Medications Modulating the Acid Sphingomyelinase/Ceramide System and 28-Day Mortality among Patients with SARS-CoV-2: An Observational Study
et al., Pharmaceuticals, doi:10.3390/ph16081107, Aug 2023
30th treatment shown to reduce risk in
November 2021, now with p = 0.00014 from 21 studies, recognized in 2 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
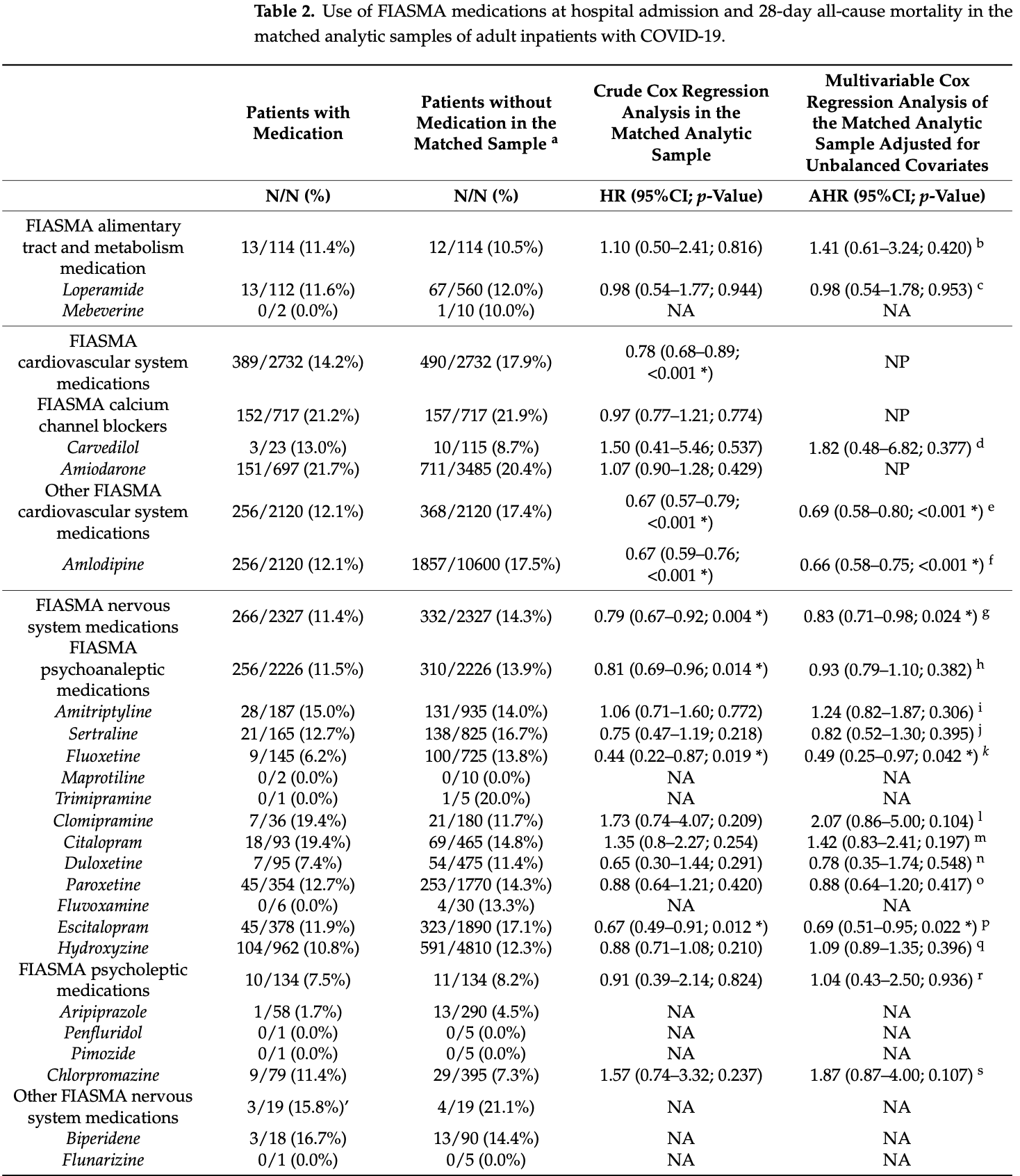
Retrospective 72,105 COVID+ hospitalized patients in France, showing lower mortality with FIASMA medications.
Study covers antihistamine H1RAs and fluvoxamine.
|
risk of death, 20.0% lower, HR 0.80, p < 0.001, treatment 625 of 4,857 (12.9%), control 772 of 4,857 (15.9%), NNT 33, day 28.
|
|
risk of death, 51.0% lower, HR 0.49, p = 0.04, treatment 9 of 145 (6.2%), control 100 of 725 (13.8%), NNT 13, adjusted per study, fluoxetine, multivariable, day 28.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Hoertel et al., 4 Aug 2023, retrospective, France, peer-reviewed, 14 authors, study period 2 May, 2020 - 31 August, 2022.
Contact: nico.hoertel@yahoo.fr (corresponding author), katrin.becker-flegler@uni-due.de.
Medications Modulating the Acid Sphingomyelinase/Ceramide System and 28-Day Mortality among Patients with SARS-CoV-2: An Observational Study
Pharmaceuticals, doi:10.3390/ph16081107
Prior evidence indicates the potential central role of the acid sphingomyelinase (ASM)/ ceramide system in the infection of cells with SARS-CoV-2. We conducted a multicenter retrospective observational study including 72,105 adult patients with laboratory-confirmed SARS-CoV-2 infection who were admitted to 36 AP-HP (Assistance Publique-Hôpitaux de Paris) hospitals from 2 May 2020 to 31 August 2022. We examined the association between the ongoing use of medications functionally inhibiting acid sphingomyelinase (FIASMA), which reduces the infection of cells with SARS-CoV-2 in vitro, upon hospital admission with 28-day all-cause mortality in a 1:1 ratio matched analytic sample based on clinical characteristics, disease severity and other medications (N = 9714). The univariate Cox regression model of the matched analytic sample showed that FIASMA medication use at admission was associated with significantly lower risks of 28-day mortality (HR = 0.80; 95% CI = 0.72-0.88; p < 0.001). In this multicenter observational study, the use of FIASMA medications was significantly and substantially associated with reduced 28-day mortality among adult patients hospitalized with COVID-19. These findings support the continuation of these medications during the treatment of SARS-CoV-2 infections. Randomized clinical trials (RCTs) are needed to confirm these results, starting with the molecules with the greatest effect size in the study, e.g., fluoxetine, escitalopram, and amlodipine.
References
Austin, Using the Standardized Difference to Compare the Prevalence of a Binary Variable between Two Groups in Observational Research, Commun. Stat. Simul. Comput, doi:10.1080/03610910902859574
Brunotte, Zheng, Mecate-Zambrano, Tang, Ludwig et al., Combination Therapy with Fluoxetine and the Nucleoside Analog GS-441524 Exerts Synergistic Antiviral Effects against Different SARS-CoV-2 Variants In Vitro, Pharmaceutics, doi:10.3390/pharmaceutics13091400
Butler, Hobbs, Gbinigie, Rahman, Hayward et al., Molnupiravir plus Usual Care versus Usual Care Alone as Early Treatment for Adults with COVID-19 at Increased Risk of Adverse Outcomes (PANORAMIC): An Open-Label, Platform-Adaptive Randomised Controlled Trial, Lancet, doi:10.1016/S0140-6736(22)02597-1
Calusic, Marcec, Luksa, Jurkovic, Kovac et al., Safety and Efficacy of Fluvoxamine in COVID-19 ICU Patients: An Open Label, Prospective Cohort Trial with Matched Controls, Br. J. Clin. Pharmacol, doi:10.1111/bcp.15126
Carpinteiro, Edwards, Hoffmann, Kochs, Gripp et al., Pharmacological Inhibition of Acid Sphingomyelinase Prevents Uptake of SARS-CoV-2 by Epithelial Cells, Cell Rep. Med, doi:10.1016/j.xcrm.2020.100142
Carpinteiro, Gripp, Hoffmann, Pöhlmann, Hoertel et al., Inhibition of Acid Sphingomyelinase by Ambroxol Prevents SARS-CoV-2 Entry into Epithelial Cells, J. Biol. Chem, doi:10.1016/j.jbc.2021.100701
Chen, Wu, Chen, Zhan, Wu et al., Sertraline Is an Effective SARS-CoV-2 Entry Inhibitor Targeting the Spike Protein, J. Virol, doi:10.1128/jvi.01245-22
Chevance, Gourion, Hoertel, Llorca, Thomas et al., Ensuring Mental Health Care during the SARS-CoV-2 Epidemic in France: A Narrative Review, L'Encephale, doi:10.1016/j.encep.2020.04.005
Cipriani, Furukawa, Salanti, Chaimani, Atkinson et al., Comparative Efficacy and Acceptability of 21 Antidepressant Drugs for the Acute Treatment of Adults with Major Depressive Disorder: A Systematic Review and Network Meta-Analysis, Lancet, doi:10.1016/S0140-6736(17)32802-7
Clelland, Ramiah, Steinberg, Clelland, Analysis of the Impact of Antidepressants and Other Medications on COVID-19 Infection Risk in a Chronic Psychiatric in-Patient Cohort, doi:10.1192/bjo.2021.1053
Creeden, Imami, Eby, Gillman, Becker et al., Fluoxetine as an Anti-Inflammatory Therapy in SARS-CoV-2 Infection, doi:10.1016/j.biopha.2021.111437
Darquennes, Le Corre, Le Moine, Loas, Association between Functional Inhibitors of Acid Sphingomyelinase (FIASMAs) and Reduced Risk of Death in COVID-19 Patients: A Retrospective Cohort Study, Pharmaceuticals, doi:10.3390/ph14030226
Dechaumes, Nekoua, Belouzard, Sane, Engelmann et al., Fluoxetine Can Inhibit SARS-CoV-2 In Vitro. Microorganisms 2021, doi:10.3390/microorganisms9020339
Dei Cas, Ottolenghi, Morano, Rinaldo, Roda et al., Link between Serum Lipid Signature and Prognostic Factors in COVID-19 Patients, Sci. Rep, doi:10.1038/s41598-021-00755-z
Deng, Rayner, Ramaraju, Abbas, Garcia et al., Efficacy and Safety of Selective Serotonin Reuptake Inhibitors in COVID-19 Management: A Systematic Review and Meta-Analysis, Clin. Microbiol. Infect, doi:10.1016/j.cmi.2023.01.010
Dhanavade, Sonawane, Role of Nutrition in COVID-19: Present Knowledge and Future Guidelines, Curr. Nutr. Food Sci, doi:10.2174/1573401318666220324115443
Elm, Altman, Egger, Pocock, Gøtzsche et al., The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies, Ann. Intern. Med, doi:10.7326/0003-4819-147-8-200710160-00010
Fred, Kuivanen, Ugurlu, Casarotto, Levanov et al., Antidepressant and Antipsychotic Drugs Reduce Viral Infection by SARS-CoV-2 and Fluoxetine Shows Antiviral Activity Against the Novel Variants in Vitro, Front. Pharmacol, doi:10.3389/fphar.2021.755600
Fritz, Hoertel, Lenze, Jalali, Reiersen, Association between Antidepressant Use and ED or Hospital Visits in Outpatients with SARS-CoV-2. Transl, Psychiatry, doi:10.1038/s41398-022-02109-3
Gulbins, Palmada, Reichel, Lüth, Böhmer et al., Acid Sphingomyelinase-Ceramide System Mediates Effects of Antidepressant Drugs, Nat. Med
Hashimoto, Suzuki, Hashimoto, Mechanisms of Action of Fluvoxamine for COVID-19: A Historical Review, Mol. Psychiatry, doi:10.1038/s41380-021-01432-3
Ho, Imai, King, Stuart, Matchit, Nonparametric Preprocessing for Parametric Causal Inference, J. Stat. Softw, doi:10.18637/jss.v042.i08
Hoertel, Blachier, Blanco, Olfson, Massetti et al., A Stochastic Agent-Based Model of the SARS-CoV-2 Epidemic in France, Nat. Med, doi:10.1038/s41591-020-1001-6
Hoertel, Blachier, Sánchez-Rico, Limosin, Leleu, Impact of the Timing and Adherence to Face Mask Use on the Course of the COVID-19 Epidemic in France, J. Travel Med, doi:10.1093/jtm/taab016
Hoertel, Boulware, Sánchez-Rico, Burgun, Limosin, Prevalence of Contraindications to Nirmatrelvir-Ritonavir among Hospitalized Patients With COVID-19 at Risk for Progression to Severe Disease, JAMA Netw. Open
Hoertel, Chevance, Limosin, Inclusion and Exclusion Criteria and Psychological Research
Hoertel, Do the Selective Serotonin Reuptake Inhibitor Antidepressants Fluoxetine and Fluvoxamine Reduce Mortality Among Patients With COVID-19?, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2021.36510
Hoertel, Rico, Vernet, Beeker, Jannot et al., Association between SSRI Antidepressant Use and Reduced Risk of Intubation or Death in Hospitalized Patients with Coronavirus Disease 2019: A Multicenter Retrospective Observational Study, doi:10.1101/2020.07.09.20143339
Hoertel, Sánchez-Rico, Cougoule, Gulbins, Kornhuber et al., Repurposing Antidepressants Inhibiting the Sphingomyelinase Acid/Ceramide System against COVID-19: Current Evidence and Potential Mechanisms, Mol. Psychiatry, doi:10.1038/s41380-021-01254-3
Hoertel, Sánchez-Rico, De La Muela, Abellán, Blanco et al., Risk of Death in Individuals Hospitalized for COVID-19 With and Without Psychiatric Disorders: An Observational Multicenter Study in France, Biol. Psychiatry Glob. Open Sci, doi:10.1016/j.bpsgos.2021.12.007
Hoertel, Sánchez-Rico, Gulbins, Kornhuber, Carpinteiro et al., Association Between FIASMAs and Reduced Risk of Intubation or Death in Individuals Hospitalized for Severe COVID-19: An Observational Multicenter Study, Clin. Pharmacol. Ther, doi:10.1002/cpt.2317
Hoertel, Sánchez-Rico, Gulbins, Kornhuber, Carpinteiro et al., Association between FIASMA Psychotropic Medications and Reduced Risk of Intubation or Death in Individuals with Psychiatric Disorders Hospitalized for Severe COVID-19: An Observational Multicenter Study, Transl. Psychiatry
Hoertel, Sánchez-Rico, Gulbins, Kornhuber, Vernet et al., Association between Benzodiazepine Receptor Agonist Use and Mortality in Patients Hospitalised for COVID-19: A Multicentre Observational Study, Epidemiol. Psychiatr. Sci, doi:10.1017/S2045796021000743
Hoertel, Sánchez-Rico, Herrera-Morueco, De La Muela, Gulbins et al., Comorbid Medical Conditions Are a Key Factor to Understand the Relationship between Psychiatric Disorders and COVID-19-Related Mortality: Results from 49,089 COVID-19 Inpatients, Mol. Psychiatry, doi:10.1038/s41380-021-01393-7
Hoertel, Sánchez-Rico, Kornhuber, Gulbins, Reiersen et al., Antidepressant Use and Its Association with 28-Day Mortality in Inpatients with SARS-CoV-2: Support for the FIASMA Model against COVID-19, J. Clin. Med, doi:10.3390/jcm11195882
Hoertel, Sánchez-Rico, Vernet, Beeker, Jannot et al., Association between Antidepressant Use and Reduced Risk of Intubation or Death in Hospitalized Patients with COVID-19: Results from an Observational Study, Mol. Psychiatry, doi:10.1038/s41380-021-01021-4
Hoertel, Sánchez-Rico, Vernet, Beeker, Neuraz et al., Dexamethasone Use and Mortality in Hospitalized Patients with Coronavirus Disease 2019: A Multicentre Retrospective Observational Study, Br. J. Clin. Pharmacol, doi:10.1111/bcp.14784
Hoertel, Sánchez-Rico, Vernet, Jannot, Neuraz et al., Observational Study of Chlorpromazine in Hospitalized Patients with COVID-19, Clin. Drug Investig, doi:10.1007/s40261-021-01001-0
Hoertel, Sánchez-Rico, Vernet, Jannot, Neuraz et al., Observational Study of Haloperidol in Hospitalized Patients with COVID-19, PLoS ONE, doi:10.1371/journal.pone.0247122
Khater, El-Khouly, Abdel-Bar, Al-Mahallawi, Ghorab, Fluoxetine Hydrochloride Loaded Lipid Polymer Hybrid Nanoparticles Showed Possible Efficiency against SARS-CoV-2 Infection, Int. J. Pharm, doi:10.1016/j.ijpharm.2021.121023
Khodadoust, Inferring a Causal Relationship between Ceramide Levels and COVID-19 Respiratory Distress, Sci. Rep, doi:10.1038/s41598-021-00286-7
Kirenga, Mugenyi, Sánchez-Rico, Kyobe, Muttamba et al., Association of Fluvoxamine with Mortality and Symptom Resolution among Inpatients with COVID-19 in Uganda: A Prospective Interventional Open-Label Cohort Study, Mol. Psychiatry, doi:10.1038/s41380-023-02004-3
Kornhuber, Hoertel, Gulbins, The Acid Sphingomyelinase/Ceramide System in COVID-19, Mol. Psychiatry, doi:10.1038/s41380-021-01309-5
Kornhuber, Muehlbacher, Trapp, Pechmann, Friedl et al., Identification of Novel Functional Inhibitors of Acid Sphingomyelinase, PLoS ONE, doi:10.1371/journal.pone.0023852
Kornhuber, Tripal, Reichel, Mühle, Rhein et al., Functional Inhibitors of Acid Sphingomyelinase (FIASMAs): A Novel Pharmacological Group of Drugs with Broad Clinical Applications, Cell. Physiol. Biochem, doi:10.1159/000315101
Kornhuber, Tripal, Reichel, Terfloth, Bleich et al., Identification of New Functional Inhibitors of Acid Sphingomyelinase Using a Structure-Property-Activity Relation Model, J. Med. Chem, doi:10.1021/jm070524a
Lagunas-Rangel, Neutrophil-to-Lymphocyte Ratio and Lymphocyte-to-C-Reactive Protein Ratio in Patients with Severe Coronavirus Disease 2019 (COVID-19): A Meta-Analysis, J. Med. Virol, doi:10.1002/jmv.25819
Lenze, Mattar, Zorumski, Stevens, Schweiger et al., Fluvoxamine vs Placebo and Clinical Deterioration in Outpatients With Symptomatic COVID-19: A Randomized Clinical Trial, JAMA, doi:10.1001/jama.2020.22760
Lenze, Reiersen, Santosh, Repurposing Fluvoxamine, and Other Psychiatric Medications, for COVID-19 and Other Conditions, World Psychiatry, doi:10.1002/wps.20983
Lim, Tignanelli, Hoertel, Boulware, Usher, Prevalence of Medical Contraindications to Nirmatrelvir/Ritonavir in a Cohort of Hospitalized and Nonhospitalized Patients With COVID-19, Open Forum Infect. Dis, doi:10.1093/ofid/ofac389
Loas, Van De Borne, Darquennes, Le Corre, Association of Amlodipine with the Risk of In-Hospital Death in Patients with COVID-19 and Hypertension: A Reanalysis on 184 COVID-19 Patients with Hypertension, Pharmaceuticals, doi:10.3390/ph15030380
Marín-Corral, Rodríguez-Morató, Gomez-Gomez, Pascual-Guardia, Muñoz-Bermúdez et al., Metabolic Signatures Associated with Severity in Hospitalized COVID-19 Patients, Int. J. Mol. Sci, doi:10.3390/ijms22094794
Matta, Wiernik, Robineau, Carrat, Touvier et al., Association of Self-Reported COVID-19 Infection and SARS-CoV-2 Serology Test Results With Persistent Physical Symptoms Among French Adults During the COVID-19 Pandemic, JAMA Intern. Med, doi:10.1001/jamainternmed.2021.6454
Mühle, Kremer, Vetter, Schmid, Achenbach et al., COVID-19 and Its Clinical Severity Are Associated with Alterations of Plasma Sphingolipids and Enzyme Activities of Sphingomyelinase and Ceramidase, doi:10.1101/2022.01.19.22269391
Naz, Asif, Alwutayd, Sarfaraz, Abbasi et al., Repurposing FIASMAs against Acid Sphingomyelinase for COVID-19: A Computational Molecular Docking and Dynamic Simulation Approach, Molecules, doi:10.3390/molecules28072989
Neuraz, Lerner, Digan, Paris, Tsopra et al., Natural Language Processing for Rapid Response to Emergent Diseases: Case Study of Calcium Channel Blockers and Hypertension in the COVID-19 Pandemic, J. Med. Internet Res, doi:10.2196/20773
Németh, Sz Űcs, Vitrai, Juhász, Németh et al., Fluoxetine Use Is Associated with Improved Survival of Patients with COVID-19 Pneumonia: A Retrospective Case-Control Study, Ideggyógy. Szle, doi:10.18071/isz.74.0389
Oskotsky, Marić, Tang, Oskotsky, Wong et al., Mortality Risk Among Patients With COVID-19 Prescribed Selective Serotonin Reuptake Inhibitor Antidepressants, JAMA Netw. Open
Petrache, Pujadas, Ganju, Serban, Borowiec et al., Marked Elevations in Lung and Plasma Ceramide in COVID-19 Linked to Microvascular Injury, doi:10.1172/jci.insight.156104
Péricat, Leon-Icaza, Sanchez Rico, Mühle, Zoicas et al., Antiviral and Anti-Inflammatory Activities of Fluoxetine in a SARS-CoV-2 Infection Mouse Model, Int. J. Mol. Sci, doi:10.3390/ijms232113623
Reis, Dos, Moreira-Silva, Silva, Thabane et al., Effect of Early Treatment with Fluvoxamine on Risk of Emergency Care and Hospitalisation among Patients with COVID-19: The TOGETHER Randomised, Platform Clinical Trial, Lancet Glob. Health, doi:10.1016/S2214-109X(21)00448-4
Schloer, Brunotte, Goretzko, Mecate-Zambrano, Korthals et al., Targeting the Endolysosomal Host-SARS-CoV-2 Interface by Clinically Licensed Functional Inhibitors of Acid Sphingomyelinase (FIASMA) Including the Antidepressant Fluoxetine, Emerg. Microbes Infect, doi:10.1080/22221751.2020.1829082
Schloer, Brunotte, Mecate-Zambrano, Zheng, Tang et al., Drug Synergy of Combinatory Treatment with Remdesivir and the Repurposed Drugs Fluoxetine and Itraconazole Effectively Impairs SARS-CoV-2 Infection in Vitro, Br. J. Pharmacol, doi:10.1111/bph.15418
Seftel, Boulware, Prospective Cohort of Fluvoxamine for Early Treatment of Coronavirus Disease 19, Open Forum Infect. Dis, doi:10.1093/ofid/ofab050
Solaimanzadeh, Nifedipine and Amlodipine Are Associated with Improved Mortality and Decreased Risk for Intubation and Mechanical Ventilation in Elderly Patients Hospitalized for COVID-19, Cureus, doi:10.7759/cureus.8069
Sonawane, Barale, Dhanavade, Waghmare, Nadaf et al., Structural Insights and Inhibition Mechanism of TMPRSS2 by Experimentally Known Inhibitors Camostat Mesylate, Nafamostat and Bromhexine Hydrochloride to Control SARS-Coronavirus-2: A Molecular Modeling Approach, Inform. Med. Unlocked, doi:10.1016/j.imu.2021.100597
Strat, Hoertel, Correlation Is No Causation: Gymnasium Proliferation and the Risk of Obesity, Addict. Abingdon Engl, doi:10.1111/j.1360-0443.2011.03547.x
Stuart, Lee, Leacy, Prognostic Score-Based Balance Measures Can Be a Useful Diagnostic for Propensity Score Methods in Comparative Effectiveness Research, J. Clin. Epidemiol, doi:10.1016/j.jclinepi.2013.01.013
Sukhatme, Reiersen, Vayttaden, Sukhatme, Fluvoxamine, A Review of Its Mechanism of Action and Its Role in COVID-19, Front. Pharmacol, doi:10.3389/fphar.2021.652688
Sánchez-Rico, De La Muela, Herrera-Morueco, Geoffroy, Limosin et al., AP-HP/Université de Paris/INSERM COVID-19 Research Collaboration/AP-HP COVID CDR Initiative/Entrepôt de Données de Santé AP-HP Consortium. Melatonin Does Not Reduce Mortality in Adult Hospitalized Patients with COVID-19: A Multicenter Retrospective Observational Study, J. Travel Med, doi:10.1093/jtm/taab195
Sánchez-Rico, Limosin, Vernet, Beeker, Neuraz et al., Hydroxyzine Use and Mortality in Patients Hospitalized for COVID-19: A Multicenter Observational Study, J. Clin. Med, doi:10.3390/jcm10245891
Sánchez-Rico, Rezaei, Delgado-Álvarez, Limosin, Hoertel et al., Comorbidity Patterns and Mortality Among Hospitalized Patients with Psychiatric Disorders and COVID-19, Rev. Bras. Psiquiatr, doi:10.47626/1516-4446-2023-3076
Terry, Grambsch, Modeling Survival Data: Extending the Cox Model
Tham, Jonsson, Andersson, Söderlund, Allard et al., Efficacy and Tolerability of Antidepressants in People Aged 65 Years or Older with Major Depressive Disorder-A Systematic Review and a Meta-Analysis, J. Affect. Disord, doi:10.1016/j.jad.2016.06.013
Torretta, Garziano, Poliseno, Capitanio, Biasin et al., Severity of COVID-19 Patients Predicted by Serum Sphingolipids Signature, Int. J. Mol. Sci, doi:10.3390/ijms221910198
Zhang, Kim, Lonjon, Zhu, None, Balance Diagnostics after Propensity Score Matching. Ann. Transl. Med, doi:10.21037/atm.2018.12.10
Zimniak, Kirschner, Hilpert, Geiger, Danov et al., The Serotonin Reuptake Inhibitor Fluoxetine Inhibits SARS-CoV-2 in Human Lung Tissue. Sci, doi:10.1038/s41598-021-85049-0
DOI record:
{
"DOI": "10.3390/ph16081107",
"ISSN": [
"1424-8247"
],
"URL": "http://dx.doi.org/10.3390/ph16081107",
"abstract": "<jats:p>Prior evidence indicates the potential central role of the acid sphingomyelinase (ASM)/ceramide system in the infection of cells with SARS-CoV-2. We conducted a multicenter retrospective observational study including 72,105 adult patients with laboratory-confirmed SARS-CoV-2 infection who were admitted to 36 AP-HP (Assistance Publique–Hôpitaux de Paris) hospitals from 2 May 2020 to 31 August 2022. We examined the association between the ongoing use of medications functionally inhibiting acid sphingomyelinase (FIASMA), which reduces the infection of cells with SARS-CoV-2 in vitro, upon hospital admission with 28-day all-cause mortality in a 1:1 ratio matched analytic sample based on clinical characteristics, disease severity and other medications (N = 9714). The univariate Cox regression model of the matched analytic sample showed that FIASMA medication use at admission was associated with significantly lower risks of 28-day mortality (HR = 0.80; 95% CI = 0.72–0.88; p < 0.001). In this multicenter observational study, the use of FIASMA medications was significantly and substantially associated with reduced 28-day mortality among adult patients hospitalized with COVID-19. These findings support the continuation of these medications during the treatment of SARS-CoV-2 infections. Randomized clinical trials (RCTs) are needed to confirm these results, starting with the molecules with the greatest effect size in the study, e.g., fluoxetine, escitalopram, and amlodipine.</jats:p>",
"alternative-id": [
"ph16081107"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-7890-1349",
"affiliation": [
{
"name": "INSERM U1266, Université Paris Cité, F-75014 Paris, France"
},
{
"name": "Service de Psychiatrie et Addictologie de l’adulte et du Sujet Agé, DMU Psychiatrie et Addictologie, Hôpital Corentin-Celton, GHU APHP.Centre, F-92130 Issy-les-Moulineaux, France"
}
],
"authenticated-orcid": false,
"family": "Hoertel",
"given": "Nicolas",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Service de Psychiatrie et Addictologie de l’adulte et du Sujet Agé, DMU Psychiatrie et Addictologie, Hôpital Corentin-Celton, GHU APHP.Centre, F-92130 Issy-les-Moulineaux, France"
}
],
"family": "Rezaei",
"given": "Katayoun",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1121-8641",
"affiliation": [
{
"name": "Service de Psychiatrie et Addictologie de l’adulte et du Sujet Agé, DMU Psychiatrie et Addictologie, Hôpital Corentin-Celton, GHU APHP.Centre, F-92130 Issy-les-Moulineaux, France"
},
{
"name": "Department of Psychobiology and Behavioural Sciences Methods, Faculty of Psychology, Universidad Complutense de Madrid, F-28223 Madrid, Spain"
}
],
"authenticated-orcid": false,
"family": "Sánchez-Rico",
"given": "Marina",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1889-4503",
"affiliation": [
{
"name": "Service de Psychiatrie et Addictologie de l’adulte et du Sujet Agé, DMU Psychiatrie et Addictologie, Hôpital Corentin-Celton, GHU APHP.Centre, F-92130 Issy-les-Moulineaux, France"
},
{
"name": "Department of Psychobiology and Behavioural Sciences Methods, Faculty of Psychology, Universidad Complutense de Madrid, F-28223 Madrid, Spain"
},
{
"name": "Department of Biological and Health Psychology, Faculty of Psychology, Universidad Autónoma de Madrid, F-28049 Madrid, Spain"
}
],
"authenticated-orcid": false,
"family": "Delgado-Álvarez",
"given": "Alfonso",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8096-3987",
"affiliation": [
{
"name": "Department of Psychiatry and Psychotherapy, University Hospital, Friedrich-Alexander-University of Erlangen-Nuremberg (FAU), 91054 Erlangen, Germany"
}
],
"authenticated-orcid": false,
"family": "Kornhuber",
"given": "Johannes",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Institute of Molecular Biology, University Hospital Essen, University of Duisburg-Essen, 47057 Essen, Germany"
}
],
"family": "Gulbins",
"given": "Erich",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Psychiatry, New York State Psychiatric Institute/Columbia University, New York, NY 10032, USA"
}
],
"family": "Olfson",
"given": "Mark",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3587-7182",
"affiliation": [
{
"name": "Service de Psychiatrie de l’Adulte, DMU Psychiatrie et Addictologie, Hôpital Hôtel-Dieu, AP-HP, Université Paris Cité, F-75004 Paris, France"
}
],
"authenticated-orcid": false,
"family": "Ouazana-Vedrines",
"given": "Charles",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Institute of Molecular Biology, University Hospital Essen, University of Duisburg-Essen, 47057 Essen, Germany"
},
{
"name": "Department of Hematology and Stem Cell Transplantation, University Hospital Essen, University of Duisburg-Essen, 47057 Essen, Germany"
}
],
"family": "Carpinteiro",
"given": "Alexander",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6795-5448",
"affiliation": [
{
"name": "Institute of Pharmacology and Structural Biology (IPBS), University of Toulouse, CNRS, 31000 Toulouse, France"
}
],
"authenticated-orcid": false,
"family": "Cougoule",
"given": "Céline",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6317-7298",
"affiliation": [
{
"name": "Institute of Molecular Biology, University Hospital Essen, University of Duisburg-Essen, 47057 Essen, Germany"
}
],
"authenticated-orcid": false,
"family": "Becker",
"given": "Katrin Anne",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4780-0147",
"affiliation": [
{
"name": "Department of Psychobiology and Behavioural Sciences Methods, Faculty of Psychology, Universidad Complutense de Madrid, F-28223 Madrid, Spain"
}
],
"authenticated-orcid": false,
"family": "Alvarado",
"given": "Jesús M.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "INSERM U1266, Université Paris Cité, F-75014 Paris, France"
},
{
"name": "Service de Psychiatrie et Addictologie de l’adulte et du Sujet Agé, DMU Psychiatrie et Addictologie, Hôpital Corentin-Celton, GHU APHP.Centre, F-92130 Issy-les-Moulineaux, France"
}
],
"family": "Limosin",
"given": "Frédéric",
"sequence": "additional"
},
{
"affiliation": [],
"name": "on behalf of AP-HP/Université Paris Cité/INSERM COVID-19 Research Collaboration, AP-HP COVID CDR Initiative and “Entrepôt de Données de Santé” AP-HP Consortium",
"sequence": "additional"
}
],
"container-title": "Pharmaceuticals",
"container-title-short": "Pharmaceuticals",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
8,
4
]
],
"date-time": "2023-08-04T13:27:48Z",
"timestamp": 1691155668000
},
"deposited": {
"date-parts": [
[
2023,
8,
4
]
],
"date-time": "2023-08-04T14:46:15Z",
"timestamp": 1691160375000
},
"indexed": {
"date-parts": [
[
2023,
8,
5
]
],
"date-time": "2023-08-05T04:24:25Z",
"timestamp": 1691209465597
},
"is-referenced-by-count": 0,
"issue": "8",
"issued": {
"date-parts": [
[
2023,
8,
4
]
]
},
"journal-issue": {
"issue": "8",
"published-online": {
"date-parts": [
[
2023,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
8,
4
]
],
"date-time": "2023-08-04T00:00:00Z",
"timestamp": 1691107200000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/1424-8247/16/8/1107/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1107",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
8,
4
]
]
},
"published-online": {
"date-parts": [
[
2023,
8,
4
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1016/j.encep.2020.04.005",
"article-title": "Ensuring Mental Health Care during the SARS-CoV-2 Epidemic in France: A Narrative Review",
"author": "Chevance",
"doi-asserted-by": "crossref",
"first-page": "193",
"journal-title": "L’Encephale",
"key": "ref_1",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1038/s41591-020-1001-6",
"article-title": "A Stochastic Agent-Based Model of the SARS-CoV-2 Epidemic in France",
"author": "Hoertel",
"doi-asserted-by": "crossref",
"first-page": "1417",
"journal-title": "Nat. Med.",
"key": "ref_2",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.3390/ijms22094794",
"doi-asserted-by": "crossref",
"key": "ref_3",
"unstructured": "Marín-Corral, J., Rodríguez-Morató, J., Gomez-Gomez, A., Pascual-Guardia, S., Muñoz-Bermúdez, R., Salazar-Degracia, A., Pérez-Terán, P., Restrepo, M.I., Khymenets, O., and Haro, N. (2021). Metabolic Signatures Associated with Severity in Hospitalized COVID-19 Patients. Int. J. Mol. Sci., 22."
},
{
"DOI": "10.3390/ijms221910198",
"doi-asserted-by": "crossref",
"key": "ref_4",
"unstructured": "Torretta, E., Garziano, M., Poliseno, M., Capitanio, D., Biasin, M., Santantonio, T.A., Clerici, M., Lo Caputo, S., Trabattoni, D., and Gelfi, C. (2021). Severity of COVID-19 Patients Predicted by Serum Sphingolipids Signature. Int. J. Mol. Sci., 22."
},
{
"DOI": "10.1101/2022.01.19.22269391",
"doi-asserted-by": "crossref",
"key": "ref_5",
"unstructured": "Mühle, C., Kremer, A., Vetter, M., Schmid, J., Achenbach, S., Schumacher, F., Lenz, B., Cougoule, C., Hoertel, N., and Carpinteiro, A. (2022). COVID-19 and Its Clinical Severity Are Associated with Alterations of Plasma Sphingolipids and Enzyme Activities of Sphingomyelinase and Ceramidase. medRxiv."
},
{
"DOI": "10.1093/jtm/taab016",
"article-title": "Impact of the Timing and Adherence to Face Mask Use on the Course of the COVID-19 Epidemic in France",
"author": "Hoertel",
"doi-asserted-by": "crossref",
"first-page": "taab016",
"journal-title": "J. Travel Med.",
"key": "ref_6",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.1093/ofid/ofac389",
"article-title": "Prevalence of Medical Contraindications to Nirmatrelvir/Ritonavir in a Cohort of Hospitalized and Nonhospitalized Patients With COVID-19",
"author": "Lim",
"doi-asserted-by": "crossref",
"first-page": "ofac389",
"journal-title": "Open Forum Infect. Dis.",
"key": "ref_7",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.1001/jamanetworkopen.2022.42140",
"article-title": "Prevalence of Contraindications to Nirmatrelvir-Ritonavir among Hospitalized Patients With COVID-19 at Risk for Progression to Severe Disease",
"author": "Hoertel",
"doi-asserted-by": "crossref",
"first-page": "e2242140",
"journal-title": "JAMA Netw. Open",
"key": "ref_8",
"volume": "5",
"year": "2022"
},
{
"DOI": "10.1001/jamanetworkopen.2021.36510",
"article-title": "Do the Selective Serotonin Reuptake Inhibitor Antidepressants Fluoxetine and Fluvoxamine Reduce Mortality Among Patients With COVID-19?",
"author": "Hoertel",
"doi-asserted-by": "crossref",
"first-page": "e2136510",
"journal-title": "JAMA Netw. Open",
"key": "ref_9",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1038/s41380-021-01393-7",
"article-title": "Comorbid Medical Conditions Are a Key Factor to Understand the Relationship between Psychiatric Disorders and COVID-19-Related Mortality: Results from 49,089 COVID-19 Inpatients",
"author": "Hoertel",
"doi-asserted-by": "crossref",
"first-page": "1278",
"journal-title": "Mol. Psychiatry",
"key": "ref_10",
"volume": "27",
"year": "2022"
},
{
"DOI": "10.1038/s41380-021-01254-3",
"article-title": "Repurposing Antidepressants Inhibiting the Sphingomyelinase Acid/Ceramide System against COVID-19: Current Evidence and Potential Mechanisms",
"author": "Hoertel",
"doi-asserted-by": "crossref",
"first-page": "7098",
"journal-title": "Mol. Psychiatry",
"key": "ref_11",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.1038/s41380-021-01309-5",
"article-title": "The Acid Sphingomyelinase/Ceramide System in COVID-19",
"author": "Kornhuber",
"doi-asserted-by": "crossref",
"first-page": "307",
"journal-title": "Mol. Psychiatry",
"key": "ref_12",
"volume": "27",
"year": "2022"
},
{
"DOI": "10.1016/j.xcrm.2020.100142",
"article-title": "Pharmacological Inhibition of Acid Sphingomyelinase Prevents Uptake of SARS-CoV-2 by Epithelial Cells",
"author": "Carpinteiro",
"doi-asserted-by": "crossref",
"first-page": "100142",
"journal-title": "Cell Rep. Med.",
"key": "ref_13",
"volume": "1",
"year": "2020"
},
{
"DOI": "10.1172/jci.insight.156104",
"article-title": "Marked Elevations in Lung and Plasma Ceramide in COVID-19 Linked to Microvascular Injury",
"author": "Petrache",
"doi-asserted-by": "crossref",
"first-page": "e156104",
"journal-title": "JCI Insight",
"key": "ref_14",
"volume": "8",
"year": "2023"
},
{
"DOI": "10.1016/j.jbc.2021.100701",
"article-title": "Inhibition of Acid Sphingomyelinase by Ambroxol Prevents SARS-CoV-2 Entry into Epithelial Cells",
"author": "Carpinteiro",
"doi-asserted-by": "crossref",
"first-page": "100701",
"journal-title": "J. Biol. Chem.",
"key": "ref_15",
"volume": "296",
"year": "2021"
},
{
"DOI": "10.1159/000315101",
"article-title": "Functional Inhibitors of Acid Sphingomyelinase (FIASMAs): A Novel Pharmacological Group of Drugs with Broad Clinical Applications",
"author": "Kornhuber",
"doi-asserted-by": "crossref",
"first-page": "9",
"journal-title": "Cell. Physiol. Biochem.",
"key": "ref_16",
"volume": "26",
"year": "2010"
},
{
"DOI": "10.3390/ijms232113623",
"doi-asserted-by": "crossref",
"key": "ref_17",
"unstructured": "Péricat, D., Leon-Icaza, S.A., Sanchez Rico, M., Mühle, C., Zoicas, I., Schumacher, F., Planès, R., Mazars, R., Gros, G., and Carpinteiro, A. (2022). Antiviral and Anti-Inflammatory Activities of Fluoxetine in a SARS-CoV-2 Infection Mouse Model. Int. J. Mol. Sci., 23."
},
{
"DOI": "10.1080/22221751.2020.1829082",
"article-title": "Targeting the Endolysosomal Host-SARS-CoV-2 Interface by Clinically Licensed Functional Inhibitors of Acid Sphingomyelinase (FIASMA) Including the Antidepressant Fluoxetine",
"author": "Schloer",
"doi-asserted-by": "crossref",
"first-page": "2245",
"journal-title": "Emerg. Microbes Infect.",
"key": "ref_18",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.3389/fphar.2021.755600",
"article-title": "Antidepressant and Antipsychotic Drugs Reduce Viral Infection by SARS-CoV-2 and Fluoxetine Shows Antiviral Activity Against the Novel Variants in Vitro",
"author": "Fred",
"doi-asserted-by": "crossref",
"first-page": "755600",
"journal-title": "Front. Pharmacol.",
"key": "ref_19",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1128/jvi.01245-22",
"article-title": "Sertraline Is an Effective SARS-CoV-2 Entry Inhibitor Targeting the Spike Protein",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "e01245-22",
"journal-title": "J. Virol.",
"key": "ref_20",
"volume": "96",
"year": "2022"
},
{
"DOI": "10.1016/j.ijpharm.2021.121023",
"article-title": "Fluoxetine Hydrochloride Loaded Lipid Polymer Hybrid Nanoparticles Showed Possible Efficiency against SARS-CoV-2 Infection",
"author": "Khater",
"doi-asserted-by": "crossref",
"first-page": "121023",
"journal-title": "Int. J. Pharm.",
"key": "ref_21",
"volume": "607",
"year": "2021"
},
{
"DOI": "10.3390/pharmaceutics13091400",
"doi-asserted-by": "crossref",
"key": "ref_22",
"unstructured": "Brunotte, L., Zheng, S., Mecate-Zambrano, A., Tang, J., Ludwig, S., Rescher, U., and Schloer, S. (2021). Combination Therapy with Fluoxetine and the Nucleoside Analog GS-441524 Exerts Synergistic Antiviral Effects against Different SARS-CoV-2 Variants In Vitro. Pharmaceutics, 13."
},
{
"DOI": "10.3390/microorganisms9020339",
"doi-asserted-by": "crossref",
"key": "ref_23",
"unstructured": "Dechaumes, A., Nekoua, M.P., Belouzard, S., Sane, F., Engelmann, I., Dubuisson, J., Alidjinou, E.K., and Hober, D. (2021). Fluoxetine Can Inhibit SARS-CoV-2 In Vitro. Microorganisms, 9."
},
{
"DOI": "10.1111/bph.15418",
"article-title": "Drug Synergy of Combinatory Treatment with Remdesivir and the Repurposed Drugs Fluoxetine and Itraconazole Effectively Impairs SARS-CoV-2 Infection in Vitro",
"author": "Schloer",
"doi-asserted-by": "crossref",
"first-page": "2339",
"journal-title": "Br. J. Pharmacol.",
"key": "ref_24",
"volume": "178",
"year": "2021"
},
{
"DOI": "10.1038/s41598-021-85049-0",
"article-title": "The Serotonin Reuptake Inhibitor Fluoxetine Inhibits SARS-CoV-2 in Human Lung Tissue",
"author": "Zimniak",
"doi-asserted-by": "crossref",
"first-page": "5890",
"journal-title": "Sci. Rep.",
"key": "ref_25",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1002/cpt.2317",
"article-title": "Association Between FIASMAs and Reduced Risk of Intubation or Death in Individuals Hospitalized for Severe COVID-19: An Observational Multicenter Study",
"author": "Hoertel",
"doi-asserted-by": "crossref",
"first-page": "1498",
"journal-title": "Clin. Pharmacol. Ther.",
"key": "ref_26",
"volume": "110",
"year": "2021"
},
{
"DOI": "10.1038/s41380-021-01021-4",
"article-title": "Association between Antidepressant Use and Reduced Risk of Intubation or Death in Hospitalized Patients with COVID-19: Results from an Observational Study",
"author": "Hoertel",
"doi-asserted-by": "crossref",
"first-page": "5199",
"journal-title": "Mol. Psychiatry",
"key": "ref_27",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.1038/s41398-022-01804-5",
"article-title": "Association between FIASMA Psychotropic Medications and Reduced Risk of Intubation or Death in Individuals with Psychiatric Disorders Hospitalized for Severe COVID-19: An Observational Multicenter Study",
"author": "Hoertel",
"doi-asserted-by": "crossref",
"first-page": "90",
"journal-title": "Transl. Psychiatry",
"key": "ref_28",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.3390/jcm11195882",
"doi-asserted-by": "crossref",
"key": "ref_29",
"unstructured": "Hoertel, N., Sánchez-Rico, M., Kornhuber, J., Gulbins, E., Reiersen, A.M., Lenze, E.J., Fritz, B.A., Jalali, F., Mills, E.J., and Cougoule, C. (2022). Antidepressant Use and Its Association with 28-Day Mortality in Inpatients with SARS-CoV-2: Support for the FIASMA Model against COVID-19. J. Clin. Med., 11."
},
{
"DOI": "10.1001/jamanetworkopen.2021.33090",
"article-title": "Mortality Risk Among Patients With COVID-19 Prescribed Selective Serotonin Reuptake Inhibitor Antidepressants",
"author": "Oskotsky",
"doi-asserted-by": "crossref",
"first-page": "e2133090",
"journal-title": "JAMA Netw. Open",
"key": "ref_30",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.3390/ph14030226",
"doi-asserted-by": "crossref",
"key": "ref_31",
"unstructured": "Darquennes, G., Le Corre, P., Le Moine, O., and Loas, G. (2021). Association between Functional Inhibitors of Acid Sphingomyelinase (FIASMAs) and Reduced Risk of Death in COVID-19 Patients: A Retrospective Cohort Study. Pharmaceuticals, 14."
},
{
"DOI": "10.3390/ph15030380",
"doi-asserted-by": "crossref",
"key": "ref_32",
"unstructured": "Loas, G., Van De Borne, P., Darquennes, G., and Le Corre, P. (2022). Association of Amlodipine with the Risk of In-Hospital Death in Patients with COVID-19 and Hypertension: A Reanalysis on 184 COVID-19 Patients with Hypertension. Pharmaceuticals, 15."
},
{
"DOI": "10.1038/s41398-022-02109-3",
"article-title": "Association between Antidepressant Use and ED or Hospital Visits in Outpatients with SARS-CoV-2",
"author": "Fritz",
"doi-asserted-by": "crossref",
"first-page": "341",
"journal-title": "Transl. Psychiatry",
"key": "ref_33",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1016/j.cmi.2023.01.010",
"article-title": "Efficacy and Safety of Selective Serotonin Reuptake Inhibitors in COVID-19 Management: A Systematic Review and Meta-Analysis",
"author": "Deng",
"doi-asserted-by": "crossref",
"first-page": "578",
"journal-title": "Clin. Microbiol. Infect.",
"key": "ref_34",
"volume": "29",
"year": "2023"
},
{
"DOI": "10.3390/jcm10245891",
"doi-asserted-by": "crossref",
"key": "ref_35",
"unstructured": "Sánchez-Rico, M., Limosin, F., Vernet, R., Beeker, N., Neuraz, A., Blanco, C., Olfson, M., Lemogne, C., Meneton, P., and Daniel, C. (2021). Hydroxyzine Use and Mortality in Patients Hospitalized for COVID-19: A Multicenter Observational Study. J. Clin. Med., 10."
},
{
"DOI": "10.1038/nm.3214",
"article-title": "Acid Sphingomyelinase–Ceramide System Mediates Effects of Antidepressant Drugs",
"author": "Gulbins",
"doi-asserted-by": "crossref",
"first-page": "934",
"journal-title": "Nat. Med.",
"key": "ref_36",
"volume": "19",
"year": "2013"
},
{
"DOI": "10.1021/jm070524a",
"article-title": "Identification of New Functional Inhibitors of Acid Sphingomyelinase Using a Structure-Property-Activity Relation Model",
"author": "Kornhuber",
"doi-asserted-by": "crossref",
"first-page": "219",
"journal-title": "J. Med. Chem.",
"key": "ref_37",
"volume": "51",
"year": "2008"
},
{
"DOI": "10.3390/molecules28072989",
"doi-asserted-by": "crossref",
"key": "ref_38",
"unstructured": "Naz, A., Asif, S., Alwutayd, K.M., Sarfaraz, S., Abbasi, S.W., Abbasi, A., Alenazi, A.M., and Hasan, M.E. (2023). Repurposing FIASMAs against Acid Sphingomyelinase for COVID-19: A Computational Molecular Docking and Dynamic Simulation Approach. Molecules, 28."
},
{
"DOI": "10.1192/bjo.2021.1053",
"article-title": "Analysis of the Impact of Antidepressants and Other Medications on COVID-19 Infection Risk in a Chronic Psychiatric in-Patient Cohort",
"author": "Clelland",
"doi-asserted-by": "crossref",
"first-page": "e6",
"journal-title": "BJPsych Open",
"key": "ref_39",
"volume": "8",
"year": "2022"
},
{
"DOI": "10.1001/jama.2020.22760",
"article-title": "Fluvoxamine vs Placebo and Clinical Deterioration in Outpatients With Symptomatic COVID-19: A Randomized Clinical Trial",
"author": "Lenze",
"doi-asserted-by": "crossref",
"first-page": "2292",
"journal-title": "JAMA",
"key": "ref_40",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1016/S2214-109X(21)00448-4",
"article-title": "Effect of Early Treatment with Fluvoxamine on Risk of Emergency Care and Hospitalisation among Patients with COVID-19: The TOGETHER Randomised, Platform Clinical Trial",
"author": "Reis",
"doi-asserted-by": "crossref",
"first-page": "e42",
"journal-title": "Lancet Glob. Health",
"key": "ref_41",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1093/ofid/ofab050",
"article-title": "Prospective Cohort of Fluvoxamine for Early Treatment of Coronavirus Disease 19",
"author": "Seftel",
"doi-asserted-by": "crossref",
"first-page": "ofab050",
"journal-title": "Open Forum Infect. Dis.",
"key": "ref_42",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1111/bcp.15126",
"article-title": "Safety and Efficacy of Fluvoxamine in COVID-19 ICU Patients: An Open Label, Prospective Cohort Trial with Matched Controls",
"author": "Calusic",
"doi-asserted-by": "crossref",
"first-page": "2065",
"journal-title": "Br. J. Clin. Pharmacol.",
"key": "ref_43",
"volume": "88",
"year": "2022"
},
{
"DOI": "10.1101/2020.07.09.20143339",
"doi-asserted-by": "crossref",
"key": "ref_44",
"unstructured": "Hoertel, N., Rico, M.S., Vernet, R., Beeker, N., Jannot, A.-S., Neuraz, A., Salamanca, E., Paris, N., Daniel, C., and Gramfort, A. (2020). Association between SSRI Antidepressant Use and Reduced Risk of Intubation or Death in Hospitalized Patients with Coronavirus Disease 2019: A Multicenter Retrospective Observational Study. medRxiv."
},
{
"article-title": "Association of Fluvoxamine with Mortality and Symptom Resolution among Inpatients with COVID-19 in Uganda: A Prospective Interventional Open-Label Cohort Study",
"author": "Kirenga",
"first-page": "1",
"journal-title": "Mol. Psychiatry",
"key": "ref_45",
"volume": "3",
"year": "2023"
},
{
"DOI": "10.18071/isz.74.0389",
"article-title": "Fluoxetine Use Is Associated with Improved Survival of Patients with COVID-19 Pneumonia: A Retrospective Case-Control Study",
"author": "Vitrai",
"doi-asserted-by": "crossref",
"first-page": "389",
"journal-title": "Ideggyógy. Szle.",
"key": "ref_46",
"volume": "74",
"year": "2021"
},
{
"DOI": "10.1016/j.biopha.2021.111437",
"article-title": "Fluoxetine as an Anti-Inflammatory Therapy in SARS-CoV-2 Infection",
"author": "Creeden",
"doi-asserted-by": "crossref",
"first-page": "111437",
"journal-title": "Biomed. Pharmacother.",
"key": "ref_47",
"volume": "138",
"year": "2021"
},
{
"article-title": "Nifedipine and Amlodipine Are Associated with Improved Mortality and Decreased Risk for Intubation and Mechanical Ventilation in Elderly Patients Hospitalized for COVID-19",
"author": "Solaimanzadeh",
"first-page": "e8069",
"journal-title": "Cureus",
"key": "ref_48",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1038/s41598-021-00286-7",
"article-title": "Inferring a Causal Relationship between Ceramide Levels and COVID-19 Respiratory Distress",
"author": "Khodadoust",
"doi-asserted-by": "crossref",
"first-page": "20866",
"journal-title": "Sci. Rep.",
"key": "ref_49",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1038/s41598-021-00755-z",
"article-title": "Link between Serum Lipid Signature and Prognostic Factors in COVID-19 Patients",
"author": "Ottolenghi",
"doi-asserted-by": "crossref",
"first-page": "21633",
"journal-title": "Sci. Rep.",
"key": "ref_50",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1001/jamainternmed.2021.6454",
"article-title": "Association of Self-Reported COVID-19 Infection and SARS-CoV-2 Serology Test Results With Persistent Physical Symptoms Among French Adults During the COVID-19 Pandemic",
"author": "Matta",
"doi-asserted-by": "crossref",
"first-page": "19",
"journal-title": "JAMA Intern. Med.",
"key": "ref_51",
"volume": "182",
"year": "2022"
},
{
"DOI": "10.1371/journal.pone.0023852",
"doi-asserted-by": "crossref",
"key": "ref_52",
"unstructured": "Kornhuber, J., Muehlbacher, M., Trapp, S., Pechmann, S., Friedl, A., Reichel, M., Mühle, C., Terfloth, L., Groemer, T.W., and Spitzer, G.M. (2011). Identification of Novel Functional Inhibitors of Acid Sphingomyelinase. PLoS ONE, 6."
},
{
"DOI": "10.1016/j.jad.2016.06.013",
"article-title": "Efficacy and Tolerability of Antidepressants in People Aged 65 Years or Older with Major Depressive Disorder—A Systematic Review and a Meta-Analysis",
"author": "Tham",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "J. Affect. Disord.",
"key": "ref_53",
"volume": "205",
"year": "2016"
},
{
"DOI": "10.1016/S0140-6736(17)32802-7",
"article-title": "Comparative Efficacy and Acceptability of 21 Antidepressant Drugs for the Acute Treatment of Adults with Major Depressive Disorder: A Systematic Review and Network Meta-Analysis",
"author": "Cipriani",
"doi-asserted-by": "crossref",
"first-page": "1357",
"journal-title": "Lancet",
"key": "ref_54",
"volume": "391",
"year": "2018"
},
{
"DOI": "10.3389/fphar.2021.652688",
"article-title": "Fluvoxamine: A Review of Its Mechanism of Action and Its Role in COVID-19",
"author": "Sukhatme",
"doi-asserted-by": "crossref",
"first-page": "652688",
"journal-title": "Front. Pharmacol.",
"key": "ref_55",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1038/s41380-021-01432-3",
"article-title": "Mechanisms of Action of Fluvoxamine for COVID-19: A Historical Review",
"author": "Hashimoto",
"doi-asserted-by": "crossref",
"first-page": "1898",
"journal-title": "Mol. Psychiatry",
"key": "ref_56",
"volume": "27",
"year": "2022"
},
{
"DOI": "10.1002/wps.20983",
"article-title": "Repurposing Fluvoxamine, and Other Psychiatric Medications, for COVID-19 and Other Conditions",
"author": "Lenze",
"doi-asserted-by": "crossref",
"first-page": "314",
"journal-title": "World Psychiatry",
"key": "ref_57",
"volume": "21",
"year": "2022"
},
{
"article-title": "Correlation Is No Causation: Gymnasium Proliferation and the Risk of Obesity",
"author": "Hoertel",
"first-page": "1871",
"journal-title": "Addict. Abingdon Engl.",
"key": "ref_58",
"volume": "106",
"year": "2011"
},
{
"DOI": "10.2174/1573401318666220324115443",
"article-title": "Role of Nutrition in COVID-19: Present Knowledge and Future Guidelines",
"author": "Dhanavade",
"doi-asserted-by": "crossref",
"first-page": "516",
"journal-title": "Curr. Nutr. Food Sci.",
"key": "ref_59",
"volume": "18",
"year": "2022"
},
{
"key": "ref_60",
"unstructured": "Hoertel, N., Chevance, A., and Limosin, F. (2017). The SAGE Encyclopedia of Abnorma l and Clinical Psychology, SAGE Reference."
},
{
"DOI": "10.1016/S0140-6736(22)02597-1",
"article-title": "Molnupiravir plus Usual Care versus Usual Care Alone as Early Treatment for Adults with COVID-19 at Increased Risk of Adverse Outcomes (PANORAMIC): An Open-Label, Platform-Adaptive Randomised Controlled Trial",
"author": "Butler",
"doi-asserted-by": "crossref",
"first-page": "281",
"journal-title": "Lancet",
"key": "ref_61",
"volume": "401",
"year": "2023"
},
{
"DOI": "10.1371/journal.pone.0247122",
"doi-asserted-by": "crossref",
"key": "ref_62",
"unstructured": "Hoertel, N., Sánchez-Rico, M., Vernet, R., Jannot, A.-S., Neuraz, A., Blanco, C., Lemogne, C., Airagnes, G., Paris, N., and Daniel, C. (2021). Observational Study of Haloperidol in Hospitalized Patients with COVID-19. PLoS ONE, 16."
},
{
"DOI": "10.1007/s40261-021-01001-0",
"article-title": "Observational Study of Chlorpromazine in Hospitalized Patients with COVID-19",
"author": "Hoertel",
"doi-asserted-by": "crossref",
"first-page": "221",
"journal-title": "Clin. Drug Investig.",
"key": "ref_63",
"volume": "41",
"year": "2021"
},
{
"DOI": "10.1111/bcp.14784",
"article-title": "Dexamethasone Use and Mortality in Hospitalized Patients with Coronavirus Disease 2019: A Multicentre Retrospective Observational Study",
"author": "Hoertel",
"doi-asserted-by": "crossref",
"first-page": "3766",
"journal-title": "Br. J. Clin. Pharmacol.",
"key": "ref_64",
"volume": "87",
"year": "2021"
},
{
"DOI": "10.1017/S2045796021000743",
"article-title": "Association between Benzodiazepine Receptor Agonist Use and Mortality in Patients Hospitalised for COVID-19: A Multicentre Observational Study",
"author": "Hoertel",
"doi-asserted-by": "crossref",
"first-page": "e18",
"journal-title": "Epidemiol. Psychiatr. Sci.",
"key": "ref_65",
"volume": "31",
"year": "2022"
},
{
"DOI": "10.1093/jtm/taab195",
"article-title": "Melatonin Does Not Reduce Mortality in Adult Hospitalized Patients with COVID-19: A Multicenter Retrospective Observational Study",
"author": "Geoffroy",
"doi-asserted-by": "crossref",
"first-page": "taab195",
"journal-title": "J. Travel Med.",
"key": "ref_66",
"volume": "29",
"year": "2022"
},
{
"DOI": "10.1016/j.bpsgos.2021.12.007",
"article-title": "Risk of Death in Individuals Hospitalized for COVID-19 With and Without Psychiatric Disorders: An Observational Multicenter Study in France",
"author": "Hoertel",
"doi-asserted-by": "crossref",
"first-page": "56",
"journal-title": "Biol. Psychiatry Glob. Open Sci.",
"key": "ref_67",
"volume": "3",
"year": "2023"
},
{
"DOI": "10.47626/1516-4446-2023-3076",
"doi-asserted-by": "crossref",
"key": "ref_68",
"unstructured": "Sánchez-Rico, M., Rezaei, K., Delgado-Álvarez, A., Limosin, F., Hoertel, N., and Alvarado, J.M. (2023). Comorbidity Patterns and Mortality Among Hospitalized Patients with Psychiatric Disorders and COVID-19. Rev. Bras. Psiquiatr."
},
{
"key": "ref_69",
"unstructured": "Haut Conseil de la Santé Publique (2020, May 01). Statement on the Management at Home or in a Care Facility of Suspected or Confirmed COVID-19 Patients. Available online: https://www.hcsp.fr."
},
{
"DOI": "10.1002/jmv.25819",
"article-title": "Neutrophil-to-Lymphocyte Ratio and Lymphocyte-to-C-Reactive Protein Ratio in Patients with Severe Coronavirus Disease 2019 (COVID-19): A Meta-Analysis",
"doi-asserted-by": "crossref",
"first-page": "1733",
"journal-title": "J. Med. Virol.",
"key": "ref_70",
"volume": "92",
"year": "2020"
},
{
"DOI": "10.2196/20773",
"article-title": "Natural Language Processing for Rapid Response to Emergent Diseases: Case Study of Calcium Channel Blockers and Hypertension in the COVID-19 Pandemic",
"author": "Neuraz",
"doi-asserted-by": "crossref",
"first-page": "e20773",
"journal-title": "J. Med. Internet Res.",
"key": "ref_71",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.1016/j.jclinepi.2013.01.013",
"article-title": "Prognostic Score–Based Balance Measures Can Be a Useful Diagnostic for Propensity Score Methods in Comparative Effectiveness Research",
"author": "Stuart",
"doi-asserted-by": "crossref",
"first-page": "S84",
"journal-title": "J. Clin. Epidemiol.",
"key": "ref_72",
"volume": "66",
"year": "2013"
},
{
"DOI": "10.1080/03610910902859574",
"article-title": "Using the Standardized Difference to Compare the Prevalence of a Binary Variable between Two Groups in Observational Research",
"author": "Austin",
"doi-asserted-by": "crossref",
"first-page": "1228",
"journal-title": "Commun. Stat. Simul. Comput.",
"key": "ref_73",
"volume": "38",
"year": "2009"
},
{
"DOI": "10.21037/atm.2018.12.10",
"article-title": "Balance Diagnostics after Propensity Score Matching",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "16",
"journal-title": "Ann. Transl. Med.",
"key": "ref_74",
"volume": "7",
"year": "2019"
},
{
"key": "ref_75",
"unstructured": "Terry, M.T., and Grambsch, P.M. (2000). Modeling Survival Data: Extending the Cox Model, Springer."
},
{
"DOI": "10.18637/jss.v042.i08",
"article-title": "MatchIt: Nonparametric Preprocessing for Parametric Causal Inference",
"author": "Ho",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "J. Stat. Softw.",
"key": "ref_76",
"volume": "42",
"year": "2011"
},
{
"DOI": "10.7326/0003-4819-147-8-200710160-00010",
"article-title": "The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies",
"author": "Altman",
"doi-asserted-by": "crossref",
"first-page": "573",
"journal-title": "Ann. Intern. Med.",
"key": "ref_77",
"volume": "147",
"year": "2007"
},
{
"DOI": "10.1016/j.imu.2021.100597",
"article-title": "Structural Insights and Inhibition Mechanism of TMPRSS2 by Experimentally Known Inhibitors Camostat Mesylate, Nafamostat and Bromhexine Hydrochloride to Control SARS-Coronavirus-2: A Molecular Modeling Approach",
"author": "Sonawane",
"doi-asserted-by": "crossref",
"first-page": "100597",
"journal-title": "Inform. Med. Unlocked",
"key": "ref_78",
"volume": "24",
"year": "2021"
}
],
"reference-count": 78,
"references-count": 78,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/1424-8247/16/8/1107"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Drug Discovery",
"Pharmaceutical Science",
"Molecular Medicine"
],
"subtitle": [],
"title": "Medications Modulating the Acid Sphingomyelinase/Ceramide System and 28-Day Mortality among Patients with SARS-CoV-2: An Observational Study",
"type": "journal-article",
"volume": "16"
}
