Diet quality and risk and severity of COVID-19: a prospective cohort study
et al., Gut, doi:10.1136/gutjnl-2021-325353, Jun 2021 (preprint)
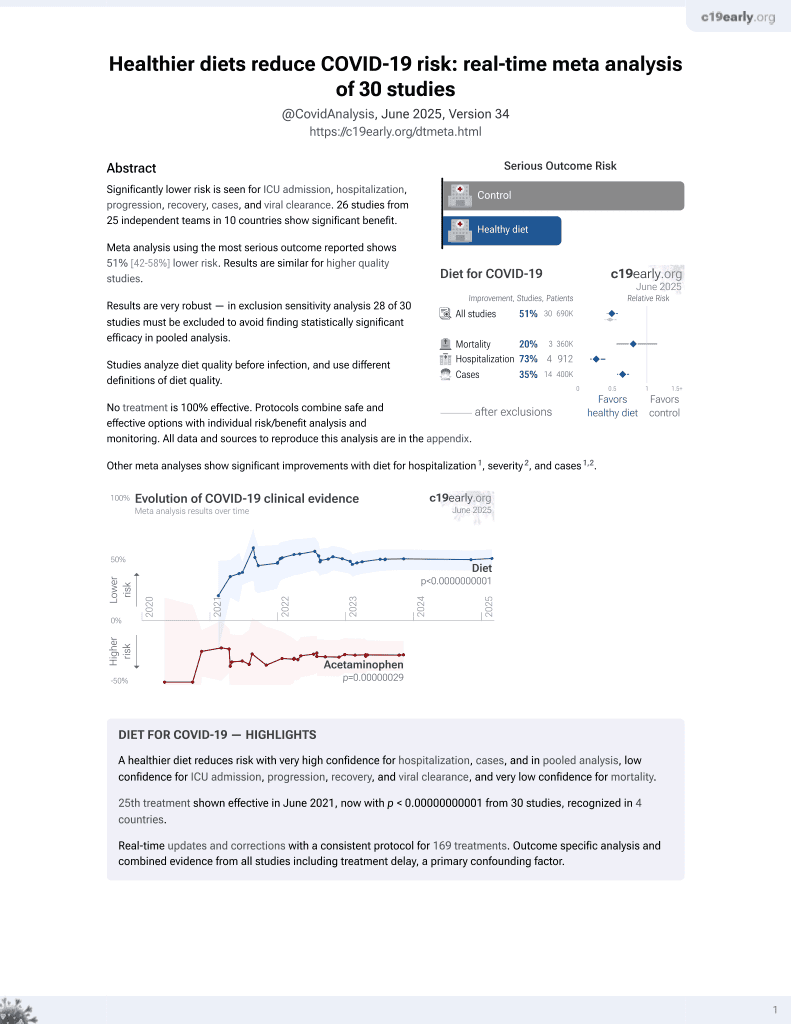
Diet for COVID-19
26th treatment shown to reduce risk in
June 2021, now with p < 0.00000000001 from 30 studies, recognized in 4 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 592,571 participants in the UK and USA with 31,815 COVID-19 cases, showing lower risk or COVID-19 cases and severity for higher healthful plant-based diet scores. Notably, the assocation was less evident with higher levels of physical activity.
|
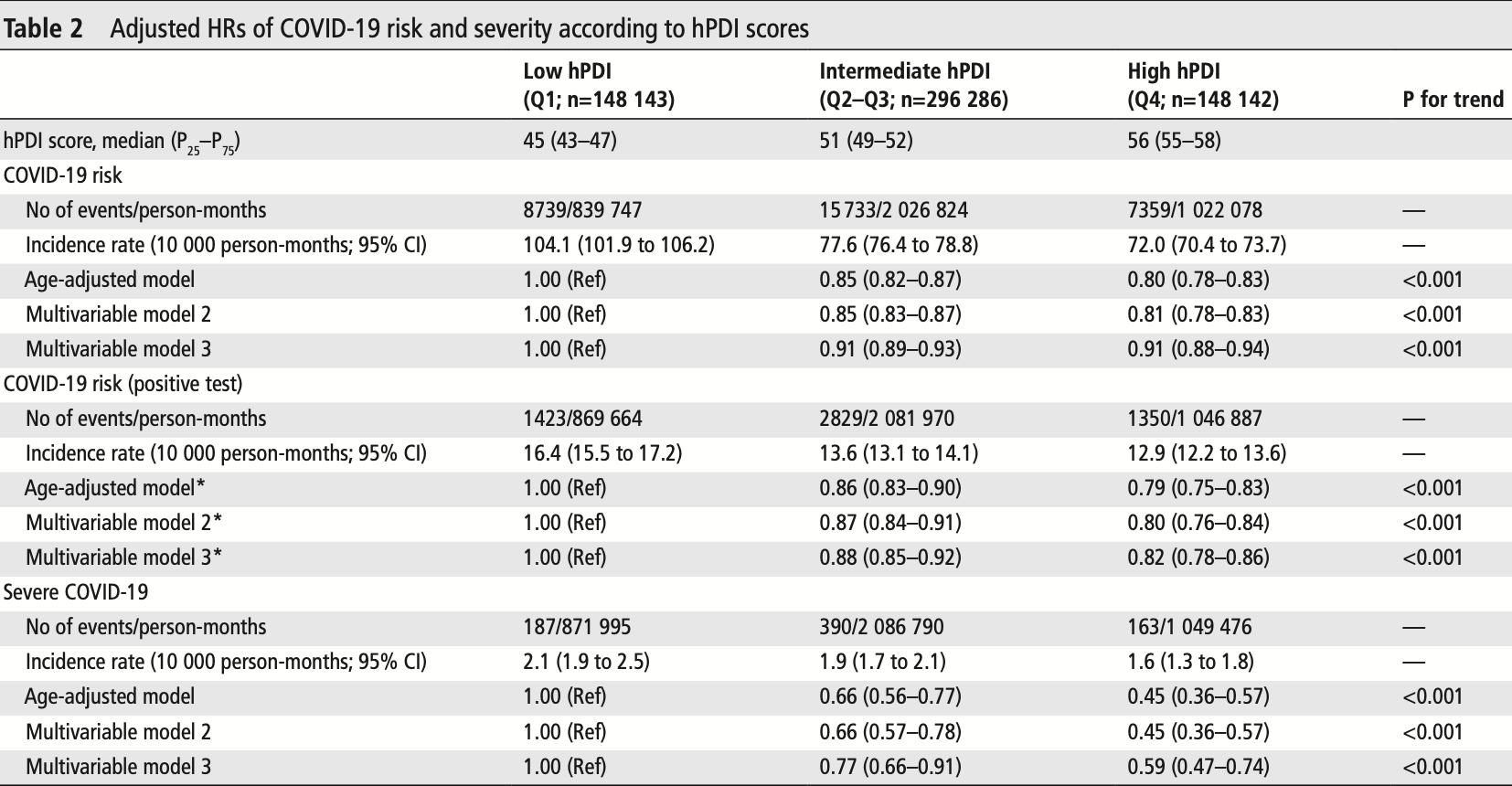
risk of severe case, 41.0% lower, HR 0.59, p < 0.001, higher quality diet 148,142, lower quality diet 148,143, adjusted per study, model 3, high vs. low hPDI, multivariable, Cox proportional hazards.
|
|
risk of case, 18.0% lower, HR 0.82, p < 0.001, higher quality diet 148,142, lower quality diet 148,143, adjusted per study, model 3, high vs. low hPDI, PCR+, multivariable, Cox proportional hazards.
|
|
risk of case, 9.0% lower, HR 0.91, p < 0.001, higher quality diet 148,142, lower quality diet 148,143, adjusted per study, model 3, high vs. low hPDI, multivariable, Cox proportional hazards.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Merino et al., 25 Jun 2021, retrospective, multiple countries, peer-reviewed, survey, 30 authors, study period 24 March, 2020 - 2 December, 2020.
Diet quality and risk and severity of COVID-19: a prospective cohort study
Gut, doi:10.1136/gutjnl-2021-325353
Objective Poor metabolic health and unhealthy lifestyle factors have been associated with risk and severity of COVID-19, but data for diet are lacking. We aimed to investigate the association of diet quality with risk and severity of COVID-19 and its interaction with socioeconomic deprivation. Design We used data from 592 571 participants of the smartphone-based COVID-19 Symptom Study. Diet information was collected for the prepandemic period using a short food frequency questionnaire, and diet quality was assessed using a healthful Plant-Based Diet Score, which emphasises healthy plant foods such as fruits or vegetables. Multivariable Cox models were fitted to calculate HRs and 95% CIs for COVID-19 risk and severity defined using a validated symptom-based algorithm or hospitalisation with oxygen support, respectively. Results Over 3 886 274 person-months of follow-up, 31 815 COVID-19 cases were documented. Compared with individuals in the lowest quartile of the diet score, high diet quality was associated with lower risk of COVID-19 (HR 0.91; 95% CI 0.88 to 0.94) and severe COVID-19 (HR 0.59; 95% CI 0.47 to 0.74). The joint association of low diet quality and increased deprivation on COVID-19 risk was higher than the sum of the risk associated with each factor alone (P interaction =0.005). The corresponding absolute excess rate per 10 000 person/months for lowest vs highest quartile of diet score was 22.5 (95% CI 18.8 to 26.3) among persons living in areas with low deprivation and 40.8 (95% CI 31.7 to 49.8) among persons living in areas with high deprivation. Conclusions A diet characterised by healthy plantbased foods was associated with lower risk and severity of COVID-19. This association may be particularly evident among individuals living in areas with higher socioeconomic deprivation.
INTRODUCTION Poor metabolic health linked to conditions such as obesity, type 2 diabetes or hypertension 1 2 has been associated with increased risk and severity of COVID-19, and excess adiposity or preexisting liver disease might be causally associated with increased risk of death from COVID-19. 3 4 Underlying these conditions is the contribution of a diet, which may be independently associated with COVID-19 risk and severity.
Significance of this study What is already known on this subject? ► Poor metabolic health and unhealthy lifestyle behaviours have been associated with higher risk and severity of COVID-19. ► Improved nutrition, especially in the context of socioeconomic deprivation, has been shown to reduce the burden of certain infectious diseases in the past. Evidence on the association of diet quality with susceptibility and progression of COVID-19 is lacking.
What are the new findings? ► A dietary pattern characterised by healthy plant-based foods was associated with lower risk and severity of COVID-19. ► We found evidence of a synergistic association of poor diet and increased socioeconomic deprivation with COVID-19 risk that was higher than..
Ethics approval The study protocol was approved by the Mass General Brigham Human Research Committee (protocol 2020P000909) and King's College London Ethics Committee (REMAS ID 18210, LRS-19/20-18210). Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement The diet quality data used for this study are held by the department of Twin Research at Kings' College London. The data can be released to bona fide researchers using our normal procedures overseen by the Wellcome Trust and its guidelines as part of our core funding (https:// web. www. healthdatagateway. org/ dataset/ fddcb382-3051-4394-8436-b92295f14259). Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
ORCID iDs Jordi Merino http:// orcid. org/ 0000-0001-8312-1438 Amit D Joshi http:// orcid. org/ 0000-0001-7581-6934 Long H..
References
Belanger, Hill, Angelidi, Covid-19 and disparities in nutrition and obesity, N Engl J Med, doi:10.1056/NEJMp2021264
Botti-Lodovico, Rosenberg, Sabeti, Testing in a Pandemic -Improving Access, Coordination, and Prioritization, N Engl J Med, doi:10.1056/NEJMp2025173
Brooks, Butler, Redfield, Universal masking to prevent SARS-CoV-2 Transmission-The time is now, JAMA, doi:10.1001/jama.2020.13107
Calder, Nutrition, immunity and COVID-19, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2020-000085
Chiuve, Fung, Rimm, Alternative dietary indices both strongly predict risk of chronic disease, J Nutr, doi:10.3945/jn.111.157222
Cleghorn, Harrison, Ransley, Can a dietary quality score derived from a short-form FFQ assess dietary quality in UK adult population surveys?, Public Health Nutr
Cleghorn, Harrison, Ransley, Can a dietary quality score derived from a short-form FFQ assess dietary quality in UK adult population surveys?, Public Health Nutr, doi:10.1017/S1368980016001099
Country, None, UK
Drew, Nguyen, Steves, Rapid implementation of mobile technology for real-time epidemiology of COVID-19, Science, doi:10.1126/science.abc0473
Eiser, Could dietary factors reduce COVID-19 mortality rates? Moderating the inflammatory state, J Altern Complement Med, doi:10.1089/acm.2020.0441
Feldman, Bassett, The relationship between neighborhood poverty and COVID-19 mortality within racial/ethnic groups
Gut, on this supplemental material which has been supplied by the author, doi:10.1136/gutjnl-2021-325353-9.:102021
Jw, Ltd, Tds, Sb, Abrams, Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study, Lancet, doi:10.1016/S0140-6736(20)31189-2
Kim, Rebholz, Hegde, Plant-Based diets, pescatarian diets and COVID-19 severity: a population-based case-control study in six countries, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2021-000272
Lancet, Endocrinology, Metabolic health: a priority for the post-pandemic era, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(21)00058-9
Leong, Cole, Brenner, Cardiometabolic risk factors for COVID-19 susceptibility and severity: a Mendelian randomization analysis, PLoS Med, doi:10.1371/journal.pmed.1003553
Ley, Hamdy, Mohan, Prevention and management of type 2 diabetes: dietary components and nutritional strategies, Lancet, doi:10.1016/S0140-6736(14)60613-9
Louca, Murray, Klaser, Modest effects of dietary supplements during the COVID-19 pandemic: insights from 445 850 users of the COVID-19 symptom study APP, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2021-000250
Marmot, Smith, Stansfeld, Health inequalities among British civil servants: the Whitehall II study, Lancet, doi:10.1016/0140-6736(91)93068-K
Mazidi, Kengne, Higher adherence to plant-based diets are associated with lower likelihood of fatty liver, Clin Nutr, doi:10.1016/j.clnu.2018.08.010
Mazidi, Leming, Merino, of 1.1 million UK and US individuals
Mazidii, Leming, Merino, Impact of COVID-19 on health behaviours and body weight: a prospective observational study in a cohort of 1.1 million UK and US individuals
Mena, Martinez, Mahmud, Socioeconomic status determines COVID-19 incidence and related mortality in Santiago, Chile, Science, doi:10.1126/science.abg5298
Menni, Valdes, Freidin, Real-Time tracking of self-reported symptoms to predict potential COVID-19, Nat Med, doi:10.1038/s41591-020-0916-2
Menni, Valdes, Freidin, Real-time tracking of self-reported symptoms to predict potential COVID-19, Nat Med
Messer, Laraia, Kaufman, The development of a standardized neighborhood deprivation index, J Urban Health, doi:10.1007/s11524-006-9094-x
O'hearn, Liu, Cudhea, Coronavirus disease 2019 hospitalizations attributable to cardiometabolic conditions in the United States: a comparative risk assessment analysis, J Am Heart Assoc, doi:10.1161/JAHA.120.019259
Race E, None, White
Rehm, Peñalvo, Afshin, Dietary intake among US adults, 1999-2012, JAMA, doi:10.1001/jama.2016.7491
Satija, Bhupathiraju, Rimm, Plant-Based dietary patterns and incidence of type 2 diabetes in US men and women: results from three prospective cohort studies, PLoS Med, doi:10.1371/journal.pmed.1002039
Satija, Bhupathiraju, Spiegelman, Healthful and Unhealthful Plant-Based Diets and the Risk of Coronary Heart Disease in U.S. Adults, J Am Coll Cardiol, doi:10.1016/j.jacc.2017.05.047
Savolainen, Lind, Bergström, Biomarkers of food intake and nutrient status are associated with glucose tolerance status and development of type 2 diabetes in older Swedish women, Am J Clin Nutr, doi:10.3945/ajcn.117.152850
Schoenfeld, Partial residuals for the proportional hazards regression model, Biometrika, doi:10.1093/biomet/69.1.239
Singh, Khan, Clinical characteristics and outcomes of coronavirus disease 2019 among patients with preexisting liver disease in the United States: a multicenter research network study, Gastroenterology, doi:10.1053/j.gastro.2020.04.064
Storm, Den Hertog, Van Oers, How to improve collaboration between the public health sector and other policy sectors to reduce health inequalities? -A study in sixteen municipalities in the Netherlands, Int J Equity Health, doi:10.1186/s12939-016-0384-y
Toutenburg, Rubin, multiple imputation for nonresponse in surveys, Statistical Papers, doi:10.1007/BF02924688
Vanderweele, Tchetgen, Attributing effects to interactions, Epidemiology, doi:10.1097/EDE.0000000000000096
Vanderweele, Tchetgen, Gut, Attributing effects to interactions, Merino J ³18, doi:10.1136/gutjnl-2021-325353-9.:102021
Varsavsky, Graham, Canas, Detecting COVID-19 infection hotspots in England using large-scale self-reported data from a mobile application: a prospective, observational study, Lancet Public Health, doi:10.1016/S2468-2667(20)30269-3
Willett, Stampfer, Current evidence on healthy eating, Annu Rev Public Health, doi:10.1146/annurev-publhealth-031811-124646
Wise, Covid-19: highest death rates seen in countries with most overweight populations, BMJ, doi:10.1136/bmj.n623
Yan, Chu, Yang, Characterization of the lipidomic profile of human coronavirus-infected cells: implications for lipid metabolism remodeling upon coronavirus replication, Viruses, doi:10.3390/v11010073
DOI record:
{
"DOI": "10.1136/gutjnl-2021-325353",
"ISSN": [
"0017-5749",
"1468-3288"
],
"URL": "http://dx.doi.org/10.1136/gutjnl-2021-325353",
"abstract": "<jats:sec><jats:title>Objective</jats:title><jats:p>Poor metabolic health and unhealthy lifestyle factors have been associated with risk and severity of COVID-19, but data for diet are lacking. We aimed to investigate the association of diet quality with risk and severity of COVID-19 and its interaction with socioeconomic deprivation.</jats:p></jats:sec><jats:sec><jats:title>Design</jats:title><jats:p>We used data from 592 571 participants of the smartphone-based COVID-19 Symptom Study. Diet information was collected for the prepandemic period using a short food frequency questionnaire, and diet quality was assessed using a healthful Plant-Based Diet Score, which emphasises healthy plant foods such as fruits or vegetables. Multivariable Cox models were fitted to calculate HRs and 95% CIs for COVID-19 risk and severity defined using a validated symptom-based algorithm or hospitalisation with oxygen support, respectively.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>Over 3 886 274 person-months of follow-up, 31 815 COVID-19 cases were documented. Compared with individuals in the lowest quartile of the diet score, high diet quality was associated with lower risk of COVID-19 (HR 0.91; 95% CI 0.88 to 0.94) and severe COVID-19 (HR 0.59; 95% CI 0.47 to 0.74). The joint association of low diet quality and increased deprivation on COVID-19 risk was higher than the sum of the risk associated with each factor alone (P<jats:sub>interaction</jats:sub>=0.005). The corresponding absolute excess rate per 10 000 person/months for lowest vs highest quartile of diet score was 22.5 (95% CI 18.8 to 26.3) among persons living in areas with low deprivation and 40.8 (95% CI 31.7 to 49.8) among persons living in areas with high deprivation.</jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p>A diet characterised by healthy plant-based foods was associated with lower risk and severity of COVID-19. This association may be particularly evident among individuals living in areas with higher socioeconomic deprivation.</jats:p></jats:sec>",
"alternative-id": [
"10.1136/gutjnl-2021-325353"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-8312-1438",
"affiliation": [],
"authenticated-orcid": false,
"family": "Merino",
"given": "Jordi",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-7581-6934",
"affiliation": [],
"authenticated-orcid": false,
"family": "Joshi",
"given": "Amit D",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5436-4219",
"affiliation": [],
"authenticated-orcid": false,
"family": "Nguyen",
"given": "Long H",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0531-4901",
"affiliation": [],
"authenticated-orcid": false,
"family": "Leeming",
"given": "Emily R",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mazidi",
"given": "Mohsen",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8813-0816",
"affiliation": [],
"authenticated-orcid": false,
"family": "Drew",
"given": "David A",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gibson",
"given": "Rachel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Graham",
"given": "Mark S",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8202-4513",
"affiliation": [],
"authenticated-orcid": false,
"family": "Lo",
"given": "Chun-Han",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Capdevila",
"given": "Joan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Murray",
"given": "Benjamin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hu",
"given": "Christina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Selvachandran",
"given": "Somesh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hammers",
"given": "Alexander",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bhupathiraju",
"given": "Shilpa N",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sharma",
"given": "Shreela V",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sudre",
"given": "Carole",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Astley",
"given": "Christina M",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chavarro",
"given": "Jorge E",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kwon",
"given": "Sohee",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ma",
"given": "Wenjie",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9790-0571",
"affiliation": [],
"authenticated-orcid": false,
"family": "Menni",
"given": "Cristina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Willett",
"given": "Walter C",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ourselin",
"given": "Sebastien",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Steves",
"given": "Claire J",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wolf",
"given": "Jonathan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Franks",
"given": "Paul W",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Spector",
"given": "Timothy D",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Berry",
"given": "Sarah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chan",
"given": "Andrew T",
"sequence": "additional"
}
],
"container-title": [
"Gut"
],
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2021,
9,
6
]
],
"date-time": "2021-09-06T17:54:34Z",
"timestamp": 1630950874000
},
"deposited": {
"date-parts": [
[
2021,
10,
26
]
],
"date-time": "2021-10-26T16:11:54Z",
"timestamp": 1635264714000
},
"funder": [
{
"DOI": "10.13039/100000062",
"award": [
"K01DK110267",
"K01DK120742",
"K23DK120899",
"K23DK125838",
"P30DK046200",
"P30DK40561"
],
"doi-asserted-by": "publisher",
"name": "National Institute of Diabetes and Digestive and Kidney Diseases"
},
{
"DOI": "10.13039/501100000320",
"award": [
"AS-JF-17-011"
],
"doi-asserted-by": "publisher",
"name": "Alzheimer's Society"
},
{
"DOI": "10.13039/501100007602",
"award": [
"MR/M016560/1"
],
"doi-asserted-by": "publisher",
"name": "Programme Grants for Applied Research"
},
{
"DOI": "10.13039/501100000266",
"award": [
"T213038/Z/18/Z"
],
"doi-asserted-by": "publisher",
"name": "Engineering and Physical Sciences Research Council"
},
{
"DOI": "10.13039/100000050",
"award": [
"U01HL145386"
],
"doi-asserted-by": "publisher",
"name": "National Heart, Lung, and Blood Institute"
},
{
"DOI": "10.13039/100009560",
"award": [
"AGA2021-5102"
],
"doi-asserted-by": "publisher",
"name": "American Gastroenterological Association"
},
{
"DOI": "10.13039/100000041",
"award": [
"7-21-JDFM-005"
],
"doi-asserted-by": "publisher",
"name": "American Diabetes Association"
},
{
"award": [
"MassCPR-003"
],
"name": "The Massachusetts Consortium on Pathogen Readiness"
},
{
"DOI": "10.13039/100000066",
"award": [
"R24ES028521"
],
"doi-asserted-by": "publisher",
"name": "National Institute of Environmental Health Sciences"
},
{
"DOI": "10.13039/100004440",
"award": [
"T213038/Z/18/Z",
"WT203148/Z/16/Z",
"WT212904/Z/18/Z"
],
"doi-asserted-by": "publisher",
"name": "Wellcome Trust"
},
{
"DOI": "10.13039/100000054",
"award": [
"R35 CA253185"
],
"doi-asserted-by": "crossref",
"name": "National Cancer Institute"
},
{
"DOI": "10.13039/100005294",
"award": [
"Stuart and Suzanne Steele MGH Research Scholar"
],
"doi-asserted-by": "publisher",
"name": "Massachusetts General Hospital"
}
],
"indexed": {
"date-parts": [
[
2022,
4,
5
]
],
"date-time": "2022-04-05T16:07:22Z",
"timestamp": 1649174842831
},
"is-referenced-by-count": 13,
"issn-type": [
{
"type": "print",
"value": "0017-5749"
},
{
"type": "electronic",
"value": "1468-3288"
}
],
"issue": "11",
"issued": {
"date-parts": [
[
2021,
9,
6
]
]
},
"journal-issue": {
"issue": "11",
"published-online": {
"date-parts": [
[
2021,
10,
7
]
]
},
"published-print": {
"date-parts": [
[
2021,
11
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://bmj.com/coronavirus/usage",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
9,
6
]
],
"date-time": "2021-09-06T00:00:00Z",
"timestamp": 1630886400000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/gutjnl-2021-325353",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "2096-2104",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2021,
9,
6
]
]
},
"published-online": {
"date-parts": [
[
2021,
9,
6
]
]
},
"published-print": {
"date-parts": [
[
2021,
11
]
]
},
"publisher": "BMJ",
"reference": [
{
"DOI": "10.1016/S0140-6736(20)31189-2",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.1"
},
{
"article-title": "Metabolic health: a priority for the post-pandemic era",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2021102608050536000_70.11.2096.2",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1053/j.gastro.2020.04.064",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.3"
},
{
"DOI": "10.1371/journal.pmed.1003553",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.4"
},
{
"DOI": "10.1016/j.jacc.2017.05.047",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.5"
},
{
"DOI": "10.3945/jn.111.157222",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.6"
},
{
"DOI": "10.1016/S0140-6736(14)60613-9",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.7"
},
{
"DOI": "10.1146/annurev-publhealth-031811-124646",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.8"
},
{
"DOI": "10.1371/journal.pmed.1002039",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.9"
},
{
"DOI": "10.1016/j.clnu.2018.08.010",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.10"
},
{
"DOI": "10.1016/0140-6736(91)93068-K",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.11"
},
{
"DOI": "10.1056/nejmp2021264",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.12"
},
{
"DOI": "10.1001/jama.2016.7491",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.13"
},
{
"DOI": "10.1186/s12939-016-0384-y",
"article-title": "How to improve collaboration between the public health sector and other policy sectors to reduce health inequalities? - A study in sixteen municipalities in the Netherlands",
"author": "Storm",
"doi-asserted-by": "crossref",
"journal-title": "Int J Equity Health",
"key": "2021102608050536000_70.11.2096.14",
"volume": "15",
"year": "2016"
},
{
"DOI": "10.1136/bmjnph-2021-000272",
"article-title": "Plant-Based diets, pescatarian diets and COVID-19 severity: a population-based case-control study in six countries",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "257",
"journal-title": "BMJ Nutr Prev Health",
"key": "2021102608050536000_70.11.2096.15",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1126/science.abc0473",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.16"
},
{
"DOI": "10.21203/rs.3.rs-179013/v1",
"doi-asserted-by": "crossref",
"key": "2021102608050536000_70.11.2096.17",
"unstructured": "Mazidii M , Leming E , Merino J . Impact of COVID-19 on health behaviours and body weight: a prospective observational study in a cohort of 1.1 million UK and US individuals. Research Square [Preprint] 2021."
},
{
"DOI": "10.1017/S1368980016001099",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.18"
},
{
"DOI": "10.1038/s41591-020-0916-2",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.19"
},
{
"DOI": "10.1016/S2468-2667(20)30269-3",
"article-title": "Detecting COVID-19 infection hotspots in England using large-scale self-reported data from a mobile application: a prospective, observational study",
"author": "Varsavsky",
"doi-asserted-by": "crossref",
"first-page": "e21",
"journal-title": "Lancet Public Health",
"key": "2021102608050536000_70.11.2096.20",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1056/nejmp2025173",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.21"
},
{
"key": "2021102608050536000_70.11.2096.22",
"unstructured": "Indices of deprivation. Available: https://www.gov.uk/government/publications/english-indices-of-deprivation-2019-technical-report [Accessed 18 Jan 2021]."
},
{
"DOI": "10.1007/s11524-006-9094-x",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.23"
},
{
"DOI": "10.1007/BF02924688",
"article-title": "Rubin, D.B.: multiple imputation for nonresponse in surveys",
"author": "Toutenburg",
"doi-asserted-by": "crossref",
"first-page": "180",
"journal-title": "Statistical Papers",
"key": "2021102608050536000_70.11.2096.24",
"volume": "31",
"year": "1990"
},
{
"DOI": "10.1093/biomet/69.1.239",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.25"
},
{
"DOI": "10.1097/EDE.0000000000000096",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.26"
},
{
"DOI": "10.1136/bmjnph-2020-000085",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.27"
},
{
"DOI": "10.3390/v11010073",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.28"
},
{
"DOI": "10.1136/bmjnph-2021-000250",
"article-title": "Modest effects of dietary supplements during the COVID-19 pandemic: insights from 445 850 users of the COVID-19 symptom study APP",
"author": "Louca",
"doi-asserted-by": "crossref",
"first-page": "149",
"journal-title": "BMJ Nutr Prev Health",
"key": "2021102608050536000_70.11.2096.29",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1089/acm.2020.0441",
"article-title": "Could dietary factors reduce COVID-19 mortality rates? Moderating the inflammatory state",
"author": "Eiser",
"doi-asserted-by": "crossref",
"first-page": "176",
"journal-title": "J Altern Complement Med",
"key": "2021102608050536000_70.11.2096.30",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1161/JAHA.120.019259",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.31"
},
{
"DOI": "10.1136/bmj.n623",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.32"
},
{
"DOI": "10.1126/science.abg5298",
"doi-asserted-by": "publisher",
"key": "2021102608050536000_70.11.2096.33"
},
{
"DOI": "10.1101/2020.10.04.20206318",
"doi-asserted-by": "crossref",
"key": "2021102608050536000_70.11.2096.34",
"unstructured": "Feldman JM , Bassett MT . The relationship between neighborhood poverty and COVID-19 mortality within racial/ethnic groups (Cook County, Illinois). medRxiv 2020:2020.10.04.20206318."
},
{
"DOI": "10.1001/jama.2020.13107",
"article-title": "Universal masking to prevent SARS-CoV-2 Transmission-The time is now",
"author": "Brooks",
"doi-asserted-by": "crossref",
"first-page": "635",
"journal-title": "JAMA",
"key": "2021102608050536000_70.11.2096.35",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.3945/ajcn.117.152850",
"article-title": "Biomarkers of food intake and nutrient status are associated with glucose tolerance status and development of type 2 diabetes in older Swedish women",
"author": "Savolainen",
"doi-asserted-by": "crossref",
"first-page": "ajcn152850",
"journal-title": "Am J Clin Nutr",
"key": "2021102608050536000_70.11.2096.36",
"volume": "106",
"year": "2017"
}
],
"reference-count": 36,
"references-count": 36,
"relation": {},
"resource": {
"primary": {
"URL": "https://gut.bmj.com/lookup/doi/10.1136/gutjnl-2021-325353"
}
},
"score": 1,
"short-container-title": [
"Gut"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Gastroenterology"
],
"subtitle": [],
"title": [
"Diet quality and risk and severity of COVID-19: a prospective cohort study"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy",
"volume": "70"
}