The Association between Lifestyle Factors and COVID-19: Findings from Qatar Biobank
et al., Nutrients, doi:10.3390/nu16071037, Nov 2023
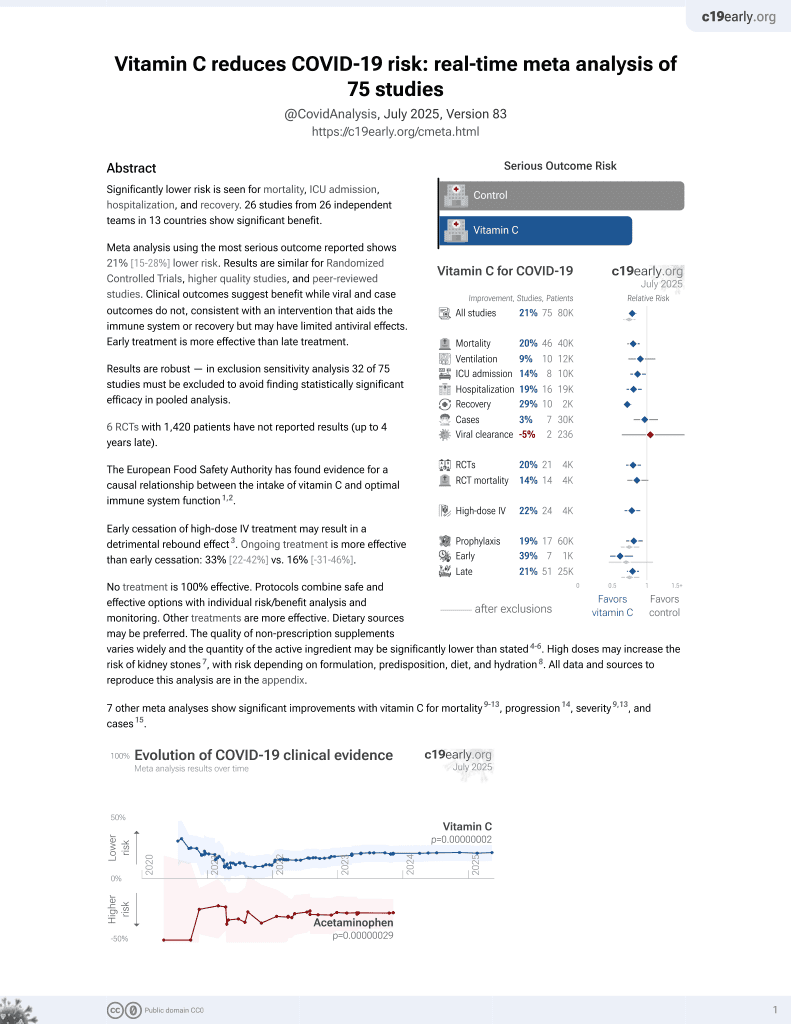
Vitamin C for COVID-19
6th treatment shown to reduce risk in
September 2020, now with p = 0.000000068 from 74 studies, recognized in 22 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 10,000 adults in Qatar, showing lower risk of COVID-19 cases with vitamin C supplementation, without statistical significance. Authors do not analyze COVID-19 severity.
This is the 67th of 74 COVID-19 controlled studies for vitamin C, which collectively show efficacy with p=0.000000068.
21 studies are RCTs, which show efficacy with p=0.0012.
|
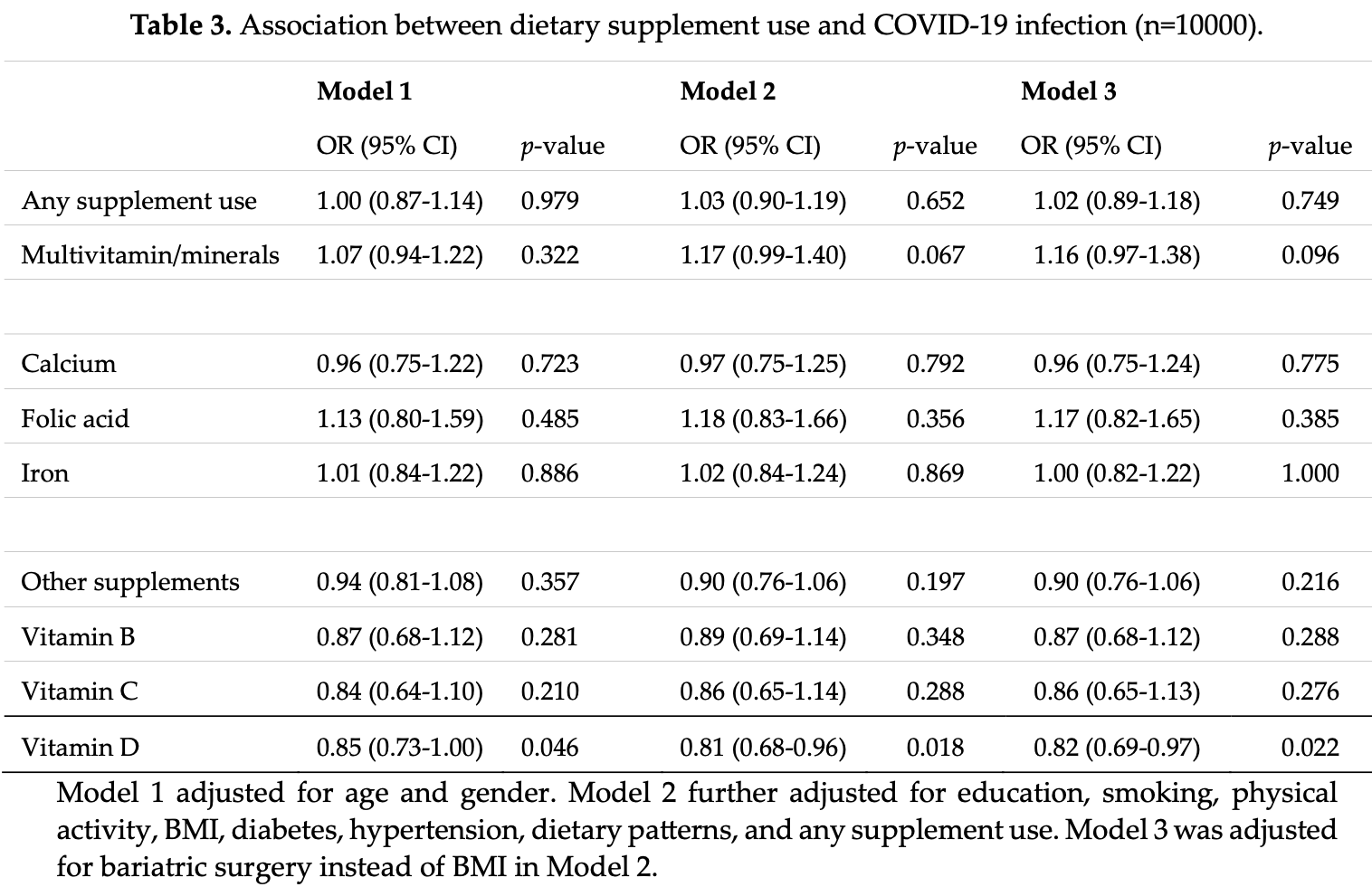
risk of case, 14.0% lower, OR 0.86, p = 0.29, treatment 665, control 9,335, adjusted per study, multivariable, model 2, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Akbar et al., 7 Nov 2023, retrospective, Qatar, peer-reviewed, mean age 40.3, 9 authors, study period March 2020 - September 2020, dosage not specified.
Contact: za1404491@student.qu.edu.qa, zumin@qu.edu.qa, almansouri@qu.edu.qa, h.alkhatib@qu.edu.qa, aaja@qu.edu.qa, abdshaito@qu.edu.qa, jessica.saliba@balamand.edu.lb, jamilnidal@gmail.com.
Association between lifestyle factors and COVID-19: findings from Qatar Biobank
doi:10.20944/preprints202311.0330.v1
Coronavirus Disease 2019 (COVID-19) exhibits a significant variation in presentation of symptoms ranging from mild to severe life-threatening symptoms, including death. COVID-19 infection susceptibility has been linked with various covariates, but studies in Qatar are limited. Data from Qatar Biobank (QBB) (n = 10,000; 18-to 79-year-old adults) were analyzed for associations between sociodemographic and lifestyle factors and susceptibility to COVID-19. Logistic regression was used to assess the associations between COVID-19 and age, gender, body mass index (BMI), smoking status, education level, dietary patterns, supplement use, physical activity, history of bariatric surgery, diabetes, and hypertension. In total, 10.5% (n = 1045) of the participants had COVID-19. Compared to non-smokers, current and ex-smokers had lower odds of having COVID-19 (odds ratio [OR]= 0.55; 95% CI: 0.44-0.68 and OR= 0.70; 95% CI: 0.57-0.86, respectively). Vitamin D supplement use was associated with an 18% reduction of the likelihood of contracting COVID-19 (OR = 0.82; 95% CI: 0.69-0.97). Obesity (BMI ≥30 kg/m 2 ), history of bariatric surgery and higher adherence to the modern dietary pattern-characterized by consumption of foods high in saturated fat and refined carbohydrates-were positively associated with COVID-19. Our findings indicate that adopting a healthy lifestyle may be helpful in the prevention of COVID-19 infection.
Author Contributions: Conceptualization, A.A.S. and Z.S.; investigation, A.A.S., Z.S., Z.A., J.S.; resources, A.A.S., Z.S.; writing-original draft preparation, A.A.S., Z.S., Z.A., ; writing-review and editing, All Authors; Supervision, A.A.S., Z.S., A.A.A.T; project administration, A.A.S.; funding acquisition, A.A.S. All authors have read and agreed to the published version of the manuscript. Funding: Qatar National Research Fund (QNRF) grant number RRC02-0807-210,022 to A.A.S. The funding source (QNRF) had no role in study design, in the collection, analysis and interpretation of data, in the writing of the manuscript, or in the decision to submit the article for publication.
Institutional Review Board
References
Adams, Baker, Sobieraj, Myth Busters: Dietary Supplements and COVID-19, Ann. Pharmacother, doi:10.1177/1060028020928052
Al Maskari, Al Blushi, Khamis, Al Tai, Al Salmi et al., Characteristics of Healthcare Workers Infected with COVID-19: A Cross-Sectional Observational Study, Int. J. Infect. Dis, doi:10.1016/j.ijid.2020.10.009
Al Thani, Fthenou, Paparrodopoulos, Al Marri, Shi et al., Qatar Biobank Cohort Study: Study Design and First Results, Am. J. Epidemiol, doi:10.1093/aje/kwz084
Aslan, Aslan, Zolbanin, Jafari, Acute Respiratory Distress Syndrome in COVID-19: Possible Mechanisms and Therapeutic Management, Pneumonia, doi:10.1186/s41479-021-00092-9
Bal, Finelli, Shope, Koch, Nutritional Deficiencies after Bariatric Surgery, Nat. Rev. Endocrinol, doi:10.1038/nrendo.2012.48
Bawadi, Akasheh, Kerkadi, Haydar, Tayyem et al., Validity and Reproducibility of a Food Frequency Questionnaire to Assess Macro and Micro-Nutrient Intake among a Convenience Cohort of Healthy Adult Qataris, Nutrients, doi:10.3390/nu13062002
Belanger, Hill, Angelidi, Dalamaga, Sowers et al., Covid-19 and Disparities in Nutrition and Obesity, N. Engl. J. Med, doi:10.1056/NEJMp2021264
Bilezikian, Bikle, Hewison, Lazaretti-Castro, Formenti et al., MECHANISMS IN ENDOCRINOLOGY: Vitamin D and COVID-19, Eur. J. Endocrinol, doi:10.1530/eje-20-0665
Bilezikian, Binkley, De Luca, Fassio, Formenti et al., Consensus and Controversial Aspects of Vitamin D and COVID-19, J. Clin. Endocrinol. Metab, doi:10.1210/clinem/dgac719
Brodin, Immune Determinants of COVID-19 Disease Presentation and Severity, Nat. Med, doi:10.1038/s41591-020-01202-8
Calder, Nutrition, Immunity and COVID-19, BMJ Nutr. Prev. Health, doi:10.1136/bmjnph-2020-000085
Clift, Von Ende, Tan, Sallis, Lindson et al., Smoking and COVID-19 Outcomes: An Observational and Mendelian Randomisation Study Using the UK Biobank Cohort, Thorax, doi:10.1136/thoraxjnl-2021-217080
De Lusignan, Dorward, Correa, Jones, Akinyemi et al., Risk Factors for SARS-CoV-2 among Patients in the Oxford Royal College of General Practitioners Research and Surveillance Centre Primary Care Network: A Cross-Sectional Study, Lancet Infect. Dis, doi:10.1016/s1473-3099(20)30371-6
Ebrahimzadeh, Taghizadeh, Milajerdi, Major Dietary Patterns in Relation to Disease Severity, Symptoms, and Inflammatory Markers in Patients Recovered from COVID-19, Front. Nutr, doi:10.3389/fnut.2022.929384
Eiser, Could Dietary Factors Reduce COVID-19 Mortality Rates? Moderating the Inflammatory State, J. Altern. Complement. Med, doi:10.1089/acm.2020.0441
Farsalinos, Eliopoulos, Leonidas, Papadopoulos, Tzartos et al., Nicotinic Cholinergic System and COVID-19: In Silico Identification of an Interaction between SARS-CoV-2 and Nicotinic Receptors with Potential Therapeutic Targeting Implications, Int. J. Mol. Sci, doi:10.3390/ijms21165807
Gallus, Scala, Possenti, Jarach, Clancy et al., The Role of Smoking in COVID-19 Progression: A Comprehensive Meta-Analysis, Eur. Respir. Rev, doi:10.1183/16000617.0191-2022
Gao, Li, Dai, Wang, Li et al., Is Prior Bariatric Surgery Associated with Poor COVID-19 Outcomes? A Systematic Review and Meta-Analysis of Case-Control Studies, J. Glob. Health, doi:10.7189/jogh.13.06012
Gibbons, Norton, Mccullough, Meltzer, Lavigne et al., Association between Vitamin D Supplementation and COVID-19 Infection and Mortality, Sci. Rep, doi:10.1038/s41598-022-24053-4
Giusti, Suter, Héraïef, Gaillard, Burckhardt, Effects of Laparoscopic Gastric Banding on Body Composition, Metabolic Profile and Nutritional Status of Obese Women: 12-Months Follow-Up, Obes. Surg
Greiller, Martineau, Modulation of the Immune Response to Respiratory Viruses by Vitamin D, Nutrients, doi:10.3390/nu7064240
Ho, Fernando, Chan, Sia, Obesity in COVID-19: A Systematic Review and Meta-Analysis, Ann. Acad. Med
Holt, Talaei, Greenig, Zenner, Symons et al., Risk Factors for Developing COVID-19: A Population-Based Longitudinal Study (COVIDENCE UK), Thorax, doi:10.1136/thoraxjnl-2021-217487
Iannelli, Bouam, Schneck, Frey, Zarca et al., The Impact of Previous History of Bariatric Surgery on Outcome of COVID-19. A Nationwide Medico-Administrative French Study, Obes. Surg, doi:10.1007/s11695-020-05120-z
Jolliffe, Holt, Greenig, Talaei, Perdek et al., Effect of a Test-and-Treat Approach to Vitamin D Supplementation on Risk of All Cause Acute Respiratory Tract Infection and Covid-19: Phase 3 Randomised Controlled Trial (CORONAVIT), BMJ, doi:10.1136/bmj-2022-071230
Kaeuffer, Le Hyaric, Fabacher, Mootien, Dervieux et al., Clinical Characteristics and Risk Factors Associated with Severe COVID-19: Prospective Analysis of 1,045 Hospitalised Cases in North-Eastern France, Euro Surveill
Keutmann, Hermes, Meinberger, Roth, Stemler et al., The Ratio of Serum LL-37 Levels to Blood Leucocyte Count Correlates with COVID-19 Severity, Sci. Rep, doi:10.1038/s41598-022-13260-8
Kilpatrick, Sánchez-Soliño, Alami, Johnson, Fang et al., EpidemiologiCal POpulatioN STudy of SARS-CoV-2 in Lake CounTy, Illinois (CONTACT): Methodology and Baseline Characteristics of a Community-Based Surveillance Study, Infect. Dis. Ther, doi:10.1007/s40121-022-00593-0
Kim, Rebholz, Hegde, Lafiura, Raghavan et al., Plant-Based Diets, Pescatarian Diets and COVID-19 Severity: A Population-Based Case-Control Study in Six Countries, BMJ Nutr. Prev. Health, doi:10.1136/bmjnph-2021-000272
Krutikov, Palmer, Tut, Fuller, Shrotri et al., Incidence of SARS-CoV-2 Infection According to Baseline Antibody Status in Staff and Residents of 100 Long-Term Care Facilities (VIVALDI): A Prospective Cohort Study, Lancet Healthy Longev, doi:10.1016/s2666-7568(21)00093-3
Kudryashova, Zani, Vilmen, Sharma, Lu et al., Inhibition of SARS-CoV-2 Infection by Human Defensin HNP1 and Retrocyclin RC-101, J. Mol. Biol, doi:10.1016/j.jmb.2021.167225
Leitzke, Is the Post-COVID-19 Syndrome a Severe Impairment of Acetylcholine-Orchestrated Neuromodulation That Responds to Nicotine Administration?, Bioelectron. Med, doi:10.1186/s42234-023-00104-7
Letizia, Ge, Vangeti, Goforth, Weir et al., SARS-CoV-2 Seropositivity and Subsequent Infection Risk in Healthy Young Adults: A Prospective Cohort Study, Lancet Respir. Med, doi:10.1016/s2213-2600(21)00158-2
Lewis, De Jersey, Seymour, Hopkins, Hickman et al., Vitamin B12, Folate and Copper Deficiency after Bariatric Surgery and the Impact on Anaemia: A Systematic Review, Obes. Surg, doi:10.1007/s11695-020-04872-y
Louca, Murray, Klaser, Graham, Mazidi et al., Modest Effects of Dietary Supplements during the COVID-19 Pandemic: Insights from 445 850 Users of the COVID-19 Symptom Study App, BMJ Nutr. Prev. Health, doi:10.1136/bmjnph-2021-000250
Lumley, O'donnell, Stoesser, Matthews, Howarth et al., Antibody Status and Incidence of SARS-CoV-2 Infection in Health Care Workers, N. Engl. J. Med, doi:10.1056/nejmoa2034545
Maggi, Rosellini, Spezia, Focosi, Macera et al., Nicotine Upregulates ACE2 Expression and Increases Competence for SARS-CoV-2 in Human Pneumocytes, ERJ Open Res, doi:10.1183/23120541.00713-2020
Mehta, Mcauley, Brown, Sanchez, Tattersall et al., Consider Cytokine Storm Syndromes and Immunosuppression, Lancet
Merino, Joshi, Nguyen, Leeming, Mazidi et al., Diet Quality and Risk and Severity of COVID-19: A Prospective Cohort Study, Gut, doi:10.1136/gutjnl-2021-325353
Michalakis, Ilias, SARS-CoV -2 Infection and Obesity: Common Inflammatory and Metabolic Aspects, Diabetes Metab Syndr
Mitchell, Vitamin-D and COVID-19: Do Deficient Risk a Poorer Outcome?, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30183-2
Mohammadi, Heidarizadeh, Entesari, Esmailpour, Esmailpour et al., In Silico Investigation on the Inhibiting Role of Nicotine/Caffeine by Blocking the S Protein of SARS-CoV-2 versus ACE2 Receptor, Microorganisms, doi:10.3390/microorganisms8101600
Morales-Marroquin, Xie, Uppuluri, Almandoz, De La Cruz-Muñoz et al., Immunosuppression and Clostridioides (Clostridium) Difficile Infection Risk in Metabolic and Bariatric Surgery Patients, J. Am. Coll. Surg, doi:10.1016/j.jamcollsurg.2021.04.028
Paleiron, Mayet, Marbac, Perisse, Barazzutti et al., Impact of Tobacco Smoking on the Risk of COVID-19: A Large Scale Retrospective Cohort Study, Nicotine Tob. Res, doi:10.1093/ntr/ntab004
Park, Lee, Suh, Song, Byun et al., Effect of Asthma and Asthma Medication on the Prognosis of Patients with COVID-19, Eur. Respir. J, doi:10.1183/13993003.02226-2020
Rahmati, Fatemi, Yon, Lee, Koyanagi et al., The Effect of Adherence to High-quality Dietary Pattern on COVID-19 Outcomes: A Systematic Review and Meta-analysis, J. Med. Virol, doi:10.1002/jmv.28298
Rodriguez-Diaz, Guilamo-Ramos, Mena, Hall, Honermann et al., Risk for COVID-19 Infection and Death among Latinos in the United States: Examining Heterogeneity in Transmission Dynamics, Ann. Epidemiol, doi:10.1016/j.annepidem.2020.07.007
Salazar-Robles, Kalantar-Zadeh, Badillo, Calderón-Juárez, García-Bárcenas et al., Association between Severity of COVID-19 Symptoms and Habitual Food Intake in Adult Outpatients, BMJ Nutr. Prev. Health, doi:10.1136/bmjnph-2021-000348
Salehi, Motlagh Ghoochani, Hasani Nourian, Jamalkandi, Ghanei, The Controversial Effect of Smoking and Nicotine in SARS-CoV-2 Infection, Allergy Asthma Clin. Immunol, doi:10.1186/s13223-023-00797-0
Simons, Shahab, Brown, Perski, The Association of Smoking Status with SARS-CoV-2 Infection, Hospitalization and Mortality from COVID-19: A Living Rapid Evidence Review with Bayesian Meta-Analyses (Version 7), Addiction, doi:10.1111/add.15276
Soltani, Jaam, Nazar, Stewart, Shaito, Attitudes and Beliefs Regarding the Use of Herbs and Supplementary Medications with COVID-19: A Systematic Review, Res. Social Adm. Pharm, doi:10.1016/j.sapharm.2022.11.004
Tadayon Najafabadi, Rayner, Shokraee, Shokraie, Panahi et al., Obesity as an Independent Risk Factor for COVID-19 Severity and Mortality, Cochrane Libr, doi:10.1002/14651858.cd015201
Theodore, Branche, Zhang, Graciaa, Choudhary et al., Clinical and Demographic Factors Associated with COVID-19, Severe COVID-19, and SARS-CoV-2 Infection in Adults: A Secondary Cross-Protocol Analysis of 4 Randomized Clinical Trials, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2023.23349
Tindle, Newhouse, Freiberg, Beyond Smoking Cessation: Investigating Medicinal Nicotine to Prevent and Treat COVID-19, Nicotine Tob. Res, doi:10.1093/ntr/ntaa077
Tracey, The Inflammatory Reflex, Nature, doi:10.1038/nature01321
Villasis-Keever, López-Alarcón, Miranda-Novales, Zurita-Cruz, Barrada-Vázquez et al., Efficacy and Safety of Vitamin D Supplementation to Prevent COVID-19 in Frontline Healthcare Workers. A Randomized Clinical Trial, Arch. Med. Res, doi:10.1016/j.arcmed.2022.04.003
Wander, Lowy, Beste, Tulloch-Palomino, Korpak et al., The Incidence of Diabetes among 2,808,106 Veterans with and without Recent SARS-CoV-2 Infection, Diabetes Care, doi:10.2337/dc21-1686
Wiersinga, Rhodes, Cheng, Peacock, Prescott et al., Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review, JAMA, doi:10.1001/jama.2020.12839
Wood, Benotti, Fano, Dove, Rolston et al., Prior Metabolic Surgery Reduced COVID-19 Severity: Systematic Analysis from Year One of the COVID-19 Pandemic, Heliyon, doi:10.1016/j.heliyon.2023.e15824
Yan, Chu, Yang, Sze, Lai et al., Characterization of the Lipidomic Profile of Human Coronavirus-Infected Cells: Implications for Lipid Metabolism Remodeling upon Coronavirus Replication, Viruses, doi:10.3390/v11010073
Zhao, Li, Gao, Zhao, Chen et al., A Review of Statistical Methods for Dietary Pattern Analysis, Nutr. J, doi:10.1186/s12937-021-00692-7
DOI record:
{
"DOI": "10.3390/nu16071037",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu16071037",
"abstract": "<jats:p>Coronavirus Disease 2019 (COVID-19) manifestations range from mild to severe life-threatening symptoms, including death. COVID-19 susceptibility has been associated with various factors, but studies in Qatar are limited. The objective of this study was to investigate the correlation between COVID-19 susceptibility and various sociodemographic and lifestyle factors, including age, gender, body mass index, smoking status, education level, dietary patterns, supplement usage, physical activity, a history of bariatric surgery, diabetes, and hypertension. We utilized logistic regression to analyze these associations, using the data of 10,000 adult participants, aged from 18 to 79, from Qatar Biobank. In total, 10.5% (n = 1045) of the participants had COVID-19. Compared to non-smokers, current and ex-smokers had lower odds of having COVID-19 (odds ratio [OR] = 0.55; 95% CI: 0.44–0.68 and OR = 0.70; 95% CI: 0.57–0.86, respectively). Vitamin D supplement use was associated with an 18% reduction in the likelihood of contracting COVID-19 (OR = 0.82; 95% CI: 0.69–0.97). Obesity (BMI ≥ 30 kg/m2), a history of bariatric surgery, and higher adherence to the modern dietary pattern—characterized by the consumption of foods high in saturated fat and refined carbohydrates—were positively associated with COVID-19. Our findings indicate that adopting a healthy lifestyle may be helpful in the prevention of COVID-19 infection.</jats:p>",
"alternative-id": [
"nu16071037"
],
"author": [
{
"affiliation": [
{
"name": "Department of Human Nutrition, College of Health Sciences, QU Health, Qatar University, Doha P.O. Box 2713, Qatar"
}
],
"family": "Akbar",
"given": "Zoha",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Biomedical Research Center, Qatar University, Doha P.O. Box 2713, Qatar"
}
],
"family": "Kunhipurayil",
"given": "Hasna H.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9117-8773",
"affiliation": [
{
"name": "Department of Public Health, Faculty of Health Sciences, University of Balamand, Beirut P.O. Box 100, Lebanon"
},
{
"name": "Department of Biology, Faculty of Sciences, Lebanese University, Beirut P.O. Box 90656, Lebanon"
}
],
"authenticated-orcid": false,
"family": "Saliba",
"given": "Jessica",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Hamad Medical Corporation, Doha P.O. Box 3050, Qatar"
}
],
"family": "Ahmad",
"given": "Jamil",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Biomedical Research Center, Qatar University, Doha P.O. Box 2713, Qatar"
},
{
"name": "Department of Biomedical Sciences, College of Health Sciences, QU Health, Qatar University, Doha P.O. Box 2713, Qatar"
}
],
"family": "Al-Mansoori",
"given": "Layla",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Biomedical Research Center, Qatar University, Doha P.O. Box 2713, Qatar"
}
],
"family": "Al-Khatib",
"given": "Hebah A.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Biomedical Research Center, Qatar University, Doha P.O. Box 2713, Qatar"
},
{
"name": "Department of Biomedical Sciences, College of Health Sciences, QU Health, Qatar University, Doha P.O. Box 2713, Qatar"
}
],
"family": "Al Thani",
"given": "Asmaa A.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3099-3299",
"affiliation": [
{
"name": "Department of Human Nutrition, College of Health Sciences, QU Health, Qatar University, Doha P.O. Box 2713, Qatar"
}
],
"authenticated-orcid": false,
"family": "Shi",
"given": "Zumin",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3524-7962",
"affiliation": [
{
"name": "Biomedical Research Center, Qatar University, Doha P.O. Box 2713, Qatar"
},
{
"name": "Department of Biomedical Sciences, College of Health Sciences, QU Health, Qatar University, Doha P.O. Box 2713, Qatar"
},
{
"name": "Department of Basic Medical Sciences, College of Medicine, QU Health, Qatar University, Doha P.O. Box 2713, Qatar"
}
],
"authenticated-orcid": false,
"family": "Shaito",
"given": "Abdullah A.",
"sequence": "additional"
}
],
"container-title": "Nutrients",
"container-title-short": "Nutrients",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
4,
3
]
],
"date-time": "2024-04-03T04:58:38Z",
"timestamp": 1712120318000
},
"deposited": {
"date-parts": [
[
2024,
4,
3
]
],
"date-time": "2024-04-03T05:32:50Z",
"timestamp": 1712122370000
},
"funder": [
{
"award": [
"RRC02-0807-210,022"
],
"name": "Qatar National Research Fund"
}
],
"indexed": {
"date-parts": [
[
2024,
4,
4
]
],
"date-time": "2024-04-04T00:58:40Z",
"timestamp": 1712192320655
},
"is-referenced-by-count": 0,
"issue": "7",
"issued": {
"date-parts": [
[
2024,
4,
3
]
]
},
"journal-issue": {
"issue": "7",
"published-online": {
"date-parts": [
[
2024,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
4,
3
]
],
"date-time": "2024-04-03T00:00:00Z",
"timestamp": 1712102400000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/16/7/1037/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1037",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2024,
4,
3
]
]
},
"published-online": {
"date-parts": [
[
2024,
4,
3
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"key": "ref_1",
"unstructured": "(2023, November 05). WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/."
},
{
"DOI": "10.1001/jama.2020.12839",
"article-title": "Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review",
"author": "Wiersinga",
"doi-asserted-by": "crossref",
"first-page": "782",
"journal-title": "JAMA",
"key": "ref_2",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1186/s41479-021-00092-9",
"article-title": "Acute Respiratory Distress Syndrome in COVID-19: Possible Mechanisms and Therapeutic Management",
"author": "Aslan",
"doi-asserted-by": "crossref",
"first-page": "14",
"journal-title": "Pneumonia",
"key": "ref_3",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1038/s41591-020-01202-8",
"article-title": "Immune Determinants of COVID-19 Disease Presentation and Severity",
"author": "Brodin",
"doi-asserted-by": "crossref",
"first-page": "28",
"journal-title": "Nat. Med.",
"key": "ref_4",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1177/1060028020928052",
"article-title": "Myth Busters: Dietary Supplements and COVID-19",
"author": "Adams",
"doi-asserted-by": "crossref",
"first-page": "820",
"journal-title": "Ann. Pharmacother.",
"key": "ref_5",
"volume": "54",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30183-2",
"article-title": "Vitamin-D and COVID-19: Do Deficient Risk a Poorer Outcome?",
"author": "Mitchell",
"doi-asserted-by": "crossref",
"first-page": "570",
"journal-title": "Lancet Diabetes Endocrinol.",
"key": "ref_6",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1001/jamanetworkopen.2023.23349",
"article-title": "Clinical and Demographic Factors Associated with COVID-19, Severe COVID-19, and SARS-CoV-2 Infection in Adults: A Secondary Cross-Protocol Analysis of 4 Randomized Clinical Trials",
"author": "Theodore",
"doi-asserted-by": "crossref",
"first-page": "e2323349",
"journal-title": "JAMA Netw. Open",
"key": "ref_7",
"volume": "6",
"year": "2023"
},
{
"DOI": "10.1016/j.annepidem.2020.07.007",
"article-title": "Risk for COVID-19 Infection and Death among Latinos in the United States: Examining Heterogeneity in Transmission Dynamics",
"author": "Mena",
"doi-asserted-by": "crossref",
"first-page": "46",
"journal-title": "Ann. Epidemiol.",
"key": "ref_8",
"volume": "52",
"year": "2020"
},
{
"DOI": "10.1136/thoraxjnl-2021-217487",
"article-title": "Risk Factors for Developing COVID-19: A Population-Based Longitudinal Study (COVIDENCE UK)",
"author": "Holt",
"doi-asserted-by": "crossref",
"first-page": "900",
"journal-title": "Thorax",
"key": "ref_9",
"volume": "77",
"year": "2022"
},
{
"DOI": "10.2807/1560-7917.ES.2020.25.48.2000895",
"article-title": "Clinical Characteristics and Risk Factors Associated with Severe COVID-19: Prospective Analysis of 1045 Hospitalised Cases in North-Eastern France, March 2020",
"author": "Kaeuffer",
"doi-asserted-by": "crossref",
"first-page": "2000895",
"journal-title": "Eurosurveillance",
"key": "ref_10",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.1136/bmjnph-2021-000250",
"article-title": "Modest Effects of Dietary Supplements during the COVID-19 Pandemic: Insights from 445 850 Users of the COVID-19 Symptom Study App",
"author": "Louca",
"doi-asserted-by": "crossref",
"first-page": "149",
"journal-title": "BMJ Nutr. Prev. Health",
"key": "ref_11",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1002/jmv.28298",
"article-title": "The Effect of Adherence to High-quality Dietary Pattern on COVID-19 Outcomes: A Systematic Review and Meta-analysis",
"author": "Rahmati",
"doi-asserted-by": "crossref",
"first-page": "e28298",
"journal-title": "J. Med. Virol.",
"key": "ref_12",
"volume": "95",
"year": "2023"
},
{
"DOI": "10.47102/annals-acadmedsg.2020299",
"article-title": "Obesity in COVID-19: A Systematic Review and Meta-Analysis",
"author": "Ho",
"doi-asserted-by": "crossref",
"first-page": "996",
"journal-title": "Ann. Acad. Med. Singapore",
"key": "ref_13",
"volume": "49",
"year": "2020"
},
{
"article-title": "Obesity as an Independent Risk Factor for COVID-19 Severity and Mortality",
"author": "Najafabadi",
"first-page": "CD015201",
"journal-title": "Cochrane Database Syst. Rev.",
"key": "ref_14",
"volume": "5",
"year": "2023"
},
{
"DOI": "10.2337/dc21-1686",
"article-title": "The Incidence of Diabetes among 2,808,106 Veterans with and without Recent SARS-CoV-2 Infection",
"author": "Wander",
"doi-asserted-by": "crossref",
"first-page": "782",
"journal-title": "Diabetes Care",
"key": "ref_15",
"volume": "45",
"year": "2022"
},
{
"DOI": "10.1016/j.lfs.2020.118661",
"article-title": "Implicating the Effect of Ketogenic Diet as a Preventive Measure to Obesity and Diabetes Mellitus",
"author": "Kumar",
"doi-asserted-by": "crossref",
"first-page": "118661",
"journal-title": "Life Sci.",
"key": "ref_16",
"volume": "264",
"year": "2021"
},
{
"key": "ref_17",
"unstructured": "(2023). Annual Report 2022–2023, Qatar Biobank."
},
{
"DOI": "10.1093/aje/kwz084",
"article-title": "Qatar Biobank Cohort Study: Study Design and First Results",
"author": "Fthenou",
"doi-asserted-by": "crossref",
"first-page": "1420",
"journal-title": "Am. J. Epidemiol.",
"key": "ref_18",
"volume": "188",
"year": "2019"
},
{
"DOI": "10.5339/jemtac.2021.qhc.6",
"doi-asserted-by": "crossref",
"key": "ref_19",
"unstructured": "Afifi, N., Fthenou, E., El Deeb, M., Frenneaux, M., Al Thani, A., Al Khal, A.L., and Biobank, Q.J. (2021). Qatar Biobank: COVID-19 Biorepository Project. Emerg. Med. Trauma Acute Care."
},
{
"DOI": "10.3390/nu13062002",
"doi-asserted-by": "crossref",
"key": "ref_20",
"unstructured": "Bawadi, H., Akasheh, R.T., Kerkadi, A., Haydar, S., Tayyem, R., and Shi, Z. (2021). Validity and Reproducibility of a Food Frequency Questionnaire to Assess Macro and Micro-Nutrient Intake among a Convenience Cohort of Healthy Adult Qataris. Nutrients, 13."
},
{
"key": "ref_21",
"unstructured": "StataCorp (2023). Stata Statistical Software: Release 17, StataCorp LLC."
},
{
"key": "ref_22",
"unstructured": "(2023, November 27). WMA Declaration of Helsinki–Ethical Principles for Medical Research Involving Human Subjects. Available online: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/."
},
{
"DOI": "10.1186/s40795-022-00522-x",
"doi-asserted-by": "crossref",
"key": "ref_23",
"unstructured": "Arab, A., Rafie, N., Hadi, A., Khorvash, F., Heidari, Z., and Askari, G. (2022). Empirically Derived Dietary Patterns and Their Association with Mental Health: A Cross-Sectional Sample of Iranian Migraine Patients (2019–2020). BMC Nutr., 8."
},
{
"DOI": "10.3390/nu15184053",
"doi-asserted-by": "crossref",
"key": "ref_24",
"unstructured": "Fituri, S., and Shi, Z. (2023). Association between Dietary Patterns and Cognitive Function among Qatari Adults: A Cross-Sectional Analysis of the Qatar Biobank Study. Nutrients, 15."
},
{
"DOI": "10.1108/NFS-05-2019-0147",
"article-title": "Dietary Patterns and Nutrients Associated with Metabolic Syndrome",
"author": "Tayyem",
"doi-asserted-by": "crossref",
"first-page": "253",
"journal-title": "Nutr. Food Sci.",
"key": "ref_25",
"volume": "50",
"year": "2019"
},
{
"DOI": "10.1186/s12937-021-00692-7",
"article-title": "A Review of Statistical Methods for Dietary Pattern Analysis",
"author": "Zhao",
"doi-asserted-by": "crossref",
"first-page": "37",
"journal-title": "Nutr. J.",
"key": "ref_26",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.1016/S1473-3099(20)30371-6",
"article-title": "Risk Factors for SARS-CoV-2 among Patients in the Oxford Royal College of General Practitioners Research and Surveillance Centre Primary Care Network: A Cross-Sectional Study",
"author": "Dorward",
"doi-asserted-by": "crossref",
"first-page": "1034",
"journal-title": "Lancet Infect. Dis.",
"key": "ref_27",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1093/ntr/ntab004",
"article-title": "Impact of Tobacco Smoking on the Risk of COVID-19: A Large Scale Retrospective Cohort Study",
"author": "Paleiron",
"doi-asserted-by": "crossref",
"first-page": "1398",
"journal-title": "Nicotine Tob. Res.",
"key": "ref_28",
"volume": "23",
"year": "2021"
},
{
"DOI": "10.1111/add.15276",
"article-title": "The Association of Smoking Status with SARS-CoV-2 Infection, Hospitalization and Mortality from COVID-19: A Living Rapid Evidence Review with Bayesian Meta-Analyses (Version 7)",
"author": "Simons",
"doi-asserted-by": "crossref",
"first-page": "1319",
"journal-title": "Addiction",
"key": "ref_29",
"volume": "116",
"year": "2021"
},
{
"DOI": "10.1183/23120541.00713-2020",
"article-title": "Nicotine Upregulates ACE2 Expression and Increases Competence for SARS-CoV-2 in Human Pneumocytes",
"author": "Maggi",
"doi-asserted-by": "crossref",
"first-page": "00713",
"journal-title": "ERJ Open Res.",
"key": "ref_30",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1186/s13223-023-00797-0",
"article-title": "The Controversial Effect of Smoking and Nicotine in SARS-CoV-2 Infection",
"author": "Salehi",
"doi-asserted-by": "crossref",
"first-page": "49",
"journal-title": "Allergy Asthma Clin. Immunol.",
"key": "ref_31",
"volume": "19",
"year": "2023"
},
{
"DOI": "10.1093/ntr/ntaa077",
"article-title": "Beyond Smoking Cessation: Investigating Medicinal Nicotine to Prevent and Treat COVID-19",
"author": "Tindle",
"doi-asserted-by": "crossref",
"first-page": "1669",
"journal-title": "Nicotine Tob. Res.",
"key": "ref_32",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.3390/microorganisms8101600",
"doi-asserted-by": "crossref",
"key": "ref_33",
"unstructured": "Mohammadi, S., Heidarizadeh, M., Entesari, M., Esmailpour, A., Esmailpour, M., Moradi, R., Sakhaee, N., and Doustkhah, E. (2020). In Silico Investigation on the Inhibiting Role of Nicotine/Caffeine by Blocking the S Protein of SARS-CoV-2 versus ACE2 Receptor. Microorganisms, 8."
},
{
"DOI": "10.3390/ijms21165807",
"doi-asserted-by": "crossref",
"key": "ref_34",
"unstructured": "Farsalinos, K., Eliopoulos, E., Leonidas, D.D., Papadopoulos, G.E., Tzartos, S., and Poulas, K. (2020). Nicotinic Cholinergic System and COVID-19: In Silico Identification of an Interaction between SARS-CoV-2 and Nicotinic Receptors with Potential Therapeutic Targeting Implications. Int. J. Mol. Sci., 21."
},
{
"DOI": "10.1186/s42234-023-00104-7",
"doi-asserted-by": "crossref",
"key": "ref_35",
"unstructured": "Leitzke, M. (2023). Is the Post-COVID-19 Syndrome a Severe Impairment of Acetylcholine-Orchestrated Neuromodulation That Responds to Nicotine Administration?. Bioelectron. Med., 9."
},
{
"DOI": "10.1016/S0140-6736(20)30628-0",
"article-title": "COVID-19: Consider Cytokine Storm Syndromes and Immunosuppression",
"author": "Mehta",
"doi-asserted-by": "crossref",
"first-page": "1033",
"journal-title": "Lancet",
"key": "ref_36",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1038/nature01321",
"article-title": "The Inflammatory Reflex",
"author": "Tracey",
"doi-asserted-by": "crossref",
"first-page": "853",
"journal-title": "Nature",
"key": "ref_37",
"volume": "420",
"year": "2002"
},
{
"DOI": "10.1136/thoraxjnl-2021-217080",
"article-title": "Smoking and COVID-19 Outcomes: An Observational and Mendelian Randomisation Study Using the UK Biobank Cohort",
"author": "Clift",
"doi-asserted-by": "crossref",
"first-page": "65",
"journal-title": "Thorax",
"key": "ref_38",
"volume": "77",
"year": "2022"
},
{
"DOI": "10.1183/16000617.0191-2022",
"article-title": "The Role of Smoking in COVID-19 Progression: A Comprehensive Meta-Analysis",
"author": "Gallus",
"doi-asserted-by": "crossref",
"first-page": "220191",
"journal-title": "Eur. Respir. Rev.",
"key": "ref_39",
"volume": "32",
"year": "2023"
},
{
"DOI": "10.1210/clinem/dgac719",
"article-title": "Consensus and Controversial Aspects of Vitamin D and COVID-19",
"author": "Bilezikian",
"doi-asserted-by": "crossref",
"first-page": "1034",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "ref_40",
"volume": "108",
"year": "2023"
},
{
"DOI": "10.1038/s41598-022-24053-4",
"article-title": "Association between Vitamin D Supplementation and COVID-19 Infection and Mortality",
"author": "Gibbons",
"doi-asserted-by": "crossref",
"first-page": "19397",
"journal-title": "Sci. Rep.",
"key": "ref_41",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1016/j.arcmed.2022.04.003",
"article-title": "Efficacy and Safety of Vitamin D Supplementation to Prevent COVID-19 in Frontline Healthcare Workers. A Randomized Clinical Trial",
"doi-asserted-by": "crossref",
"first-page": "423",
"journal-title": "Arch. Med. Res.",
"key": "ref_42",
"volume": "53",
"year": "2022"
},
{
"DOI": "10.1136/bmj-2022-071230",
"article-title": "Effect of a Test-and-Treat Approach to Vitamin D Supplementation on Risk of All Cause Acute Respiratory Tract Infection and Covid-19: Phase 3 Randomised Controlled Trial (CORONAVIT)",
"author": "Jolliffe",
"doi-asserted-by": "crossref",
"first-page": "e071230",
"journal-title": "BMJ",
"key": "ref_43",
"volume": "378",
"year": "2022"
},
{
"DOI": "10.3390/nu7064240",
"article-title": "Modulation of the Immune Response to Respiratory Viruses by Vitamin D",
"author": "Greiller",
"doi-asserted-by": "crossref",
"first-page": "4240",
"journal-title": "Nutrients",
"key": "ref_44",
"volume": "7",
"year": "2015"
},
{
"DOI": "10.1038/s41598-022-13260-8",
"article-title": "The Ratio of Serum LL-37 Levels to Blood Leucocyte Count Correlates with COVID-19 Severity",
"author": "Keutmann",
"doi-asserted-by": "crossref",
"first-page": "9447",
"journal-title": "Sci. Rep.",
"key": "ref_45",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1101/2021.05.27.445985",
"doi-asserted-by": "crossref",
"key": "ref_46",
"unstructured": "Kudryashova, E., Zani, A., Vilmen, G., Sharma, A., Lu, W., Yount, J.S., and Kudryashov, D.S. (2022). Inhibition of SARS-CoV-2 Infection by Human Defensin HNP1 and Retrocyclin RC-101. J. Mol. Biol., 434."
},
{
"DOI": "10.1530/EJE-20-0665",
"article-title": "Mechanisms In Endocrinology: Vitamin D and COVID-19",
"author": "Bilezikian",
"doi-asserted-by": "crossref",
"first-page": "R133",
"journal-title": "Eur. J. Endocrinol.",
"key": "ref_47",
"volume": "183",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.04.033",
"article-title": "SARS-CoV -2 Infection and Obesity: Common Inflammatory and Metabolic Aspects",
"author": "Michalakis",
"doi-asserted-by": "crossref",
"first-page": "469",
"journal-title": "Diabetes Metab. Syndr.",
"key": "ref_48",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.7189/jogh.13.06012",
"article-title": "Is Prior Bariatric Surgery Associated with Poor COVID-19 Outcomes? A Systematic Review and Meta-Analysis of Case-Control Studies",
"author": "Gao",
"doi-asserted-by": "crossref",
"first-page": "06012",
"journal-title": "J. Glob. Health",
"key": "ref_49",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1016/j.heliyon.2023.e15824",
"article-title": "Prior Metabolic Surgery Reduced COVID-19 Severity: Systematic Analysis from Year One of the COVID-19 Pandemic",
"author": "Wood",
"doi-asserted-by": "crossref",
"first-page": "e15824",
"journal-title": "Heliyon",
"key": "ref_50",
"volume": "9",
"year": "2023"
},
{
"DOI": "10.1007/s11695-020-05120-z",
"article-title": "The Impact of Previous History of Bariatric Surgery on Outcome of COVID-19. A Nationwide Medico-Administrative French Study",
"author": "Iannelli",
"doi-asserted-by": "crossref",
"first-page": "1455",
"journal-title": "Obes. Surg.",
"key": "ref_51",
"volume": "31",
"year": "2021"
},
{
"DOI": "10.1007/s11695-020-04872-y",
"article-title": "Iron, Vitamin B12, Folate and Copper Deficiency after Bariatric Surgery and the Impact on Anaemia: A Systematic Review",
"author": "Lewis",
"doi-asserted-by": "crossref",
"first-page": "4542",
"journal-title": "Obes. Surg.",
"key": "ref_52",
"volume": "30",
"year": "2020"
},
{
"DOI": "10.1038/nrendo.2012.48",
"article-title": "Nutritional Deficiencies after Bariatric Surgery",
"author": "Bal",
"doi-asserted-by": "crossref",
"first-page": "544",
"journal-title": "Nat. Rev. Endocrinol.",
"key": "ref_53",
"volume": "8",
"year": "2012"
},
{
"DOI": "10.1381/096089204322857636",
"article-title": "Effects of Laparoscopic Gastric Banding on Body Composition, Metabolic Profile and Nutritional Status of Obese Women: 12-Months Follow-Up",
"author": "Giusti",
"doi-asserted-by": "crossref",
"first-page": "239",
"journal-title": "Obes. Surg.",
"key": "ref_54",
"volume": "14",
"year": "2004"
},
{
"DOI": "10.1016/j.jamcollsurg.2021.04.028",
"article-title": "Immunosuppression and Clostridioides (Clostridium) Difficile Infection Risk in Metabolic and Bariatric Surgery Patients",
"author": "Xie",
"doi-asserted-by": "crossref",
"first-page": "223",
"journal-title": "J. Am. Coll. Surg.",
"key": "ref_55",
"volume": "233",
"year": "2021"
},
{
"DOI": "10.3389/fnut.2022.929384",
"article-title": "Major Dietary Patterns in Relation to Disease Severity, Symptoms, and Inflammatory Markers in Patients Recovered from COVID-19",
"author": "Ebrahimzadeh",
"doi-asserted-by": "crossref",
"first-page": "929384",
"journal-title": "Front. Nutr.",
"key": "ref_56",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.1136/gutjnl-2021-325353",
"article-title": "Diet Quality and Risk and Severity of COVID-19: A Prospective Cohort Study",
"author": "Merino",
"doi-asserted-by": "crossref",
"first-page": "2096",
"journal-title": "Gut",
"key": "ref_57",
"volume": "70",
"year": "2021"
},
{
"DOI": "10.1136/bmjnph-2021-000272",
"article-title": "Pescatarian Diets and COVID-19 Severity: A Population-Based Case–Control Study in Six Countries",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "257",
"journal-title": "BMJ Nutr. Prev. Health",
"key": "ref_58",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1136/bmjnph-2021-000348",
"article-title": "Association between Severity of COVID-19 Symptoms and Habitual Food Intake in Adult Outpatients",
"author": "Badillo",
"doi-asserted-by": "crossref",
"first-page": "469",
"journal-title": "BMJ Nutr. Prev. Health",
"key": "ref_59",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1136/bmjnph-2020-000085",
"article-title": "Nutrition, Immunity and COVID-19",
"author": "Calder",
"doi-asserted-by": "crossref",
"first-page": "74",
"journal-title": "BMJ Nutr. Prev. Health",
"key": "ref_60",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1056/NEJMp2021264",
"article-title": "COVID-19 and Disparities in Nutrition and Obesity",
"author": "Belanger",
"doi-asserted-by": "crossref",
"first-page": "e69",
"journal-title": "N. Engl. J. Med.",
"key": "ref_61",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.3390/v11010073",
"doi-asserted-by": "crossref",
"key": "ref_62",
"unstructured": "Yan, B., Chu, H., Yang, D., Sze, K.-H., Lai, P.-M., Yuan, S., Shuai, H., Wang, Y., Kao, R.Y.-T., and Chan, J.F.-W. (2019). Characterization of the Lipidomic Profile of Human Coronavirus-Infected Cells: Implications for Lipid Metabolism Remodeling upon Coronavirus Replication. Viruses, 11."
},
{
"DOI": "10.1089/acm.2020.0441",
"article-title": "Could Dietary Factors Reduce COVID-19 Mortality Rates? Moderating the Inflammatory State",
"author": "Eiser",
"doi-asserted-by": "crossref",
"first-page": "176",
"journal-title": "J. Altern. Complement. Med.",
"key": "ref_63",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1016/j.bbi.2020.04.040",
"article-title": "The Impact of Nutrition on COVID-19 Susceptibility and Long-Term Consequences",
"author": "Butler",
"doi-asserted-by": "crossref",
"first-page": "53",
"journal-title": "Brain Behav. Immun.",
"key": "ref_64",
"volume": "87",
"year": "2020"
},
{
"DOI": "10.1016/j.sapharm.2022.11.004",
"article-title": "Attitudes and Beliefs Regarding the Use of Herbs and Supplementary Medications with COVID-19: A Systematic Review",
"author": "Soltani",
"doi-asserted-by": "crossref",
"first-page": "343",
"journal-title": "Res. Social Adm. Pharm.",
"key": "ref_65",
"volume": "19",
"year": "2023"
},
{
"DOI": "10.3390/molecules27175573",
"doi-asserted-by": "crossref",
"key": "ref_66",
"unstructured": "Hassan, S.S.U., Abdel-Daim, M.M., Behl, T., and Bungau, S. (2022). Natural Products for Chronic Diseases: A Ray of Hope. Molecules, 27."
}
],
"reference-count": 66,
"references-count": 66,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2072-6643/16/7/1037"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "The Association between Lifestyle Factors and COVID-19: Findings from Qatar Biobank",
"type": "journal-article",
"volume": "16"
}
akbar2