Infrared light therapy relieves TLR-4 dependent hyper-inflammation of the type induced by COVID-19
et al., Communicative & Integrative Biology, doi:10.1080/19420889.2021.1965718, Sep 2021
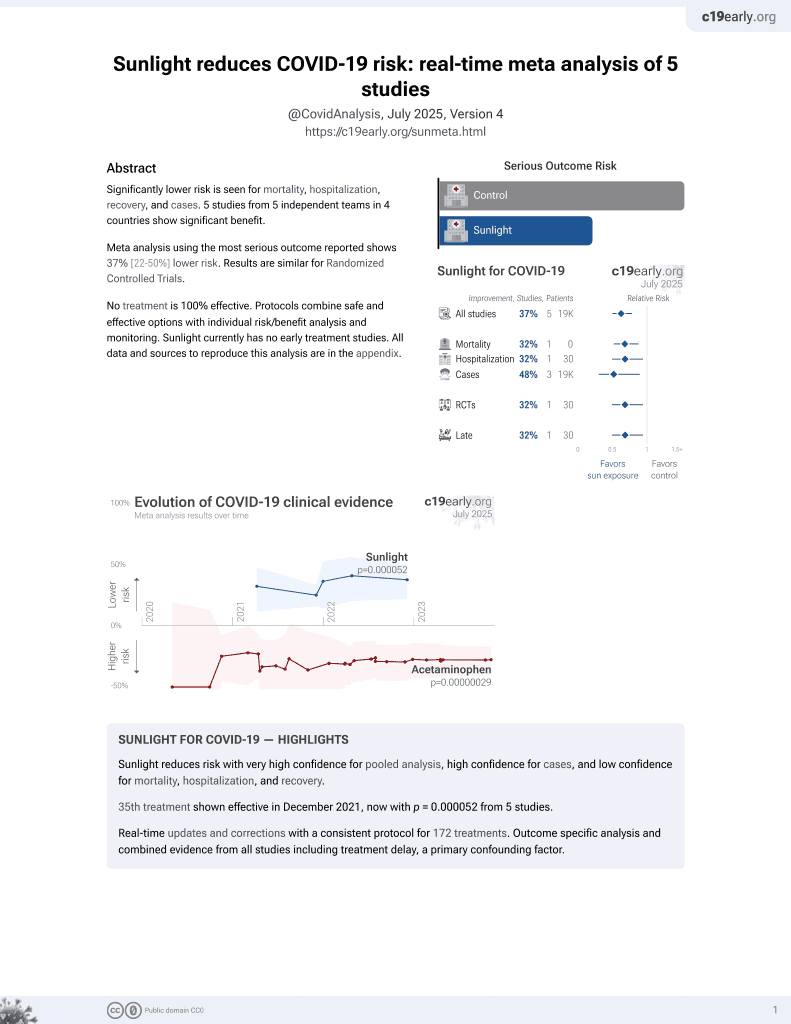
Sunlight for COVID-19
36th treatment shown to reduce risk in
December 2021, now with p = 0.000052 from 5 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
In vitro study of human cell cultures showing decreased inflammation and cytokine production with infrared light therapy. Cells were engineered to express components of the TLR4 inflammation pathway implicated in COVID-19 cytokine storms. Authors suggest infrared therapy could help treat COVID-19 respiratory distress by suppressing lung inflammation and cytokine production, but note that clinical trials are still needed to demonstrate effectiveness in patients.
2 preclinical studies support the efficacy of sunlight for COVID-19:
Aguida et al., 15 Sep 2021, USA, peer-reviewed, 4 authors.
Contact: margaret.ahmad@sorbonne-universite.fr, nathalie.jourdan@sorbonne-universite.fr.
Infrared light therapy relieves TLR-4 dependent hyper-inflammation of the type induced by COVID-19
Communicative & Integrative Biology, doi:10.1080/19420889.2021.1965718
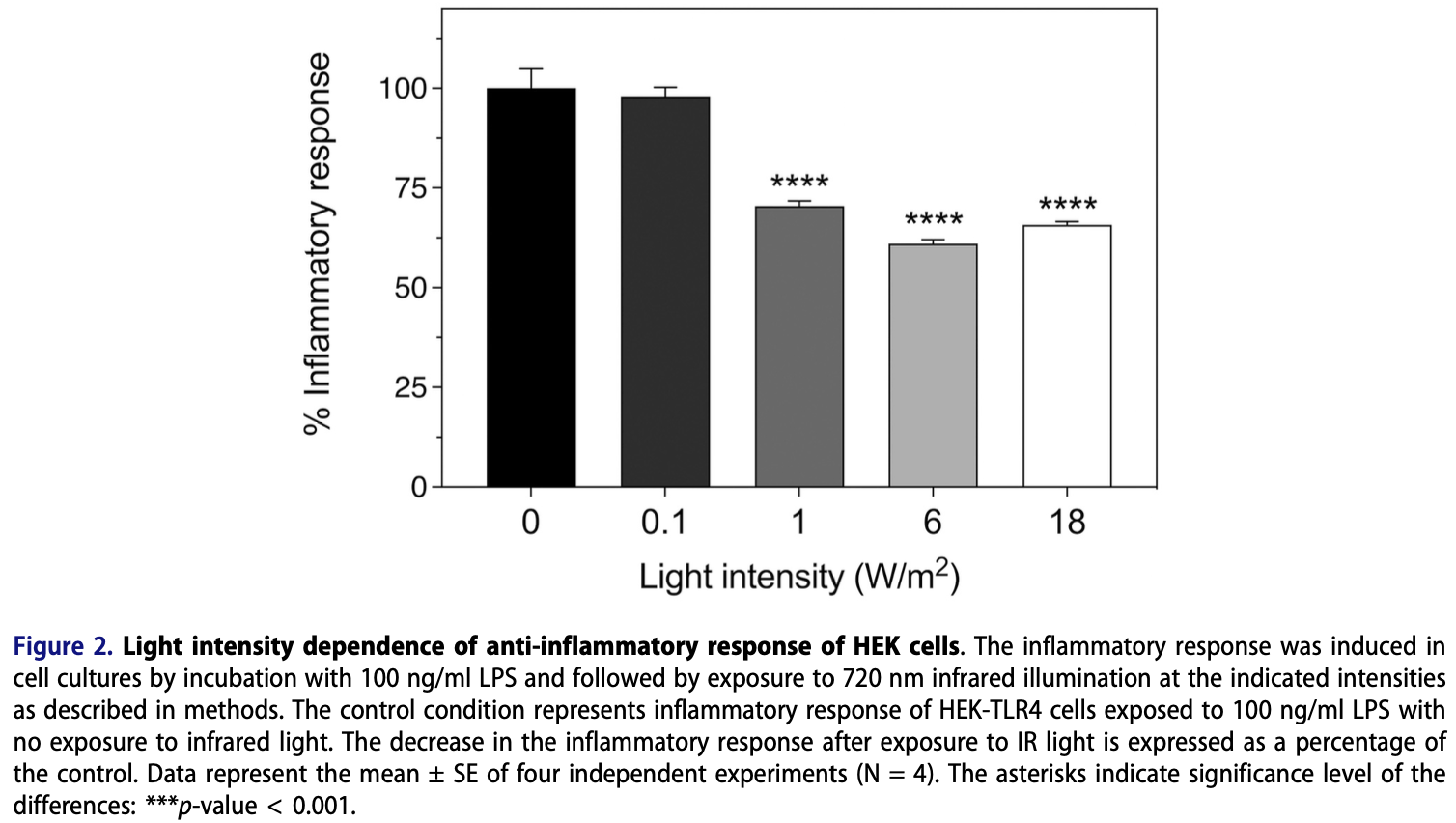
The leading cause of mortality from COVID-19 infection is respiratory distress due to an exaggerated host immune response, resulting in hyper-inflammation and ensuing cytokine storms in the lungs. Current drug-based therapies are of limited efficacy, costly, and have potential negative side effects. By contrast, photobiomodulation therapy, which involves periodic brief exposure to red or infrared light, is a noninvasive, safe, and affordable method that is currently being used to treat a wide range of diseases with underlying inflammatory conditions. Here, we show that exposure to two 10-min, high-intensity periods per day of infrared light causes a marked reduction in the TLR-4 dependent inflammatory response pathway, which has been implicated in the onset of cytokine storms in COVID-19 patients. Infrared light exposure resulted in a significant decline in NFkB and AP1 activity as measured by the reporter gene assay; decreased expression of inflammatory marker genes IL-6, IL-8, TNF-alpha, INF-alpha, and INF-beta as determined by qPCR gene expression assay; and an 80% decline in secreted cytokine IL6 as measured by ELISA assay in cultured human cells. All of these changes occurred after only 48 hours of treatment. We suggest that an underlying cellular mechanism involving modulation of ROS may downregulate the host immune response after Infrared Light exposure, leading to decrease in inflammation. We further discuss technical considerations involving light sources and exposure conditions to put these observations into potential clinical use to treat COVID-19 induced mortality.
Author contributions BA designed the experiments, conducted research, data analysis, and wrote the manuscript. MP designed the experiments, conducted research, data analysis, and wrote the manuscript; NJ designed the experiments, analyzed data; MA designed the experiments, obtained funding, analyzed data, and wrote the paper, as well as assisted in the experimental design and analyzed the data.
Disclosure statement No potential conflict of interest was reported by the author(s).
Funding
References
Ablon, Combination 830-nm and 633-nm light-emitting diode phototherapy shows promise in the treatment of recalcitrant psoriasis: preliminary findings, Photomed Laser Surg
Aboudounya, Heads, Dozio, COVID-19 and toll-like receptor 4 (TLR4): SARS-CoV-2 may bind and activate TLR4 to increase ACE2 expression, facilitating entry and causing hyperinflammation, Mediators Inflamm
Avci, Gupta, Clark, Low-level laser (light) therapy (LLLT) for treatment of hair loss, Lasers Surg Med
Bhattacharya, Sharma, Mallick, Immunoinformatics approach to understand molecular interaction between multi-epitopic regions of SARS-CoV-2 spike-protein with TLR4/MD-2 complex, Infect Genet Evol
Bjordal, Iversen, A randomised, placebo controlled trial of low level laser therapy for activated Achilles tendinitis with microdialysis measurement of peritendinous prostaglandin E2 concentrations, Br J Sports Med
Carvalho, De Brito, De Oliveira, The chemokines secretion and the oxidative stress are targets of low-level laser therapy in allergic lung inflammation, J Biophotonics
Choi, Na, Cho, Low level light could work on skin inflammatory disease: a case report on refractory acrodermatitis continua, J Korean Med Sci
Choudhury, In silico studies on the comparative characterization of the interactions of SARS-CoV-2 spike glycoprotein with ACE-2 receptor homologs and human TLRs -Choudhury -2020, J Med Virol
Chowdhury, Hossain, Kashem, Immune response in COVID-19: a review, J Infect Public Health
Chu, Zhou, Jiang, Staphylococcus aureus phenol-soluble modulins α1-α3 act as novel toll-like receptor (TLR) 4 antagonists to inhibit HMGB1/TLR4/ NF-κB signaling pathway, Front Immunol
Della-Torre, Lanzillotta, Campochiaro, Respiratory impairment predicts response to IL-1 and IL-6 blockade in COVID-19 patients with severe pneumonia and hyper-inflammation, Front Immunol, doi:10.3389/fimmu.2021.675678
Fekrazad, Photobiomodulation and antiviral photodynamic therapy as a possible novel approach in COVID-19 management, Photobiomodul Photomed Laser Surg
Gupta, Foley, A critical assessment of the evidence for low-level laser therapy in the treatment of hair loss, Dermatol Surg
Hamblin, Mechanisms and applications of the anti-inflammatory effects of photobiomodulation, AIMS Biophys
Hu, Guo, Zhou, Characteristics of SARS-CoV-2 and COVID-19, Nat Rev Microbiol
Höfling, Chavantes, Acencio, Effects of low-level laser therapy on the serum TGF-β1 concentrations in individuals with autoimmune thyroiditis, Photomed Laser Surg
Imai, Kuba, Neely, Identification of oxidative stress and toll-like receptor 4 signaling as a key pathway of acute lung injury, Cell
Ip, Does addition of low-level laser therapy (LLLT) in conservative care of knee arthritis successfully postpone the need for joint replacement?, Lasers Med Sci
Johnston, Xing, Wolterink, IL-1 and IL-36 are dominant cytokines in generalized pustular psoriasis, J Allergy Clin Immunol
Lecca, Nevin, Mulas, Neuroprotective and anti-inflammatory properties of a novel nonthiazolidinedione PPARγ agonist in vitro and in MPTP-treated mice, Neuroscience
Lima, Albertini, Dantas, Low-Level laser therapy restores the oxidative stress balance in acute lung injury induced by gut ischemia and reperfusion, Photochem Photobiol
Lima, Villaverde, Albertini, Dual Effect of low-level laser therapy (LLLT) on the acute lung inflammation induced by intestinal ischemia and reperfusion: action on anti-and pro-inflammatory cytokines, Lasers Surg Med
Mishra, Singh, Singh, Hyperinflammation and Immune Response Generation in COVID-19, NIM
Mittal, Siddiqui, Tran, Reactive oxygen species in inflammation and tissue injury, Antioxid Redox Signal
Moretti, Smets, Hofman, Human inflammatory response of endotoxin affected by particulate matter-bound transition metals, Environ Pollut
Mortaz, Tabarsi, Varahram, The immune response and immunopathology of COVID-19, Front Immunol, doi:10.3389/fimmu.2020.02037
Nejatifard, Asefi, Jamali, Probable positive effects of the photobiomodulation as an adjunctive treatment in COVID-19: a systematic review, Cytokine
Olejnik, Hume, Mühlberger, Toll-like receptor 4 in acute viral infection: too much of a good thing, PLoS Pathog
Oyler, Khan, Smith, top down tandem mass spectrometric analysis of a chemically modified rough-type lipopolysaccharide vaccine candidate, J Am Soc Mass Spectrom
Park, Lee, Recognition of lipopolysaccharide pattern by TLR4 complexes, Exp Mol Med
Park, Shin, Shah, TLR4/MD2 specific peptides stalled in vivo LPS-induced immune exacerbation, Biomaterials
Peng, Bishop, Ferguson, Screening of cytotoxicity and anti-inflammatory properties of feijoa extracts using genetically modified cell models targeting TLR2, TLR4 and NOD2 pathways, and the implication for inflammatory bowel disease, Nutrients
Pooam, Aguida, Drahy, Therapeutic application of light and electromagnetic fields to reduce hyper-inflammation triggered by COVID-19, Commun Integr Biol
Ragab, Salah Eldin, Taeimah, The COVID-19 cytokine storm; what we know so far, Front Immunol, doi:10.3389/fimmu.2020.01446
Rahiman, Morgan, Gray, Inhibitory effects of dynorphin 3-14 on the lipopolysaccharide-induced toll-like receptor 4 signalling pathway, Peptides
Rajendran, Kumar, George, the influence of light on reactive oxygen species and NF-кB in disease progression, Antioxidants
Sender, Stamme, Lung cell-specific modulation of LPS-induced TLR4 receptor and adaptor localization, Commun Integr Biol
Shirato, Kizaki, SARS-CoV-2 spike protein S1 subunit induces pro-inflammatory responses via toll-like receptor 4 signaling in murine and human macrophages, Heliyon
Shuai, Chu, Hou, Differential immune activation profile of SARS-CoV-2 and SARS-CoV infection in human lung and intestinal cells: implications for treatment with IFN-β and IFN inducer, J Infect
Sigman, Mokmeli, Monici, A 57-Year-old African American man with severe covid-19 pneumonia who responded to supportive Photobiomodulation Therapy (PBMT): first use of PBMT in COVID-19, Am J Case Rep
Sigman, Mokmeli, Vetrici, Adjunct low level laser therapy (LLLT) in a morbidly obese patient with severe COVID-19 pneumonia: a case report, Can J Respir Ther
Silva, Marcondes, Silva, Low-level laser therapy inhibits bronchoconstriction, Th2 inflammation and airway remodeling in allergic asthma, Respir Physiol Neurobiol
Silva, Santos, De Almeida, Effect of systemic photobiomodulation in the course of acute lung injury in rats, Lasers Med Sci
Sohn, Lee, Kim, COVID-19 patients upregulate toll-like receptor 4-mediated inflammatory signaling that mimics bacterial sepsis, J Korean Med Sci
Ss, Farazmand, Motamed, Effects of guluronic acid (G2013) on SHIP1, SOCS1 induction and related molecules in TLR4 signaling pathway, Int Immunopharmacol
Vetrici, Mokmeli, Bohm, Evaluation of adjunctive photobiomodulation (PBMT) for COVID-19 pneumonia via clinical status and pulmonary severity indices in a preliminary trial, JIR
West, Brodsky, Rahner, TLR signaling augments macrophage bactericidal activity through mitochondrial ROS, Nature
Xie, Matigian, Vithanage, Effect of perioperative opioids on cancer-relevant circulating parameters: mu opioid receptor and toll-like receptor 4 activation potential, and proteolytic profile, Clin Cancer Res
Xu, Chen, Cao, Discovery of novel small molecule TLR4 inhibitors as potent anti-inflammatory agents, Eur J Med Chem
Xu, Han, Li, Effective treatment of severe COVID-19 patients with tocilizumab, PNAS
Zhao, Kuang, Li, Publisher correction: SARS-CoV-2 spike protein interacts with and activates TLR4, Cell Res
Zhao, Kuang, Li, SARS-CoV-2 spike protein interacts with and activates TLR41, Cell Res
Zhou, Wang, Lin, Specific TLR4 blocking effect of a novel 3,4-dihydropyrimidinone derivative, Front Pharmacol
DOI record:
{
"DOI": "10.1080/19420889.2021.1965718",
"ISSN": [
"1942-0889"
],
"URL": "http://dx.doi.org/10.1080/19420889.2021.1965718",
"alternative-id": [
"10.1080/19420889.2021.1965718"
],
"assertion": [
{
"label": "Peer Review Statement",
"name": "peerreview_statement",
"order": 1,
"value": "The publishing and review policy for this title is described in its Aims & Scope."
},
{
"URL": "http://www.tandfonline.com/action/journalInformation?show=aimsScope&journalCode=kcib20",
"label": "Aim & Scope",
"name": "aims_and_scope_url",
"order": 2,
"value": "http://www.tandfonline.com/action/journalInformation?show=aimsScope&journalCode=kcib20"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2021-07-08"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Revised",
"name": "revised",
"order": 1,
"value": "2021-08-03"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "2021-08-04"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 3,
"value": "2021-09-15"
}
],
"author": [
{
"affiliation": [
{
"name": "Cnrs, Ibps, Sorbonne Université, Paris, France"
}
],
"family": "Aguida",
"given": "Blanche",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Biology, Faculty of Science, Naresuan University, Phitsanulok, Thailand"
}
],
"family": "Pooam",
"given": "Marootpong",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4524-5813",
"affiliation": [
{
"name": "Cnrs, Ibps, Sorbonne Université, Paris, France"
},
{
"name": "Department of Biology, Xavier University, Cincinnati, Ohio, USA"
}
],
"authenticated-orcid": false,
"family": "Ahmad",
"given": "Margaret",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Cnrs, Ibps, Sorbonne Université, Paris, France"
}
],
"family": "Jourdan",
"given": "Nathalie",
"sequence": "additional"
}
],
"container-title": "Communicative & Integrative Biology",
"container-title-short": "Communicative & Integrative Biology",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"www.tandfonline.com"
]
},
"created": {
"date-parts": [
[
2021,
9,
16
]
],
"date-time": "2021-09-16T06:06:54Z",
"timestamp": 1631772414000
},
"deposited": {
"date-parts": [
[
2022,
1,
4
]
],
"date-time": "2022-01-04T11:17:34Z",
"timestamp": 1641295054000
},
"funder": [
{
"DOI": "10.13039/501100009708",
"doi-asserted-by": "publisher",
"name": "Novo Nordisk Foundation"
},
{
"DOI": "10.13039/501100009708",
"award": [
"NNF19OC0057729"
],
"doi-asserted-by": "publisher",
"name": "Novo Nordisk Fonden"
}
],
"indexed": {
"date-parts": [
[
2023,
10,
2
]
],
"date-time": "2023-10-02T17:14:13Z",
"timestamp": 1696266853371
},
"is-referenced-by-count": 7,
"issue": "1",
"issued": {
"date-parts": [
[
2021,
1,
1
]
]
},
"journal-issue": {
"issue": "1",
"published-print": {
"date-parts": [
[
2021,
1,
1
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
1,
1
]
],
"date-time": "2021-01-01T00:00:00Z",
"timestamp": 1609459200000
}
}
],
"link": [
{
"URL": "https://www.tandfonline.com/doi/pdf/10.1080/19420889.2021.1965718",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "301",
"original-title": [],
"page": "200-211",
"prefix": "10.1080",
"published": {
"date-parts": [
[
2021,
1,
1
]
]
},
"published-online": {
"date-parts": [
[
2021,
9,
15
]
]
},
"published-print": {
"date-parts": [
[
2021,
1,
1
]
]
},
"publisher": "Informa UK Limited",
"reference": [
{
"DOI": "10.3389/fimmu.2020.02037",
"doi-asserted-by": "publisher",
"key": "cit0001"
},
{
"DOI": "10.1038/s41579-020-00459-7",
"doi-asserted-by": "publisher",
"key": "cit0002"
},
{
"DOI": "10.3389/fimmu.2020.01446",
"doi-asserted-by": "publisher",
"key": "cit0003"
},
{
"author": "Mishra KP",
"first-page": "80",
"journal-title": "NIM",
"key": "cit0004",
"volume": "27",
"year": "2020"
},
{
"DOI": "10.1016/j.jiph.2020.07.001",
"doi-asserted-by": "publisher",
"key": "cit0005"
},
{
"DOI": "10.1371/journal.ppat.1007390",
"doi-asserted-by": "publisher",
"key": "cit0006"
},
{
"DOI": "10.1038/emm.2013.97",
"doi-asserted-by": "publisher",
"key": "cit0007"
},
{
"DOI": "10.1016/j.biomaterials.2017.02.023",
"doi-asserted-by": "publisher",
"key": "cit0008"
},
{
"DOI": "10.1016/j.cell.2008.02.043",
"doi-asserted-by": "publisher",
"key": "cit0009"
},
{
"author": "Sohn KM",
"first-page": "35(38):e343",
"journal-title": "J Korean Med Sci",
"key": "cit0010",
"year": "2020"
},
{
"DOI": "10.1016/j.meegid.2020.104587",
"doi-asserted-by": "publisher",
"key": "cit0011"
},
{
"author": "choudhury and mukherjee",
"journal-title": "J Med Virol",
"key": "cit0012",
"year": "2020"
},
{
"DOI": "10.1038/s41422-021-00495-9",
"doi-asserted-by": "publisher",
"key": "cit0013"
},
{
"DOI": "10.1038/s41422-021-00501-0",
"doi-asserted-by": "publisher",
"key": "cit0014"
},
{
"DOI": "10.1016/j.heliyon.2021.e06187",
"doi-asserted-by": "publisher",
"key": "cit0015"
},
{
"DOI": "10.4161/cib.29053",
"doi-asserted-by": "publisher",
"key": "cit0016"
},
{
"DOI": "10.1073/pnas.2005615117",
"doi-asserted-by": "publisher",
"key": "cit0017"
},
{
"DOI": "10.3389/fimmu.2021.675678",
"doi-asserted-by": "publisher",
"key": "cit0018"
},
{
"DOI": "10.1056/NEJMoa2100433",
"doi-asserted-by": "publisher",
"key": "cit0019"
},
{
"DOI": "10.1089/photob.2020.4868",
"doi-asserted-by": "publisher",
"key": "cit0020"
},
{
"DOI": "10.1016/j.cyto.2020.155312",
"doi-asserted-by": "publisher",
"key": "cit0021"
},
{
"DOI": "10.1136/bjsm.2005.020842",
"doi-asserted-by": "publisher",
"key": "cit0022"
},
{
"DOI": "10.1002/lsm.22170",
"doi-asserted-by": "publisher",
"key": "cit0023"
},
{
"DOI": "10.1097/DSS.0000000000000904",
"doi-asserted-by": "publisher",
"key": "cit0024"
},
{
"DOI": "10.1089/pho.2009.2484",
"doi-asserted-by": "publisher",
"key": "cit0025"
},
{
"DOI": "10.3346/jkms.2011.26.3.454",
"doi-asserted-by": "publisher",
"key": "cit0026"
},
{
"DOI": "10.1089/pho.2014.3716",
"doi-asserted-by": "publisher",
"key": "cit0027"
},
{
"DOI": "10.3934/biophy.2017.3.337",
"doi-asserted-by": "publisher",
"key": "cit0028"
},
{
"DOI": "10.1007/s10103-015-1814-6",
"doi-asserted-by": "publisher",
"key": "cit0029"
},
{
"DOI": "10.1002/jbio.201600061",
"doi-asserted-by": "publisher",
"key": "cit0030"
},
{
"DOI": "10.1016/j.resp.2014.01.008",
"doi-asserted-by": "publisher",
"key": "cit0031"
},
{
"DOI": "10.1002/lsm.21053",
"doi-asserted-by": "publisher",
"key": "cit0032"
},
{
"DOI": "10.1111/j.1751-1097.2012.01214.x",
"doi-asserted-by": "publisher",
"key": "cit0033"
},
{
"DOI": "10.1007/s10103-020-03119-7",
"doi-asserted-by": "publisher",
"key": "cit0034"
},
{
"DOI": "10.3390/antiox8120640",
"doi-asserted-by": "publisher",
"key": "cit0035"
},
{
"DOI": "10.1080/19420889.2021.1911413",
"doi-asserted-by": "publisher",
"key": "cit0036"
},
{
"DOI": "10.12659/AJCR.926779",
"doi-asserted-by": "publisher",
"key": "cit0037"
},
{
"DOI": "10.29390/cjrt-2020-022",
"doi-asserted-by": "publisher",
"key": "cit0038"
},
{
"DOI": "10.2147/JIR.S301625",
"doi-asserted-by": "publisher",
"key": "cit0039"
},
{
"DOI": "10.1016/j.neuroscience.2015.04.026",
"doi-asserted-by": "publisher",
"key": "cit0040"
},
{
"DOI": "10.1016/j.peptides.2017.02.004",
"doi-asserted-by": "publisher",
"key": "cit0041"
},
{
"author": "Chu M",
"first-page": "9:862",
"journal-title": "Front Immunol",
"key": "cit0042",
"year": "2018"
},
{
"DOI": "10.1016/j.intimp.2018.01.003",
"doi-asserted-by": "publisher",
"key": "cit0043"
},
{
"DOI": "10.1007/s13361-018-1897-y",
"doi-asserted-by": "publisher",
"key": "cit0044"
},
{
"DOI": "10.3390/nu10091188",
"doi-asserted-by": "publisher",
"key": "cit0045"
},
{
"DOI": "10.1158/1078-0432.CCR-18-0172",
"doi-asserted-by": "publisher",
"key": "cit0046"
},
{
"DOI": "10.1016/j.ejmech.2018.05.033",
"doi-asserted-by": "publisher",
"key": "cit0047"
},
{
"DOI": "10.1016/j.envpol.2018.09.148",
"doi-asserted-by": "publisher",
"key": "cit0048"
},
{
"author": "Zhou M",
"first-page": "11",
"journal-title": "Front Pharmacol",
"key": "cit0049",
"year": "2021"
},
{
"DOI": "10.1016/j.jinf.2020.07.016",
"doi-asserted-by": "publisher",
"key": "cit0050"
},
{
"DOI": "10.1155/2021/8874339",
"doi-asserted-by": "publisher",
"key": "cit0051"
},
{
"DOI": "10.1016/j.jaci.2016.08.056",
"doi-asserted-by": "publisher",
"key": "cit0052"
},
{
"DOI": "10.1089/ars.2012.5149",
"doi-asserted-by": "publisher",
"key": "cit0053"
},
{
"DOI": "10.1038/nature09973",
"doi-asserted-by": "publisher",
"key": "cit0054"
}
],
"reference-count": 54,
"references-count": 54,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.tandfonline.com/doi/full/10.1080/19420889.2021.1965718"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Agricultural and Biological Sciences"
],
"subtitle": [],
"title": "Infrared light therapy relieves TLR-4 dependent hyper-inflammation of the type induced by COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1080/tandf_crossmark_01",
"volume": "14"
}