Association between vitamin D supplementation and COVID-19 infection and mortality
et al., Scientific Reports, doi:10.1038/s41598-022-24053-4, Nov 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
PSM retrospective in the USA, showing lower COVID-19 mortality and cases with vitamin D prophylaxis.
This is the 105th of 135 COVID-19 controlled studies for vitamin D, which collectively show efficacy with p<0.0000000001.
40 studies are RCTs, which show efficacy with p=0.0000001.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
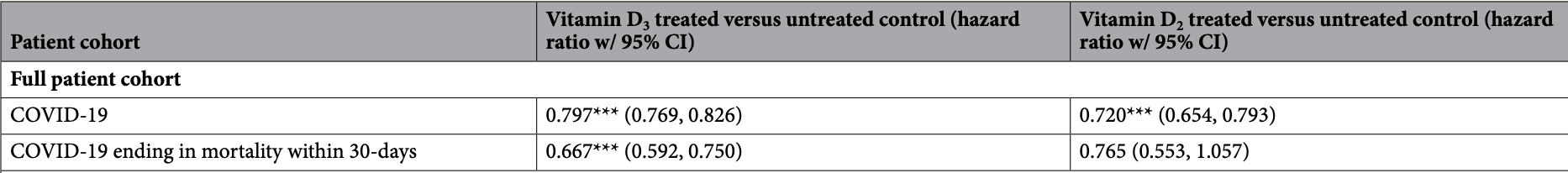
risk of death, 33.3% lower, HR 0.67, p < 0.001, treatment 5,315 of 199,498 (2.7%), control 6,591 of 199,498 (3.3%), D3, propensity score matching, Cox proportional hazards.
|
|
risk of death, 23.5% lower, HR 0.77, p = 0.10, treatment 716 of 33,216 (2.2%), control 987 of 33,216 (3.0%), NNT 123, D2, propensity score matching, Cox proportional hazards.
|
|
risk of case, 20.3% lower, HR 0.80, p < 0.001, treatment 462 of 199,498 (0.2%), control 689 of 199,498 (0.3%), D3, propensity score matching, Cox proportional hazards.
|
|
risk of case, 28.0% lower, HR 0.72, p < 0.001, treatment 65 of 33,216 (0.2%), control 86 of 33,216 (0.3%), NNT 1582, D2, propensity score matching, Cox proportional hazards.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Gibbons et al., 12 Nov 2022, retrospective, USA, peer-reviewed, 7 authors, dosage varies.
Contact: jgibbo13@jhu.edu.
Association between vitamin D supplementation and COVID-19 infection and mortality
Scientific Reports, doi:10.1038/s41598-022-24053-4
Vitamin D deficiency has long been associated with reduced immune function that can lead to viral infection. Several studies have shown that Vitamin D deficiency is associated with increases the risk of infection with COVID-19. However, it is unknown if treatment with Vitamin D can reduce the associated risk of COVID-19 infection, which is the focus of this study. In the population of US veterans, we show that Vitamin D 2 and D 3 fills were associated with reductions in COVID-19 infection of 28% and 20%, respectively [(D 3 Hazard Ratio (HR) = 0.80, [95% CI 0.77, 0.83]), D 2 HR = 0.72, [95% CI 0.65, 0.79]]. Mortality within 30-days of COVID-19 infection was similarly 33% lower with Vitamin D 3 and 25% lower with D 2 (D 3 HR = 0.67, [95% CI 0.59, 0.75]; D 2 HR = 0.75, [95% CI 0.55, 1.04]). We also find that after controlling for vitamin D blood levels, veterans receiving higher dosages of Vitamin D obtained greater benefits from supplementation than veterans receiving lower dosages. Veterans with Vitamin D blood levels between 0 and 19 ng/ml exhibited the largest decrease in COVID-19 infection following supplementation. Black veterans received greater associated COVID-19 risk reductions with supplementation than White veterans. As a safe, widely available, and affordable treatment, Vitamin D may help to reduce the severity of the COVID-19 pandemic. Vitamin D insufficiency and deficiency affect approximately half of the US population, with increased rates in people with darker skin, reduced sun exposure, people living in higher latitudes in the winter, nursing home residents, and healthcare workers 1 . Populations with low levels of Vitamin D have also experienced higher rates of COVID-19 [2] [3] [4] [5] [6] . Despite several studies pointing to an association between low levels of vitamin D and COVID-19 2-7 , limited information is available regarding the potential for supplementation with vitamin D to reduce the risk of COVID-19 infection. Expanding supplementation with vitamin D may present a new and unique opportunity to mitigate global infection rates, given that it is a widely available over-the-counter (OTC), inexpensive, and is associated with relatively few side effects. We conducted a large-scale pharmacoepidemiologic study of the association between vitamin D 3 and D 2 supplementation and the probability of COVID-19 infection and COVID-19 infection ending in mortality within 30-days in the Department of Veterans Administration (VA) in the United States. We also studied whether patient sex, race, vitamin D serum levels, and cumulative D 3 supplementation dosage modified the association.
Author contributions J.G. Wrote the manuscript, analyzed the data, planned the analysis, and reviewed the manuscript. E.N. planned the analysis and reviewed the manuscript. J.M. planned the analysis and reviewed the manuscript. D.M. planned the analysis and reviewed the manuscript. J.L. planned the analysis and reviewed the manuscript and obtained the data. V.F.. planned the analysis and reviewed the manuscript. R.G. Wrote the manuscript, planned the analysis, and reviewed the manuscript.
Competing interests Dr. DO Meltzer reported grants from the National Institutes of Health during the conduct of the study. Dr. JB Gibbons, Dr. J Lavigne, Dr. VC Fiedler, Dr. EC Norton, Dr. J McCullough, Dr. RD Gibbons have no conflicts to report.
Additional information
Supplementary Information The online version contains supplementary material available at https:// doi. org/ 10. 1038/ s41598-022-24053-4. Correspondence and requests for materials should be addressed to J.B.G. Reprints and permissions information is available at www.nature.com/reprints. Publisher's note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Akbar, Wibowo, Pranata, Setiabudiawan, Low serum 25-hydroxyvitamin D (Vitamin D) level is associated with susceptibility to COVID-19, severity, and mortality: A systematic review and meta-analysis, Front. Nutr
Break, Aberrant type 1 immunity drives susceptibility to mucosal fungal infections, Science
Cardone, Complement regulator CD46 temporally regulates cytokine production by conventional and unconventional T cells, Nat. Immunol
Castillo, Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2020.105751
Chauss, Autocrine Vitamin D signaling switches off pro-inflammatory programs of TH1 cells, Nat. Immunol, doi:10.1038/s41590-021-01080-3
Chen, Low vitamin D levels do not aggravate COVID-19 risk or death, and vitamin D supplementation does not improve outcomes in hospitalized patients with COVID-19: A meta-analysis and GRADE assessment of cohort studies and RCTs, Nutr. J, doi:10.1186/s12937-021-00744-y
Chiodini, Vitamin D status and SARS-CoV-2 infection and COVID-19 clinical outcomes, Front. Public Health, doi:10.3389/fpubh.2021.736665
Dror, Pre-infection 25-hydroxyvitamin D3 levels and association with severity of COVID-19 illness, PLoS ONE, doi:10.1371/journal.pone.0263069
Forrest, Stuhldreher, Prevalence and correlates of vitamin D deficiency in US adults, Nutr. Res, doi:10.1016/j.nutres.2010.12.001
Gazzinelli, In the absence of endogenous IL10, mice acutely infected with Toxoplasma gondii succumb to a lethal immune response dependent on CD4+ T cells and accomplished by overproduction of IL12, IFN gamma and TNF alpha, J. Immunol
Grove, Association between vitamin D supplementation or serum vitamin D level and susceptibility to SARS-CoV-2 infection or COVID-19 including clinical course, morbidity and mortality outcomes? A systematic review, BMJ Open, doi:10.1136/bmjopen-2020-043737
Israel, Assi Cicurel, Feldhamer, Dror, Giveon et al., The link between vitamin D deficiency and COVID-19 in a large population, doi:10.1101/2020.09.04.20188268
Kaufman, Niles, Kroll, Bi, Holick, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PLoS ONE, doi:10.1371/journal.pone.0239252
Loucera, Real world evidence of calcifediol or vitamin D prescription and mortality rate of COVID-19 in a retrospective cohort of hospitalized Andalusian patients, Sci. Rep, doi:10.1038/s41598-021-02701-5
Lucas, Longitudinal analyses reveal immunological misfiring in severe COVID-19, Nature
Maghbooli, Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection, PLoS ONE, doi:10.1371/journal.pone.0239799
Martineau, Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data, BMJ, doi:10.1136/bmj.i6583
Martín Giménez, Vitamin D deficiency in African Americans is associated with a high risk of severe disease and mortality by SARS-CoV-2, J. Hum. Hypertens, doi:10.1038/s41371-020-00398-z
Meltzer, Association of vitamin D status and other clinical characteristics with COVID-19 test results, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2020.19722
Meltzer, Best, Schram, Solway, Comment On Murai et al., Reanalysis suggests vitamin D decreased intensive care and mechanical ventilation use, JAMA
Meltzer, Best, Vokes, Association of vitamin D levels, race/ethnicity, and clinical characteristics with COVID-19 test results, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2021.4117
Merzon, Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: An Israeli population-based study, FEBS J, doi:10.1111/febs.15495
Murai, Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: A randomized clinical trial, JAMA, doi:10.1001/jama.2020.26848
Richie, Ortiz-Ospina, Beltekian, Mathieu, Hassel et al., Statistics and research-Coronavirus pandemic (COVID-19)
Sanghera, Sapkota, Aston, Blackett, Vitamin D status, gender differences, and cardiometabolic health disparities, Ann. Nutr. Metab, doi:10.1159/000458765
Sinkovits, Complement overactivation and consumption predicts in-hospital mortality in SARS-CoV-2 infection, Front. Immunol
Stroehlein, Vitamin D supplementation for the treatment of COVID-19: A living systematic review, Cochrane Database Syst. Rev, doi:10.1002/14651858.CD015043
West, Kolev, Kemper, Complement and the regulation of T cell responses, Annu. Rev. Immunol
Yan, SARS-CoV-2 drives JAK1/2-dependent local complement hyperactivation, Scientific Reports
DOI record:
{
"DOI": "10.1038/s41598-022-24053-4",
"ISSN": [
"2045-2322"
],
"URL": "http://dx.doi.org/10.1038/s41598-022-24053-4",
"abstract": "<jats:title>Abstract</jats:title><jats:p>Vitamin D deficiency has long been associated with reduced immune function that can lead to viral infection. Several studies have shown that Vitamin D deficiency is associated with increases the risk of infection with COVID-19. However, it is unknown if treatment with Vitamin D can reduce the associated risk of COVID-19 infection, which is the focus of this study. In the population of US veterans, we show that Vitamin D<jats:sub>2</jats:sub> and D<jats:sub>3</jats:sub> fills were associated with reductions in COVID-19 infection of 28% and 20%, respectively [(D<jats:sub>3</jats:sub> Hazard Ratio (HR) = 0.80, [95% CI 0.77, 0.83]), D<jats:sub>2</jats:sub> HR = 0.72, [95% CI 0.65, 0.79]]. Mortality within 30-days of COVID-19 infection was similarly 33% lower with Vitamin D<jats:sub>3</jats:sub> and 25% lower with D<jats:sub>2</jats:sub> (D<jats:sub>3</jats:sub> HR = 0.67, [95% CI 0.59, 0.75]; D<jats:sub>2</jats:sub> HR = 0.75, [95% CI 0.55, 1.04]). We also find that after controlling for vitamin D blood levels, veterans receiving higher dosages of Vitamin D obtained greater benefits from supplementation than veterans receiving lower dosages. Veterans with Vitamin D blood levels between 0 and 19 ng/ml exhibited the largest decrease in COVID-19 infection following supplementation. Black veterans received greater associated COVID-19 risk reductions with supplementation than White veterans. As a safe, widely available, and affordable treatment, Vitamin D may help to reduce the severity of the COVID-19 pandemic.</jats:p>",
"alternative-id": [
"24053"
],
"article-number": "19397",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "16 March 2022"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "9 November 2022"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "12 November 2022"
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1,
"value": "Dr. DO Meltzer reported grants from the National Institutes of Health during the conduct of the study. Dr. JB Gibbons, Dr. J Lavigne, Dr. VC Fiedler, Dr. EC Norton, Dr. J McCullough, Dr. RD Gibbons have no conflicts to report."
}
],
"author": [
{
"affiliation": [],
"family": "Gibbons",
"given": "Jason B.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Norton",
"given": "Edward C.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "McCullough",
"given": "Jeffrey S.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Meltzer",
"given": "David O.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lavigne",
"given": "Jill",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fiedler",
"given": "Virginia C.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gibbons",
"given": "Robert D.",
"sequence": "additional"
}
],
"container-title": "Scientific Reports",
"container-title-short": "Sci Rep",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2022,
11,
12
]
],
"date-time": "2022-11-12T13:29:40Z",
"timestamp": 1668259780000
},
"deposited": {
"date-parts": [
[
2022,
11,
12
]
],
"date-time": "2022-11-12T13:33:35Z",
"timestamp": 1668260015000
},
"indexed": {
"date-parts": [
[
2022,
11,
13
]
],
"date-time": "2022-11-13T05:48:59Z",
"timestamp": 1668318539351
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2022,
11,
12
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2022,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
11,
12
]
],
"date-time": "2022-11-12T00:00:00Z",
"timestamp": 1668211200000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
11,
12
]
],
"date-time": "2022-11-12T00:00:00Z",
"timestamp": 1668211200000
}
}
],
"link": [
{
"URL": "https://www.nature.com/articles/s41598-022-24053-4.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-022-24053-4",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-022-24053-4.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1038",
"published": {
"date-parts": [
[
2022,
11,
12
]
]
},
"published-online": {
"date-parts": [
[
2022,
11,
12
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1016/j.nutres.2010.12.001",
"author": "KY Forrest",
"doi-asserted-by": "publisher",
"first-page": "48",
"issue": "1",
"journal-title": "Nutr. Res.",
"key": "24053_CR1",
"unstructured": "Forrest, K. Y. & Stuhldreher, W. L. Prevalence and correlates of vitamin D deficiency in US adults. Nutr. Res. 31(1), 48–54. https://doi.org/10.1016/j.nutres.2010.12.001 (2011).",
"volume": "31",
"year": "2011"
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"author": "DO Meltzer",
"doi-asserted-by": "publisher",
"issue": "9",
"journal-title": "JAMA Netw. Open.",
"key": "24053_CR2",
"unstructured": "Meltzer, D. O. et al. Association of vitamin D status and other clinical characteristics with COVID-19 test results. JAMA Netw. Open. 3(9), e2019722. https://doi.org/10.1001/jamanetworkopen.2020.19722 (2020).",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0239799",
"author": "Z Maghbooli",
"doi-asserted-by": "publisher",
"issue": "9",
"journal-title": "PLoS ONE",
"key": "24053_CR3",
"unstructured": "Maghbooli, Z. et al. Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection. PLoS ONE 15(9), e0239799. https://doi.org/10.1371/journal.pone.0239799 (2020).",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0239252",
"author": "HW Kaufman",
"doi-asserted-by": "publisher",
"issue": "9",
"journal-title": "PLoS ONE",
"key": "24053_CR4",
"unstructured": "Kaufman, H. W., Niles, J. K., Kroll, M. H., Bi, C. & Holick, M. F. SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels. PLoS ONE 15(9), e0239252. https://doi.org/10.1371/journal.pone.0239252 (2020).",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1111/febs.15495",
"author": "E Merzon",
"doi-asserted-by": "publisher",
"first-page": "3693",
"issue": "17",
"journal-title": "FEBS J.",
"key": "24053_CR5",
"unstructured": "Merzon, E. et al. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: An Israeli population-based study. FEBS J. 287(17), 3693–3702. https://doi.org/10.1111/febs.15495 (2020).",
"volume": "287",
"year": "2020"
},
{
"DOI": "10.1101/2020.09.04.20188268",
"doi-asserted-by": "publisher",
"key": "24053_CR6",
"unstructured": "Israel, A., Assi Cicurel, A. A., Feldhamer, I., Dror, Y., Giveon, S. M., Gillis, D., Strich, D., & Lavie, G. The link between vitamin D deficiency and COVID-19 in a large population. medRxiv. Published online September 07, 2021. https://doi.org/10.1101/2020.09.04.20188268"
},
{
"DOI": "10.3389/fnut.2021.660420",
"author": "MR Akbar",
"doi-asserted-by": "publisher",
"journal-title": "Front. Nutr.",
"key": "24053_CR7",
"unstructured": "Akbar, M. R., Wibowo, A., Pranata, R. & Setiabudiawan, B. Low serum 25-hydroxyvitamin D (Vitamin D) level is associated with susceptibility to COVID-19, severity, and mortality: A systematic review and meta-analysis. Front. Nutr. 8, 660420 (2021).",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2021.663187",
"author": "G Sinkovits",
"doi-asserted-by": "publisher",
"journal-title": "Front. Immunol.",
"key": "24053_CR8",
"unstructured": "Sinkovits, G. et al. Complement overactivation and consumption predicts in-hospital mortality in SARS-CoV-2 infection. Front. Immunol. 12, 663187 (2021).",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1038/s41586-020-2588-y",
"author": "C Lucas",
"doi-asserted-by": "publisher",
"first-page": "463",
"journal-title": "Nature",
"key": "24053_CR9",
"unstructured": "Lucas, C. et al. Longitudinal analyses reveal immunological misfiring in severe COVID-19. Nature 584, 463–469 (2020).",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.1146/annurev-immunol-042617-053245",
"author": "EE West",
"doi-asserted-by": "publisher",
"first-page": "309",
"journal-title": "Annu. Rev. Immunol.",
"key": "24053_CR10",
"unstructured": "West, E. E., Kolev, M. & Kemper, C. Complement and the regulation of T cell responses. Annu. Rev. Immunol. 36, 309–338 (2018).",
"volume": "36",
"year": "2018"
},
{
"DOI": "10.1126/science.aay5731",
"author": "TJ Break",
"doi-asserted-by": "publisher",
"first-page": "eaay5731",
"journal-title": "Science",
"key": "24053_CR11",
"unstructured": "Break, T. J. et al. Aberrant type 1 immunity drives susceptibility to mucosal fungal infections. Science 371, eaay5731 (2021).",
"volume": "371",
"year": "2021"
},
{
"DOI": "10.1126/sciimmunol.abg0833",
"author": "B Yan",
"doi-asserted-by": "publisher",
"first-page": "eabg0833",
"journal-title": "Sci. Immunol.",
"key": "24053_CR12",
"unstructured": "Yan, B. et al. SARS-CoV-2 drives JAK1/2-dependent local complement hyperactivation. Sci. Immunol. 6, eabg0833 (2021).",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1038/ni.1917",
"author": "J Cardone",
"doi-asserted-by": "publisher",
"first-page": "862",
"journal-title": "Nat. Immunol.",
"key": "24053_CR13",
"unstructured": "Cardone, J. et al. Complement regulator CD46 temporally regulates cytokine production by conventional and unconventional T cells. Nat. Immunol. 11, 862–871 (2010).",
"volume": "11",
"year": "2010"
},
{
"author": "RT Gazzinelli",
"first-page": "798",
"journal-title": "J. Immunol.",
"key": "24053_CR14",
"unstructured": "Gazzinelli, R. T. et al. In the absence of endogenous IL10, mice acutely infected with Toxoplasma gondii succumb to a lethal immune response dependent on CD4+ T cells and accomplished by overproduction of IL12, IFN gamma and TNF alpha. J. Immunol. 157, 798–805 (1996).",
"volume": "157",
"year": "1996"
},
{
"DOI": "10.1038/s41590-021-01080-3",
"author": "D Chauss",
"doi-asserted-by": "publisher",
"journal-title": "Nat. Immunol.",
"key": "24053_CR15",
"unstructured": "Chauss, D. et al. Autocrine Vitamin D signaling switches off pro-inflammatory programs of TH1 cells. Nat. Immunol. https://doi.org/10.1038/s41590-021-01080-3 (2021).",
"year": "2021"
},
{
"DOI": "10.1136/bmj.i6583",
"author": "AR Martineau",
"doi-asserted-by": "publisher",
"journal-title": "BMJ",
"key": "24053_CR16",
"unstructured": "Martineau, A. R. et al. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ 356, i6583. https://doi.org/10.1136/bmj.i6583 (2017).",
"volume": "356",
"year": "2017"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"author": "M Entrenas Castillo",
"doi-asserted-by": "publisher",
"journal-title": "J. Steroid Biochem. Mol. Biol.",
"key": "24053_CR17",
"unstructured": "Entrenas Castillo, M. et al. Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study. J. Steroid Biochem. Mol. Biol. 203, 105751. https://doi.org/10.1016/j.jsbmb.2020.105751 (2020).",
"volume": "203",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.26848",
"author": "IH Murai",
"doi-asserted-by": "publisher",
"journal-title": "JAMA",
"key": "24053_CR18",
"unstructured": "Murai, I. H. et al. Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: A randomized clinical trial. JAMA https://doi.org/10.1001/jama.2020.26848 (2021).",
"year": "2021"
},
{
"key": "24053_CR19",
"unstructured": "Meltzer, D.O., Best, T., Schram, A., Solway, J. Comment on Murai, I.H., Fernandes, A.L., Sales, L.P., et al. Reanalysis suggests vitamin D decreased intensive care and mechanical ventilation use. JAMA (2021). Accessed March 21, 2021. Available at https://jamanetwork.com/journals/jama/fullarticle/2776738."
},
{
"DOI": "10.3389/fpubh.2021.736665",
"author": "I Chiodini",
"doi-asserted-by": "publisher",
"journal-title": "Front. Public Health.",
"key": "24053_CR20",
"unstructured": "Chiodini, I. et al. Vitamin D status and SARS-CoV-2 infection and COVID-19 clinical outcomes. Front. Public Health. 9, 736665. https://doi.org/10.3389/fpubh.2021.736665 (2021).",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1038/s41598-021-02701-5",
"author": "C Loucera",
"doi-asserted-by": "publisher",
"first-page": "23380",
"journal-title": "Sci. Rep.",
"key": "24053_CR21",
"unstructured": "Loucera, C. et al. Real world evidence of calcifediol or vitamin D prescription and mortality rate of COVID-19 in a retrospective cohort of hospitalized Andalusian patients. Sci. Rep. 11, 23380. https://doi.org/10.1038/s41598-021-02701-5 (2021).",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0263069",
"author": "AA Dror",
"doi-asserted-by": "publisher",
"issue": "2",
"journal-title": "PLoS ONE",
"key": "24053_CR22",
"unstructured": "Dror, A. A. et al. Pre-infection 25-hydroxyvitamin D3 levels and association with severity of COVID-19 illness. PLoS ONE 17(2), e0263069. https://doi.org/10.1371/journal.pone.0263069 (2022).",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.1002/14651858.CD015043",
"author": "JK Stroehlein",
"doi-asserted-by": "publisher",
"first-page": "CD015043",
"journal-title": "Cochrane Database Syst. Rev.",
"key": "24053_CR23",
"unstructured": "Stroehlein, J. K. et al. Vitamin D supplementation for the treatment of COVID-19: A living systematic review. Cochrane Database Syst. Rev. 5, CD015043. https://doi.org/10.1002/14651858.CD015043 (2021).",
"volume": "5",
"year": "2021"
},
{
"DOI": "10.1136/bmjopen-2020-043737",
"author": "A Grove",
"doi-asserted-by": "publisher",
"journal-title": "BMJ Open",
"key": "24053_CR24",
"unstructured": "Grove, A. et al. Association between vitamin D supplementation or serum vitamin D level and susceptibility to SARS-CoV-2 infection or COVID-19 including clinical course, morbidity and mortality outcomes? A systematic review. BMJ Open 11, e043737. https://doi.org/10.1136/bmjopen-2020-043737 (2021).",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1186/s12937-021-00744-y",
"author": "J Chen",
"doi-asserted-by": "publisher",
"first-page": "89",
"journal-title": "Nutr. J.",
"key": "24053_CR25",
"unstructured": "Chen, J. et al. Low vitamin D levels do not aggravate COVID-19 risk or death, and vitamin D supplementation does not improve outcomes in hospitalized patients with COVID-19: A meta-analysis and GRADE assessment of cohort studies and RCTs. Nutr. J. 20, 89. https://doi.org/10.1186/s12937-021-00744-y (2021).",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.1038/s41371-020-00398-z",
"author": "VM Martín Giménez",
"doi-asserted-by": "publisher",
"journal-title": "J. Hum. Hypertens.",
"key": "24053_CR26",
"unstructured": "Martín Giménez, V. M. et al. Vitamin D deficiency in African Americans is associated with a high risk of severe disease and mortality by SARS-CoV-2. J. Hum. Hypertens. https://doi.org/10.1038/s41371-020-00398-z (2020).",
"year": "2020"
},
{
"DOI": "10.1159/000458765",
"author": "DK Sanghera",
"doi-asserted-by": "publisher",
"first-page": "79",
"issue": "2",
"journal-title": "Ann. Nutr. Metab.",
"key": "24053_CR27",
"unstructured": "Sanghera, D. K., Sapkota, B. R., Aston, C. E. & Blackett, P. R. Vitamin D status, gender differences, and cardiometabolic health disparities. Ann. Nutr. Metab. 70(2), 79–87. https://doi.org/10.1159/000458765 (2017).",
"volume": "70",
"year": "2017"
},
{
"DOI": "10.1001/jamanetworkopen.2021.4117",
"author": "DO Meltzer",
"doi-asserted-by": "publisher",
"first-page": "14117",
"issue": "3",
"journal-title": "JAMA Netw. Open.",
"key": "24053_CR28",
"unstructured": "Meltzer, D. O., Best, T. J. & Vokes, Z. H. Association of vitamin D levels, race/ethnicity, and clinical characteristics with COVID-19 test results. JAMA Netw. Open. 4(3), 14117. https://doi.org/10.1001/jamanetworkopen.2021.4117 (2021).",
"volume": "4",
"year": "2021"
},
{
"key": "24053_CR29",
"unstructured": "Richie, H., Ortiz-Ospina, E., Beltekian, D., Mathieu, E., Hassel, J., Macdonald, B., Giattino, C., Appel, C., & Roser, M. Statistics and research—Coronavirus pandemic (COVID-19). Our World in Data. Accessed March 21, 2021. Available at https://ourworldindata.org/coronavirus."
},
{
"key": "24053_CR30",
"unstructured": "United States Department of Veterans Affairs. COVID-19 National Summary. Accessed October 3, 2021. Available at https://www.accesstocare.va.gov/Healthcare/COVID19NationalSummary."
}
],
"reference-count": 30,
"references-count": 30,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.nature.com/articles/s41598-022-24053-4"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": "Association between vitamin D supplementation and COVID-19 infection and mortality",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "12"
}
