Association of Vitamin D Levels, Race/Ethnicity, and Clinical Characteristics With COVID-19 Test Results
et al., JAMA Netw Open., doi:10.1001/jamanetworkopen.2021.4117, Mar 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 4,638 individuals with vitamin D levels within 1 year before COVID-19 testing, showing higher risk of COVID-19 PCR+ for vitamin D deficient individuals, and lower (but not statistically significant) cases for individuals using vitamin D supplementation.
This is the 56th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
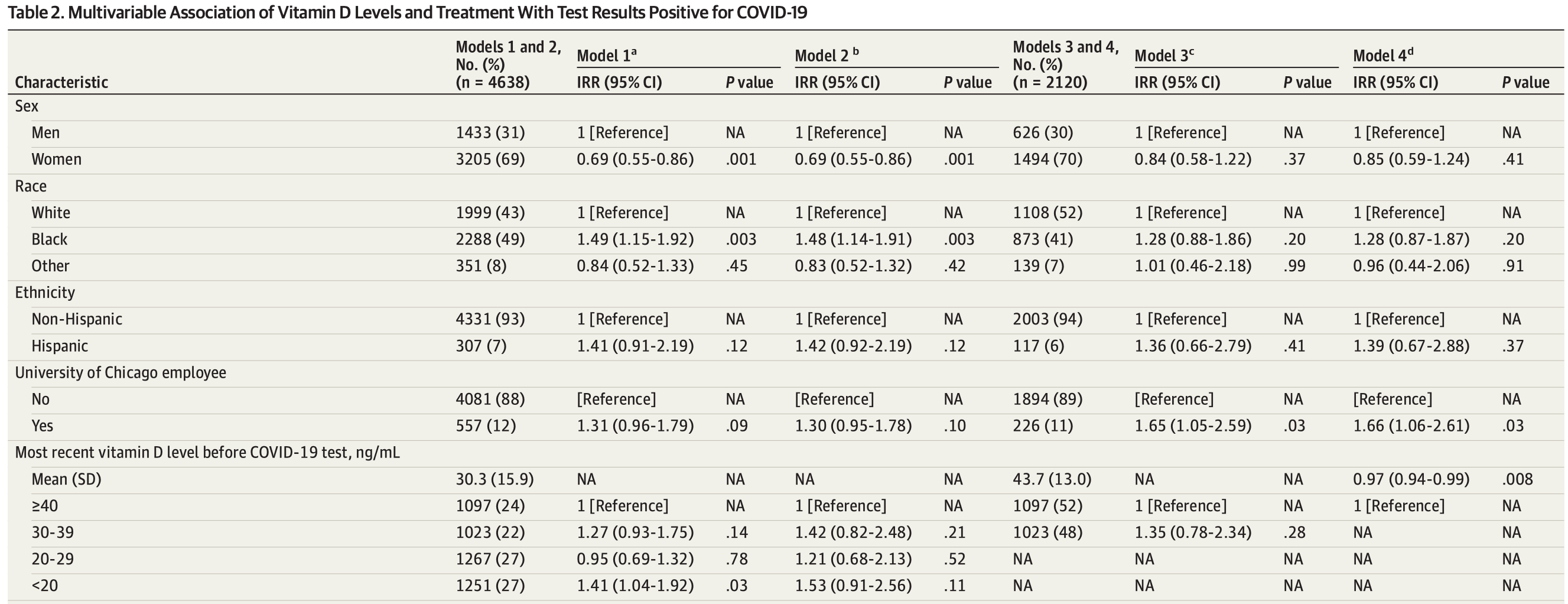
risk of case, 34.6% lower, RR 0.65, p = 0.11, high D levels 61 of 1,097 (5.6%), low D levels 118 of 1,251 (9.4%), NNT 26, adjusted per study, inverted to make RR<1 favor high D levels, >40ng/mL vs. <20ng/mL, Table 2, Model 2.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Meltzer et al., 19 Mar 2021, retrospective, database analysis, USA, peer-reviewed, 6 authors.
Association of Vitamin D Levels, Race/Ethnicity, and Clinical Characteristics With COVID-19 Test Results
JAMA Network Open, doi:10.1001/jamanetworkopen.2021.4117
IMPORTANCE Deficient (ie, <20 ng/mL) or insufficient (ie, 20 to <30 ng/mL) 25-hydroxyvitamin D (also known as calcifediol) levels are more common in Black individuals than White individuals and are associated with increased coronavirus disease 2019 (COVID-19) risk. Whether COVID-19 risk is associated with differences in vitamin D levels of 30 ng/mL or greater is not known. OBJECTIVE To examine whether COVID-19 test results are associated with differences in vitamin D levels of 30 ng/mL or greater, including for White individuals and for Black individuals. DESIGN, SETTING, AND PARTICIPANTS This retrospective cohort study was conducted at an academic medical center in Chicago, Illinois. Participants included individuals with data on vitamin D
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. Additional Contributions: Data from this study were provided by the Clinical Research Data Warehouse (CRDW) maintained by the Center for Research Informatics (CRI) at University of Chicago. The CRI is funded by Clinical and Translational Sciences Award from the Biological Sciences Division of the Institute for Translational Medicine. Thomas Sutton, MS, and Julie Johnson, PhD, MPH, RN (UChicago CRI), appended additional data to the CRDW for this analysis; they were not compensated for this contribution.
References
Baktash, Hosack, Patel, Vitamin D status and outcomes for hospitalised older patients with COVID-19, Postgrad Med J. Published online, doi:10.1136/postgradmedj-2020-138712
Benskin, A basic review of the preliminary evidence that COVID-19 risk and severity is increased in vitamin D deficiency, Front Public Health, doi:10.3389/fpubh.2020.00513
Bergman, Lindh, Björkhem-Bergman, Lindh, Vitamin D and respiratory tract infections: a systematic review and meta-analysis of randomized controlled trials, PLoS One, doi:10.1371/journal.pone.0065835
Bikle, Schwartz, Vitamin D Binding protein, total and free vitamin D levels in different physiological and pathophysiological conditions front, Endocrinol, doi:10.3389/fendo.2019.00317
Billington, Burt, Rose, Safety of high-dose vitamin D supplementation: secondary analysis of a randomized controlled trial, J Clin Endocrinol Metab, doi:10.1210/clinem/dgz212
Blizzard, Hosmer, Parameter estimation and goodness-of-fit in log binomial regression, Biom J, doi:10.1002/bimj.200410165
Boucher, Vitamin D status as a predictor of COVID-19 risk in Black, Asian and other ethnic minority groups in the UK, Diabetes Metab Res Rev, doi:10.1002/dmrr.3375
Bouillon, Schuit, Antonio, Rastinejad, Vitamin D binding protein: a historic overview, Front Endocrinol, doi:10.3389/fendo.2019.00910
Brown, Cohen, Tabor, Zappalà, Maruvada et al., The vitamin D paradox in Black Americans: a systems-based approach to investigating clinical practice, research, and public health-expert panel meeting report, BMC Proc, doi:10.1186/s12919-018-0102-4
Charoenngam, Holick, Immunologic effects of vitamin D on human health and disease, Nutrients, doi:10.3390/nu12072097
Dhaliwal, Mikhail, Feuerman, Aloia, The vitamin d dose response in obesity, Endocr Pract, doi:10.4158/EP13518.OR
Diagnostics, Zhang, Jx, Iwashyna, Christakis, The performance of different lookback periods and sources of information for Charlson comorbidity adjustment in Medicare claims, doi:10.1097/00005650-199911000-00005
Elliott, Binkley, Carnes, Fracture risks for women in long-term care: high prevalence of calcaneal osteoporosis and hypovitaminosis D, Pharmacotherapy, doi:10.1592/phco.23.6.702.32182
Forrest, Stuhldreher, Prevalence and correlates of vitamin D deficiency in US adults, Nutr Res, doi:10.1016/j.nutres.2010.12.001
Freedman, Register, Effect of race and genetics on vitamin D metabolism, bone and vascular health, Nat Rev Nephrol, doi:10.1038/nrneph.2012.112
Frieden, Former, Chief Dr, Tom Frieden, coronavirus infection risk may be reduced by vitamin D. Fox News
Garg, Kim, Whitaker, Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019-COVID-NET, 14 states, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm6915e3
Grant, Lahore, Mcdonnell, Infectious Diseases Association of Vitamin D Levels and Clinical Characteristics With COVID-19 Test Results, Nutrients, doi:10.3390/nu12040988
Hastie, Mackay, Ho, Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.04.050
Holick, Binkley, Bischoff-Ferrari, Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline, J Clin Endocrinol Metab, doi:10.1210/jc.2011-0385
Huotari, Herzig, Vitamin D and living in northern latitudes-an endemic risk area for vitamin D deficiency, Int J Circumpolar Health, doi:10.3402/ijch.v67i2-3.18258
Israel, Cicurel, Feldhamer, Dror, Giveon et al., The link between vitamin D deficiency and COVID-19 in a large population medRxiv, doi:10.1101/2020.09.04.20188268
Kaufman, Niles, Kroll, Bi, Holick, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PLoS One, doi:10.1371/journal.pone.0239252
Libon, Cavalier, Nikkels, Skin color is relevant to vitamin D synthesis, Dermatology, doi:10.1159/000354750
Looker, Johnson, Lacher, Vitamin D Status: United States 2001-2006
Maghbooli, Sahraian, Ebrahimi, Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection, PLoS One, doi:10.1371/journal.pone.0239799
Mardani, Alamdary, Nasab, Gholami, Ahmadi et al., Association of vitamin D with the modulation of the disease severity in COVID-19, Virus Res, doi:10.1016/j.virusres.2020.198148
Martineau, Jolliffe, Hooper, Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data, BMJ, doi:10.1136/bmj.i6583
Mccall, Medical societies advise on vitamin D in midst of COVID-19, Medscape Medical News
Mccullagh, Nelder, Generalized Linear Models, doi:10.1007/978-1-4899-3242-6
Mccullough, Lehrer, Amend, Daily oral dosing of vitamin D 3 using 5000 to 50,000 international units a day in long-term hospitalized patients: insights from a seven year experience, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2018.12.010
Mcnutt, Wu, Xue, Hafner, Estimating the relative risk in cohort studies and clinical trials of common outcomes, Am J Epidemiol, doi:10.1093/aje/kwg074
Meltzer, Best, Zhang, Vokes, Arora et al., Association of vitamin D status and other clinical characteristics with COVID-19 test results, JAMA Netw Open, doi:https://jama.jamanetwork.com/article.aspx?doi=10.1001/jamanetworkopen.2020.19722&utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jamanetworkopen.2021.4117
Merzon, Tworowski, Gorohovski, Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study, FEBS J, doi:10.1111/febs.15495
Mohammad, Mishra, Ashraf, Emerging role of vitamin D and its associated molecules in pathways related to pathogenesis of thrombosis, Biomolecules, doi:10.3390/biom9110649
Oleröd, Hultén, Hammarsten, Klingberg, The variation in free 25-hydroxy vitamin D and vitamin D-binding protein with season and vitamin D status, Endocr Connect, doi:10.1530/EC-16-0078
Pregibon, Data Analytic Methods for Generalized Linear Models
Prietl, Treiber, Pieber, Amrein, Vitamin D and immune function, Nutrients, doi:10.3390/nu5072502
Ross, Dietary Reference Intakes for Calcium and Vitamin D
Sowah, Fan, Dennett, Hagtvedt, Straube, Vitamin D levels and deficiency with different occupations: a systematic review, BMC Public Health, doi:10.1186/s12889-017-4436-z
Supplement, Multivariable Association of Vitamin D Levels and Treatment with Test Results Positive for COVID-19 Among Individuals Reporting White Race eTable 2. COVID-19 Test Positivity Rate by Most Recent Vitamin D Level and by Time Since Most Recent Measurement eTable 3. Multivariable Association of Vitamin D Levels and Treatment with Test Results Positive for COVID-19 Among Individuals With No Active Vitamin D Treatment Before COVID-19 Test eTable 4. Multivariable Association of Vitamin D Levels and Treatment with Test Results Positive for COVID-19 Among Individuals With Active Vitamin D Treatment Before COVID-19 Test eFigure. COVID-19 Test Positivity Rate by Race and by Most Recent Vitamin D Levels Before COVID-19 Tests eAppendix, Supplemental Methods
Viracor, Coronavirus (COVID-19) SARS-CoV-2 RT-PCR
Xue, Moncla, Bedford, Bloom, Within-host evolution of human influenza virus, Trends Microbiol, doi:10.1016/j.tim.2018.02.007
Yancy, COVID-19 and African Americans, JAMA, doi:https://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.2020.6548&utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jamanetworkopen.2021.4117
Zhang, Fang, Tang, Association between vitamin D supplementation and mortality: systematic review and meta-analysis, BMJ, doi:10.1136/bmj.l4673
DOI record:
{
"DOI": "10.1001/jamanetworkopen.2021.4117",
"ISSN": [
"2574-3805"
],
"URL": "http://dx.doi.org/10.1001/jamanetworkopen.2021.4117",
"author": [
{
"affiliation": [
{
"name": "The University of Chicago, Chicago, Illinois"
}
],
"family": "Meltzer",
"given": "David O.",
"sequence": "first"
},
{
"affiliation": [
{
"name": "The University of Chicago, Chicago, Illinois"
}
],
"family": "Best",
"given": "Thomas J.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "The University of Chicago, Chicago, Illinois"
}
],
"family": "Zhang",
"given": "Hui",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "The University of Chicago, Chicago, Illinois"
}
],
"family": "Vokes",
"given": "Tamara",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "The University of Chicago, Chicago, Illinois"
}
],
"family": "Arora",
"given": "Vineet M.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "The University of Chicago, Chicago, Illinois"
}
],
"family": "Solway",
"given": "Julian",
"sequence": "additional"
}
],
"container-title": "JAMA Network Open",
"container-title-short": "JAMA Netw Open",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
3,
19
]
],
"date-time": "2021-03-19T15:30:53Z",
"timestamp": 1616167853000
},
"deposited": {
"date-parts": [
[
2021,
3,
19
]
],
"date-time": "2021-03-19T15:31:23Z",
"timestamp": 1616167883000
},
"indexed": {
"date-parts": [
[
2024,
4,
2
]
],
"date-time": "2024-04-02T15:10:10Z",
"timestamp": 1712070610035
},
"is-referenced-by-count": 50,
"issue": "3",
"issued": {
"date-parts": [
[
2021,
3,
19
]
]
},
"journal-issue": {
"issue": "3",
"published-print": {
"date-parts": [
[
2021,
3,
1
]
]
}
},
"language": "en",
"link": [
{
"URL": "https://jamanetwork.com/journals/jamanetworkopen/articlepdf/2777682/meltzer_2021_oi_210150_1615560090.38365.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "10",
"original-title": [],
"page": "e214117",
"prefix": "10.1001",
"published": {
"date-parts": [
[
2021,
3,
19
]
]
},
"published-online": {
"date-parts": [
[
2021,
3,
19
]
]
},
"publisher": "American Medical Association (AMA)",
"reference": [
{
"DOI": "10.1016/j.nutres.2010.12.001",
"article-title": "Prevalence and correlates of vitamin D deficiency in US adults.",
"author": "Forrest",
"doi-asserted-by": "publisher",
"first-page": "48",
"issue": "1",
"journal-title": "Nutr Res",
"key": "zoi210150r1",
"volume": "31",
"year": "2011"
},
{
"DOI": "10.1210/jc.2011-0385",
"article-title": "Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline.",
"author": "Holick",
"doi-asserted-by": "publisher",
"first-page": "1911",
"issue": "7",
"journal-title": "J Clin Endocrinol Metab",
"key": "zoi210150r2",
"volume": "96",
"year": "2011"
},
{
"DOI": "10.3390/nu12072097",
"article-title": "Immunologic effects of vitamin D on human health and disease.",
"author": "Charoenngam",
"doi-asserted-by": "publisher",
"first-page": "2097",
"issue": "7",
"journal-title": "Nutrients",
"key": "zoi210150r3",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1186/s12919-018-0102-4",
"article-title": "The vitamin D paradox in Black Americans: a systems-based approach to investigating clinical practice, research, and public health—expert panel meeting report.",
"author": "Brown",
"doi-asserted-by": "publisher",
"first-page": "6",
"journal-title": "BMC Proc",
"key": "zoi210150r5",
"volume": "12",
"year": "2018"
},
{
"DOI": "10.1136/bmj.i6583",
"article-title": "Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data.",
"author": "Martineau",
"doi-asserted-by": "publisher",
"first-page": "i6583",
"journal-title": "BMJ",
"key": "zoi210150r6",
"volume": "356",
"year": "2017"
},
{
"DOI": "10.3389/fpubh.2020.00513",
"article-title": "A basic review of the preliminary evidence that COVID-19 risk and severity is increased in vitamin D deficiency.",
"author": "Benskin",
"doi-asserted-by": "publisher",
"first-page": "513",
"journal-title": "Front Public Health",
"key": "zoi210150r7",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0239799",
"article-title": "Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection.",
"author": "Maghbooli",
"doi-asserted-by": "crossref",
"issue": "9",
"journal-title": "PLoS One",
"key": "zoi210150r8",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1136/postgradmedj-2020-138712",
"article-title": "Vitamin D status and outcomes for hospitalised older patients with COVID-19.",
"author": "Baktash",
"doi-asserted-by": "crossref",
"journal-title": "Postgrad Med J",
"key": "zoi210150r9",
"year": "2020"
},
{
"DOI": "10.1016/j.virusres.2020.198148",
"article-title": "Association of vitamin D with the modulation of the disease severity in COVID-19.",
"author": "Mardani",
"doi-asserted-by": "crossref",
"journal-title": "Virus Res",
"key": "zoi210150r10",
"volume": "289",
"year": "2020"
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"article-title": "Association of vitamin D status and other clinical characteristics with COVID-19 test results.",
"author": "Meltzer",
"doi-asserted-by": "crossref",
"issue": "9",
"journal-title": "JAMA Netw Open",
"key": "zoi210150r11",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1111/febs.v287.17",
"article-title": "Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study.",
"author": "Merzon",
"doi-asserted-by": "publisher",
"first-page": "3693",
"issue": "17",
"journal-title": "FEBS J",
"key": "zoi210150r12",
"volume": "287",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0239252",
"article-title": "SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels.",
"author": "Kaufman",
"doi-asserted-by": "crossref",
"issue": "9",
"journal-title": "PLoS One",
"key": "zoi210150r13",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.3390/nu12040988",
"article-title": "Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths.",
"author": "Grant",
"doi-asserted-by": "publisher",
"first-page": "988",
"issue": "4",
"journal-title": "Nutrients",
"key": "zoi210150r15",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1002/dmrr.3375",
"article-title": "Vitamin D status as a predictor of COVID-19 risk in Black, Asian and other ethnic minority groups in the UK.",
"author": "Boucher",
"doi-asserted-by": "crossref",
"issue": "8",
"journal-title": "Diabetes Metab Res Rev",
"key": "zoi210150r16",
"volume": "36",
"year": "2020"
},
{
"DOI": "10.1097/00005650-199911000-00005",
"article-title": "The performance of different lookback periods and sources of information for Charlson comorbidity adjustment in Medicare claims.",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "1128",
"issue": "11",
"journal-title": "Med Care",
"key": "zoi210150r21",
"volume": "37",
"year": "1999"
},
{
"DOI": "10.1093/aje/kwg074",
"article-title": "Estimating the relative risk in cohort studies and clinical trials of common outcomes.",
"author": "McNutt",
"doi-asserted-by": "publisher",
"first-page": "940",
"issue": "10",
"journal-title": "Am J Epidemiol",
"key": "zoi210150r23",
"volume": "157",
"year": "2003"
},
{
"DOI": "10.1002/(ISSN)1521-4036",
"article-title": "Parameter estimation and goodness-of-fit in log binomial regression.",
"author": "Blizzard",
"doi-asserted-by": "publisher",
"first-page": "5",
"issue": "1",
"journal-title": "Biom J",
"key": "zoi210150r25",
"volume": "48",
"year": "2006"
},
{
"DOI": "10.1136/bmj.l4673",
"article-title": "Association between vitamin D supplementation and mortality: systematic review and meta-analysis.",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "l4673",
"journal-title": "BMJ",
"key": "zoi210150r26",
"volume": "366",
"year": "2019"
},
{
"DOI": "10.1038/nrneph.2012.112",
"article-title": "Effect of race and genetics on vitamin D metabolism, bone and vascular health.",
"author": "Freedman",
"doi-asserted-by": "publisher",
"first-page": "459",
"issue": "8",
"journal-title": "Nat Rev Nephrol",
"key": "zoi210150r27",
"volume": "8",
"year": "2012"
},
{
"DOI": "10.1016/j.dsx.2020.04.050",
"article-title": "Vitamin D concentrations and COVID-19 infection in UK Biobank.",
"author": "Hastie",
"doi-asserted-by": "publisher",
"first-page": "561",
"issue": "4",
"journal-title": "Diabetes Metab Syndr",
"key": "zoi210150r28",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.6548",
"article-title": "COVID-19 and African Americans.",
"author": "Yancy",
"doi-asserted-by": "publisher",
"first-page": "1891",
"issue": "19",
"journal-title": "JAMA",
"key": "zoi210150r29",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1159/000354750",
"article-title": "Skin color is relevant to vitamin D synthesis.",
"author": "Libon",
"doi-asserted-by": "publisher",
"first-page": "250",
"issue": "3",
"journal-title": "Dermatology",
"key": "zoi210150r30",
"volume": "227",
"year": "2013"
},
{
"DOI": "10.3389/fendo.2019.00910",
"article-title": "Vitamin D binding protein: a historic overview.",
"author": "Bouillon",
"doi-asserted-by": "publisher",
"first-page": "910",
"journal-title": "Front Endocrinol (Lausanne)",
"key": "zoi210150r31",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1530/EC-16-0078",
"article-title": "The variation in free 25-hydroxy vitamin D and vitamin D-binding protein with season and vitamin D status.",
"author": "Oleröd",
"doi-asserted-by": "publisher",
"first-page": "111",
"issue": "2",
"journal-title": "Endocr Connect",
"key": "zoi210150r32",
"volume": "6",
"year": "2017"
},
{
"article-title": "Binding protein, total and free vitamin D levels in different physiological and pathophysiological conditions front.",
"author": "Bikle",
"first-page": "317",
"journal-title": "Endocrinol",
"key": "zoi210150r33",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1371/journal.pone.0065835",
"article-title": "Vitamin D and respiratory tract infections: a systematic review and meta-analysis of randomized controlled trials.",
"author": "Bergman",
"doi-asserted-by": "crossref",
"issue": "6",
"journal-title": "PLoS One",
"key": "zoi210150r34",
"volume": "8",
"year": "2013"
},
{
"DOI": "10.1016/j.jsbmb.2018.12.010",
"article-title": "Daily oral dosing of vitamin D3 using 5000 to 50,000 international units a day in long-term hospitalized patients: insights from a seven year experience.",
"author": "McCullough",
"doi-asserted-by": "publisher",
"first-page": "228",
"journal-title": "J Steroid Biochem Mol Biol",
"key": "zoi210150r36",
"volume": "189",
"year": "2019"
},
{
"DOI": "10.4158/EP13518.OR",
"article-title": "The vitamin d dose response in obesity.",
"author": "Dhaliwal",
"doi-asserted-by": "publisher",
"first-page": "1258",
"issue": "12",
"journal-title": "Endocr Pract",
"key": "zoi210150r37",
"volume": "20",
"year": "2014"
},
{
"DOI": "10.1210/clinem/dgz212",
"article-title": "Safety of high-dose vitamin D supplementation: secondary analysis of a randomized controlled trial.",
"author": "Billington",
"doi-asserted-by": "crossref",
"issue": "4",
"journal-title": "J Clin Endocrinol Metab",
"key": "zoi210150r38",
"volume": "105",
"year": "2020"
},
{
"DOI": "10.15585/mmwr.mm6915e3",
"article-title": "Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019—COVID-NET, 14 states, March 1-30, 2020.",
"author": "Garg",
"doi-asserted-by": "publisher",
"first-page": "458",
"issue": "15",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "zoi210150r39",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1016/j.tim.2018.02.007",
"article-title": "Within-host evolution of human influenza virus.",
"author": "Xue",
"doi-asserted-by": "publisher",
"first-page": "781",
"issue": "9",
"journal-title": "Trends Microbiol",
"key": "zoi210150r40",
"volume": "26",
"year": "2018"
},
{
"DOI": "10.3390/nu5072502",
"article-title": "Vitamin D and immune function.",
"author": "Prietl",
"doi-asserted-by": "publisher",
"first-page": "2502",
"issue": "7",
"journal-title": "Nutrients",
"key": "zoi210150r41",
"volume": "5",
"year": "2013"
},
{
"DOI": "10.3390/biom9110649",
"article-title": "Emerging role of vitamin D and its associated molecules in pathways related to pathogenesis of thrombosis.",
"author": "Mohammad",
"doi-asserted-by": "publisher",
"first-page": "649",
"issue": "11",
"journal-title": "Biomolecules",
"key": "zoi210150r42",
"volume": "9",
"year": "2019"
},
{
"DOI": "10.15585/mmwr.mm6915e6",
"article-title": "Characteristics of Health Care Personnel with COVID-19—United States, February 12-April 9, 2020.",
"author": "CDC COVID-19 Response Team",
"doi-asserted-by": "publisher",
"first-page": "477",
"issue": "15",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "zoi210150r44",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.3402/ijch.v67i2-3.18258",
"article-title": "Vitamin D and living in northern latitudes—an endemic risk area for vitamin D deficiency.",
"author": "Huotari",
"doi-asserted-by": "publisher",
"first-page": "164",
"issue": "2-3",
"journal-title": "Int J Circumpolar Health",
"key": "zoi210150r45",
"volume": "67",
"year": "2008"
},
{
"DOI": "10.1592/phco.23.6.702.32182",
"article-title": "Fracture risks for women in long-term care: high prevalence of calcaneal osteoporosis and hypovitaminosis D.",
"author": "Elliott",
"doi-asserted-by": "publisher",
"first-page": "702",
"issue": "6",
"journal-title": "Pharmacotherapy",
"key": "zoi210150r46",
"volume": "23",
"year": "2003"
},
{
"DOI": "10.1186/s12889-017-4436-z",
"article-title": "Vitamin D levels and deficiency with different occupations: a systematic review.",
"author": "Sowah",
"doi-asserted-by": "publisher",
"first-page": "519",
"issue": "1",
"journal-title": "BMC Public Health",
"key": "zoi210150r47",
"volume": "17",
"year": "2017"
},
{
"author": "Del Valle",
"key": "zoi210150r4",
"volume-title": "Dietary Reference Intakes for Calcium and Vitamin D.",
"year": "2011"
},
{
"DOI": "10.1007/978-1-4899-3242-6",
"author": "McCullagh",
"doi-asserted-by": "crossref",
"edition": "2nd ed",
"key": "zoi210150r22",
"volume-title": "Generalized Linear Models",
"year": "1989"
},
{
"author": "Looker",
"key": "zoi210150r35",
"volume-title": "Vitamin D Status: United States 2001–2006. NCHS Data Brief, No 59",
"year": "2011"
},
{
"DOI": "10.1101/2020.09.04.20188268",
"doi-asserted-by": "crossref",
"key": "zoi210150r14",
"unstructured": "Israel? A, Assi Cicurel? AA, Feldhamer? I, Dror? Y, Giveon? SM, Gillis? D, Strich? D, Lavie? G. The link between vitamin D deficiency and COVID-19 in a large population? medRxiv. doi:10.1101/2020.09.04.20188268"
},
{
"key": "zoi210150r17",
"unstructured": "Centers for Disease Control and Prevention. CDC Diagnostic Tests for COVID-19. Accessed July 13, 2020. https://www.cdc.gov/coronavirus/2019-ncov/lab/testing.html"
},
{
"key": "zoi210150r18",
"unstructured": "Eurofins Viracor. Coronavirus (COVID-19) SARS-CoV-2 RT-PCR. Accessed July 13, 2020. https://www.viracor-eurofins.com/test-menu/8300-coronavirus-covid-19-sars-cov-2-rt-pcr/"
},
{
"key": "zoi210150r19",
"unstructured": "Roche Diagnostics. Cobas SARS-CoV-2 Test (for the COVID-19 coronavirus). Accessed July 13 2020. https://diagnostics.roche.com/us/en/products/params/cobas-sars-cov-2-test.html"
},
{
"key": "zoi210150r20",
"unstructured": "Centers for Disease Control and Prevention. International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). Accessed February 15, 2021. https://www.cdc.gov/nchs/icd/icd10cm.htm"
},
{
"key": "zoi210150r24",
"unstructured": "Pregibon? D. Data Analytic Methods for Generalized Linear Models. Dissertation. University of Toronto; 1979."
},
{
"key": "zoi210150r43",
"unstructured": "National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases. Preparing for COVID-19 in nursing homes. Accessed April 27, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care.html"
},
{
"key": "zoi210150r48",
"unstructured": "Frieden? T. Former CDC Chief Dr. Tom Frieden: coronavirus infection risk may be reduced by vitamin D. Fox News. March 23, 2020. Accessed April 13, 2020. https://www.foxnews.com/opinion/former-cdc-chief-tom-frieden-coronavirus-risk-may-be-reduced-with-vitamin-d"
},
{
"key": "zoi210150r49",
"unstructured": "McCall? B. Medical societies advise on vitamin D in midst of COVID-19. Medscape Medical News. July 10, 2020. Accessed July 10, 2020. https://www.medscape.com/viewarticle/933715"
}
],
"reference-count": 49,
"references-count": 49,
"relation": {},
"resource": {
"primary": {
"URL": "https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2777682"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Association of Vitamin D Levels, Race/Ethnicity, and Clinical Characteristics With COVID-19 Test Results",
"type": "journal-article",
"volume": "4"
}
