Association between antidepressant use and ED or hospital visits in outpatients with SARS-CoV-2
et al., Translational Psychiatry, doi:10.1038/s41398-022-02109-3, Aug 2022
31st treatment shown to reduce risk in
November 2021, now with p = 0.00014 from 21 studies, recognized in 2 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
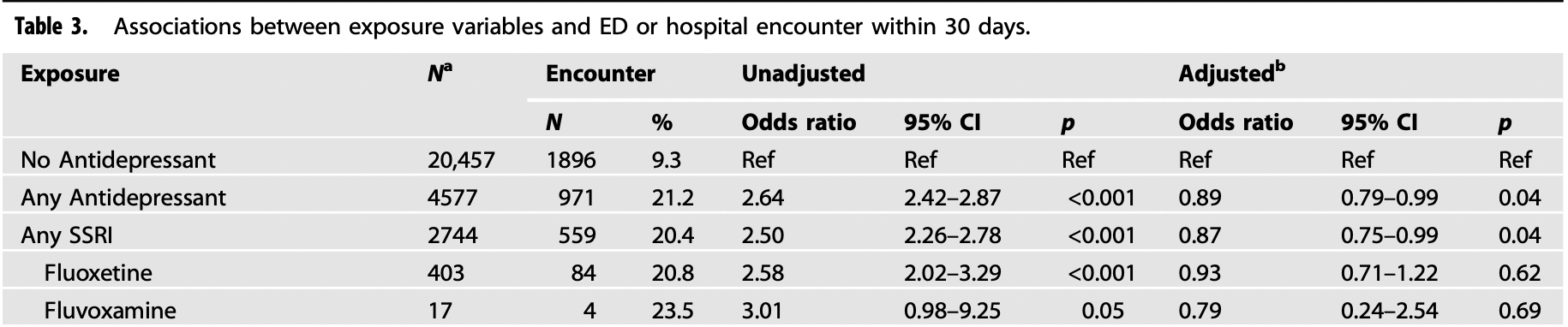
Retrospective 25,034 COVID+ outpatients showing significantly lower ER/hospitalization with antidepressants and FIASMA antidepressants, and a dose-dependent response.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of hospitalization/ER, 19.4% lower, RR 0.81, p = 0.69, treatment 4 of 17 (23.5%), control 1,896 of 20,457 (9.3%), adjusted per study, odds ratio converted to relative risk, fluvoxamine, multivariable.
|
|
risk of hospitalization/ER, 11.9% lower, RR 0.88, p = 0.03, treatment 707 of 3,414 (20.7%), control 1,896 of 20,457 (9.3%), adjusted per study, odds ratio converted to relative risk, FIASMA, multivariable.
|
|
risk of hospitalization/ER, 11.9% lower, RR 0.88, p = 0.04, treatment 559 of 2,744 (20.4%), control 1,896 of 20,457 (9.3%), adjusted per study, odds ratio converted to relative risk, SSRI, multivariable.
|
|
risk of hospitalization/ER, 10.1% lower, RR 0.90, p = 0.04, treatment 971 of 4,577 (21.2%), control 1,896 of 20,457 (9.3%), adjusted per study, odds ratio converted to relative risk, all antidepressants, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Fritz et al., 22 Aug 2022, retrospective, USA, peer-reviewed, 5 authors, study period 1 March, 2020 - 16 May, 2021.
Contact: bafritz@wustl.edu.
Association between antidepressant use and ED or hospital visits in outpatients with SARS-CoV-2
Translational Psychiatry, doi:10.1038/s41398-022-02109-3
Antidepressants have previously been associated with better outcomes in patients hospitalized with COVID-19, but their effect on clinical deterioration among ambulatory patients has not been fully explored. The objective of this study was to assess whether antidepressant exposure was associated with reduced emergency department (ED) or hospital visits among ambulatory patients with SARS-CoV-2 infection. This retrospective cohort study included adult patients (N = 25 034) with a positive SARS-CoV-2 test performed in a non-hospital setting. Logistic regression analyses tested associations between home use of antidepressant medications and a composite outcome of ED visitation or hospital admission within 30 days. Secondary exposures included individual antidepressants and antidepressants with functional inhibition of acid sphingomyelinase (FIASMA) activity. Patients with antidepressant exposure were less likely to experience the primary composite outcome compared to patients without antidepressant exposure (adjusted odds ratio [aOR] 0.89, 95% CI 0.79-0.99, p = 0.04). This association was only observed with daily doses of at least 20 mg fluoxetine-equivalent (aOR 0.87, 95% CI 0.77-0.99, p = 0.04), but not with daily doses lower than 20 mg fluoxetine-equivalent (aOR 0.94, 95% CI 0.80-1.11, p = 0.48). In exploratory secondary analyses, the outcome incidence was also reduced with exposure to selective serotonin reuptake inhibitors (aOR 0.87, 95% CI 0.75-0.99, p = 0.04), bupropion (aOR 0.70, 95% CI 0.55-0.90, p = 0.005), and FIASMA antidepressant drugs (aOR 0.87, 95% CI 0.77-0.99, p = 0.03). Antidepressant exposure was associated with a reduced incidence of emergency department visitation or hospital admission among SARS-CoV-2 positive patients, in a dose-dependent manner. These data support the FIASMA model of antidepressants' effects against COVID-19.
AUTHOR CONTRIBUTIONS Dr. Fritz had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: Fritz, Lenze, Reiersen. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: Fritz. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: Fritz. Administrative, technical, or material support: Lenze, Reiersen.
COMPETING INTERESTS
ADDITIONAL INFORMATION Supplementary information The online version contains supplementary material available at https://doi.org/10.1038/s41398-022-02109-3. Correspondence and requests for materials should be addressed to Bradley A. Fritz. Reprints and permission information is available at http://www.nature.com/ reprints Publisher's note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Althaus, Marini, Zlamal, Pelzl, Singh et al., Antibodyinduced procoagulant platelets in severe COVID-19 infection, Blood
Bayat, Ryono, Phelps, Geis, Sedghi et al., Reduced mortality with ondansetron use in SARS-CoV-2-infected inpatients, Open Forum Infect Dis
Brody, Gu, Antidepressant Use Among Adults: United States
Carpinteiro, Edwards, Hoffmann, Kochs, Gripp et al., Pharmacological inhibition of acid sphingomyelinase prevents uptake of SARS-CoV-2 by epithelial cells, Cell Rep. Med
Carpinteiro, Gripp, Hoffmann, Pöhlmann, Hoertel et al., Inhibition of acid sphingomyelinase by ambroxol prevents SARS-CoV-2 entry into epithelial cells, J Biol Chem
Clelland, Ramiah, Steinberg, Clelland, Analysis of the impact of antidepressants and other medications on COVID-19 infection risk in a chronic psychiatric in-patient cohort, BJPsych Open
Cloutier, Allaeys, Marcoux, Machlus, Mailhot et al., Platelets release pathogenic serotonin and return to circulation after immune complexmediated sequestration, Proc Natl Acad Sci
Dechaumes, Nekoua, Belouzard, Sane, Engelmann et al., Fluoxetine Can Inhibit SARS-CoV-2 in vitro, Microorganisms
Dhir, Kulkarni, Possible involvement of sigma-1 receptors in the antiimmobility action of bupropion, a dopamine reuptake inhibitor, Fundam Clin Pharm
Ettman, Abdalla, Cohen, Sampson, Vivier et al., Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic, JAMA Netw Open
Facente, Reiersen, Lenze, Boulware, Klausner, Fluvoxamine for the early treatment of SARS-CoV-2 infection: a review of current evidence, Drugs
Hashimoto, Repurposing of CNS drugs to treat COVID-19 infection: targeting the sigma-1 receptor, Eur Arch Psychiatry Clin Neurosci
Hashimoto, Suzuki, Hashimoto, Mechanisms of action of fluvoxamine for COVID-19: a historical review, Mol Psychiatry
Hayasaka, Purgato, Magni, Ogawa, Takeshima et al., Dose equivalents of antidepressants: evidence-based recommendations from randomized controlled trials, J Affect Disord
Hergovich, Aigner, Eichler, Entlicher, Drucker et al., Paroxetine decreases platelet serotonin storage and platelet function in human beings, Clin Pharm Ther
Herr, Bode, Duerschmied, The effects of serotonin in immune cells, Front Cardiovasc Med
Hoehn, Jernigan, Japtok, Chang, Midura et al., Acid Sphingomyelinase Inhibition in Stored Erythrocytes Reduces Transfusion-Associated Lung Inflammation, Ann Surg
Hoertel, Blachier, Blanco, Olfson, Massetti et al., A stochastic agent-based model of the SARS-CoV-2 epidemic in France, Nat Med
Hoertel, Do the selective serotonin reuptake inhibitor antidepressants fluoxetine and fluvoxamine reduce mortality among patients with COVID-19?, JAMA Netw Open
Hoertel, Sánchez-Rico, Gulbins, Kornhuber, Carpinteiro et al., Association between FIASMA psychotropic medications and reduced risk of intubation or death in individuals with psychiatric disorders hospitalized for severe COVID-19: an observational multicenter study, Transl Psychiatry
Hoertel, Sánchez-Rico, Gulbins, Kornhuber, Carpinteiro et al., Association between FIASMAs and reduced risk of intubation or death in individuals hospitalized for severe COVID-19: an observational multicenter study, Clin Pharm Ther
Hoertel, Sánchez-Rico, Gulbins, Kornhuber, Vernet et al., Association between benzodiazepine receptor agonist use and mortality in patients hospitalized for COVID-19: a multicenter observational study, Epidemiol Psychiatric Sci
Hoertel, Sánchez-Rico, Herrera-Morueco, De La Muela, Gulbins et al., Comorbid medical conditions are a key factor to understand the relationship between psychiatric disorders and COVID-19-related mortality: results from 49,089 COVID-19 inpatients, Mol. Psychiatry
Hoertel, Sánchez-Rico, Muela, Abellán, Blanco et al., Risk of death in individuals hospitalized for COVID-19 with and without psychiatric disorders: an observational multicenter study in France, Biol. Psychiatry Glob Open Sci, doi:10.1016/j.bpsgos.2021.12.007
Hoertel, Sánchez-Rico, Vernet, Beeker, Jannot et al., Association between antidepressant use and reduced risk of intubation or death in hospitalized patients with COVID-19: results from an observational study, Mol Psychiatry
Hoertel, Sánchez-Rico, Vernet, Beeker, Neuraz et al., Dexamethasone use and mortality in hospitalized patients with coronavirus disease 2019: A multicentre retrospective observational study, Br J Clin Pharm
Hoertel, Sánchez-Rico, Vernet, Jannot, Neuraz et al., Observational Study of Chlorpromazine in Hospitalized Patients with COVID-19, Clin Drug Investig
Hoertel, Sánchez-Rico, Vernet, Jannot, Neuraz et al., Observational study of haloperidol in hospitalized patients with COVID-19, PLoS ONE
Horby, Lim, Emberson, Mafham, Bell et al., Dexamethasone in hospitalized patients with Covid-19, N. Engl J Med
Ishima, Fujita, Hashimoto, Interaction of new antidepressants with sigma-1 receptor chaperones and their potentiation of neurite outgrowth in PC12 cells, Eur J Pharm
Kast, Anti-and pro-inflammatory considerations in antidepressant use during medical illness: bupropion lowers and mirtazapine increases circulating tumor necrosis factor-alpha levels, Gen Hosp Psychiatry
Khodadoust, Inferring a causal relationship between ceramide levels and COVID-19 respiratory distress, Sci Rep
Kopczyńska, Szereda-Przestaszewska, 5HT2 and 5HT3 receptors' contribution to modeling of post-serotonin respiratory pattern in cats, Life Sci
Kornhuber, Hoertel, Gulbins, The acid sphingomyelinase/ceramide system in COVID-19, Mol Psychiatry
Kornhuber, Muehlbacher, Trapp, Pechmann, Friedl et al., Identification of novel functional inhibitors of acid sphingomyelinase, PLoS ONE
Kornhuber, Tripal, Reichel, Terfloth, Bleich et al., Identification of new functional inhibitors of acid sphingomyelinase using a structure-propertyactivity relation model, J Med Chem
Köhler, Freitas, Stubbs, Maes, Solmi et al., Peripheral alterations in cytokine and chemokine levels after antidepressant drug treatment for major depressive disorder: systematic review and meta-analysis, Mol Neurobiol
Lenze, Mattar, Zorumski, Stevens, Schweiger et al., Fluvoxamine vs placebo and clinical deterioration in outpatients with symptomatic COVID-19: a randomized clinical trial, Jama
Luber, Meyers, Williams-Russo, Hollenberg, Didomenico et al., Depression and service utilization in elderly primary care patients, Am J Geriatr Psychiatry
Macfadden, Brown, Buchan, Chung, Kozak et al., Screening large population health databases for potential coronavirus disease 2019 therapeutics: a pharmacopeia-wide association study of commonly prescribed medications, Open Forum Infect Dis
Marín-Corral, Rodríguez-Morató, Gomez-Gomez, Pascual-Guardia, Muñoz-Bermúdez et al., Metabolic signatures associated with severity in hospitalized COVID-19 patients, Int J Mol Sci
Mühle, Kremer, Vetter, Schmid, Achenbach et al., COVID-19 and its clinical severity are associated with alterations of plasma sphingolipids and enzyme activities of sphingomyelinase and ceramidase, medRxiv, doi:10.1101/2022.01.19.22269391
Nishikawa, Kanno, Zhou, Xiao, Suzuki et al., Massive imagebased single-cell profiling reveals high levels of circulating platelet aggregates in patients with COVID-19, Nat Commun
Oskotsky, Maric, Tang, Oskotsky, Wong et al., Mortality risk among patients with COVID-19 prescribed selective serotonin reuptake inhibitor antidepressants, JAMA Netw Open
Pandhare, Pappu, Wilms, Blanton, Jansen, The antidepressant bupropion is a negative allosteric modulator of serotonin type 3A receptors, Neuropharmacology
Rabeea, Merchant, Khan, Kow, Hasan, Surging trends in prescriptions and costs of antidepressants in England amid COVID-19, Daru
Reis, Santos Moreira-Silva, Silva, Thabane, Milagres et al., Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with COVID-19: the TOGETHER randomised, platform clinical trial, Lancet Glob Health
Rico, Cougoule, Gulbins, Kornhuber, Carpinteiro, Repurposing antidepressants inhibiting the sphingomyelinase acid/ceramide system against COVID-19: current evidence and potential mechanisms, Mol Psychiatry
Ritchie, Matieu, Rodés-Guirao, Appel, Giattino et al., Coronavirus pandemic (COVID-19) vaccinations
Roweth, Yan, Bedwani, Chauhan, Fowler et al., Citalopram inhibits platelet function independently of SERT-mediated 5-HT transport, Sci Rep
Sawada, Uchida, Suzuki, Watanabe, Kikuchi et al., Persistence and compliance to antidepressant treatment in patients with depression: a chart review, BMC Psychiatry
Schloer, Brunotte, Goretzko, Mecate-Zambrano, Korthals et al., Targeting the endolysosomal host-SARS-CoV-2 interface by clinically licensed functional inhibitors of acid sphingomyelinase (FIASMA) including the antidepressant fluoxetine, Emerg Microbes Infect
Schloer, Brunotte, Mecate-Zambrano, Zheng, Tang et al., Drug synergy of combinatory treatment with remdesivir and the repurposed drugs fluoxetine and itraconazole effectively impairs SARS-CoV-2 infection in vitro, Br J Pharm
Seftel, Boulware, Prospective cohort of fluvoxamine for early treatment of Coronavirus Disease 19, Open Forum Infect Dis
Singh, Parida, Lingaraju, Kesavan, Kumar et al., Drug repurposing approach to fight COVID-19, Pharm Rep
Sukhatme, Reiersen, Vayttaden, Sukhatme, Fluvoxamine: a review of its mechanism of action and its role in COVID-19, Front Pharm
Torretta, Garziano, Poliseno, Capitanio, Biasin et al., Severity of COVID-19 Patients Predicted by Serum Sphingolipids Signature, Int J Mol Sci
Vai, Mazza, Colli, Foiselle, Allen et al., Mental disorders and risk of COVID-19-related mortality, hospitalisation, and intensive care unit admission: a systematic review and meta-analysis, Lancet Psychiatry
Van Walraven, Austin, Jennings, Quan, Forster, A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data, Med Care
Venkatesan, Repurposing drugs for treatment of COVID-19, Lancet Respir Med
Von Elm, Altman, Egger, Pocock, Gøtzsche et al., The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies, Lancet
Zaid, Guessous, Puhm, Elhamdani, Chentoufi et al., Platelet reactivity to thrombin differs between patients with COVID-19 and those with ARDS unrelated to COVID-19, Blood Adv
Zimniak, Kirschner, Hilpert, Geiger, Danov et al., The serotonin reuptake inhibitor Fluoxetine inhibits SARS-CoV-2 in human lung tissue, Sci Rep
DOI record:
{
"DOI": "10.1038/s41398-022-02109-3",
"ISSN": [
"2158-3188"
],
"URL": "http://dx.doi.org/10.1038/s41398-022-02109-3",
"abstract": "<jats:title>Abstract</jats:title><jats:p>Antidepressants have previously been associated with better outcomes in patients hospitalized with COVID-19, but their effect on clinical deterioration among ambulatory patients has not been fully explored. The objective of this study was to assess whether antidepressant exposure was associated with reduced emergency department (ED) or hospital visits among ambulatory patients with SARS-CoV-2 infection. This retrospective cohort study included adult patients (<jats:italic>N</jats:italic> = 25 034) with a positive SARS-CoV-2 test performed in a non-hospital setting. Logistic regression analyses tested associations between home use of antidepressant medications and a composite outcome of ED visitation or hospital admission within 30 days. Secondary exposures included individual antidepressants and antidepressants with functional inhibition of acid sphingomyelinase (FIASMA) activity. Patients with antidepressant exposure were less likely to experience the primary composite outcome compared to patients without antidepressant exposure (adjusted odds ratio [aOR] 0.89, 95% CI 0.79–0.99, <jats:italic>p</jats:italic> = 0.04). This association was only observed with daily doses of at least 20 mg fluoxetine-equivalent (aOR 0.87, 95% CI 0.77–0.99, <jats:italic>p</jats:italic> = 0.04), but not with daily doses lower than 20 mg fluoxetine-equivalent (aOR 0.94, 95% CI 0.80–1.11, <jats:italic>p</jats:italic> = 0.48). In exploratory secondary analyses, the outcome incidence was also reduced with exposure to selective serotonin reuptake inhibitors (aOR 0.87, 95% CI 0.75–0.99, <jats:italic>p</jats:italic> = 0.04), bupropion (aOR 0.70, 95% CI 0.55–0.90, <jats:italic>p</jats:italic> = 0.005), and FIASMA antidepressant drugs (aOR 0.87, 95% CI 0.77–0.99, <jats:italic>p</jats:italic> = 0.03). Antidepressant exposure was associated with a reduced incidence of emergency department visitation or hospital admission among SARS-CoV-2 positive patients, in a dose-dependent manner. These data support the FIASMA model of antidepressants’ effects against COVID-19.</jats:p>",
"alternative-id": [
"2109"
],
"article-number": "341",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "24 March 2022"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Revised",
"name": "revised",
"order": 2,
"value": "8 August 2022"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 3,
"value": "9 August 2022"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 4,
"value": "22 August 2022"
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1,
"value": "N.H. reported being listed as an inventor on a patent application related to methods of treating COVID-19, filled by Assistance Publique-Hôpitaux de Paris, and he has received consulting fees and nonfinancial support from Lundbeck outside this study. E.J.L. and A.M.R. are co-inventors on a patent application related to methods of treating COVID-19, filed by Washington University in St. Louis. E.J.L. has grant support from Meractus Ventures-Fast Grants (COVID-19 treatment research) and PCORI, and he has done consulting for Boehringer-Ingelheim and Prodeo. No other disclosures were reported."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-7239-8877",
"affiliation": [],
"authenticated-orcid": false,
"family": "Fritz",
"given": "Bradley A.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Hoertel",
"given": "Nicolas",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lenze",
"given": "Eric J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jalali",
"given": "Farid",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3203-4590",
"affiliation": [],
"authenticated-orcid": false,
"family": "Reiersen",
"given": "Angela M.",
"sequence": "additional"
}
],
"container-title": "Translational Psychiatry",
"container-title-short": "Transl Psychiatry",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2022,
8,
22
]
],
"date-time": "2022-08-22T14:04:27Z",
"timestamp": 1661177067000
},
"deposited": {
"date-parts": [
[
2022,
8,
22
]
],
"date-time": "2022-08-22T15:06:09Z",
"timestamp": 1661180769000
},
"funder": [
{
"DOI": "10.13039/100005831",
"award": [
"MRTG08152020FRITZ"
],
"doi-asserted-by": "publisher",
"name": "Foundation for Anesthesia Education and Research"
},
{
"DOI": "10.13039/100006108",
"award": [
"UL1TR002345",
"UL1TR002345"
],
"doi-asserted-by": "publisher",
"name": "U.S. Department of Health & Human Services | NIH | National Center for Advancing Translational Sciences"
},
{
"name": "U.S. Department of Health & Human Services | NIH | National Center for Advancing Translational Sciences"
}
],
"indexed": {
"date-parts": [
[
2022,
8,
22
]
],
"date-time": "2022-08-22T15:43:28Z",
"timestamp": 1661183008128
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2022,
8,
22
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2022,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
8,
22
]
],
"date-time": "2022-08-22T00:00:00Z",
"timestamp": 1661126400000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
8,
22
]
],
"date-time": "2022-08-22T00:00:00Z",
"timestamp": 1661126400000
}
}
],
"link": [
{
"URL": "https://www.nature.com/articles/s41398-022-02109-3.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41398-022-02109-3",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41398-022-02109-3.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1038",
"published": {
"date-parts": [
[
2022,
8,
22
]
]
},
"published-online": {
"date-parts": [
[
2022,
8,
22
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1038/s41591-020-1001-6",
"author": "N Hoertel",
"doi-asserted-by": "publisher",
"first-page": "1417",
"journal-title": "Nat Med",
"key": "2109_CR1",
"unstructured": "Hoertel N, Blachier M, Blanco C, Olfson M, Massetti M, Rico MS, et al. A stochastic agent-based model of the SARS-CoV-2 epidemic in France. Nat Med. 2020;26:1417–21.",
"volume": "26",
"year": "2020"
},
{
"key": "2109_CR2",
"unstructured": "Ritchie H, Matieu E, Rodés-Guirao L, Appel C, Giattino C, Ortiz-Ospina E, et al. Coronavirus pandemic (COVID-19) vaccinations. 2020; OurWorldInData.org."
},
{
"key": "2109_CR3",
"unstructured": "Centers for Disease Control and Prevention. The possibility of COVID-19 after vaccination: breakthrough infection. 2021."
},
{
"DOI": "10.1007/s43440-020-00155-6",
"author": "TU Singh",
"doi-asserted-by": "publisher",
"first-page": "1479",
"journal-title": "Pharm Rep.",
"key": "2109_CR4",
"unstructured": "Singh TU, Parida S, Lingaraju MC, Kesavan M, Kumar D, Singh RK. Drug repurposing approach to fight COVID-19. Pharm Rep. 2020;72:1479–508.",
"volume": "72",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(21)00270-8",
"author": "P Venkatesan",
"doi-asserted-by": "publisher",
"first-page": "e63",
"journal-title": "Lancet Respir Med",
"key": "2109_CR5",
"unstructured": "Venkatesan P. Repurposing drugs for treatment of COVID-19. Lancet Respir Med. 2021;9:e63.",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.36510",
"author": "N Hoertel",
"doi-asserted-by": "publisher",
"first-page": "e2136510",
"journal-title": "JAMA Netw Open",
"key": "2109_CR6",
"unstructured": "Hoertel N. Do the selective serotonin reuptake inhibitor antidepressants fluoxetine and fluvoxamine reduce mortality among patients with COVID-19? JAMA Netw Open. 2021;4:e2136510.",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1038/s41380-020-01012-x",
"author": "N Hoertel",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Mol Psychiatry",
"key": "2109_CR7",
"unstructured": "Hoertel N, Sánchez-Rico M, Cougoule C, Gulbins E, Kornhuber J, Carpinteiro A, et al. Repurposing antidepressants inhibiting the sphingomyelinase acid/ceramide system against COVID-19: current evidence and potential mechanisms. Mol Psychiatry. 2021;26:1–2.",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.1038/s41598-021-85049-0",
"author": "M Zimniak",
"doi-asserted-by": "publisher",
"journal-title": "Sci Rep.",
"key": "2109_CR8",
"unstructured": "Zimniak M, Kirschner L, Hilpert H, Geiger N, Danov O, Oberwinkler H, et al. The serotonin reuptake inhibitor Fluoxetine inhibits SARS-CoV-2 in human lung tissue. Sci Rep. 2021;11:5890.",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1111/bph.15418",
"author": "S Schloer",
"doi-asserted-by": "publisher",
"first-page": "2339",
"journal-title": "Br J Pharm",
"key": "2109_CR9",
"unstructured": "Schloer S, Brunotte L, Mecate-Zambrano A, Zheng S, Tang J, Ludwig S, et al. Drug synergy of combinatory treatment with remdesivir and the repurposed drugs fluoxetine and itraconazole effectively impairs SARS-CoV-2 infection in vitro. Br J Pharm. 2021;178:2339–50.",
"volume": "178",
"year": "2021"
},
{
"DOI": "10.1016/j.xcrm.2020.100142",
"author": "A Carpinteiro",
"doi-asserted-by": "publisher",
"first-page": "100142",
"journal-title": "Cell Rep. Med",
"key": "2109_CR10",
"unstructured": "Carpinteiro A, Edwards MJ, Hoffmann M, Kochs G, Gripp B, Weigang S, et al. Pharmacological inhibition of acid sphingomyelinase prevents uptake of SARS-CoV-2 by epithelial cells. Cell Rep. Med. 2020;1:100142.",
"volume": "1",
"year": "2020"
},
{
"DOI": "10.3390/microorganisms9020339",
"author": "A Dechaumes",
"doi-asserted-by": "publisher",
"first-page": "339.",
"journal-title": "Microorganisms",
"key": "2109_CR11",
"unstructured": "Dechaumes A, Nekoua MP, Belouzard S, Sane F, Engelmann I, Dubuisson J, et al. Fluoxetine Can Inhibit SARS-CoV-2 in vitro. Microorganisms. 2021;9:339.",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1080/22221751.2020.1829082",
"author": "S Schloer",
"doi-asserted-by": "publisher",
"first-page": "2245",
"journal-title": "Emerg Microbes Infect",
"key": "2109_CR12",
"unstructured": "Schloer S, Brunotte L, Goretzko J, Mecate-Zambrano A, Korthals N, Gerke V, et al. Targeting the endolysosomal host-SARS-CoV-2 interface by clinically licensed functional inhibitors of acid sphingomyelinase (FIASMA) including the antidepressant fluoxetine. Emerg Microbes Infect. 2020;9:2245–55.",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.3389/fphar.2021.652688",
"author": "VP Sukhatme",
"doi-asserted-by": "publisher",
"first-page": "652688",
"journal-title": "Front Pharm",
"key": "2109_CR13",
"unstructured": "Sukhatme VP, Reiersen AM, Vayttaden SJ, Sukhatme VV. Fluvoxamine: a review of its mechanism of action and its role in COVID-19. Front Pharm. 2021;12:652688.",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1038/s41380-021-01432-3",
"author": "Y Hashimoto",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Mol Psychiatry",
"key": "2109_CR14",
"unstructured": "Hashimoto Y, Suzuki T, Hashimoto K. Mechanisms of action of fluvoxamine for COVID-19: a historical review. Mol Psychiatry. 2022;27:1–10.",
"volume": "27",
"year": "2022"
},
{
"DOI": "10.1007/s40265-021-01636-5",
"author": "SN Facente",
"doi-asserted-by": "publisher",
"first-page": "2081",
"journal-title": "Drugs",
"key": "2109_CR15",
"unstructured": "Facente SN, Reiersen AM, Lenze EJ, Boulware DR, Klausner JD. Fluvoxamine for the early treatment of SARS-CoV-2 infection: a review of current evidence. Drugs 2021;81:2081–9.",
"volume": "81",
"year": "2021"
},
{
"author": "J Kornhuber",
"first-page": "1",
"journal-title": "Mol Psychiatry",
"key": "2109_CR16",
"unstructured": "Kornhuber J, Hoertel N, Gulbins E. The acid sphingomyelinase/ceramide system in COVID-19. Mol Psychiatry. 2021;27:1–8.",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1097/SLA.0000000000001648",
"author": "RS Hoehn",
"doi-asserted-by": "publisher",
"first-page": "218",
"journal-title": "Ann Surg",
"key": "2109_CR17",
"unstructured": "Hoehn RS, Jernigan PL, Japtok L, Chang AL, Midura EF, Caldwell CC, et al. Acid Sphingomyelinase Inhibition in Stored Erythrocytes Reduces Transfusion-Associated Lung Inflammation. Ann Surg. 2017;265:218–26.",
"volume": "265",
"year": "2017"
},
{
"DOI": "10.1016/j.jbc.2021.100701",
"author": "A Carpinteiro",
"doi-asserted-by": "publisher",
"first-page": "100701",
"journal-title": "J Biol Chem",
"key": "2109_CR18",
"unstructured": "Carpinteiro A, Gripp B, Hoffmann M, Pöhlmann S, Hoertel N, Edwards MJ, et al. Inhibition of acid sphingomyelinase by ambroxol prevents SARS-CoV-2 entry into epithelial cells. J Biol Chem. 2021;296:100701.",
"volume": "296",
"year": "2021"
},
{
"DOI": "10.1038/s41380-021-01021-4",
"author": "N Hoertel",
"doi-asserted-by": "publisher",
"first-page": "5199",
"journal-title": "Mol Psychiatry",
"key": "2109_CR19",
"unstructured": "Hoertel N, Sánchez-Rico M, Vernet R, Beeker N, Jannot AS, Neuraz A, et al. Association between antidepressant use and reduced risk of intubation or death in hospitalized patients with COVID-19: results from an observational study. Mol Psychiatry. 2021;26:5199–212.",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.33090",
"author": "T Oskotsky",
"doi-asserted-by": "publisher",
"first-page": "e2133090",
"journal-title": "JAMA Netw Open",
"key": "2109_CR20",
"unstructured": "Oskotsky T, Maric I, Tang A, Oskotsky B, Wong RJ, Aghaeepour N, et al. Mortality risk among patients with COVID-19 prescribed selective serotonin reuptake inhibitor antidepressants. JAMA Netw Open. 2021;4:e2133090.",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1038/s41398-022-01804-5",
"author": "N Hoertel",
"doi-asserted-by": "publisher",
"journal-title": "Transl Psychiatry",
"key": "2109_CR21",
"unstructured": "Hoertel N, Sánchez-Rico M, Gulbins E, Kornhuber J, Carpinteiro A, Abellán M, et al. Association between FIASMA psychotropic medications and reduced risk of intubation or death in individuals with psychiatric disorders hospitalized for severe COVID-19: an observational multicenter study. Transl Psychiatry. 2022;12:90.",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1001/jama.2020.22760",
"author": "EJ Lenze",
"doi-asserted-by": "publisher",
"first-page": "2292",
"journal-title": "Jama",
"key": "2109_CR22",
"unstructured": "Lenze EJ, Mattar C, Zorumski CF, Stevens A, Schweiger J, Nicol GE, et al. Fluvoxamine vs placebo and clinical deterioration in outpatients with symptomatic COVID-19: a randomized clinical trial. Jama 2020;324:2292–2300.",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1016/S2214-109X(21)00448-4",
"author": "G Reis",
"doi-asserted-by": "publisher",
"first-page": "e42",
"journal-title": "Lancet Glob Health",
"key": "2109_CR23",
"unstructured": "Reis G, Dos Santos Moreira-Silva EA, Silva DCM, Thabane L, Milagres AC, Ferreira TS, et al. Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with COVID-19: the TOGETHER randomised, platform clinical trial. Lancet Glob Health. 2021;10:e42–e51.",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1093/ofid/ofab050",
"author": "D Seftel",
"doi-asserted-by": "publisher",
"first-page": "ofab050",
"journal-title": "Open Forum Infect Dis",
"key": "2109_CR24",
"unstructured": "Seftel D, Boulware DR. Prospective cohort of fluvoxamine for early treatment of Coronavirus Disease 19. Open Forum Infect Dis. 2021;8:ofab050.",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(07)61602-X",
"author": "E von Elm",
"doi-asserted-by": "publisher",
"first-page": "1453",
"journal-title": "Lancet",
"key": "2109_CR25",
"unstructured": "von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007;370:1453–7.",
"volume": "370",
"year": "2007"
},
{
"DOI": "10.1016/j.ejphar.2014.01.064",
"author": "T Ishima",
"doi-asserted-by": "publisher",
"first-page": "167",
"journal-title": "Eur J Pharm",
"key": "2109_CR26",
"unstructured": "Ishima T, Fujita Y, Hashimoto K. Interaction of new antidepressants with sigma-1 receptor chaperones and their potentiation of neurite outgrowth in PC12 cells. Eur J Pharm. 2014;727:167–73.",
"volume": "727",
"year": "2014"
},
{
"DOI": "10.1371/journal.pone.0023852",
"author": "J Kornhuber",
"doi-asserted-by": "publisher",
"first-page": "e23852",
"journal-title": "PLoS ONE",
"key": "2109_CR27",
"unstructured": "Kornhuber J, Muehlbacher M, Trapp S, Pechmann S, Friedl A, Reichel M, et al. Identification of novel functional inhibitors of acid sphingomyelinase. PLoS ONE. 2011;6:e23852.",
"volume": "6",
"year": "2011"
},
{
"DOI": "10.1016/j.jad.2015.03.021",
"author": "Y Hayasaka",
"doi-asserted-by": "publisher",
"first-page": "179",
"journal-title": "J Affect Disord",
"key": "2109_CR28",
"unstructured": "Hayasaka Y, Purgato M, Magni LR, Ogawa Y, Takeshima N, Cipriani A, et al. Dose equivalents of antidepressants: evidence-based recommendations from randomized controlled trials. J Affect Disord. 2015;180:179–84.",
"volume": "180",
"year": "2015"
},
{
"DOI": "10.1016/j.bpsgos.2021.12.007",
"doi-asserted-by": "publisher",
"key": "2109_CR29",
"unstructured": "Hoertel N, Sánchez-Rico M, Muela P, Abellán M, Blanco C, Leboyer M, et al. Risk of death in individuals hospitalized for COVID-19 with and without psychiatric disorders: an observational multicenter study in France. Biol. Psychiatry Glob Open Sci. 2022. https://doi.org/10.1016/j.bpsgos.2021.12.007. online ahead of print."
},
{
"DOI": "10.1371/journal.pone.0247122",
"author": "N Hoertel",
"doi-asserted-by": "publisher",
"first-page": "e0247122",
"journal-title": "PLoS ONE",
"key": "2109_CR30",
"unstructured": "Hoertel N, Sánchez-Rico M, Vernet R, Jannot AS, Neuraz A, Blanco C, et al. Observational study of haloperidol in hospitalized patients with COVID-19. PLoS ONE. 2021;16:e0247122.",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1007/s40261-021-01001-0",
"author": "N Hoertel",
"doi-asserted-by": "publisher",
"first-page": "221",
"journal-title": "Clin Drug Investig",
"key": "2109_CR31",
"unstructured": "Hoertel N, Sánchez-Rico M, Vernet R, Jannot AS, Neuraz A, Blanco C, et al. Observational Study of Chlorpromazine in Hospitalized Patients with COVID-19. Clin Drug Investig. 2021;41:221–33.",
"volume": "41",
"year": "2021"
},
{
"DOI": "10.1038/s41380-021-01393-7",
"doi-asserted-by": "crossref",
"key": "2109_CR32",
"unstructured": "Hoertel N, Sánchez-Rico M, Herrera-Morueco JJ, de la Muela P, Gulbins E, Kornhuber J, et al. Comorbid medical conditions are a key factor to understand the relationship between psychiatric disorders and COVID-19-related mortality: results from 49,089 COVID-19 inpatients. Mol. Psychiatry. 2021:1–3."
},
{
"DOI": "10.1017/S2045796021000743",
"author": "N Hoertel",
"doi-asserted-by": "publisher",
"first-page": "e18.",
"journal-title": "Epidemiol Psychiatric Sci",
"key": "2109_CR33",
"unstructured": "Hoertel N, Sánchez-Rico M, Gulbins E, Kornhuber J, Vernet R, Beeker N, et al. Association between benzodiazepine receptor agonist use and mortality in patients hospitalized for COVID-19: a multicenter observational study. Epidemiol Psychiatric Sci. 2022;31:e18.",
"volume": "31",
"year": "2022"
},
{
"DOI": "10.1097/MLR.0b013e31819432e5",
"author": "C van Walraven",
"doi-asserted-by": "publisher",
"first-page": "626",
"journal-title": "Med Care",
"key": "2109_CR34",
"unstructured": "van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47:626–33.",
"volume": "47",
"year": "2009"
},
{
"DOI": "10.1002/cpt.2317",
"author": "N Hoertel",
"doi-asserted-by": "publisher",
"first-page": "1498",
"journal-title": "Clin Pharm Ther",
"key": "2109_CR35",
"unstructured": "Hoertel N, Sánchez-Rico M, Gulbins E, Kornhuber J, Carpinteiro A, Lenze EJ, et al. Association between FIASMAs and reduced risk of intubation or death in individuals hospitalized for severe COVID-19: an observational multicenter study. Clin Pharm Ther. 2021;110:1498–511.",
"volume": "110",
"year": "2021"
},
{
"DOI": "10.1007/s00406-020-01231-x",
"author": "K Hashimoto",
"doi-asserted-by": "publisher",
"first-page": "249",
"journal-title": "Eur Arch Psychiatry Clin Neurosci",
"key": "2109_CR36",
"unstructured": "Hashimoto K. Repurposing of CNS drugs to treat COVID-19 infection: targeting the sigma-1 receptor. Eur Arch Psychiatry Clin Neurosci. 2021;271:249–58.",
"volume": "271",
"year": "2021"
},
{
"DOI": "10.1016/S2215-0366(21)00232-7",
"author": "B Vai",
"doi-asserted-by": "publisher",
"first-page": "797",
"journal-title": "Lancet Psychiatry",
"key": "2109_CR37",
"unstructured": "Vai B, Mazza MG, Delli Colli C, Foiselle M, Allen B, Benedetti F, et al. Mental disorders and risk of COVID-19-related mortality, hospitalisation, and intensive care unit admission: a systematic review and meta-analysis. Lancet Psychiatry. 2021;8:797–812.",
"volume": "8",
"year": "2021"
},
{
"author": "CA Köhler",
"first-page": "4195",
"journal-title": "Mol Neurobiol",
"key": "2109_CR38",
"unstructured": "Köhler CA, Freitas TH, Stubbs B, Maes M, Solmi M, Veronese N, et al. Peripheral alterations in cytokine and chemokine levels after antidepressant drug treatment for major depressive disorder: systematic review and meta-analysis. Mol Neurobiol. 2018;55:4195–206.",
"volume": "55",
"year": "2018"
},
{
"DOI": "10.1021/jm070524a",
"author": "J Kornhuber",
"doi-asserted-by": "publisher",
"first-page": "219",
"journal-title": "J Med Chem",
"key": "2109_CR39",
"unstructured": "Kornhuber J, Tripal P, Reichel M, Terfloth L, Bleich S, Wiltfang J, et al. Identification of new functional inhibitors of acid sphingomyelinase using a structure-property-activity relation model. J Med Chem. 2008;51:219–37.",
"volume": "51",
"year": "2008"
},
{
"DOI": "10.1192/bjo.2021.1053",
"author": "CL Clelland",
"doi-asserted-by": "publisher",
"first-page": "e6",
"journal-title": "BJPsych Open",
"key": "2109_CR40",
"unstructured": "Clelland CL, Ramiah K, Steinberg L, Clelland JD. Analysis of the impact of antidepressants and other medications on COVID-19 infection risk in a chronic psychiatric in-patient cohort. BJPsych Open. 2021;8:e6.",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1093/ofid/ofac156",
"author": "DR MacFadden",
"doi-asserted-by": "publisher",
"first-page": "ofac156",
"journal-title": "Open Forum Infect Dis",
"key": "2109_CR41",
"unstructured": "MacFadden DR, Brown K, Buchan SA, Chung H, Kozak R, Kwong JC, et al. Screening large population health databases for potential coronavirus disease 2019 therapeutics: a pharmacopeia-wide association study of commonly prescribed medications. Open Forum Infect Dis. 2022;9:ofac156.",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.3390/ijms22094794",
"author": "J Marín-Corral",
"doi-asserted-by": "publisher",
"first-page": "4794",
"journal-title": "Int J Mol Sci",
"key": "2109_CR42",
"unstructured": "Marín-Corral J, Rodríguez-Morató J, Gomez-Gomez A, Pascual-Guardia S, Muñoz-Bermúdez R, Salazar-Degracia A, et al. Metabolic signatures associated with severity in hospitalized COVID-19 patients. Int J Mol Sci. 2021;22:4794.",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1038/s41598-021-00286-7",
"author": "MM Khodadoust",
"doi-asserted-by": "publisher",
"journal-title": "Sci Rep.",
"key": "2109_CR43",
"unstructured": "Khodadoust MM. Inferring a causal relationship between ceramide levels and COVID-19 respiratory distress. Sci Rep. 2021;11:20866.",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.3390/ijms221910198",
"author": "E Torretta",
"doi-asserted-by": "publisher",
"first-page": "10198.",
"journal-title": "Int J Mol Sci",
"key": "2109_CR44",
"unstructured": "Torretta E, Garziano M, Poliseno M, Capitanio D, Biasin M, Santantonio TA, et al. Severity of COVID-19 Patients Predicted by Serum Sphingolipids Signature. Int J Mol Sci. 2021;22:10198.",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1101/2022.01.19.22269391",
"doi-asserted-by": "publisher",
"key": "2109_CR45",
"unstructured": "Mühle C, Kremer A, Vetter M, Schmid J, Achenbach S, Schumacher F, et al. COVID-19 and its clinical severity are associated with alterations of plasma sphingolipids and enzyme activities of sphingomyelinase and ceramidase. medRxiv 2022. https://doi.org/10.1101/2022.01.19.22269391"
},
{
"DOI": "10.1038/s41598-018-21348-3",
"author": "HG Roweth",
"doi-asserted-by": "publisher",
"journal-title": "Sci Rep.",
"key": "2109_CR46",
"unstructured": "Roweth HG, Yan R, Bedwani NH, Chauhan A, Fowler N, Watson AH, et al. Citalopram inhibits platelet function independently of SERT-mediated 5-HT transport. Sci Rep. 2018;8:3494.",
"volume": "8",
"year": "2018"
},
{
"DOI": "10.3389/fcvm.2017.00048",
"author": "N Herr",
"doi-asserted-by": "publisher",
"first-page": "48",
"journal-title": "Front Cardiovasc Med",
"key": "2109_CR47",
"unstructured": "Herr N, Bode C, Duerschmied D. The effects of serotonin in immune cells. Front Cardiovasc Med. 2017;4:48.",
"volume": "4",
"year": "2017"
},
{
"DOI": "10.1067/mcp.2000.110456",
"author": "N Hergovich",
"doi-asserted-by": "publisher",
"first-page": "435",
"journal-title": "Clin Pharm Ther",
"key": "2109_CR48",
"unstructured": "Hergovich N, Aigner M, Eichler HG, Entlicher J, Drucker C, Jilma B. Paroxetine decreases platelet serotonin storage and platelet function in human beings. Clin Pharm Ther. 2000;68:435–42.",
"volume": "68",
"year": "2000"
},
{
"DOI": "10.1073/pnas.1720553115",
"author": "N Cloutier",
"doi-asserted-by": "publisher",
"first-page": "E1550",
"journal-title": "Proc Natl Acad Sci USA",
"key": "2109_CR49",
"unstructured": "Cloutier N, Allaeys I, Marcoux G, Machlus KR, Mailhot B, Zufferey A, et al. Platelets release pathogenic serotonin and return to circulation after immune complex-mediated sequestration. Proc Natl Acad Sci USA. 2018;115:E1550–9.",
"volume": "115",
"year": "2018"
},
{
"DOI": "10.1182/blood.2020008762",
"author": "K Althaus",
"doi-asserted-by": "publisher",
"first-page": "1061",
"journal-title": "Blood",
"key": "2109_CR50",
"unstructured": "Althaus K, Marini I, Zlamal J, Pelzl L, Singh A, Häberle H, et al. Antibody-induced procoagulant platelets in severe COVID-19 infection. Blood 2021;137:1061–71.",
"volume": "137",
"year": "2021"
},
{
"DOI": "10.1093/ofid/ofab336",
"author": "V Bayat",
"doi-asserted-by": "publisher",
"first-page": "ofab336",
"journal-title": "Open Forum Infect Dis",
"key": "2109_CR51",
"unstructured": "Bayat V, Ryono R, Phelps S, Geis E, Sedghi F, Etminani P, et al. Reduced mortality with ondansetron use in SARS-CoV-2-infected inpatients. Open Forum Infect Dis. 2021;8:ofab336.",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2021436",
"author": "P Horby",
"doi-asserted-by": "publisher",
"first-page": "693",
"journal-title": "N. Engl J Med",
"key": "2109_CR52",
"unstructured": "Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, et al. Dexamethasone in hospitalized patients with Covid-19. N. Engl J Med. 2021;384:693–704.",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1111/bcp.14784",
"author": "N Hoertel",
"doi-asserted-by": "publisher",
"first-page": "3766",
"journal-title": "Br J Clin Pharm",
"key": "2109_CR53",
"unstructured": "Hoertel N, Sánchez-Rico M, Vernet R, Beeker N, Neuraz A, Alvarado JM, et al. Dexamethasone use and mortality in hospitalized patients with coronavirus disease 2019: A multicentre retrospective observational study. Br J Clin Pharm. 2021;87:3766–75.",
"volume": "87",
"year": "2021"
},
{
"DOI": "10.1111/j.1472-8206.2008.00605.x",
"author": "A Dhir",
"doi-asserted-by": "publisher",
"first-page": "387",
"journal-title": "Fundam Clin Pharm",
"key": "2109_CR54",
"unstructured": "Dhir A, Kulkarni SK. Possible involvement of sigma-1 receptors in the anti-immobility action of bupropion, a dopamine reuptake inhibitor. Fundam Clin Pharm. 2008;22:387–94.",
"volume": "22",
"year": "2008"
},
{
"DOI": "10.1016/j.neuropharm.2016.09.021",
"author": "A Pandhare",
"doi-asserted-by": "publisher",
"first-page": "89",
"journal-title": "Neuropharmacology",
"key": "2109_CR55",
"unstructured": "Pandhare A, Pappu AS, Wilms H, Blanton MP, Jansen M. The antidepressant bupropion is a negative allosteric modulator of serotonin type 3A receptors. Neuropharmacology 2017;113:89–99.",
"volume": "113",
"year": "2017"
},
{
"DOI": "10.1016/j.lfs.2004.03.029",
"author": "B Kopczyńska",
"doi-asserted-by": "publisher",
"first-page": "2281",
"journal-title": "Life Sci",
"key": "2109_CR56",
"unstructured": "Kopczyńska B, Szereda-Przestaszewska M. 5HT2 and 5HT3 receptors’ contribution to modeling of post-serotonin respiratory pattern in cats. Life Sci. 2004;75:2281–90.",
"volume": "75",
"year": "2004"
},
{
"DOI": "10.1038/s41467-021-27378-2",
"author": "M Nishikawa",
"doi-asserted-by": "publisher",
"journal-title": "Nat Commun",
"key": "2109_CR57",
"unstructured": "Nishikawa M, Kanno H, Zhou Y, Xiao TH, Suzuki T, Ibayashi Y, et al. Massive image-based single-cell profiling reveals high levels of circulating platelet aggregates in patients with COVID-19. Nat Commun. 2021;12:7135.",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1182/bloodadvances.2020003513",
"author": "Y Zaid",
"doi-asserted-by": "publisher",
"first-page": "635",
"journal-title": "Blood Adv",
"key": "2109_CR58",
"unstructured": "Zaid Y, Guessous F, Puhm F, Elhamdani W, Chentoufi L, Morris AC, et al. Platelet reactivity to thrombin differs between patients with COVID-19 and those with ARDS unrelated to COVID-19. Blood Adv. 2021;5:635–9.",
"volume": "5",
"year": "2021"
},
{
"DOI": "10.1016/S0163-8343(03)00093-8",
"author": "RE Kast",
"doi-asserted-by": "publisher",
"first-page": "495",
"journal-title": "Gen Hosp Psychiatry",
"key": "2109_CR59",
"unstructured": "Kast RE. Anti- and pro-inflammatory considerations in antidepressant use during medical illness: bupropion lowers and mirtazapine increases circulating tumor necrosis factor-alpha levels. Gen Hosp Psychiatry. 2003;25:495–6.",
"volume": "25",
"year": "2003"
},
{
"key": "2109_CR60",
"unstructured": "Brody DJ, Gu Q. Antidepressant Use Among Adults: United States, 2015-2018. in NCHS Data Brief, no 377. Hyattsville, MD, National Center for Health Statistics; 2020."
},
{
"DOI": "10.1001/jamanetworkopen.2020.19686",
"author": "CK Ettman",
"doi-asserted-by": "publisher",
"first-page": "e2019686",
"journal-title": "JAMA Netw Open",
"key": "2109_CR61",
"unstructured": "Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. 2020;3:e2019686.",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1007/s40199-021-00390-z",
"author": "SA Rabeea",
"doi-asserted-by": "publisher",
"first-page": "217",
"journal-title": "Daru",
"key": "2109_CR62",
"unstructured": "Rabeea SA, Merchant HA, Khan MU, Kow CS, Hasan SS. Surging trends in prescriptions and costs of antidepressants in England amid COVID-19. Daru 2021;29:217–21.",
"volume": "29",
"year": "2021"
},
{
"DOI": "10.1097/00019442-200105000-00009",
"author": "MP Luber",
"doi-asserted-by": "publisher",
"first-page": "169",
"journal-title": "Am J Geriatr Psychiatry",
"key": "2109_CR63",
"unstructured": "Luber MP, Meyers BS, Williams-Russo PG, Hollenberg JP, DiDomenico TN, Charlson ME, et al. Depression and service utilization in elderly primary care patients. Am J Geriatr Psychiatry. 2001;9:169–76.",
"volume": "9",
"year": "2001"
},
{
"DOI": "10.1186/1471-244X-9-38",
"author": "N Sawada",
"doi-asserted-by": "publisher",
"journal-title": "BMC Psychiatry",
"key": "2109_CR64",
"unstructured": "Sawada N, Uchida H, Suzuki T, Watanabe K, Kikuchi T, Handa T, et al. Persistence and compliance to antidepressant treatment in patients with depression: a chart review. BMC Psychiatry. 2009;9:38.",
"volume": "9",
"year": "2009"
}
],
"reference-count": 64,
"references-count": 64,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.nature.com/articles/s41398-022-02109-3"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Biological Psychiatry",
"Cellular and Molecular Neuroscience",
"Psychiatry and Mental health"
],
"subtitle": [],
"title": "Association between antidepressant use and ED or hospital visits in outpatients with SARS-CoV-2",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "12"
}
