Pre-infection 25-hydroxyvitamin D3 levels and association with severity of COVID-19 illness
et al., PLOS ONE, doi:10.1371/journal.pone.0263069, Jun 2021 (preprint)
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
This paper was retracted.
Dror et al., 7 Jun 2021, peer-reviewed, 18 authors.
Pre-infection 25-hydroxyvitamin D3 levels and association with severity of COVID-19 illness
PLOS ONE, doi:10.1371/journal.pone.0263069
Objective Studies have demonstrated a potential correlation between low vitamin D status and both an increased risk of infection with SARS-CoV-2 and poorer clinical outcomes. This retrospective study examines if, and to what degree, a relationship exists between pre-infection serum 25-hydroxyvitamin D (25(OH)D) level and disease severity and mortality due to SARS-CoV-2.
Participants The records of individuals admitted between April 7 th , 2020 and February 4 th , 2021 to the Galilee Medical Center (GMC) in Nahariya, Israel, with positive polymerase chain reaction (PCR) tests for SARS-CoV-2 (COVID-19) were searched for historical 25(OH)D levels measured 14 to 730 days prior to the positive PCR test.
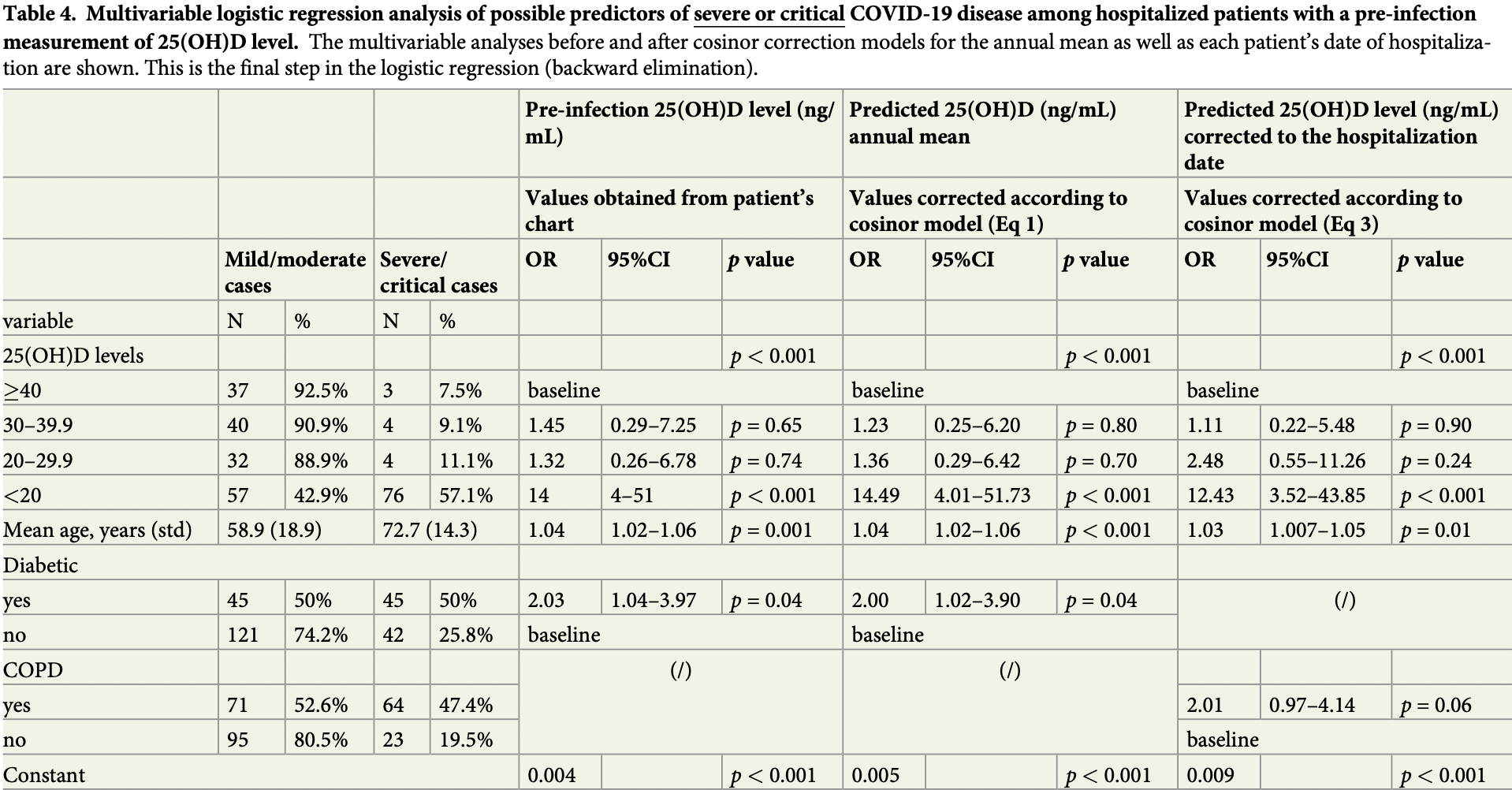
Design Patients admitted to GMC with COVID-19 were categorized according to disease severity and level of 25(OH)D. An association between pre-infection 25(OH)D levels, divided between four categories (deficient, insufficient, adequate, and high-normal), and COVID-19 severity was ascertained utilizing a multivariable regression analysis. To isolate the possible influence of the sinusoidal pattern of seasonal 25(OH)D changes throughout the year, a cosinor model was used.
Results Of 1176 patients admitted, 253 had records of a 25(OH)D level prior to COVID-19 infection. A lower vitamin D status was more common in patients with the severe or critical disease (<20 ng/mL [87.4%]) than in individuals with mild or moderate disease (<20 ng/mL [34.3%] p
References
Abu-Saad, Murad, Lubin, Freedman, Ziv et al., Jews and Arabs in the Same Region in Israel Exhibit Major Differences in Dietary Patterns, The Journal of Nutrition, doi:10.3945/jn.112.166611
Al Attia, Ibrahim, The high prevalence of vitamin D inadequacy and dress style of women in the sunny UAE, Archives of osteoporosis, doi:10.1007/s11657-012-0104-1
Al-Anouti, Mousa, Karras, Grant, Alhalwachi et al., Associations between Genetic Variants in the Vitamin D Metabolism Pathway and Severity of COVID-19 among UAE Residents, Nutrients, doi:10.3390/nu13113680
Bassil, Rahme, Hoteit, Fuleihan, Hypovitaminosis D in the Middle East and North Africa: Prevalence, risk factors and impact on outcomes, Dermato-endocrinology, doi:10.4161/derm.25111
Batieha, Khader, Jaddou, Hyassat, Batieha et al., Vitamin D status in Jordan: dress style and gender discrepancies, Annals of nutrition & metabolism, doi:10.1159/000323097
Bergman, Lindh, Bjo ¨rkhem-Bergman, Lindh, Vitamin D and Respiratory Tract Infections: A Systematic Review and Meta-Analysis of Randomized Controlled Trials, PLoS ONE, doi:10.1371/journal.pone.0065835
Bouillon, Genetic and environmental determinants of vitamin D status, The Lancet, doi:10.1016/S0140-6736%2810%2960635-6
Chakhtoura, Rahme, Chamoun, El-Hajj Fuleihan, Vitamin D in the Middle East and North Africa, Bone reports, doi:10.1016/j.bonr.2018.03.004
Charoenngam, Holick, Immunologic effects of vitamin d on human health and disease, Nutrients, doi:10.3390/nu12072097
Charoenngam, Shirvani, Reddy, Vodopivec, Apovian et al., Association of vitamin D status with hospital morbidity and mortality in adult hospitalized COVID-19 patients, Endocrine practice: official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists, doi:10.1016/j.eprac.2021.02.013
Cozier, Castro-Webb, Hochberg, Rosenberg, Albert et al., Lower serum 25(OH)D levels associated with higher risk of COVID-19 infection in U.S. Black women, PLOS ONE, doi:10.1371/journal.pone.0255132
Crowe, Steur, Allen, Appleby, Travis et al., Plasma concentrations of 25-hydroxyvitamin D in meat eaters, fish eaters, vegetarians and vegans: results from the EPIC-Oxford study, Public health nutrition, doi:10.1017/S1368980010002454
De Lucena, Da, Santos, De Lima, De et al., Mechanism of inflammatory response in associated comorbidities in COVID-19. Diabetes & Metabolic Syndrome, Clinical Research & Reviews, doi:10.1016/j.dsx.2020.05.025
Degerud, Bergen Open Research Archive: Vitamin D status and cardiovascular disease
Degerud, Hoff, Nygård, Strand, Nilsen et al., Cosinor modelling of seasonal variation in 25-hydroxyvitamin D concentrations in cardiovascular patients in Norway, European Journal of Clinical Nutrition, doi:10.1038/ejcn.2015.200
Elkum, Alkayal, Noronha, Ali, Melhem et al., Vitamin D Insufficiency in Arabs and South Asians Positively Associates with Polymorphisms in GC and CYP2R1 Genes, PLOS ONE, doi:10.1371/journal.pone.0113102
Evans, Lippman, Shining Light on the COVID-19 Pandemic: A Vitamin D Receptor Checkpoint in Defense of Unregulated Wound Healing, Cell Metabolism, doi:10.1016/j.cmet.2020.09.007
Grant, Lordan, Vitamin D for COVID-19 on Trial: An Update on Prevention and Therapeutic Application, Endocrine Practice, doi:10.1016/j.eprac.2021.10.001
Hobbs, Habib, Alromaihi, Idi, Parikh et al., Severe Vitamin D Deficiency in Arab-American Women Living in Dearborn, Michigan, Endocrine Practice, doi:10.4158/EP.15.1.35
Jain, Chaurasia, Sengar, Singh, Mahor et al., Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers, Scientific reports, doi:10.1038/s41598-020-77093-z
Jolliffe, Camargo, Sluyter, Aglipay, Aloia et al., Vitamin D supplementation to prevent acute respiratory infections: a systematic review and meta-analysis of aggregate data from randomised controlled trials, The Lancet Diabetes & Endocrinology, doi:10.1016/S2213-8587%2821%2900051-6
Kara, Ekiz, Ricci, Kara, Chang, Scientific Strabismus" or two related pandemics: coronavirus disease and vitamin D deficiency. The British journal of nutrition, doi:10.1017/S0007114520001749
Kaufman, Niles, Kroll, Bi, Holick, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PLOS ONE, doi:10.1371/journal.pone.0239252
Levis, Gomez, Jimenez, Veras, Ma et al., Vitamin D Deficiency and Seasonal Variation in an Adult South Florida Population, The Journal of Clinical Endocrinology & Metabolism, doi:10.1210/JC.2004-0746
Loucera, Peña-Chilet, Medina, Muñoyerro-Muñiz, Villegas et al., Real world evidence of calcifediol or vitamin D prescription and mortality rate of COVID-19 in a retrospective cohort of hospitalized Andalusian patients, Scientific Reports, doi:10.1038/s41598-021-02701-5
Ma, Nguyen, Yue, Ding, Drew et al., Associations between predicted vitamin D status, vitamin D intake, and risk of SARS-CoV-2 infection and Coronavirus Disease 2019 severity, The American Journal of Clinical Nutrition, doi:10.1093/AJCN/NQAB389
Maghbooli, Sahraian, Jamalimoghadamsiahkali, Asadi, Zarei et al., Treatment With 25-Hydroxyvitamin D3 (Calcifediol) Is Associated With a Reduction in the Blood Neutrophilto-Lymphocyte Ratio Marker of Disease Severity in Hospitalized Patients With COVID-19: A Pilot Multicenter, Randomized, Placebo-Controlled, Double-Blinded Clinical Trial, Endocrine Practice, doi:10.1016/j.eprac.2021.09.016
Major, Graubard, Dodd, Iwan, Alexander et al., Variability and Reproducibility of Circulating Vitamin D in a Nationwide U.S. Population, The Journal of Clinical Endocrinology and Metabolism, doi:10.1210/jc.2012-2643
Mark, Weldon, James, Grey, Bacon et al., The effects of seasonal variation of 25-hydroxyvitamin D on diagnosis of vitamin D insufficiency, The New Zealand medical journal
Meltzer, Best, Zhang, Vokes, Arora et al., Association of Vitamin D Status and Other Clinical Characteristics With COVID-19 Test Results, JAMA network open, doi:10.1001/jamanetworkopen.2020.19722
Merzon, Tworowski, Gorohovski, Vinker, Cohen et al., Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study, FEBS Journal, doi:10.1111/febs.15495
Mishal, Effects of different dress styles on vitamin D levels in healthy young Jordanian women. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA, doi:10.1007/s001980170021
Mora, Iwata, Von Andrian, Vitamin effects on the immune system: Vitamins A and D take centre stage, Nature Reviews Immunology, doi:10.1038/nri2378
Muhsen, Green, Soskolne, Neumark, Inequalities in non-communicable diseases between the major population groups in Israel: achievements and challenges, The Lancet, doi:10.1016/S0140-6736%2817%2930574-3
Oren, Shapira, Agmon-Levin, Kivity, Zafrir et al., Vitamin D insufficiency in a sunny environment: A demographic and seasonal analysis, The Israel Medical Association journal
Prietl, Treiber, Pieber, Amrein, Vitamin D and immune function, Nutrients, doi:10.3390/nu5072502
Rawat, Roy, Maitra, Shankar, Khanna et al., Vitamin D supplementation and COVID-19 treatment: A systematic review and meta-analysis, Diabetes & Metabolic Syndrome, doi:10.1016/J.DSX.2021.102189
Rhodes, Subramanian, Laird, Griffin, Kenny, Perspective: Vitamin D deficiency and COVID-19 severity-plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis, Journal of internal medicine, doi:10.1111/joim.13149
Rubin, Sorting Out Whether Vitamin D Deficiency Raises COVID-19 Risk, JAMA, doi:10.1001/jama.2020.24127
Sachs, Shoben, Levin, Robinson-Cohen, Hoofnagle et al., Estimating mean annual 25-hydroxyvitamin D concentrations from single measurements: the Multi-Ethnic Study of Atherosclerosis, The American Journal of Clinical Nutrition, doi:10.3945/ajcn.112.054502
Shoben, Kestenbaum, Levin, Hoofnagle, Psaty et al., Seasonal Variation in 25-Hydroxyvitamin D Concentrations in the Cardiovascular Health Study, American Journal of Epidemiology, doi:10.1093/aje/kwr258
Smolders, Van Den Ouweland, Geven, Pickkers, Kox, Letter to the Editor: Vitamin D deficiency in COVID-19: Mixing up cause and consequence, Metabolism, doi:10.1016/j.metabol.2020.154434
Wang, Jacobs, Mccullough, Rodriguez, Thun et al., Comparing Methods for Accounting for Seasonal Variability in a Biomarker When Only a Single Sample Is Available: Insights From Simulations Based on Serum 25-Hydroxyvitamin D, American Journal of Epidemiology, doi:10.1093/aje/kwp086
Woitge, Knothe, Witte, Schmidt-Gayk, Ziegler et al., Circannual Rhythms and Interactions of Vitamin D Metabolites, Parathyroid Hormone, and Biochemical Markers of Skeletal Homeostasis: A Prospective Study, Journal of Bone and Mineral Research, doi:10.1359/jbmr.2000.15.12.2443
Yancy, COVID-19 and African Americans, JAMA, doi:10.1001/jama.2020.6548
Zhao, Meng, Kumar, Wu, Huang et al., The impact of COPD and smoking history on the severity of COVID-19: A systemic review and meta-analysis, Journal of Medical Virology, doi:10.1002/jmv.25889
DOI record:
{
"DOI": "10.1371/journal.pone.0263069",
"ISSN": [
"1932-6203"
],
"URL": "http://dx.doi.org/10.1371/journal.pone.0263069",
"abstract": "<jats:sec id=\"sec001\">\n<jats:title>Objective</jats:title>\n<jats:p>Studies have demonstrated a potential correlation between low vitamin D status and both an increased risk of infection with SARS-CoV-2 and poorer clinical outcomes. This retrospective study examines if, and to what degree, a relationship exists between pre-infection serum 25-hydroxyvitamin D (25(OH)D) level and disease severity and mortality due to SARS-CoV-2.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec002\">\n<jats:title>Participants</jats:title>\n<jats:p>The records of individuals admitted between April 7<jats:sup>th</jats:sup>, 2020 and February 4<jats:sup>th</jats:sup>, 2021 to the Galilee Medical Center (GMC) in Nahariya, Israel, with positive polymerase chain reaction (PCR) tests for SARS-CoV-2 (COVID-19) were searched for historical 25(OH)D levels measured 14 to 730 days prior to the positive PCR test.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec003\">\n<jats:title>Design</jats:title>\n<jats:p>Patients admitted to GMC with COVID-19 were categorized according to disease severity and level of 25(OH)D. An association between pre-infection 25(OH)D levels, divided between four categories (deficient, insufficient, adequate, and high-normal), and COVID-19 severity was ascertained utilizing a multivariable regression analysis. To isolate the possible influence of the sinusoidal pattern of seasonal 25(OH)D changes throughout the year, a cosinor model was used.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec004\">\n<jats:title>Results</jats:title>\n<jats:p>Of 1176 patients admitted, 253 had records of a 25(OH)D level prior to COVID-19 infection. A lower vitamin D status was more common in patients with the severe or critical disease (<20 ng/mL [87.4%]) than in individuals with mild or moderate disease (<20 ng/mL [34.3%] <jats:italic>p</jats:italic> < 0.001). Patients with vitamin D deficiency (<20 ng/mL) were 14 times more likely to have severe or critical disease than patients with 25(OH)D ≥40 ng/mL (odds ratio [OR], 14; 95% confidence interval [CI], 4 to 51; <jats:italic>p</jats:italic> < 0.001).</jats:p>\n</jats:sec>\n<jats:sec id=\"sec005\">\n<jats:title>Conclusions</jats:title>\n<jats:p>Among hospitalized COVID-19 patients, pre-infection deficiency of vitamin D was associated with increased disease severity and mortality.</jats:p>\n</jats:sec>",
"author": [
{
"ORCID": "http://orcid.org/0000-0002-7178-6771",
"affiliation": [],
"authenticated-orcid": true,
"family": "Dror",
"given": "Amiel A.",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-6869-8626",
"affiliation": [],
"authenticated-orcid": true,
"family": "Morozov",
"given": "Nicole",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Daoud",
"given": "Amani",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Namir",
"given": "Yoav",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yakir",
"given": "Orly",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shachar",
"given": "Yair",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lifshitz",
"given": "Mark",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Segal",
"given": "Ella",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fisher",
"given": "Lior",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mizrachi",
"given": "Matti",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Eisenbach",
"given": "Netanel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rayan",
"given": "Doaa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gruber",
"given": "Maayan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bashkin",
"given": "Amir",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kaykov",
"given": "Edward",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Barhoum",
"given": "Masad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Edelstein",
"given": "Michael",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sela",
"given": "Eyal",
"sequence": "additional"
}
],
"container-title": "PLOS ONE",
"container-title-short": "PLoS ONE",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"www.plosone.org"
]
},
"created": {
"date-parts": [
[
2022,
2,
3
]
],
"date-time": "2022-02-03T18:54:53Z",
"timestamp": 1643914493000
},
"deposited": {
"date-parts": [
[
2022,
2,
3
]
],
"date-time": "2022-02-03T18:55:25Z",
"timestamp": 1643914525000
},
"editor": [
{
"affiliation": [],
"family": "Jin",
"given": "Dong-Yan",
"sequence": "first"
}
],
"indexed": {
"date-parts": [
[
2024,
3,
31
]
],
"date-time": "2024-03-31T18:58:30Z",
"timestamp": 1711911510781
},
"is-referenced-by-count": 62,
"issue": "2",
"issued": {
"date-parts": [
[
2022,
2,
3
]
]
},
"journal-issue": {
"issue": "2",
"published-online": {
"date-parts": [
[
2022,
2,
3
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
2,
3
]
],
"date-time": "2022-02-03T00:00:00Z",
"timestamp": 1643846400000
}
}
],
"link": [
{
"URL": "https://dx.plos.org/10.1371/journal.pone.0263069",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "340",
"original-title": [],
"page": "e0263069",
"prefix": "10.1371",
"published": {
"date-parts": [
[
2022,
2,
3
]
]
},
"published-online": {
"date-parts": [
[
2022,
2,
3
]
]
},
"publisher": "Public Library of Science (PLoS)",
"reference": [
{
"article-title": "Immunologic effects of vitamin d on human health and disease.",
"author": "N Charoenngam",
"first-page": "1",
"journal-title": "Nutrients.",
"key": "pone.0263069.ref001",
"year": "2020"
},
{
"DOI": "10.3390/nu5072502",
"article-title": "Vitamin D and immune function.",
"author": "B Prietl",
"doi-asserted-by": "crossref",
"first-page": "2502",
"journal-title": "Nutrients",
"key": "pone.0263069.ref002",
"year": "2013"
},
{
"DOI": "10.1016/j.bonr.2018.03.004",
"article-title": "Vitamin D in the Middle East and North Africa",
"author": "M Chakhtoura",
"doi-asserted-by": "crossref",
"first-page": "135",
"journal-title": "Bone reports",
"key": "pone.0263069.ref003",
"volume": "8",
"year": "2018"
},
{
"DOI": "10.1159/000323097",
"article-title": "Vitamin D status in Jordan: dress style and gender discrepancies.",
"author": "A Batieha",
"doi-asserted-by": "crossref",
"first-page": "10",
"journal-title": "Annals of nutrition & metabolism",
"key": "pone.0263069.ref004",
"volume": "58",
"year": "2011"
},
{
"DOI": "10.1371/journal.pone.0065835",
"article-title": "Vitamin D and Respiratory Tract Infections: A Systematic Review and Meta-Analysis of Randomized Controlled Trials.",
"author": "P Bergman",
"doi-asserted-by": "crossref",
"first-page": "e65835",
"journal-title": "PLoS ONE.",
"key": "pone.0263069.ref005",
"year": "2013"
},
{
"DOI": "10.1016/S2213-8587(21)00051-6",
"article-title": "Vitamin D supplementation to prevent acute respiratory infections: a systematic review and meta-analysis of aggregate data from randomised controlled trials.",
"author": "DA Jolliffe",
"doi-asserted-by": "crossref",
"first-page": "276",
"journal-title": "The Lancet Diabetes & Endocrinology.",
"key": "pone.0263069.ref006",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1111/joim.13149",
"article-title": "Perspective: Vitamin D deficiency and COVID-19 severity—plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis",
"author": "JM Rhodes",
"doi-asserted-by": "crossref",
"first-page": "97",
"journal-title": "Journal of internal medicine",
"key": "pone.0263069.ref007",
"volume": "289",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"article-title": "Association of Vitamin D Status and Other Clinical Characteristics With COVID-19 Test Results.",
"author": "DO Meltzer",
"doi-asserted-by": "crossref",
"first-page": "e2019722",
"journal-title": "JAMA network open",
"key": "pone.0263069.ref008",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1111/febs.15495",
"article-title": "vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study",
"author": "E Merzon",
"doi-asserted-by": "crossref",
"first-page": "3693",
"issue": "OH",
"journal-title": "FEBS Journal",
"key": "pone.0263069.ref009",
"volume": "287",
"year": "2020"
},
{
"DOI": "10.1038/s41598-020-77093-z",
"article-title": "Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers.",
"author": "A Jain",
"doi-asserted-by": "crossref",
"first-page": "20191",
"journal-title": "Scientific reports.",
"key": "pone.0263069.ref010",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1017/S0007114520001749",
"article-title": "“Scientific Strabismus” or two related pandemics: coronavirus disease and vitamin D deficiency.",
"author": "M Kara",
"doi-asserted-by": "crossref",
"first-page": "736",
"journal-title": "The British journal of nutrition",
"key": "pone.0263069.ref011",
"volume": "124",
"year": "2020"
},
{
"DOI": "10.1210/jc.2012-2643",
"article-title": "Variability and Reproducibility of Circulating Vitamin D in a Nationwide U.S. Population",
"author": "JM Major",
"doi-asserted-by": "crossref",
"first-page": "97",
"journal-title": "The Journal of Clinical Endocrinology and Metabolism",
"key": "pone.0263069.ref012",
"volume": "98",
"year": "2013"
},
{
"DOI": "10.1093/aje/kwp086",
"article-title": "Comparing Methods for Accounting for Seasonal Variability in a Biomarker When Only a Single Sample Is Available: Insights From Simulations Based on Serum 25-Hydroxyvitamin D",
"author": "Y Wang",
"doi-asserted-by": "crossref",
"first-page": "88",
"journal-title": "American Journal of Epidemiology",
"key": "pone.0263069.ref013",
"volume": "170",
"year": "2009"
},
{
"DOI": "10.1093/aje/kwr258",
"article-title": "Seasonal Variation in 25-Hydroxyvitamin D Concentrations in the Cardiovascular Health Study",
"author": "AB Shoben",
"doi-asserted-by": "crossref",
"first-page": "1363",
"journal-title": "American Journal of Epidemiology",
"key": "pone.0263069.ref014",
"volume": "174",
"year": "2011"
},
{
"article-title": "The effects of seasonal variation of 25-hydroxyvitamin D on diagnosis of vitamin D insufficiency",
"author": "Mark J Bolland",
"first-page": "63",
"journal-title": "The New Zealand medical journal",
"key": "pone.0263069.ref015",
"volume": "121",
"year": "2008"
},
{
"DOI": "10.3945/ajcn.112.054502",
"article-title": "Estimating mean annual 25-hydroxyvitamin D concentrations from single measurements: the Multi-Ethnic Study of Atherosclerosis",
"author": "MC Sachs",
"doi-asserted-by": "crossref",
"first-page": "1243",
"journal-title": "The American Journal of Clinical Nutrition",
"key": "pone.0263069.ref016",
"volume": "97",
"year": "2013"
},
{
"key": "pone.0263069.ref017",
"unstructured": "Degerud E. Bergen Open Research Archive: Vitamin D status and cardiovascular disease. Observational studies in patients who underwent coronary angiography. In: PhD thesis [Internet]. [cited 10 Sep 2021]. Available: https://bora.uib.no/bora-xmlui/handle/1956/12732"
},
{
"article-title": "Cosinor modelling of seasonal variation in 25-hydroxyvitamin D concentrations in cardiovascular patients in Norway",
"author": "E Degerud",
"first-page": "517",
"journal-title": "European Journal of Clinical Nutrition 2016 70:4.",
"key": "pone.0263069.ref018",
"volume": "70",
"year": "2015"
},
{
"DOI": "10.1359/jbmr.2000.15.12.2443",
"article-title": "Circannual Rhythms and Interactions of Vitamin D Metabolites, Parathyroid Hormone, and Biochemical Markers of Skeletal Homeostasis: A Prospective Study",
"author": "HW Woitge",
"doi-asserted-by": "crossref",
"first-page": "2443",
"journal-title": "Journal of Bone and Mineral Research",
"key": "pone.0263069.ref019",
"volume": "15",
"year": "2000"
},
{
"DOI": "10.1210/jc.2004-0746",
"article-title": "Vitamin D Deficiency and Seasonal Variation in an Adult South Florida Population.",
"author": "S Levis",
"doi-asserted-by": "crossref",
"first-page": "1557",
"journal-title": "The Journal of Clinical Endocrinology & Metabolism.",
"key": "pone.0263069.ref020",
"volume": "90",
"year": "2005"
},
{
"DOI": "10.1038/nri2378",
"article-title": "Vitamin effects on the immune system: Vitamins A and D take centre stage",
"author": "JR Mora",
"doi-asserted-by": "crossref",
"first-page": "685",
"journal-title": "Nature Reviews Immunology",
"key": "pone.0263069.ref021",
"year": "2008"
},
{
"DOI": "10.1016/j.dsx.2020.05.025",
"article-title": "Mechanism of inflammatory response in associated comorbidities in COVID-19.",
"author": "TMC de Lucena",
"doi-asserted-by": "crossref",
"first-page": "597",
"journal-title": "Diabetes & Metabolic Syndrome: Clinical Research & Reviews.",
"key": "pone.0263069.ref022",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2020.09.007",
"article-title": "Shining Light on the COVID-19 Pandemic: A Vitamin D Receptor Checkpoint in Defense of Unregulated Wound Healing.",
"author": "RM Evans",
"doi-asserted-by": "crossref",
"first-page": "704",
"journal-title": "Cell Metabolism",
"key": "pone.0263069.ref023",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1016/j.metabol.2020.154434",
"article-title": "Letter to the Editor: Vitamin D deficiency in COVID-19: Mixing up cause and consequence",
"author": "J Smolders",
"doi-asserted-by": "crossref",
"first-page": "154434",
"journal-title": "Metabolism",
"key": "pone.0263069.ref024",
"volume": "115",
"year": "2021"
},
{
"article-title": "Association of vitamin D status with hospital morbidity and mortality in adult hospitalized COVID-19 patients.",
"author": "N Charoenngam",
"journal-title": "Endocrine practice: official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists",
"key": "pone.0263069.ref025",
"year": "2021"
},
{
"DOI": "10.4161/derm.25111",
"article-title": "Hypovitaminosis D in the Middle East and North Africa: Prevalence, risk factors and impact on outcomes.",
"author": "D Bassil",
"doi-asserted-by": "crossref",
"first-page": "274",
"journal-title": "Dermato-endocrinology.",
"key": "pone.0263069.ref026",
"volume": "5",
"year": "2013"
},
{
"DOI": "10.4158/EP.15.1.35",
"article-title": "Severe Vitamin D Deficiency in Arab-American Women Living in Dearborn, Michigan.",
"author": "RD Hobbs",
"doi-asserted-by": "crossref",
"first-page": "35",
"journal-title": "Endocrine Practice",
"key": "pone.0263069.ref027",
"volume": "15",
"year": "2009"
},
{
"DOI": "10.1016/S0140-6736(10)60635-6",
"article-title": "Genetic and environmental determinants of vitamin D status.",
"author": "R Bouillon",
"doi-asserted-by": "crossref",
"first-page": "148",
"journal-title": "The Lancet",
"key": "pone.0263069.ref028",
"volume": "376",
"year": "2010"
},
{
"DOI": "10.1371/journal.pone.0113102",
"article-title": "Vitamin D Insufficiency in Arabs and South Asians Positively Associates with Polymorphisms in GC and CYP2R1 Genes.",
"author": "N Elkum",
"doi-asserted-by": "crossref",
"first-page": "e113102",
"journal-title": "PLOS ONE.",
"key": "pone.0263069.ref029",
"volume": "9",
"year": "2014"
},
{
"DOI": "10.3390/nu13113680",
"article-title": "Associations between Genetic Variants in the Vitamin D Metabolism Pathway and Severity of COVID-19 among UAE Residents.",
"author": "F Al-Anouti",
"doi-asserted-by": "crossref",
"first-page": "3680",
"journal-title": "Nutrients",
"key": "pone.0263069.ref030",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1007/s001980170021",
"article-title": "Effects of different dress styles on vitamin D levels in healthy young Jordanian women",
"author": "AA Mishal",
"doi-asserted-by": "crossref",
"first-page": "931",
"journal-title": "Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA",
"key": "pone.0263069.ref031",
"volume": "12",
"year": "2001"
},
{
"DOI": "10.1007/s11657-012-0104-1",
"article-title": "The high prevalence of vitamin D inadequacy and dress style of women in the sunny UAE.",
"author": "HM al Attia",
"doi-asserted-by": "crossref",
"first-page": "307",
"journal-title": "Archives of osteoporosis.",
"key": "pone.0263069.ref032",
"volume": "7",
"year": "2012"
},
{
"article-title": "Vitamin D insufficiency in a sunny environment: A demographic and seasonal analysis.",
"author": "Y Oren",
"first-page": "751",
"journal-title": "The Israel Medical Association journal: IMAJ.",
"key": "pone.0263069.ref033",
"volume": "12",
"year": "2010"
},
{
"article-title": "Associations between predicted vitamin D status, vitamin D intake, and risk of SARS-CoV-2 infection and Coronavirus Disease 2019 severity.",
"author": "W Ma",
"journal-title": "The American Journal of Clinical Nutrition",
"key": "pone.0263069.ref034",
"year": "2021"
},
{
"DOI": "10.3945/jn.112.166611",
"article-title": "Jews and Arabs in the Same Region in Israel Exhibit Major Differences in Dietary Patterns",
"author": "K Abu-Saad",
"doi-asserted-by": "crossref",
"first-page": "2175",
"journal-title": "The Journal of Nutrition",
"key": "pone.0263069.ref035",
"volume": "142",
"year": "2012"
},
{
"DOI": "10.1017/S1368980010002454",
"article-title": "Plasma concentrations of 25-hydroxyvitamin D in meat eaters, fish eaters, vegetarians and vegans: results from the EPIC-Oxford study.",
"author": "FL Crowe",
"doi-asserted-by": "crossref",
"first-page": "340",
"journal-title": "Public health nutrition.",
"key": "pone.0263069.ref036",
"volume": "14",
"year": "2011"
},
{
"DOI": "10.1016/S0140-6736(17)30574-3",
"article-title": "Inequalities in non-communicable diseases between the major population groups in Israel: achievements and challenges",
"author": "K Muhsen",
"doi-asserted-by": "crossref",
"first-page": "2531",
"journal-title": "The Lancet",
"key": "pone.0263069.ref037",
"volume": "389",
"year": "2017"
},
{
"DOI": "10.1371/journal.pone.0239252",
"article-title": "SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels.",
"author": "HW Kaufman",
"doi-asserted-by": "crossref",
"first-page": "e0239252",
"journal-title": "PLOS ONE",
"key": "pone.0263069.ref038",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0255132",
"article-title": "Lower serum 25(OH)D levels associated with higher risk of COVID-19 infection in U.S. Black women.",
"author": "YC Cozier",
"doi-asserted-by": "crossref",
"first-page": "e0255132",
"journal-title": "PLOS ONE",
"key": "pone.0263069.ref039",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.6548",
"article-title": "COVID-19 and African Americans.",
"author": "CW Yancy",
"doi-asserted-by": "crossref",
"first-page": "1891",
"journal-title": "JAMA",
"key": "pone.0263069.ref040",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1002/jmv.25889",
"article-title": "The impact of COPD and smoking history on the severity of COVID-19: A systemic review and meta-analysis",
"author": "Q Zhao",
"doi-asserted-by": "crossref",
"first-page": "1915",
"journal-title": "Journal of Medical Virology",
"key": "pone.0263069.ref041",
"volume": "92",
"year": "2020"
},
{
"DOI": "10.1016/j.eprac.2021.10.001",
"article-title": "Vitamin D for COVID-19 on Trial: An Update on Prevention and Therapeutic Application",
"author": "WB Grant",
"doi-asserted-by": "crossref",
"first-page": "1266",
"journal-title": "Endocrine Practice",
"key": "pone.0263069.ref042",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2021.102189",
"article-title": "“Vitamin D supplementation and COVID-19 treatment: A systematic review and meta-analysis.”",
"author": "D Rawat",
"doi-asserted-by": "crossref",
"first-page": "102189",
"journal-title": "Diabetes & Metabolic Syndrome: Clinical Research & Reviews.",
"key": "pone.0263069.ref043",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1016/j.eprac.2021.09.016",
"article-title": "Treatment With 25-Hydroxyvitamin D3 (Calcifediol) Is Associated With a Reduction in the Blood Neutrophil-to-Lymphocyte Ratio Marker of Disease Severity in Hospitalized Patients With COVID-19: A Pilot Multicenter, Randomized, Placebo-Controlled, Double-Blinded Clinical Trial.",
"author": "Z Maghbooli",
"doi-asserted-by": "crossref",
"first-page": "1242",
"journal-title": "Endocrine Practice.",
"key": "pone.0263069.ref044",
"volume": "27",
"year": "2021"
},
{
"article-title": "Real world evidence of calcifediol or vitamin D prescription and mortality rate of COVID-19 in a retrospective cohort of hospitalized Andalusian patients.",
"author": "C Loucera",
"first-page": "1",
"journal-title": "Scientific Reports 2021 11",
"key": "pone.0263069.ref045",
"volume": "11",
"year": "2021"
},
{
"article-title": "Sorting Out Whether Vitamin D Deficiency Raises COVID-19 Risk.",
"author": "R. Rubin",
"journal-title": "JAMA",
"key": "pone.0263069.ref046",
"year": "2021"
}
],
"reference-count": 46,
"references-count": 46,
"relation": {
"has-preprint": [
{
"asserted-by": "object",
"id": "10.1101/2021.06.04.21258358",
"id-type": "doi"
}
]
},
"resource": {
"primary": {
"URL": "https://dx.plos.org/10.1371/journal.pone.0263069"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": "Pre-infection 25-hydroxyvitamin D3 levels and association with severity of COVID-19 illness",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1371/journal.pone.corrections_policy",
"volume": "17"
}
