00575-3PMID:37734391
Vanblargan, Errico, Halfmann, Zost, Crowe et al., An infectious SARS-CoV-2 B.1.1.529 Omicron virus escapes neutralization by therapeutic monoclonal antibodies, Nat Med, doi:10.1038/s41591-021-01678-yPMID:35046573
Wright, Harvey, Hughes, Cox, Peacock et al., Tracking SARS-CoV-2 mutations and variants through the COG-UK-Mutation Explorer, Virus Evol, doi:10.1093/ve/veac023PMID:35502202
Yamasoba, Kosugi, Kimura, Fujita, Uriu et al., Neutralisation sensitivity of SARS-CoV-2 omicron subvariants to therapeutic monoclonal antibodies, Lancet Infect Dis, doi:10.1016/S1473-3099(22)00365-6PMID:35690075
Yang, Yu, Jian, Song, Yisimayi et al., Antigenicity and infectivity characterisation of SARS-CoV-2 BA.2.86, Lancet Infect Dis, doi:10.1016/S1473-3099(23)00573-XPMID:37738994
Zhao, Li, Zhong, Mechanism of action of small-molecule agents in ongoing clinical trials for SARS-CoV-2: a review, Front Pharmacol, doi:10.3389/fphar.2022.840639
Zhou, Ayeh, Chidambaram, Karakousis, Modes of transmission of SARS-CoV-2 and evidence for preventive behavioral interventions, BMC Infect Dis, doi:10.1186/s12879-021-06222-4PMID:34049515
DOI record:
{
"DOI": "10.2807/1560-7917.es.2025.30.10.2400252",
"ISSN": [
"1560-7917"
],
"URL": "http://dx.doi.org/10.2807/1560-7917.ES.2025.30.10.2400252",
"abstract": "<jats:sec>\n <jats:title>Background</jats:title>\n <jats:p>Monoclonal antibodies (mAbs) and antiviral drugs have emerged as additional tools for treatment of COVID-19.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Aim</jats:title>\n <jats:p>We aimed to review data on susceptibility of 14 SARS-CoV-2 variants to mAbs and antiviral drugs authorised in the European Union/European Economic Area (EU/EEA) countries.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>We constructed a literature review compiling 298 publications from four databases: PubMed, Science Direct, LitCovid and BioRxiv/MedRxiv preprint servers. We included publications on nirmatrelvir and ritonavir, remdesivir and tixagevimab and cilgavimab, regdanvimab, casirivimab and imdevimab, and sotrovimab approved by the European Medicines Agency (EMA) by 1 October 2024.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>The mutations identified in the open reading frame (ORF)1ab, specifically nsp5:H172Y, nsp5:H172Y and Q189E, nsp5:L50F and E166V and nsp5:L50F, E166A and L167V, led to a decrease in susceptibility to nirmatrelvir and ritonavir, ranging from moderate (25-99) to high reductions (> 100). Casirivimab and imdevimab exhibited highly reduced neutralisation capacity across all Omicron sub-lineages. Sub-lineages BA.1, BA.2 and BA.5 had decreased susceptibility to regdanvimab, while sotrovimab showed decreased efficacy for BA.2, BA.4, BQ.1.1 and BA.2.86. Tixagevimab and cilgavimab exhibited highly reduced neutralisation activity against BQ.1, BQ.1.1, XBB, XBB.1.5 and BA.2.86 sub-lineages.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Conclusions</jats:title>\n <jats:p>The emergence of new variants, some with altered antigenic characteristics, may lead to resistance against mAbs and/or antiviral drugs and evasion of immunity induced naturally or by vaccination. This summary of mutations, combination of mutations and SARS-CoV-2 variants linked to reduced susceptibility to mAbs and antiviral drugs, should aid the selection of appropriate treatment strategies and/or phasing out therapies that have lost their effectiveness.</jats:p>\n </jats:sec>",
"author": [
{
"affiliation": [
{
"name": "European Centre for Disease Prevention and Control (ECDC), Stockholm, Sweden"
}
],
"family": "Vukovikj",
"given": "Maja",
"sequence": "first"
},
{
"affiliation": [
{
"name": "European Centre for Disease Prevention and Control (ECDC), Stockholm, Sweden"
}
],
"family": "Melidou",
"given": "Angeliki",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "European Centre for Disease Prevention and Control (ECDC), Stockholm, Sweden"
}
],
"family": "Nannapaneni",
"given": "Priyanka",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "European Centre for Disease Prevention and Control (ECDC), Stockholm, Sweden"
}
],
"family": "Normark",
"given": "Tanja",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "European Centre for Disease Prevention and Control (ECDC), Stockholm, Sweden"
}
],
"family": "Kraus",
"given": "Annette",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0003-2693-7224",
"affiliation": [
{
"name": "European Centre for Disease Prevention and Control (ECDC), Stockholm, Sweden"
}
],
"authenticated-orcid": false,
"family": "Broberg",
"given": "Eeva K",
"sequence": "additional"
}
],
"container-title": "Eurosurveillance",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2025,
3,
14
]
],
"date-time": "2025-03-14T10:15:41Z",
"timestamp": 1741947341000
},
"deposited": {
"date-parts": [
[
2025,
3,
14
]
],
"date-time": "2025-03-14T10:15:54Z",
"timestamp": 1741947354000
},
"indexed": {
"date-parts": [
[
2025,
3,
15
]
],
"date-time": "2025-03-15T04:17:21Z",
"timestamp": 1742012241318,
"version": "3.38.0"
},
"is-referenced-by-count": 0,
"issue": "10",
"issued": {
"date-parts": [
[
2025,
3,
13
]
]
},
"journal-issue": {
"issue": "10",
"published-print": {
"date-parts": [
[
2025,
3,
13
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
3,
13
]
],
"date-time": "2025-03-13T00:00:00Z",
"timestamp": 1741824000000
}
}
],
"member": "7995",
"original-title": [],
"prefix": "10.2807",
"published": {
"date-parts": [
[
2025,
3,
13
]
]
},
"published-print": {
"date-parts": [
[
2025,
3,
13
]
]
},
"publisher": "European Centre for Disease Control and Prevention (ECDC)",
"reference": [
{
"key": "r1",
"unstructured": "World Health Organization (WHO). WHO COVID-19 dashboard. Geneva: WHO. [Accessed: 10 Mar 2025]. Available from: https://covid19.who.int"
},
{
"DOI": "10.1016/j.drup.2021.100794",
"article-title": "An update on drugs with therapeutic potential for SARS-CoV-2 (COVID-19) treatment.",
"author": "Drożdżal",
"doi-asserted-by": "crossref",
"journal-title": "Drug Resist Updat",
"key": "r2",
"volume": "59",
"year": "2021"
},
{
"DOI": "10.1186/s12879-021-06222-4",
"article-title": "Modes of transmission of SARS-CoV-2 and evidence for preventive behavioral interventions.",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "496",
"issue": "1",
"journal-title": "BMC Infect Dis",
"key": "r3",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.3390/v12050526",
"article-title": "SARS-CoV-2/COVID-19: viral genomics, epidemiology, vaccines, and therapeutic interventions.",
"author": "Uddin",
"doi-asserted-by": "crossref",
"first-page": "526",
"issue": "5",
"journal-title": "Viruses",
"key": "r4",
"volume": "12",
"year": "2020"
},
{
"key": "r5",
"unstructured": "European Centre for Disease Prevention and Control (ECDC). Case management and treatment of COVID-19. Stockholm: ECDC; 2023. Available from: https://www.ecdc.europa.eu/en/infectious-disease-topics/z-disease-list/covid-19/facts/case-management-and-treatment-covid-19"
},
{
"article-title": "Mechanism of action of small-molecule agents in ongoing clinical trials for SARS-CoV-2: a review.",
"author": "Zhao",
"journal-title": "Front Pharmacol",
"key": "r6",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1016/j.biopha.2023.114367",
"article-title": "Paxlovid (Nirmatrelvir/Ritonavir): A new approach to Covid-19 therapy?",
"author": "Hashemian",
"doi-asserted-by": "crossref",
"journal-title": "Biomed Pharmacother",
"key": "r7",
"volume": "162",
"year": "2023"
},
{
"DOI": "10.1128/CMR.00162-20",
"article-title": "Remdesivir against COVID-19 and other viral diseases.",
"author": "Malin",
"doi-asserted-by": "crossref",
"first-page": "e00162",
"issue": "1",
"journal-title": "Clin Microbiol Rev",
"key": "r8",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.1038/s41577-021-00542-x",
"article-title": "Neutralizing monoclonal antibodies for treatment of COVID-19.",
"author": "Taylor",
"doi-asserted-by": "crossref",
"first-page": "382",
"issue": "6",
"journal-title": "Nat Rev Immunol",
"key": "r9",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1038/s41579-022-00809-7",
"article-title": "SARS-CoV-2 variant evasion of monoclonal antibodies based on in vitro studies.",
"author": "Cox",
"doi-asserted-by": "crossref",
"first-page": "112",
"issue": "2",
"journal-title": "Nat Rev Microbiol",
"key": "r10",
"volume": "21",
"year": "2023"
},
{
"key": "r11",
"unstructured": "Food and Drug Administration (FDA). Fact sheet for healthcare providers: emergency use authorization for Evusheld ™ (tixagevimab co-packaged with cilgavimab). Silver Spring: FDA; 2023. Revoked: 26 Jan 2023. Available from: https://www.fda.gov/media/154701/download"
},
{
"DOI": "10.1038/s41591-022-01911-2",
"article-title": "Emergence of SARS-CoV-2 Omicron lineages BA.4 and BA.5 in South Africa.",
"author": "Tegally",
"doi-asserted-by": "crossref",
"first-page": "1785",
"issue": "9",
"journal-title": "Nat Med",
"key": "r12",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1038/s41586-022-04980-y",
"article-title": "BA.2.12.1, BA.4 and BA.5 escape antibodies elicited by Omicron infection.",
"author": "Cao",
"doi-asserted-by": "crossref",
"first-page": "593",
"issue": "7923",
"journal-title": "Nature",
"key": "r13",
"volume": "608",
"year": "2022"
},
{
"DOI": "10.1016/S1473-3099(22)00365-6",
"article-title": "Neutralisation sensitivity of SARS-CoV-2 omicron subvariants to therapeutic monoclonal antibodies.",
"author": "Yamasoba",
"doi-asserted-by": "crossref",
"first-page": "942",
"issue": "7",
"journal-title": "Lancet Infect Dis",
"key": "r14",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.1038/s41586-021-03944-y",
"article-title": "SARS-CoV-2 B.1.617.2 Delta variant replication and immune evasion.",
"author": "Mlcochova",
"doi-asserted-by": "crossref",
"first-page": "114",
"issue": "7883",
"journal-title": "Nature",
"key": "r15",
"volume": "599",
"year": "2021"
},
{
"key": "r16",
"unstructured": "European Centre for Disease Prevention and Control (ECDC). European Respiratory Virus Surveillance Summary (ERVISS). Stockholm: ECDC. [Accessed: 10 Mar 2025]. Available from: https://erviss.org/"
},
{
"key": "r17",
"unstructured": "European Centre for Disease Prevention and Control (ECDC) and World Health Organization Regional Office for Europe (WHO/Europe). Technical guidance for antigenic SARS-CoV-2 monitoring. Stockholm: ECDC and Copenhagen: WHO/Europe; Jun 2022 Available from: https://www.ecdc.europa.eu/sites/default/files/documents/Antigenic-SARS-CoV-2-monitoring-Joint-ECDC-WHO-report-June-2022.pdf"
},
{
"DOI": "10.1128/JCM.02504-20",
"article-title": "Evaluation of a SARS-CoV-2 surrogate virus neutralization test for detection of antibody in human, canine, cat, and hamster sera.",
"author": "Perera",
"doi-asserted-by": "crossref",
"first-page": "e02504",
"issue": "2",
"journal-title": "J Clin Microbiol",
"key": "r18",
"volume": "59",
"year": "2021"
},
{
"DOI": "10.1038/s41596-021-00536-y",
"article-title": "Quantification of SARS-CoV-2 neutralizing antibody by wild-type plaque reduction neutralization, microneutralization and pseudotyped virus neutralization assays.",
"author": "Bewley",
"doi-asserted-by": "crossref",
"first-page": "3114",
"issue": "6",
"journal-title": "Nat Protoc",
"key": "r19",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.2807/1560-7917.ES.2020.25.16.2000421",
"article-title": "Serological assays for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), March 2020.",
"author": "Perera",
"doi-asserted-by": "crossref",
"issue": "16",
"journal-title": "Euro Surveill",
"key": "r20",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0261045",
"article-title": "Coronavirus Resistance Database (CoV-RDB): SARS-CoV-2 susceptibility to monoclonal antibodies, convalescent plasma, and plasma from vaccinated persons.",
"author": "Tzou",
"doi-asserted-by": "crossref",
"issue": "3",
"journal-title": "PLoS One",
"key": "r21",
"volume": "17",
"year": "2022"
},
{
"article-title": "Tracking SARS-CoV-2 mutations and variants through the COG-UK-Mutation Explorer.",
"author": "Wright",
"issue": "1",
"journal-title": "Virus Evol",
"key": "r22",
"volume": "8",
"year": "2022"
},
{
"key": "r23",
"unstructured": "European Medicines Agency (EMA). Annex I - Summary of product characteristics, Regkirona. Amsterdam: EMA; 12 Nov 2021. Available from: https://www.ema.europa.eu/en/documents/product-information/regkirona-epar-product-information_en.pdf"
},
{
"key": "r24",
"unstructured": "European Medicines Agency (EMA). Annex I - Summary of product characteristics, Evusheld. Amsterdam: EMA; 2024. Available from: https://www.ema.europa.eu/en/documents/product-information/evusheld-epar-product-information_en.pdf"
},
{
"key": "r25",
"unstructured": "Food and Drug Administration (FDA). Fact sheet for healthcare providers: emergency use authorization (EUA) of Regen-CoV® (casirivimab and imdevimab). Silver Spring: FDA; 2021. Revoked: 13 Dec 2024. Available from: https://www.fda.gov/media/145611/download"
},
{
"key": "r26"
},
{
"key": "r27",
"unstructured": "European Centre for Disease Prevention and Control (ECDC). SARS-CoV-2 variant mutations conferring reduced susceptibility to antiviral drugs and monoclonal antibodies: a non-systematic literature review for surveillance purposes. Stockholm: ECDC; Jul 2023. Available from: https://www.ecdc.europa.eu/sites/default/files/documents/SARS-CoV-2_variant_mutations_conferring_reduced_susceptibility_to_antiviral_drugs_and_monoclonal_antibodies.pdf"
},
{
"article-title": "The dual function monoclonal antibodies VIR-7831 and VIR-7832 demonstrate potent in vitro and in vivo activity against SARS-CoV-2.",
"author": "Cathcart",
"journal-title": "bioRxiv",
"key": "r28",
"year": "2022"
},
{
"DOI": "10.1021/acscentsci.3c00538",
"article-title": "Naturally occurring mutations of SARS-CoV-2 main protease confer drug resistance to nirmatrelvir.",
"author": "Hu",
"doi-asserted-by": "crossref",
"first-page": "1658",
"issue": "8",
"journal-title": "ACS Cent Sci",
"key": "r29",
"volume": "9",
"year": "2023"
},
{
"DOI": "10.1021/acs.jcim.3c00344",
"article-title": "Integrative approach to dissect the drug resistance mechanism of the H172Y mutation of SARS-CoV-2 main protease.",
"author": "Clayton",
"doi-asserted-by": "crossref",
"first-page": "3521",
"issue": "11",
"journal-title": "J Chem Inf Model",
"key": "r30",
"volume": "63",
"year": "2023"
},
{
"DOI": "10.1038/s44259-023-00009-0",
"article-title": "Rapid resistance profiling of SARS-CoV-2 protease inhibitors.",
"author": "Moghadasi",
"doi-asserted-by": "crossref",
"first-page": "9",
"issue": "1",
"journal-title": "NPJ Antimicrob Resist",
"key": "r31",
"volume": "1",
"year": "2023"
},
{
"DOI": "10.1074/jbc.AC120.015720",
"article-title": "Template-dependent inhibition of coronavirus RNA-dependent RNA polymerase by remdesivir reveals a second mechanism of action.",
"author": "Tchesnokov",
"doi-asserted-by": "crossref",
"first-page": "16156",
"issue": "47",
"journal-title": "J Biol Chem",
"key": "r32",
"volume": "295",
"year": "2020"
},
{
"DOI": "10.1056/NEJMc2119407",
"article-title": "Efficacy of antibodies and antiviral drugs against Covid-19 Omicron variant.",
"author": "Takashita",
"doi-asserted-by": "crossref",
"first-page": "995",
"issue": "10",
"journal-title": "N Engl J Med",
"key": "r33",
"volume": "386",
"year": "2022"
},
{
"DOI": "10.1038/s41586-022-04474-x",
"article-title": "Altered TMPRSS2 usage by SARS-CoV-2 Omicron impacts infectivity and fusogenicity.",
"author": "Meng",
"doi-asserted-by": "crossref",
"first-page": "706",
"issue": "7902",
"journal-title": "Nature",
"key": "r34",
"volume": "603",
"year": "2022"
},
{
"article-title": "SARS-CoV-2 Omicron potently neutralized by a novel antibody with unique spike binding properties.",
"author": "Fenwick",
"journal-title": "bioRxiv",
"key": "r35",
"year": "2022"
},
{
"DOI": "10.1016/S1473-3099(22)00416-9",
"article-title": "Efficacy and safety of a single dose of casirivimab and imdevimab for the prevention of COVID-19 over an 8-month period: a randomised, double-blind, placebo-controlled trial.",
"author": "Herman",
"doi-asserted-by": "crossref",
"first-page": "1444",
"issue": "10",
"journal-title": "Lancet Infect Dis",
"key": "r36",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.1038/s41591-021-01678-y",
"article-title": "An infectious SARS-CoV-2 B.1.1.529 Omicron virus escapes neutralization by therapeutic monoclonal antibodies.",
"author": "VanBlargan",
"doi-asserted-by": "crossref",
"first-page": "490",
"issue": "3",
"journal-title": "Nat Med",
"key": "r37",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1016/j.intimp.2022.108570",
"article-title": "Regdanvimab in patients with mild-to-moderate SARS-CoV-2 infection: A propensity score-matched retrospective cohort study.",
"author": "Lee",
"doi-asserted-by": "crossref",
"journal-title": "Int Immunopharmacol",
"key": "r38",
"volume": "106",
"year": "2022"
},
{
"DOI": "10.1056/NEJMc2207519",
"article-title": "Efficacy of antibodies and antiviral drugs against Omicron BA.2.12.1, BA.4, and BA.5 subvariants.",
"author": "Takashita",
"doi-asserted-by": "crossref",
"first-page": "468",
"issue": "5",
"journal-title": "N Engl J Med",
"key": "r39",
"volume": "387",
"year": "2022"
},
{
"DOI": "10.1016/j.antiviral.2023.105638",
"article-title": "Activity of Sotrovimab against BQ.1.1 and XBB.1 Omicron sublineages in a hamster model.",
"author": "Driouich",
"doi-asserted-by": "crossref",
"journal-title": "Antiviral Res",
"key": "r40",
"volume": "215",
"year": "2023"
},
{
"DOI": "10.1038/s41467-022-31615-7",
"article-title": "Resilience of S309 and AZD7442 monoclonal antibody treatments against infection by SARS-CoV-2 Omicron lineage strains.",
"author": "Case",
"doi-asserted-by": "crossref",
"first-page": "3824",
"issue": "1",
"journal-title": "Nat Commun",
"key": "r41",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1016/j.jinf.2022.06.033",
"article-title": "Sotrovimab to prevent severe COVID-19 in high-risk patients infected with Omicron BA.2.",
"author": "Martin-Blondel",
"doi-asserted-by": "crossref",
"first-page": "e104",
"issue": "4",
"journal-title": "J Infect",
"key": "r42",
"volume": "85",
"year": "2022"
},
{
"DOI": "10.1007/s40121-022-00755-0",
"article-title": "Real-world effectiveness of sotrovimab for the early treatment of COVID-19 during SARS-CoV-2 Delta and Omicron waves in the USA.",
"author": "Cheng",
"doi-asserted-by": "crossref",
"first-page": "607",
"issue": "2",
"journal-title": "Infect Dis Ther",
"key": "r43",
"volume": "12",
"year": "2023"
},
{
"DOI": "10.1016/S1473-3099(23)00575-3",
"article-title": "Transmissibility, infectivity, and immune evasion of the SARS-CoV-2 BA.2.86 variant.",
"author": "Uriu",
"doi-asserted-by": "crossref",
"first-page": "e460",
"issue": "11",
"journal-title": "Lancet Infect Dis",
"key": "r44",
"volume": "23",
"year": "2023"
},
{
"DOI": "10.1016/S1473-3099(23)00588-1",
"article-title": "Sensitivity of the SARS-CoV-2 BA.2.86 variant to prevailing neutralising antibody responses.",
"author": "Sheward",
"doi-asserted-by": "crossref",
"first-page": "e462",
"issue": "11",
"journal-title": "Lancet Infect Dis",
"key": "r45",
"volume": "23",
"year": "2023"
},
{
"DOI": "10.1016/S1473-3099(23)00573-X",
"article-title": "Antigenicity and infectivity characterisation of SARS-CoV-2 BA.2.86.",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "e457",
"issue": "11",
"journal-title": "Lancet Infect Dis",
"key": "r46",
"volume": "23",
"year": "2023"
},
{
"DOI": "10.1038/s41598-021-03154-6",
"article-title": "Calibration of two validated SARS-CoV-2 pseudovirus neutralization assays for COVID-19 vaccine evaluation.",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "23921",
"issue": "1",
"journal-title": "Sci Rep",
"key": "r47",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1128/JCM.00527-21",
"article-title": "Evaluation of cell-based and surrogate SARS-CoV-2 neutralization assays.",
"author": "Sholukh",
"doi-asserted-by": "crossref",
"issue": "10",
"journal-title": "J Clin Microbiol",
"key": "r48",
"volume": "59",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(21)00527-4",
"article-title": "WHO International Standard for anti-SARS-CoV-2 immunoglobulin.",
"author": "Kristiansen",
"doi-asserted-by": "crossref",
"first-page": "1347",
"issue": "10282",
"journal-title": "Lancet",
"key": "r49",
"volume": "397",
"year": "2021"
}
],
"reference-count": 49,
"references-count": 49,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2025.30.10.2400252"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Impact of SARS-CoV-2 variant mutations on susceptibility to monoclonal antibodies and antiviral drugs: a non-systematic review, April 2022 to October 2024",
"type": "journal-article",
"update-policy": "https://doi.org/10.2807/1560-7917.es.crp2020",
"volume": "30"
}