Simulated Sunlight Rapidly Inactivates SARS-CoV-2 on Surfaces
et al., The Journal of Infectious Diseases, doi:10.1093/infdis/jiaa274, May 2020
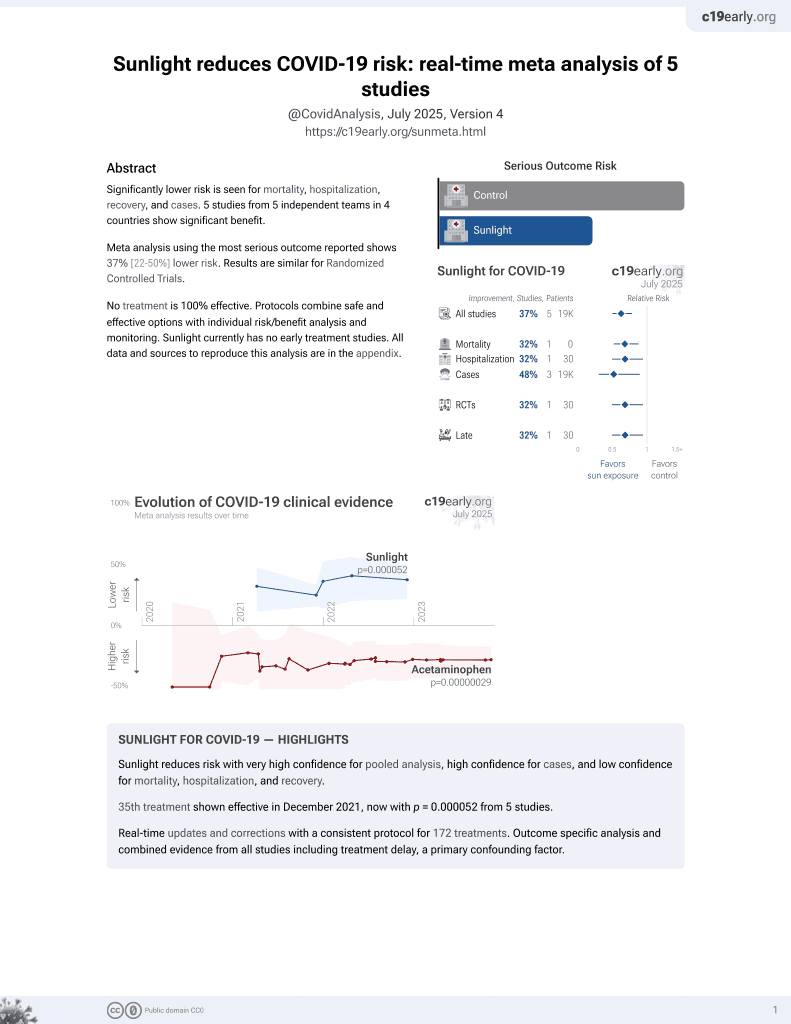
Sunlight for COVID-19
36th treatment shown to reduce risk in
December 2021, now with p = 0.000052 from 5 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
In vitro study showing that simulated sunlight rapidly inactivates SARS-CoV-2 on surfaces.
2 preclinical studies support the efficacy of sunlight for COVID-19:
Ratnesar-Shumate et al., 20 May 2020, USA, peer-reviewed, 19 authors.
Contact: shanna.ratnesarshumate@st.dhs.gov.
Simulated Sunlight Rapidly Inactivates SARS-CoV-2 on Surfaces
The Journal of Infectious Diseases, doi:10.1093/infdis/jiaa274
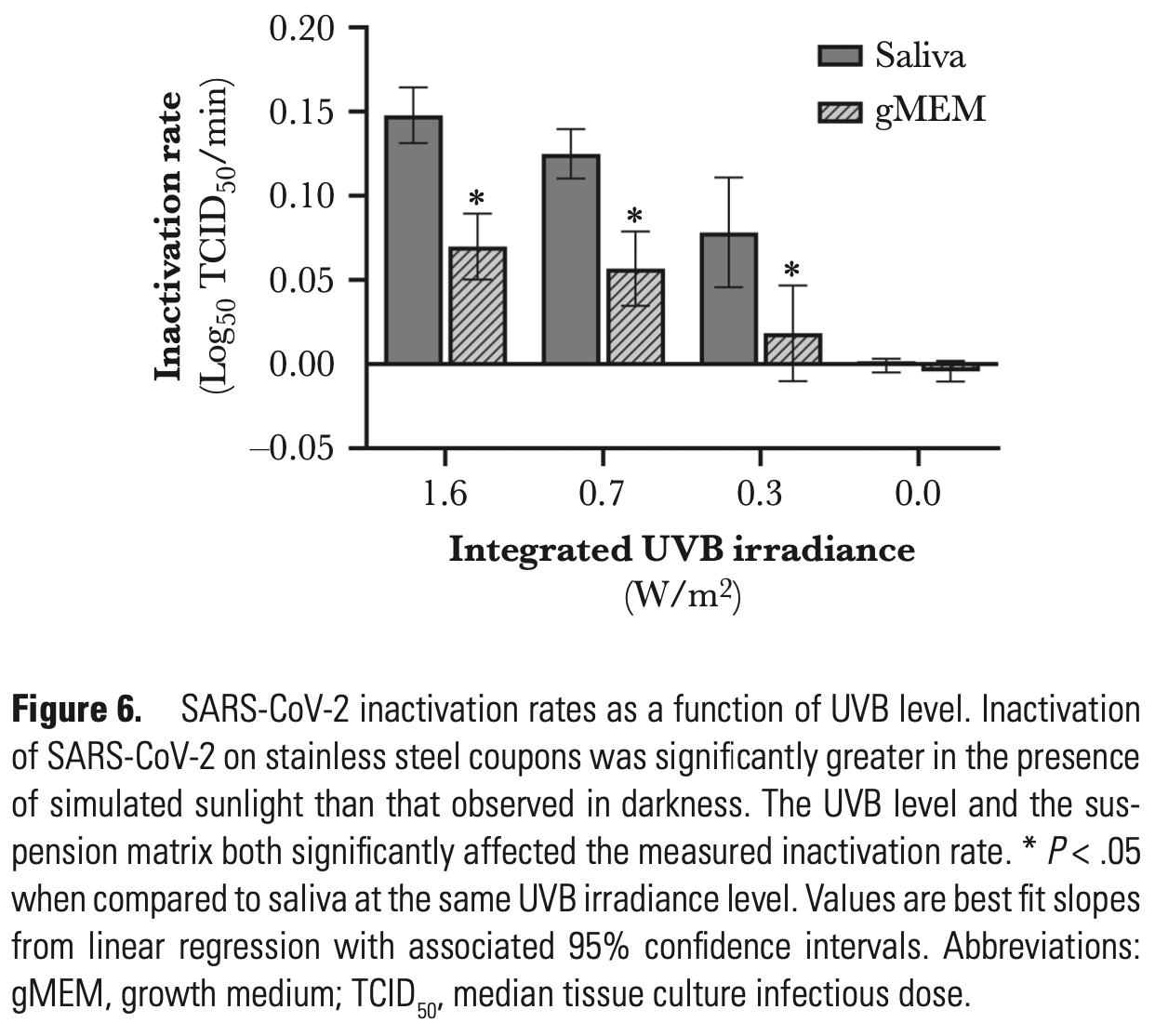
Previous studies have demonstrated that SARS-CoV-2 is stable on surfaces for extended periods under indoor conditions. In the present study, simulated sunlight rapidly inactivated SARS-CoV-2 suspended in either simulated saliva or culture media and dried on stainless steel coupons. Ninety percent of infectious virus was inactivated every 6.8 minutes in simulated saliva and every 14.3 minutes in culture media when exposed to simulated sunlight representative of the summer solstice at 40°N latitude at sea level on a clear day. Significant inactivation also occurred, albeit at a slower rate, under lower simulated sunlight levels. The present study provides the first evidence that sunlight may rapidly inactivate SARS-CoV-2 on surfaces, suggesting that persistence, and subsequently exposure risk, may vary significantly between indoor and outdoor environments. Additionally, these data indicate that natural sunlight may be effective as a disinfectant for contaminated nonporous materials.
References
Abad, Pintó, Bosch, Survival of enteric viruses on environmental fomites, Appl Environ Microbiol
Beck, Rodriguez, Hawkins, Hargy, Larason et al., Comparison of UV-induced inactivation and RNA damage in MS2 phage across the germicidal UV spectrum, Appl Environ Microbiol
Berendt, Dorsey, Effect of simulated solar radiation and sodium fluorescein on the recovery of Venezuelan equine encephalomyelitis virus from aerosols, Appl Microbiol
Casanova, Jeon, Rutala, Weber, Sobsey, Effects of air temperature and relative humidity on coronavirus survival on surfaces, Appl Environ Microbiol
Chan, Peiris, Lam, Poon, Yuen et al., The effects of temperature and relative humidity on the viability of the SARS coronavirus, Adv Virol
Chin, Shu, Mahen, Stability of SARS-CoV-2 in different environmental conditions, Lancet Microbe
Darnell, Subbarao, Feinstone, Taylor, Inactivation of the coronavirus that induces severe acute respiratory syndrome, SARS-CoV, J Virol Methods
Darnell, Taylor, Evaluation of inactivation methods for severe acute respiratory syndrome coronavirus in noncellular blood products, Transfusion
Graphpad, Knowledgebase, Multiple comparisons: two-way ANOVA
Guo, Wang, Zhang, Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards
Han, Weng, Huang, Characterizations of particle size distribution of the droplets exhaled by sneeze, J R Soc Interface
Heimbuch, Wallace, Kinney, A pandemic influenza preparedness study: use of energetic methods to decontaminate filtering facepiece respirators contaminated with H1N1 aerosols and droplets, Am J Infect Control
Kӓrber, Beitrag zur kollektiven Behandlung pharmakologischer Reihenversuche
Mbithi, Springthorpe, Sattar, Effect of relative humidity and air temperature on survival of hepatitis A virus on environmental surfaces, Appl Environ Microbiol
Mcdevitt, Lai, Rudnick, Houseman, First et al., Characterization of UVC light sensitivity of vaccinia virus, Appl Environ Microbiol
Nelson, Boehm, Davies-Colley, Sunlightmediated inactivation of health-relevant microorganisms in water: a review of mechanisms and modeling approaches, Environ Sci Process Impacts
Ong, Tan, Chia, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient, doi:10.1001/jama.2020.3227
Rabenau, Cinatl, Morgenstern, Bauer, Preiser et al., Stability and inactivation of SARS coronavirus, Med Microbiol Immunol
Schuit, Gardner, Wood, The influence of simulated sunlight on the inactivation of influenza virus in aerosols, J Infect Dis
Sohrabi, Alsafi, Neill, World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19), Int J Surg
Spearman, The method of "right and wrong cases" ("constant stimuli") without Gauss's formulae, Br J Psychol
Thomas, Boquete-Suter, Koch, Pittet, Kaiser, Survival of influenza virus on human fingers, Clin Microbiol Infect
Van Doremalen, Bushmaker, Morris, Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1, N Engl J Med
Woo, Hsu, Wu, Heimbuch, Wander, Method for contamination of filtering facepiece respirators by deposition of MS2 viral aerosols, J Aerosol Sci
Zayas, Chiang, Wong, Cough aerosol in healthy participants: fundamental knowledge to optimize droplet-spread infectious respiratory disease management, BMC Pulm Med
Zuo, Kuehn, Bekele, Survival of airborne MS2 bacteriophage generated from human saliva, artificial saliva, and cell culture medium, Appl Environ Microbiol
DOI record:
{
"DOI": "10.1093/infdis/jiaa274",
"ISSN": [
"0022-1899",
"1537-6613"
],
"URL": "http://dx.doi.org/10.1093/infdis/jiaa274",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:p>Previous studies have demonstrated that SARS-CoV-2 is stable on surfaces for extended periods under indoor conditions. In the present study, simulated sunlight rapidly inactivated SARS-CoV-2 suspended in either simulated saliva or culture media and dried on stainless steel coupons. Ninety percent of infectious virus was inactivated every 6.8 minutes in simulated saliva and every 14.3 minutes in culture media when exposed to simulated sunlight representative of the summer solstice at 40°N latitude at sea level on a clear day. Significant inactivation also occurred, albeit at a slower rate, under lower simulated sunlight levels. The present study provides the first evidence that sunlight may rapidly inactivate SARS-CoV-2 on surfaces, suggesting that persistence, and subsequently exposure risk, may vary significantly between indoor and outdoor environments. Additionally, these data indicate that natural sunlight may be effective as a disinfectant for contaminated nonporous materials.</jats:p>",
"author": [
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by Battelle National Biodefense Institute for the US Department of Homeland Security, Frederick, Maryland, USA"
}
],
"family": "Ratnesar-Shumate",
"given": "Shanna",
"sequence": "first"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by Battelle National Biodefense Institute for the US Department of Homeland Security, Frederick, Maryland, USA"
}
],
"family": "Williams",
"given": "Gregory",
"sequence": "first"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by Battelle National Biodefense Institute for the US Department of Homeland Security, Frederick, Maryland, USA"
}
],
"family": "Green",
"given": "Brian",
"sequence": "first"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by Battelle National Biodefense Institute for the US Department of Homeland Security, Frederick, Maryland, USA"
}
],
"family": "Krause",
"given": "Melissa",
"sequence": "first"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by Battelle National Biodefense Institute for the US Department of Homeland Security, Frederick, Maryland, USA"
}
],
"family": "Holland",
"given": "Brian",
"sequence": "first"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by Battelle National Biodefense Institute for the US Department of Homeland Security, Frederick, Maryland, USA"
}
],
"family": "Wood",
"given": "Stewart",
"sequence": "first"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by Battelle National Biodefense Institute for the US Department of Homeland Security, Frederick, Maryland, USA"
}
],
"family": "Bohannon",
"given": "Jordan",
"sequence": "first"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by Battelle National Biodefense Institute for the US Department of Homeland Security, Frederick, Maryland, USA"
}
],
"family": "Boydston",
"given": "Jeremy",
"sequence": "first"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by Battelle National Biodefense Institute for the US Department of Homeland Security, Frederick, Maryland, USA"
}
],
"family": "Freeburger",
"given": "Denise",
"sequence": "first"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by Battelle National Biodefense Institute for the US Department of Homeland Security, Frederick, Maryland, USA"
}
],
"family": "Hooper",
"given": "Idris",
"sequence": "first"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by Battelle National Biodefense Institute for the US Department of Homeland Security, Frederick, Maryland, USA"
}
],
"family": "Beck",
"given": "Katie",
"sequence": "first"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by Battelle National Biodefense Institute for the US Department of Homeland Security, Frederick, Maryland, USA"
}
],
"family": "Yeager",
"given": "John",
"sequence": "first"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by Battelle National Biodefense Institute for the US Department of Homeland Security, Frederick, Maryland, USA"
}
],
"family": "Altamura",
"given": "Louis A",
"sequence": "first"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by Battelle National Biodefense Institute for the US Department of Homeland Security, Frederick, Maryland, USA"
}
],
"family": "Biryukov",
"given": "Jennifer",
"sequence": "first"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by Battelle National Biodefense Institute for the US Department of Homeland Security, Frederick, Maryland, USA"
}
],
"family": "Yolitz",
"given": "Jason",
"sequence": "first"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by Battelle National Biodefense Institute for the US Department of Homeland Security, Frederick, Maryland, USA"
}
],
"family": "Schuit",
"given": "Michael",
"sequence": "first"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by Battelle National Biodefense Institute for the US Department of Homeland Security, Frederick, Maryland, USA"
}
],
"family": "Wahl",
"given": "Victoria",
"sequence": "first"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by Battelle National Biodefense Institute for the US Department of Homeland Security, Frederick, Maryland, USA"
}
],
"family": "Hevey",
"given": "Michael",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-3181-6825",
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by Battelle National Biodefense Institute for the US Department of Homeland Security, Frederick, Maryland, USA"
}
],
"authenticated-orcid": false,
"family": "Dabisch",
"given": "Paul",
"sequence": "first"
}
],
"container-title": "The Journal of Infectious Diseases",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2020,
5,
16
]
],
"date-time": "2020-05-16T04:56:48Z",
"timestamp": 1589605008000
},
"deposited": {
"date-parts": [
[
2020,
6,
29
]
],
"date-time": "2020-06-29T12:35:45Z",
"timestamp": 1593434145000
},
"funder": [
{
"award": [
"HSHQDC-15-C-00064"
],
"name": "DHS Science and Technology Directorate"
}
],
"indexed": {
"date-parts": [
[
2022,
12,
21
]
],
"date-time": "2022-12-21T01:11:06Z",
"timestamp": 1671585066858
},
"is-referenced-by-count": 217,
"issue": "2",
"issued": {
"date-parts": [
[
2020,
5,
20
]
]
},
"journal-issue": {
"issue": "2",
"published-online": {
"date-parts": [
[
2020,
5,
20
]
]
},
"published-print": {
"date-parts": [
[
2020,
6,
29
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
5,
20
]
],
"date-time": "2020-05-20T00:00:00Z",
"timestamp": 1589932800000
}
}
],
"link": [
{
"URL": "http://academic.oup.com/jid/advance-article-pdf/doi/10.1093/infdis/jiaa274/33339356/jiaa274.pdf",
"content-type": "application/pdf",
"content-version": "am",
"intended-application": "syndication"
},
{
"URL": "http://academic.oup.com/jid/article-pdf/222/2/214/33441804/jiaa274.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "syndication"
},
{
"URL": "http://academic.oup.com/jid/article-pdf/222/2/214/33441804/jiaa274.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "286",
"original-title": [],
"page": "214-222",
"prefix": "10.1093",
"published": {
"date-parts": [
[
2020,
5,
20
]
]
},
"published-online": {
"date-parts": [
[
2020,
5,
20
]
]
},
"published-other": {
"date-parts": [
[
2020,
7,
15
]
]
},
"published-print": {
"date-parts": [
[
2020,
6,
29
]
]
},
"publisher": "Oxford University Press (OUP)",
"reference": [
{
"DOI": "10.1016/j.ijsu.2020.02.034",
"article-title": "World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19)",
"author": "Sohrabi",
"doi-asserted-by": "crossref",
"first-page": "71",
"journal-title": "Int J Surg",
"key": "2020062908342008600_CIT0001",
"volume": "76",
"year": "2020"
},
{
"article-title": "Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020",
"author": "Guo",
"journal-title": "Emerg Infect Dis",
"key": "2020062908342008600_CIT0002"
},
{
"article-title": "Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient",
"author": "Ong",
"journal-title": "JAMA",
"key": "2020062908342008600_CIT0003"
},
{
"DOI": "10.1056/NEJMc2004973",
"article-title": "Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1",
"author": "van Doremalen",
"doi-asserted-by": "crossref",
"first-page": "1564",
"journal-title": "N Engl J Med",
"key": "2020062908342008600_CIT0004",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1016/S2666-5247(20)30003-3",
"article-title": "Stability of SARS-CoV-2 in different environmental conditions",
"author": "Chin",
"doi-asserted-by": "crossref",
"first-page": "E10",
"journal-title": "Lancet Microbe",
"key": "2020062908342008600_CIT0005",
"volume": "1",
"year": "2020"
},
{
"DOI": "10.1128/AEM.60.10.3704-3710.1994",
"article-title": "Survival of enteric viruses on environmental fomites",
"author": "Abad",
"doi-asserted-by": "crossref",
"first-page": "3704",
"journal-title": "Appl Environ Microbiol",
"key": "2020062908342008600_CIT0006",
"volume": "60",
"year": "1994"
},
{
"DOI": "10.1128/AEM.21.3.447-450.1971",
"article-title": "Effect of simulated solar radiation and sodium fluorescein on the recovery of Venezuelan equine encephalomyelitis virus from aerosols",
"author": "Berendt",
"doi-asserted-by": "crossref",
"first-page": "447",
"journal-title": "Appl Microbiol",
"key": "2020062908342008600_CIT0007",
"volume": "21",
"year": "1971"
},
{
"DOI": "10.1128/AEM.02291-09",
"article-title": "Effects of air temperature and relative humidity on coronavirus survival on surfaces",
"author": "Casanova",
"doi-asserted-by": "crossref",
"first-page": "2712",
"journal-title": "Appl Environ Microbiol",
"key": "2020062908342008600_CIT0008",
"volume": "76",
"year": "2010"
},
{
"DOI": "10.1155/2011/734690",
"article-title": "The effects of temperature and relative humidity on the viability of the SARS coronavirus",
"author": "Chan",
"doi-asserted-by": "crossref",
"first-page": "734690",
"journal-title": "Adv Virol",
"key": "2020062908342008600_CIT0009",
"volume": "2011",
"year": "2011"
},
{
"DOI": "10.1128/AEM.00110-07",
"article-title": "Characterization of UVC light sensitivity of vaccinia virus",
"author": "McDevitt",
"doi-asserted-by": "crossref",
"first-page": "5760",
"journal-title": "Appl Environ Microbiol",
"key": "2020062908342008600_CIT0010",
"volume": "73",
"year": "2007"
},
{
"DOI": "10.1128/AEM.57.5.1394-1399.1991",
"article-title": "Effect of relative humidity and air temperature on survival of hepatitis A virus on environmental surfaces",
"author": "Mbithi",
"doi-asserted-by": "crossref",
"first-page": "1394",
"journal-title": "Appl Environ Microbiol",
"key": "2020062908342008600_CIT0011",
"volume": "57",
"year": "1991"
},
{
"DOI": "10.1111/j.2044-8295.1908.tb00176.x",
"article-title": "The method of “right and wrong cases” (“constant stimuli”) without Gauss’s formulae",
"author": "Spearman",
"doi-asserted-by": "crossref",
"first-page": "227",
"journal-title": "Br J Psychol 1904",
"key": "2020062908342008600_CIT0012",
"volume": "2",
"year": "1908"
},
{
"DOI": "10.1007/BF01863914",
"article-title": "Beitrag zur kollektiven Behandlung pharmakologischer Reihenversuche [in German]",
"author": "Kӓrber",
"doi-asserted-by": "crossref",
"first-page": "480",
"journal-title": "Archiv Exp Pathol Pharmakol",
"key": "2020062908342008600_CIT0013",
"volume": "162",
"year": "1931"
},
{
"DOI": "10.1093/infdis/jiz582",
"article-title": "The influence of simulated sunlight on the inactivation of influenza virus in aerosols",
"author": "Schuit",
"doi-asserted-by": "crossref",
"first-page": "372",
"journal-title": "J Infect Dis",
"key": "2020062908342008600_CIT0014",
"volume": "221",
"year": "2020"
},
{
"author": "National Center for Atmospheric Research",
"key": "2020062908342008600_CIT0015"
},
{
"DOI": "10.1016/j.jviromet.2004.06.006",
"article-title": "Inactivation of the coronavirus that induces severe acute respiratory syndrome, SARS-CoV",
"author": "Darnell",
"doi-asserted-by": "crossref",
"first-page": "85",
"journal-title": "J Virol Methods",
"key": "2020062908342008600_CIT0016",
"volume": "121",
"year": "2004"
},
{
"DOI": "10.1016/j.jaerosci.2010.07.003",
"article-title": "Method for contamination of filtering facepiece respirators by deposition of MS2 viral aerosols",
"author": "Woo",
"doi-asserted-by": "crossref",
"first-page": "944",
"journal-title": "J Aerosol Sci",
"key": "2020062908342008600_CIT0017",
"volume": "41",
"year": "2010"
},
{
"DOI": "10.1128/AEM.00056-14",
"article-title": "Survival of airborne MS2 bacteriophage generated from human saliva, artificial saliva, and cell culture medium",
"author": "Zuo",
"doi-asserted-by": "crossref",
"first-page": "2796",
"journal-title": "Appl Environ Microbiol",
"key": "2020062908342008600_CIT0018",
"volume": "80",
"year": "2014"
},
{
"author": "GraphPad",
"key": "2020062908342008600_CIT0019"
},
{
"DOI": "10.1007/s00430-004-0219-0",
"article-title": "Stability and inactivation of SARS coronavirus",
"author": "Rabenau",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Med Microbiol Immunol",
"key": "2020062908342008600_CIT0020",
"volume": "194",
"year": "2005"
},
{
"DOI": "10.1186/1471-2466-12-11",
"article-title": "Cough aerosol in healthy participants: fundamental knowledge to optimize droplet-spread infectious respiratory disease management",
"author": "Zayas",
"doi-asserted-by": "crossref",
"first-page": "11",
"journal-title": "BMC Pulm Med",
"key": "2020062908342008600_CIT0021",
"volume": "12",
"year": "2012"
},
{
"DOI": "10.1098/rsif.2013.0560",
"article-title": "Characterizations of particle size distribution of the droplets exhaled by sneeze",
"author": "Han",
"doi-asserted-by": "crossref",
"first-page": "20130560",
"journal-title": "J R Soc Interface",
"key": "2020062908342008600_CIT0022",
"volume": "10",
"year": "2013"
},
{
"DOI": "10.1111/1469-0691.12324",
"article-title": "Survival of influenza virus on human fingers",
"author": "Thomas",
"doi-asserted-by": "crossref",
"first-page": "O58",
"journal-title": "Clin Microbiol Infect",
"key": "2020062908342008600_CIT0023",
"volume": "20",
"year": "2014"
},
{
"DOI": "10.1111/j.1537-2995.2006.00976.x",
"article-title": "Evaluation of inactivation methods for severe acute respiratory syndrome coronavirus in noncellular blood products",
"author": "Darnell",
"doi-asserted-by": "crossref",
"first-page": "1770",
"journal-title": "Transfusion",
"key": "2020062908342008600_CIT0024",
"volume": "46",
"year": "2006"
},
{
"DOI": "10.1039/C8EM00047F",
"article-title": "Sunlight-mediated inactivation of health-relevant microorganisms in water: a review of mechanisms and modeling approaches",
"author": "Nelson",
"doi-asserted-by": "crossref",
"first-page": "1089",
"journal-title": "Environ Sci Process Impacts",
"key": "2020062908342008600_CIT0025",
"volume": "20",
"year": "2018"
},
{
"DOI": "10.1016/j.ajic.2010.07.004",
"article-title": "A pandemic influenza preparedness study: use of energetic methods to decontaminate filtering facepiece respirators contaminated with H1N1 aerosols and droplets",
"author": "Heimbuch",
"doi-asserted-by": "crossref",
"first-page": "e1",
"journal-title": "Am J Infect Control",
"key": "2020062908342008600_CIT0026",
"volume": "39",
"year": "2011"
},
{
"DOI": "10.1128/AEM.02773-15",
"article-title": "Comparison of UV-induced inactivation and RNA damage in MS2 phage across the germicidal UV spectrum",
"author": "Beck",
"doi-asserted-by": "crossref",
"first-page": "1468",
"journal-title": "Appl Environ Microbiol",
"key": "2020062908342008600_CIT0027",
"volume": "82",
"year": "2015"
}
],
"reference-count": 27,
"references-count": 27,
"relation": {},
"resource": {
"primary": {
"URL": "https://academic.oup.com/jid/article/222/2/214/5841129"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Infectious Diseases",
"Immunology and Allergy"
],
"subtitle": [],
"title": "Simulated Sunlight Rapidly Inactivates SARS-CoV-2 on Surfaces",
"type": "journal-article",
"volume": "222"
}