Associations between predicted vitamin D status, vitamin D intake, and risk of SARS-CoV-2 infection and Coronavirus Disease 2019 severity
et al., The American Journal of Clinical Nutrition, doi:10.1093/ajcn/nqab389, Dec 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
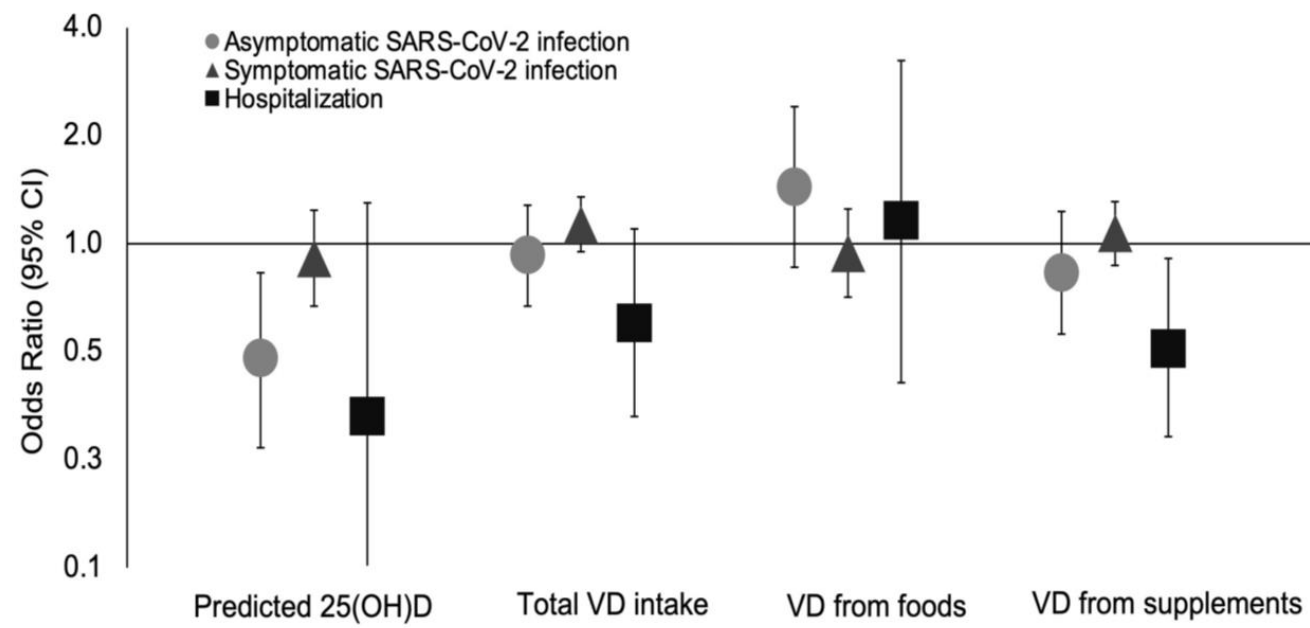
Analysis of 39,915 patients with 1,768 COVID+ cases based on surveys in the Nurses' Health Study II, showing higher predicted vitamin D levels associated with lower risk of COVID-19 cases. There was significantly lower risk of hospitalization with vitamin D supplementation (≥400 IU/d), but no significant differences for cases based on supplementation.
This is the 60th of 135 COVID-19 controlled studies for vitamin D, which collectively show efficacy with p<0.0000000001.
40 studies are RCTs, which show efficacy with p=0.0000001.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
Study covers sunlight and vitamin D.
|
risk of hospitalization, 49.0% lower, OR 0.51, p = 0.04, treatment 26,605, control 12,710, adjusted per study, supplementation ≥400 IU/day, model 3, supplemental table 3, multivariable, RR approximated with OR.
|
|
risk of symptomatic case, 7.0% higher, OR 1.07, p = 0.25, treatment 7,895, control 31,420, adjusted per study, supplementation ≥2000 IU/day vs. <400 IU/day, model 3, supplemental table 3, multivariable, RR approximated with OR.
|
|
risk of case, 17.0% lower, OR 0.83, p = 0.07, treatment 7,895, control 31,420, adjusted per study, supplementation ≥2000 IU/day vs. <400 IU/day, model 3, supplemental table 3, multivariable, RR approximated with OR.
|
|
risk of hospitalization, 67.0% lower, OR 0.33, p = 0.15, high D levels 7,893, low D levels 7,823, adjusted per study, highest quintile vs. lowest quintile predicted vitamin D levels, model 3, supplemental table 3, multivariable, RR approximated with OR, outcome based on serum levels.
|
|
risk of symptomatic case, 9.0% lower, OR 0.91, p = 0.52, high D levels 7,893, low D levels 7,823, adjusted per study, highest quintile vs. lowest quintile predicted vitamin D levels, model 3, supplemental table 3, multivariable, RR approximated with OR, outcome based on serum levels.
|
|
risk of case, 52.0% lower, OR 0.48, p = 0.01, high D levels 7,893, low D levels 7,823, adjusted per study, highest quintile vs. lowest quintile predicted vitamin D levels, model 3, supplemental table 3, multivariable, RR approximated with OR, outcome based on serum levels.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Ma et al., 3 Dec 2021, retrospective, USA, peer-reviewed, 16 authors, study period May 2020 - March 2021, dosage varies.
Contact: achan@mgh.harvard.edu.
Associations between predicted vitamin D status, vitamin D intake, and risk of SARS-CoV-2 infection and Coronavirus Disease 2019 severity
doi:10.1093/ajcn/nqab389/6448988
Background: Vitamin D may have a role in immune responses to viral infections. However, data on the association between vitamin D and SARS-CoV-2 infection and Coronavirus Disease 2019 (COVID-19) severity have been limited and inconsistent. Objective: We examined the associations of predicted vitamin D status and intake with risk of SARS-CoV-2 infection and COVID-19 severity. Design: We used data from periodic surveys (May 2020 to March 2021) within the Nurses' Health Study II. Among 39,315 participants, 1,768 reported a positive test for SARS-CoV-2 infection. Usual vitamin D intake from foods and supplements were measured using a semi-quantitative, pre-pandemic food frequency questionnaire in 2015. Predicted 25-hydroxyvitamin D [25(OH)D] levels were calculated based on a previously validated model including dietary and supplementary vitamin D intake, ultraviolet-B (UVB), and other behavioral predictors of vitamin D status. Results: Higher predicted 25(OH)D levels, but not vitamin D intake, were associated with a lower risk of SARS-CoV-2 infection. Comparing participants in the highest quintile of predicted 25(OH)D levels to the lowest, the multivariable-adjusted odds ratio was 0.76 (95% CI: 0.58, 0.99; P-trend=0.04). Participants in the highest quartile of UVB (OR: 0.76; 95% CI: 0.66, 0.87; P-trend=0.002) and UVA (OR: 0.76; 95% CI: 0.66, 0.88; P-trend<0.001) also had lower risk of SARS-CoV-2 infection compared
93 Logistic regression models were used in the analysis. The number of participants included in the analysis was 39,315, and the number of participants who reported a positive SARS-CoV-2 infection was 1,768. Model 1 was adjusted for age, white race, smoking pack-years (0, 0.1-10.0, 10.1-20.0, >20.0), and the Alternate Healthy Eating Index (quintiles). Vitamin D intakes from foods and supplements were mutually adjusted. Model 2 was further adjusted for body mass index (<22.5, 22.5-24.9, 25.0-27.4, 27.5-29.9, 30-34.9, ≥35.0 kg/m 2 ), physical activity (quintiles), and alcohol intake (0, 0.1-5.0, 5.1-10.0, >10 g/d). Model 3 was further adjusted for being a frontline healthcare worker, chronic comorbidities including hypertension, hypercholesterolemia, diabetes, heart disease, cancer, and asthma, and 2010 census tract median income (quintiles). P-trend was evaluated using the median value in each category as a continuous variable. Abbreviations: 25(OH)D, 25-hydroxyvitamin D. .001 Logistic regression models were used in the analysis. The number of participants included in the analysis was 39,315, and the number of participants who reported a positive SARS-CoV-2 infection was 1,768. Model 1 was adjusted for age, white race, smoking pack-years (0, 0.1-10.0, 10.1-20.0, >20.0), and the Alternate Healthy Eating Index (quintiles). Model 2 was further adjusted for body mass index (<22.5, 22.5-24.9, 25.0-27.4, 27.5-29.9, 30-34.9, ≥35.0 kg/m 2 ), physical activity..
References
Age, None
Ali, Role of vitamin D in preventing of COVID-19 infection, progression and severity, J Infect Public Health, doi:10.1016/j.jiph.2020.06.021
Ananthakrishnan, Khalili, Higuchi, Bao, Korzenik et al., Higher predicted vitamin D status is associated with reduced risk of Crohn's disease, Gastroenterology, doi:10.1053/j.gastro.2011.11.040
Annweiler, Corvaisier, Gautier, Dubee, Legrand et al., Vitamin D Supplementation Associated to Better Survival in Hospitalized Frail Elderly COVID-19 Patients: The GERIA-COVID Quasi-Experimental Study, Nutrients, doi:10.3390/nu12113377
Aranow, Vitamin D and the immune system, J Investig Med, doi:10.2310/JIM.0b013e31821b8755
Bennouar, Cherif, Kessira, Bennouar, Abdi, Vitamin D Deficiency and Low Serum Calcium as Predictors of Poor Prognosis in Patients with Severe COVID-19, J Am Coll Nutr, doi:10.1080/07315724.2020.1856013
Bertone-Johnson, Hankinson, Bendich, Johnson, Willett et al., Calcium and vitamin D intake and risk of incident premenstrual syndrome, Arch Intern Med, doi:10.1001/archinte.165.11.1246
Bertrand, Chang, Abel, Zhang, Spiegelman et al., Sunlight exposure, vitamin D, and risk of non-Hodgkin lymphoma in the Nurses' Health Study, Cancer Causes Control, doi:10.1007/s10552-011-9849-x
Bertrand, Giovannucci, Liu, Malspeis, Eliassen et al., Determinants of plasma 25-hydroxyvitamin D and development of prediction models in three US cohorts, Br J Nutr, doi:10.1017/S0007114511007409
Bowe, Xie, Gibson, Cai, Van Donkelaar et al., Ambient fine particulate matter air pollution and the risk of hospitalization among COVID-19 positive individuals: Cohort study, Environ Int, doi:10.1016/j.envint.2021.106564
Carleton, Cornetet, Huybers, Meng, Proctor, Global evidence for ultraviolet radiation decreasing COVID-19 growth rates, Proc Natl Acad Sci U S A, doi:10.1073/pnas.2012370118
Castillo, Costa, Barrios, Diaz, Miranda et al., Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2020.105751
Cherrie, Clemens, Colandrea, Feng, Webb et al., Ultraviolet A radiation and COVID-19 deaths in the USA with replication studies in England and Italy, Br J Dermatol, doi:10.1111/bjd.20093
Choi, Tuel, Eltahir, On the Environmental Determinants of COVID-19 Seasonality, Geohealth, doi:10.1029/2021GH000413
Cozier, Castro-Webb, Hochberg, Rosenberg, Albert et al., Lower serum 25(OH)D levels associated with higher risk of COVID-19 infection in U.S. Black women, PLoS One, doi:10.1371/journal.pone.0255132
Ding, Rocheleau, Boiano, Kang, Brcene et al., American Frontline Healthcare Personnel's Access to and Use of Personal Protective Equipment Early in the Coronavirus Disease
Durrleman, Simon, Flexible regression models with cubic splines, Stat Med, doi:10.1002/sim.4780080504
Fears, Bird, Dt, Sagebiel, Gail et al., Average midrange ultraviolet radiation flux and time outdoors predict melanoma risk, Cancer Res
Fuchs, Yuan, Sato, Niedzwiecki, Ye et al., Predicted vitamin D status and colon cancer recurrence and mortality in CALGB 89803 (Alliance), Ann Oncol, doi:10.1093/annonc/mdx109
Giovannucci, Liu, Rimm, Hollis, Fuchs et al., Prospective study of predictors of vitamin D status and cancer incidence and mortality in men, J Natl Cancer Inst, doi:10.1093/jnci/djj101
Hernandez, Nan, Fernandez-Ayala, Garcia-Unzueta, Hernandez-Hernandez et al., Vitamin D Status in Hospitalized Patients with SARS-CoV-2 Infection, J Clin Endocrinol Metab, doi:10.1210/clinem/dgaa733
Holick, Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease, Am J Clin Nutr, doi:10.1093/ajcn/80.6.1678S
Jude, Ling, Allcock, Yeap, Pappachan, Vitamin D deficiency is associated with higher hospitalisation risk from COVID-19: a retrospective case-control study, J Clin Endocrinol Metab, doi:10.1210/clinem/dgab439
Kaufman, Niles, Kroll, Bi, Holick, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PLoS One, doi:10.1371/journal.pone.0239252
Lee, Ma, Sikavi, Drew, Nguyen et al., Cancer and Risk of COVID-19 Through a General Community Survey, Oncologist, doi:10.1634/theoncologist.2020-0572
Lo, Nguyen, Drew, Graham, Warner et al., Racial and ethnic determinants of Covid-19 risk, medRxiv, doi:10.1101/2020.06.18.20134742
Louca, Murray, Klaser, Graham, Mazidi et al., Dietary supplements during the COVID-19 pandemic: insights from 1.4M users of the COVID Symptom Study app -a longitudinal app-based community survey, medRxiv, doi:10.1101/2020.11.27.20239087
Luo, Liao, Shen, Li, Cheng, Vitamin D Deficiency Is Inversely Associated with COVID-19 Incidence and Disease Severity in Chinese People, J Nutr, doi:10.1093/jn/nxaa332
Ma, Zhou, Heianza, Qi, Habitual use of vitamin D supplements and risk of coronavirus disease 2019 (COVID-19) infection: a prospective study in UK Biobank, Am J Clin Nutr, doi:10.1093/ajcn/nqaa381
Manson, Bassuk, Commentary. Eliminating vitamin D deficiency during the COVID-19 pandemic: A call to action, Metabolism, doi:10.1016/j.metabol.2020.154322
Martineau, Forouhi, Vitamin D for COVID-19: a case to answer?, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30268-0
Meltzer, Best, Zhang, Vokes, Arora et al., Association of Vitamin D Levels, Race/Ethnicity, and Clinical Characteristics With COVID-19 Test Results, JAMA Netw Open, doi:10.1001/jamanetworkopen.2021.4117
Meltzer, Best, Zhang, Vokes, Arora et al., Association of Vitamin D Status and Other Clinical Characteristics With COVID-19 Test Results, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.19722
Merzon, Tworowski, Gorohovski, Vinker, Cohen et al., Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study, FEBS J, doi:10.1111/febs.15495
Moozhipurath, Kraft, Skiera, Evidence of protective role of Ultraviolet-B (UVB) radiation in reducing COVID-19 deaths, Sci Rep, doi:10.1038/s41598-020-74825-z
Murai, Fernandes, Sales, Pinto, Goessler et al., Effect of a Single High Dose of Vitamin D3 on Hospital Length of Stay in Patients With Moderate to Severe COVID-19: A Randomized Clinical Trial, JAMA, doi:10.1001/jama.2020.26848
Ng, Wolpin, Meyerhardt, Wu, Chan et al., Prospective study of predictors of vitamin D status and survival in patients with colorectal cancer, Br J Cancer, doi:10.1038/sj.bjc.6605262
Oristrell, Oliva, Casado, Subirana, Dominguez et al., Vitamin D supplementation and COVID-19 risk: a population-based, cohort study, J Endocrinol Invest, doi:10.1007/s40618-021-01639-9
Pal, Banerjee, Bhadada, Shetty, Singh et al., Vitamin D supplementation and clinical outcomes in COVID-19: a systematic review and metaanalysis, J Endocrinol Invest, doi:10.1007/s40618-021-01614-4
Panagiotou, Tee, Ihsan, Athar, Marchitelli et al., Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalized with COVID-19 are associated with greater disease severity, Clin Endocrinol (Oxf), doi:10.1111/cen.14276
Ratnesar-Shumate, Williams, Green, Krause, Holland et al., Simulated Sunlight Rapidly Inactivates SARS-CoV-2 on Surfaces, J Infect Dis, doi:10.1093/infdis/jiaa274
Rimm, Giovannucci, Stampfer, Colditz, Litin et al., Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals, Am J Epidemiol
Sabico, Enani, Sheshah, Aljohani, Aldisi et al., Effects of a 2-Week 5000 IU versus
Smet, Smet, Herroelen, Gryspeerdt, Martens, Serum 25(OH)D Level on Hospital Admission Associated With COVID-19 Stage and Mortality, Am J Clin Pathol, doi:10.1093/ajcp/aqaa252
Smolders, Van Den Ouweland, Geven, Pickkers, Kox, Letter to the Editor: Vitamin D deficiency in COVID-19: Mixing up cause and consequence, Metabolism, doi:10.1016/j.metabol.2020.154434
Waldron, Ashby, Cornes, Bechervaise, Razavi et al., Vitamin D: a negative acute phase reactant, J Clin Pathol, doi:10.1136/jclinpath-2012-201301
Wang, Degruttola, Lei, Mayer, Redline et al., The vitamin D for COVID-19 (VIVID) trial: A pragmatic
Whowgotc, Management of C-i. A minimal common outcome measure set for COVID-19 clinical research, Lancet Infect Dis, doi:10.1016/S1473-3099(20)30483-7
Wise, Covid-19: Evidence is lacking to support vitamin D's role in treatment and prevention, BMJ, doi:10.1136/bmj.m4912
DOI record:
{
"DOI": "10.1093/ajcn/nqab389",
"ISSN": [
"0002-9165",
"1938-3207"
],
"URL": "http://dx.doi.org/10.1093/ajcn/nqab389",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:sec>\n <jats:title>Background</jats:title>\n <jats:p>Vitamin D may have a role in immune responses to viral infections. However, data on the association between vitamin D and SARS-CoV-2 infection and Coronavirus Disease 2019 (COVID-19) severity have been limited and inconsistent.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Objective</jats:title>\n <jats:p>We examined the associations of predicted vitamin D status and intake with risk of SARS-CoV-2 infection and COVID-19 severity.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Design</jats:title>\n <jats:p>We used data from periodic surveys (May 2020 to March 2021) within the Nurses’ Health Study II. Among 39,315 participants, 1,768 reported a positive test for SARS-CoV-2 infection. Usual vitamin D intake from foods and supplements were measured using a semi-quantitative, pre-pandemic food frequency questionnaire in 2015. Predicted 25-hydroxyvitamin D [25(OH)D] levels were calculated based on a previously validated model including dietary and supplementary vitamin D intake, ultraviolet-B (UVB), and other behavioral predictors of vitamin D status.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>Higher predicted 25(OH)D levels, but not vitamin D intake, were associated with a lower risk of SARS-CoV-2 infection. Comparing participants in the highest quintile of predicted 25(OH)D levels to the lowest, the multivariable-adjusted odds ratio was 0.76 (95% CI: 0.58, 0.99; P-trend = 0.04). Participants in the highest quartile of UVB (OR: 0.76; 95% CI: 0.66, 0.87; P-trend = 0.002) and UVA (OR: 0.76; 95% CI: 0.66, 0.88; P-trend&lt;0.001) also had lower risk of SARS-CoV-2 infection compared to the lowest. High intake of vitamin D from supplements (≥400 IU/d) was associated with a lower risk of hospitalization (OR: 0.51; 95% CI: 0.29, 0.91; P-trend = 0.04).</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Conclusions</jats:title>\n <jats:p>Our study provides suggestive evidence on the association between higher predicted circulating 25(OH)D levels and a lower risk of SARS-CoV-2 infection. Greater intake of vitamin D supplements was associated with a lower risk of hospitalization. Our data also support an association between exposure to UVB or UVA, independent of vitamin D, and SARS-CoV-2 infection, so results for predicted 25(OH)D need to be interpreted cautiously.</jats:p>\n </jats:sec>",
"author": [
{
"ORCID": "http://orcid.org/0000-0001-9894-7072",
"affiliation": [
{
"name": "Clinical and Translational Epidemiology Unit, Massachusetts General Hospital and Harvard Medical School, Boston, MA"
},
{
"name": "Division of Gastroenterology, Massachusetts General Hospital and Harvard Medical School, Boston, MA"
}
],
"authenticated-orcid": false,
"family": "Ma",
"given": "Wenjie",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Clinical and Translational Epidemiology Unit, Massachusetts General Hospital and Harvard Medical School, Boston, MA"
},
{
"name": "Division of Gastroenterology, Massachusetts General Hospital and Harvard Medical School, Boston, MA"
}
],
"family": "Nguyen",
"given": "Long H",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6018-2980",
"affiliation": [
{
"name": "Department of Nutrition, Harvard T.H. Chan School of Public Health, Boston, MA"
}
],
"authenticated-orcid": false,
"family": "Yue",
"given": "Yiyang",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Nutrition, Harvard T.H. Chan School of Public Health, Boston, MA"
}
],
"family": "Ding",
"given": "Ming",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Clinical and Translational Epidemiology Unit, Massachusetts General Hospital and Harvard Medical School, Boston, MA"
},
{
"name": "Division of Gastroenterology, Massachusetts General Hospital and Harvard Medical School, Boston, MA"
}
],
"family": "Drew",
"given": "David A",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5614-5618",
"affiliation": [
{
"name": "Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, MA"
}
],
"authenticated-orcid": false,
"family": "Wang",
"given": "Kai",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8312-1438",
"affiliation": [
{
"name": "Diabetes Unit and Center for Genomic Medicine, Massachusetts General Hospital, Boston, MA"
},
{
"name": "Program in Medical and Population Genetics, Broad Institute, Cambridge, MA"
},
{
"name": "Department of Medicine, Harvard Medical School, Boston, MA"
}
],
"authenticated-orcid": false,
"family": "Merino",
"given": "Jordi",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, MA"
},
{
"name": "Division of Women's Health, Department of Medicine, Brigham and Women's Hospital and Harvard Medical School, Boston, MA"
}
],
"family": "Rich-Edwards",
"given": "Janet W",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8480-1563",
"affiliation": [
{
"name": "Department of Nutrition, Harvard T.H. Chan School of Public Health, Boston, MA"
},
{
"name": "Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, MA"
},
{
"name": "Division of Women's Health, Department of Medicine, Brigham and Women's Hospital and Harvard Medical School, Boston, MA"
}
],
"authenticated-orcid": false,
"family": "Sun",
"given": "Qi",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, MA"
},
{
"name": "Channing Division of Network Medicine, Department of Medicine, Brigham and Women's Hospital and Harvard Medical School, Boston, MA"
},
{
"name": "Department of Emergency Medicine, Massachusetts General Hospital and Harvard Medical School, Boston, MA"
}
],
"family": "Camargo",
"given": "Carlos A",
"sequence": "additional",
"suffix": "Jr"
},
{
"ORCID": "http://orcid.org/0000-0002-6123-0219",
"affiliation": [
{
"name": "Department of Nutrition, Harvard T.H. Chan School of Public Health, Boston, MA"
},
{
"name": "Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, MA"
},
{
"name": "Channing Division of Network Medicine, Department of Medicine, Brigham and Women's Hospital and Harvard Medical School, Boston, MA"
}
],
"authenticated-orcid": false,
"family": "Giovannucci",
"given": "Edward",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Nutrition, Harvard T.H. Chan School of Public Health, Boston, MA"
},
{
"name": "Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, MA"
},
{
"name": "Channing Division of Network Medicine, Department of Medicine, Brigham and Women's Hospital and Harvard Medical School, Boston, MA"
}
],
"family": "Willett",
"given": "Walter",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, MA"
},
{
"name": "Division of Preventive Medicine, Department of Medicine, Brigham and Women's Hospital and Harvard Medical School, Boston, MA"
}
],
"family": "Manson",
"given": "JoAnn E",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4780-4642",
"affiliation": [
{
"name": "Clinical and Translational Epidemiology Unit, Massachusetts General Hospital and Harvard Medical School, Boston, MA"
},
{
"name": "Division of Gastroenterology, Massachusetts General Hospital and Harvard Medical School, Boston, MA"
},
{
"name": "Department of Nutrition, Harvard T.H. Chan School of Public Health, Boston, MA"
},
{
"name": "Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, MA"
}
],
"authenticated-orcid": false,
"family": "Song",
"given": "Mingyang",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Nutrition, Harvard T.H. Chan School of Public Health, Boston, MA"
},
{
"name": "Channing Division of Network Medicine, Department of Medicine, Brigham and Women's Hospital and Harvard Medical School, Boston, MA"
}
],
"family": "Bhupathiraju",
"given": "Shilpa N",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7284-6767",
"affiliation": [
{
"name": "Clinical and Translational Epidemiology Unit, Massachusetts General Hospital and Harvard Medical School, Boston, MA"
},
{
"name": "Division of Gastroenterology, Massachusetts General Hospital and Harvard Medical School, Boston, MA"
},
{
"name": "Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, MA"
},
{
"name": "Channing Division of Network Medicine, Department of Medicine, Brigham and Women's Hospital and Harvard Medical School, Boston, MA"
}
],
"authenticated-orcid": false,
"family": "Chan",
"given": "Andrew T",
"sequence": "additional"
}
],
"container-title": [
"The American Journal of Clinical Nutrition"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
11,
22
]
],
"date-time": "2021-11-22T12:06:50Z",
"timestamp": 1637582810000
},
"deposited": {
"date-parts": [
[
2021,
12,
5
]
],
"date-time": "2021-12-05T09:08:09Z",
"timestamp": 1638695289000
},
"indexed": {
"date-parts": [
[
2021,
12,
6
]
],
"date-time": "2021-12-06T05:49:49Z",
"timestamp": 1638769789018
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "print",
"value": "0002-9165"
},
{
"type": "electronic",
"value": "1938-3207"
}
],
"issued": {
"date-parts": [
[
2021,
12,
3
]
]
},
"language": "en",
"license": [
{
"URL": "https://academic.oup.com/journals/pages/open_access/funder_policies/chorus/standard_publication_model",
"content-version": "am",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
12,
3
]
],
"date-time": "2021-12-03T00:00:00Z",
"timestamp": 1638489600000
}
}
],
"link": [
{
"URL": "https://academic.oup.com/ajcn/advance-article-pdf/doi/10.1093/ajcn/nqab389/41505202/nqab389.pdf",
"content-type": "application/pdf",
"content-version": "am",
"intended-application": "syndication"
},
{
"URL": "https://academic.oup.com/ajcn/advance-article-pdf/doi/10.1093/ajcn/nqab389/41505202/nqab389.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "286",
"original-title": [],
"prefix": "10.1093",
"published": {
"date-parts": [
[
2021,
12,
3
]
]
},
"published-online": {
"date-parts": [
[
2021,
12,
3
]
]
},
"publisher": "Oxford University Press (OUP)",
"reference-count": 0,
"references-count": 0,
"relation": {},
"score": 1,
"short-container-title": [],
"short-title": [],
"source": "Crossref",
"subject": [
"Nutrition and Dietetics",
"Medicine (miscellaneous)"
],
"subtitle": [],
"title": [
"Associations between predicted vitamin D status, vitamin D intake, and risk of SARS-CoV-2 infection and Coronavirus Disease 2019 severity"
],
"type": "journal-article"
}
