Risk factors for developing COVID-19: a population-based longitudinal study (COVIDENCE UK)
et al., Thorax, doi:10.1136/thoraxjnl-2021-217487, COVIDENCE UK, NCT04330599, Mar 2021
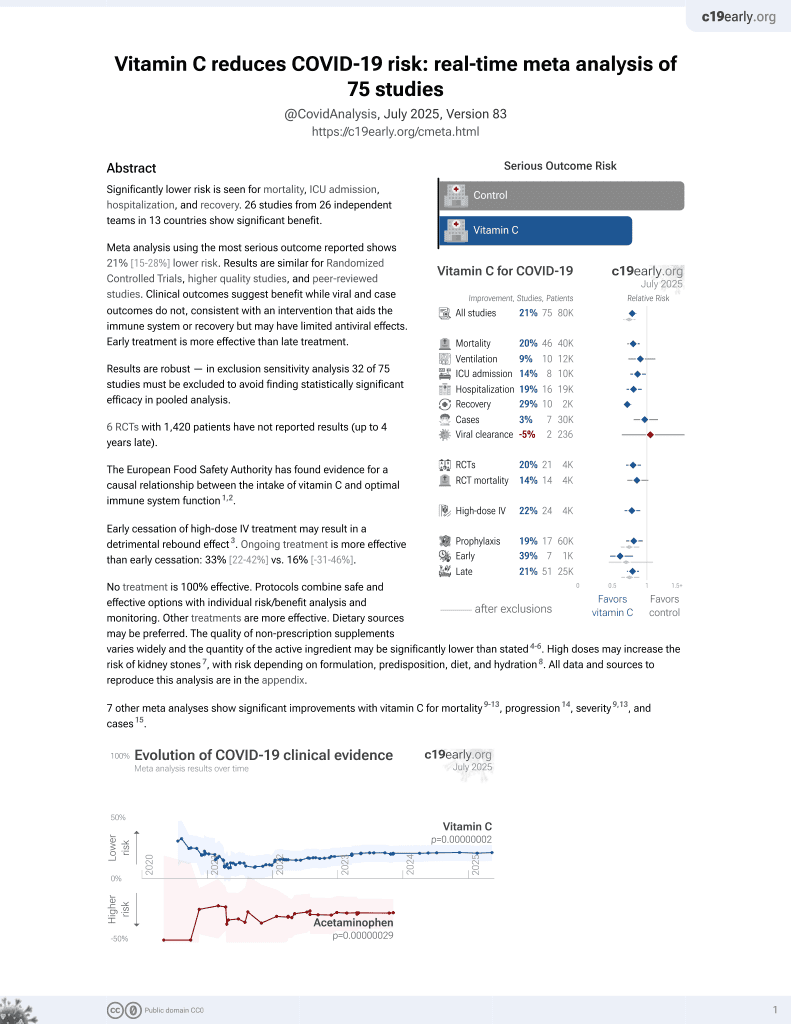
Vitamin C for COVID-19
6th treatment shown to reduce risk in
September 2020, now with p = 0.000000068 from 74 studies, recognized in 22 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
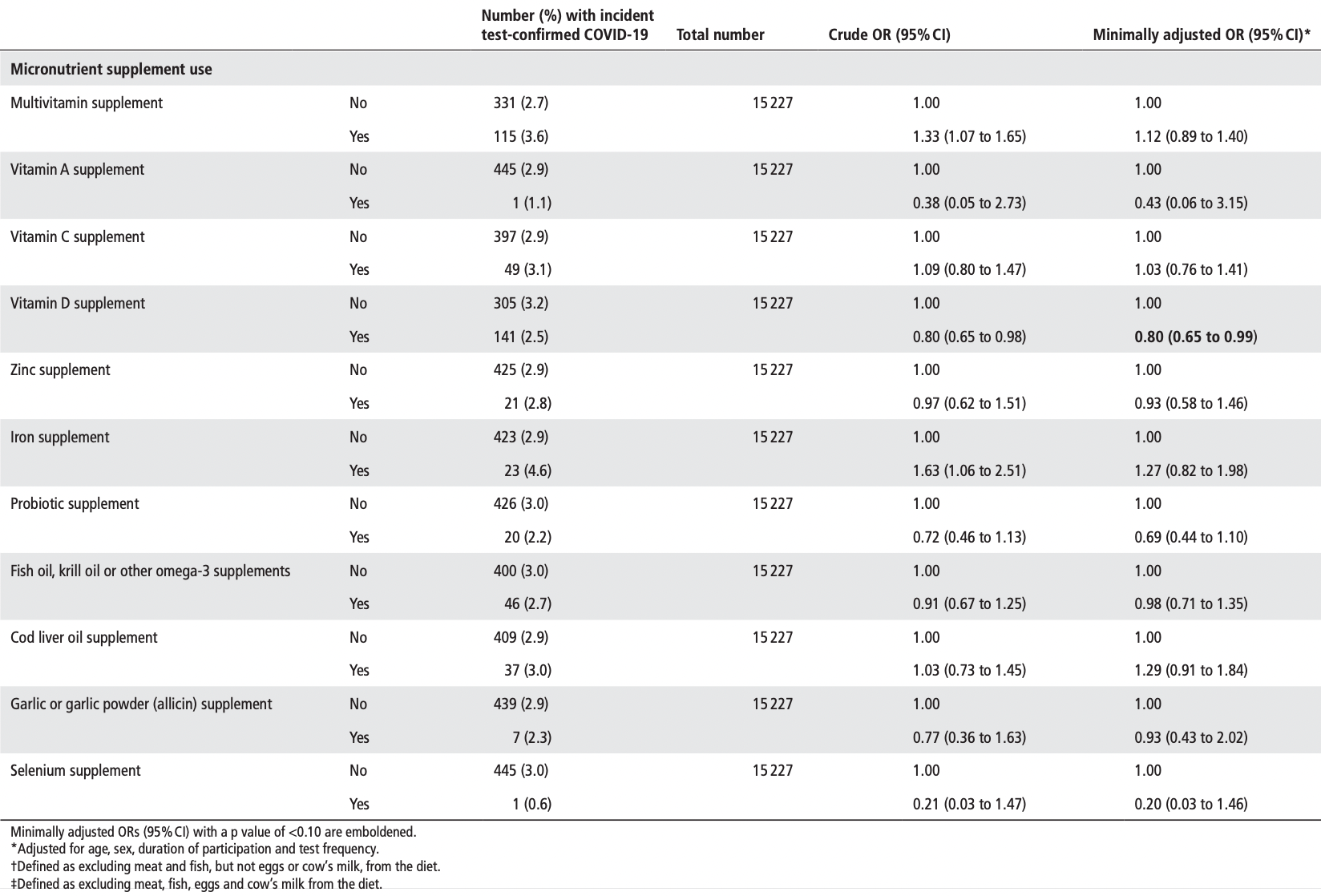
Prospective survey-based study with 15,227 people in the UK, showing lower risk of COVID-19 cases with vitamin A, vitamin D, zinc, selenium, probiotics, and inhaled corticosteroids; and higher risk with metformin and vitamin C. Statistical significance was not reached for any of these. Except for vitamin D, the results for treatments we follow were only adjusted for age, sex, duration of participation, and test frequency.
Meta-analysis of all vitamin C studies shows benefit for clinical outcomes but not for viral or case outcomes, consistent with an intervention that may have limited or no direct antiviral effect, but minimizes progression via other mechanisms (for example by aiding the immune system, minimizing immune over-activation, minizing secondary complications, or aiding recovery).
This is the 17th of 74 COVID-19 controlled studies for vitamin C, which collectively show efficacy with p=0.000000068.
21 studies are RCTs, which show efficacy with p=0.0012.
This study is excluded in the after exclusion results of meta-analysis:
significant unadjusted confounding possible.
Study covers vitamin D, sleep, exercise, vitamin C, vitamin A, zinc, probiotics, metformin, budesonide, and selenium.
|
risk of case, 2.9% higher, RR 1.03, p = 0.86, treatment 49 of 1,580 (3.1%), control 397 of 13,647 (2.9%), adjusted per study, odds ratio converted to relative risk, minimally adjusted, group sizes approximated.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Holt et al., 30 Mar 2021, prospective, United Kingdom, peer-reviewed, 34 authors, study period 1 May, 2020 - 5 February, 2021, trial NCT04330599 (history) (COVIDENCE UK).
Contact: a.martineau@qmul.ac.uk.
Risk factors for developing COVID-19: a population-based longitudinal study (COVIDENCE UK)
Thorax, doi:10.1136/thoraxjnl-2021-217487
Background Risk factors for severe COVID-19 include older age, male sex, obesity, black or Asian ethnicity and underlying medical conditions. Whether these factors also influence susceptibility to developing COVID-19 is uncertain. Methods We undertook a prospective, populationbased cohort study (COVIDENCE UK) from 1 May 2020 to 5 February 2021. Baseline information on potential risk factors was captured by an online questionnaire. Monthly follow-up questionnaires captured incident COVID-19. We used logistic regression models to estimate multivariable-adjusted ORs (aORs) for associations between potential risk factors and odds of COVID-19.
Results We recorded 446 incident cases of COVID-19 in 15 227 participants (2.9%). Increased odds of developing COVID-19 were independently associated with Asian/Asian British versus white ethnicity (aOR 2.28, 95% CI 1.33 to 3.91), household overcrowding (aOR per additional 0.5 people/bedroom 1.26, 1.11 to 1.43), any versus no visits to/from other households in previous week (aOR 1.31, 1.06 to 1.62), number of visits to indoor public places (aOR per extra visit per week 1.05, 1.02 to 1.09), frontline occupation excluding health/social care versus no frontline occupation (aOR 1.49, 1.12 to 1.98) and raised body mass index (BMI) (aOR 1.50 (1.19 to 1.89) for BMI 25.0-30.0 kg/m 2 and 1.39 (1.06 to 1.84) for BMI >30.0 kg/m 2 versus BMI <25.0 kg/m 2 ). Atopic disease was independently associated with decreased odds (aOR 0.75, 0.59 to 0.97). No independent associations were seen for age, sex, other medical conditions, diet or micronutrient supplement use. Conclusions After rigorous adjustment for factors influencing exposure to SARS-CoV-2, Asian/Asian British ethnicity and raised BMI were associated with increased odds of developing COVID-19, while atopic disease was associated with decreased odds. Trial registration number ClinicalTrials. gov Registry (NCT04330599).
INTRODUCTION COVID-19 has taken a heavy toll on the health of populations globally. [1][2][3] Risk factors for severe and fatal disease are well recognised, and include male sex, black or Asian ethnic origin, obesity, deprivation and a range of comorbidities including diabetes mellitus, cardiovascular disease, COPD and hypertension. 4 5 Characterisation of risks for milder disease has been relatively neglected, but is important, both from a public health perspective (since it drives transmission to individuals at risk of severe disease), and from a biological perspective (since understanding susceptibility factors can provide insights into pathogenesis). There is growing evidence from population-based studies to suggest that at least some risk factors for
Key messages
What is the key question? ► How do demographic, socioeconomic, lifestyle, dietary, pharmacological and comorbidity factors relate to the risk of developing COVID-19 in the general adult population of the UK? What is the bottom line? ► After rigorous adjustment for factors..
Supplementary Appendix: Risk factors for developing COVID-19: a population-based longitudinal study (COVIDENCE UK)
Table of Contents Supplementary
Supplementary Methods
Sample size The sample size required to detect an odds ratio of at least 1.08 (effect size) for a binary exposure variable with maximum variability (probability = 0.50 changing to 0.52) and correlated with other variables in the model (R 2 = 0.4), with a power of 90% using a two-sided test with 5% significance level was estimated as 10,964, using the 'powerlog' program in Stata 14.2 (College Station, TX). Assuming 10% censoring at baseline (prevalent COVID-19 and missing) and 20% loss to follow-up, we aimed to recruit a minimum of 15,228 participants. No upper limit for sample size was specified.
Statistical methods Statistical analyses were performed using Stata 14.2. Putative risk factors for COVID-19 were selected a priori and classified into the following groups: socio-demographic, occupational and lifestyle factors; longstanding medical conditions, medication use and vaccination status; and diet and supplemental micronutrient intake. To produce patient-level covariates for each class of medications investigated, participant answers were mapped to drug classes listed on the British National Formulary (BNF) or the DrugBank and Electronic Medicines Compendium databases if not explicitly listed on the BNF; further details of the computational methods used to achieve this are presented in supplementary..
References
Aburto, Kashyap, Schöley, Estimating the burden of the COVID-19 pandemic on mortality, life expectancy and lifespan inequality in England and Wales: a population-level analysis, J Epidemiol Community Health, doi:10.1136/jech-2020-215505
Bhala, Curry, Martineau, Sharpening the global focus on ethnicity and race in the time of COVID-19, Lancet, doi:10.1016/S0140-6736(20)31102-8
Clift, Coupland, Keogh, Living risk prediction algorithm (QCOVID) for risk of hospital admission and mortality from coronavirus 19 in adults: national derivation and validation cohort study, BMJ, doi:10.1136/bmj.m3731
Cramér, Mathematical Methods of Statistics
Cramér, Mathematical Methods of Statistics
De Lusignan, Dorward, Correa, Risk factors for SARS-CoV-2 among patients in the Oxford Royal College of general practitioners research and surveillance centre primary care network: a cross-sectional study, Lancet Infect Dis, doi:10.1016/S1473-3099(20)30371-6
Ding, Vanderweele, Sensitivity Analysis Without Assumptions, Epidemiology
Ding, Vanderweele, Sensitivity Analysis Without Assumptions, Epidemiology
Ding, Vanderweele, Sensitivity analysis without assumptions, Epidemiology, doi:10.1097/EDE.0000000000000457
Doll, Hill, Mortality in relation to smoking: ten years' observations of British doctors, Br Med J, doi:10.1136/bmj.1.5396.1460
Griffith, Morris, Tudball, Collider bias undermines our understanding of COVID-19 disease risk and severity, Nat Commun, doi:10.1038/s41467-020-19478-2
Hamer, Kivimäki, Gale, Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: a community-based cohort study of 387,109 adults in UK, Brain Behav Immun, doi:10.1016/j.bbi.2020.05.059
Ho, Celis-Morales, Gray, Modifiable and non-modifiable risk factors for COVID-19, and comparison to risk factors for influenza and pneumonia: results from a UK Biobank prospective cohort study, BMJ Open, doi:10.1136/bmjopen-2020-040402
Jackson, Busse, Bacharier, Association of respiratory allergy, asthma, and expression of the SARS-CoV-2 receptor ACE2, J Allergy Clin Immunol
Jackson, Busse, Bacharier, Association of respiratory allergy, asthma, and expression of the SARS-CoV-2 receptor ACE2, J Allergy Clin Immunol
Jackson, Busse, Bacharier, Association of respiratory allergy, asthma, and expression of the SARS-CoV-2 receptor ACE2, J Allergy Clin Immunol, doi:10.1016/j.jaci.2020.04.009
Levenshtein, Binary codes capable of correcting deletions, insertions, and reversals, Soviet Physics Doklady
Levenshtein, Binary codes capable of correcting deletions, insertions, and reversals, Soviet Physics Doklady
Linden, Mathur, Vanderweele, Conducting sensitivity analysis for unmeasured confounding in observational studies using E-values: The evalue package, The Stata Journal
Linden, Mathur, Vanderweele, Conducting sensitivity analysis for unmeasured confounding in observational studies using E-values: The evalue package, The Stata Journal
Linden, Mathur, Vanderweele, Conducting sensitivity analysis for unmeasured confounding in observational studies using E-values: the evalue package, Stata J, doi:10.1177/1536867X20909696
Louca, Murray, Klaser, Modest effects of dietary supplements during the COVID-19 pandemic: insights from 445 850 users of the COVID-19 symptom study APP, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2021-000250
Ma, Zhou, Heianza, Habitual use of vitamin D supplements and risk of coronavirus disease 2019 (COVID-19) infection: a prospective study in UK Biobank, Am J Clin Nutr, doi:10.1093/ajcn/nqaa381
Martineau, Forouhi, Vitamin D for COVID-19: a case to answer?, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30268-0
Mathur, Rentsch, Ethnic differences in COVID-19 infection, hospitalisation, and mortality: an OpenSAFELY analysis of 17 million adults in England
Menni, Valdes, Freidin, Real-Time tracking of self-reported symptoms to predict potential COVID-19, Nat Med, doi:10.1038/s41591-020-0916-2
Menni, Valdes, Freidin, Real-time tracking of self-reported symptoms to predict potential COVID-19, Nat Med
Menni, Valdes, Freidin, Real-time tracking of self-reported symptoms to predict potential COVID-19, Nat Med
Miller, Becker, Grenfell, Disease and healthcare burden of COVID-19 in the United States, Nat Med, doi:10.1038/s41591-020-0952-y
Philips, Hanging on the Metaphone, Computer Language
Philips, Hanging on the Metaphone, Computer Language
Pifarré I Arolas, Acosta, López-Casasnovas, Years of life lost to COVID-19 in 81 countries, Sci Rep, doi:10.1038/s41598-021-83040-3
Popkin, Du, Green, Individuals with obesity and COVID-19: a global perspective on the epidemiology and biological relationships, Obes Rev, doi:10.1111/obr.13128
Rothman, No adjustments are needed for multiple comparisons, Epidemiology
Rothman, No adjustments are needed for multiple comparisons, Epidemiology
Rothman, No adjustments are needed for multiple comparisons, Epidemiology, doi:10.1097/00001648-199001000-00010
Stringhini, Wisniak, Piumatti, Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): a population-based study, Lancet, doi:10.1016/S0140-6736(20)31304-0
Venkatesan, The changing demographics of COVID-19, Lancet Respir Med, doi:10.1016/S2213-2600(20)30461-6
Ward, Atchison, Whitaker, Antibody prevalence for SARS-CoV-2 following the peak of the pandemic in England: REACT2 study in 100,000 adults
Williamson, Walker, Bhaskaran, Factors associated with COVID-19-related death using OpenSAFELY, Nature, doi:10.1038/s41586-020-2521-4
DOI record:
{
"DOI": "10.1136/thoraxjnl-2021-217487",
"ISSN": [
"0040-6376",
"1468-3296"
],
"URL": "http://dx.doi.org/10.1136/thoraxjnl-2021-217487",
"abstract": "<jats:sec><jats:title>Background</jats:title><jats:p>Risk factors for severe COVID-19 include older age, male sex, obesity, black or Asian ethnicity and underlying medical conditions. Whether these factors also influence susceptibility to developing COVID-19 is uncertain.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>We undertook a prospective, population-based cohort study (COVIDENCE UK) from 1 May 2020 to 5 February 2021. Baseline information on potential risk factors was captured by an online questionnaire. Monthly follow-up questionnaires captured incident COVID-19. We used logistic regression models to estimate multivariable-adjusted ORs (aORs) for associations between potential risk factors and odds of COVID-19.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>We recorded 446 incident cases of COVID-19 in 15 227 participants (2.9%). Increased odds of developing COVID-19 were independently associated with Asian/Asian British versus white ethnicity (aOR 2.28, 95% CI 1.33 to 3.91), household overcrowding (aOR per additional 0.5 people/bedroom 1.26, 1.11 to 1.43), any versus no visits to/from other households in previous week (aOR 1.31, 1.06 to 1.62), number of visits to indoor public places (aOR per extra visit per week 1.05, 1.02 to 1.09), frontline occupation excluding health/social care versus no frontline occupation (aOR 1.49, 1.12 to 1.98) and raised body mass index (BMI) (aOR 1.50 (1.19 to 1.89) for BMI 25.0–30.0 kg/m<jats:sup>2</jats:sup> and 1.39 (1.06 to 1.84) for BMI >30.0 kg/m<jats:sup>2</jats:sup> versus BMI <25.0 kg/m<jats:sup>2</jats:sup>). Atopic disease was independently associated with decreased odds (aOR 0.75, 0.59 to 0.97). No independent associations were seen for age, sex, other medical conditions, diet or micronutrient supplement use.</jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p>After rigorous adjustment for factors influencing exposure to SARS-CoV-2, Asian/Asian British ethnicity and raised BMI were associated with increased odds of developing COVID-19, while atopic disease was associated with decreased odds.</jats:p></jats:sec><jats:sec><jats:title>Trial registration number</jats:title><jats:p>ClinicalTrials.gov Registry (<jats:ext-link xmlns:xlink=\"http://www.w3.org/1999/xlink\" ext-link-type=\"clintrialgov\" xlink:href=\"NCT04330599\">NCT04330599</jats:ext-link>).</jats:p></jats:sec>",
"alternative-id": [
"10.1136/thoraxjnl-2021-217487"
],
"author": [
{
"affiliation": [],
"family": "Holt",
"given": "Hayley",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-6901-3665",
"affiliation": [],
"authenticated-orcid": false,
"family": "Talaei",
"given": "Mohammad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Greenig",
"given": "Matthew",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zenner",
"given": "Dominik",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Symons",
"given": "Jane",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Relton",
"given": "Clare",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Young",
"given": "Katherine S",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Davies",
"given": "Molly R",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Thompson",
"given": "Katherine N",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ashman",
"given": "Jed",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rajpoot",
"given": "Sultan Saeed",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kayyale",
"given": "Ahmed Ali",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9194-479X",
"affiliation": [],
"authenticated-orcid": false,
"family": "El Rifai",
"given": "Sarah",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6946-0780",
"affiliation": [],
"authenticated-orcid": false,
"family": "Lloyd",
"given": "Philippa J",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jolliffe",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Timmis",
"given": "Olivia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Finer",
"given": "Sarah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Iliodromiti",
"given": "Stamatina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Miners",
"given": "Alec",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3235-0454",
"affiliation": [],
"authenticated-orcid": false,
"family": "Hopkinson",
"given": "Nicholas S",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alam",
"given": "Bodrul",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8191-4389",
"affiliation": [],
"authenticated-orcid": false,
"family": "Lloyd-Jones",
"given": "Graham",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dietrich",
"given": "Thomas",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chapple",
"given": "Iain",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0369-2885",
"affiliation": [],
"authenticated-orcid": false,
"family": "Pfeffer",
"given": "Paul E",
"sequence": "additional"
},
{
"affiliation": [],
"family": "McCoy",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Davies",
"given": "Gwyneth",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lyons",
"given": "Ronan A",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Griffiths",
"given": "Christopher",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0606-8167",
"affiliation": [],
"authenticated-orcid": false,
"family": "Kee",
"given": "Frank",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sheikh",
"given": "Aziz",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Breen",
"given": "Gerome",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shaheen",
"given": "Seif O",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5387-1721",
"affiliation": [],
"authenticated-orcid": false,
"family": "Martineau",
"given": "Adrian R",
"sequence": "additional"
}
],
"clinical-trial-number": [
{
"clinical-trial-number": "nct04330599",
"registry": "10.18810/clinical-trials-gov"
}
],
"container-title": [
"Thorax"
],
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2021,
12,
1
]
],
"date-time": "2021-12-01T01:05:17Z",
"timestamp": 1638320717000
},
"deposited": {
"date-parts": [
[
2021,
12,
1
]
],
"date-time": "2021-12-01T01:05:34Z",
"timestamp": 1638320734000
},
"funder": [
{
"award": [
"MC_PC_19004"
],
"name": "Health Data Research UK"
},
{
"DOI": "10.13039/100015652",
"award": [
"MGU0466"
],
"doi-asserted-by": "publisher",
"name": "Barts Charity"
}
],
"indexed": {
"date-parts": [
[
2022,
1,
3
]
],
"date-time": "2022-01-03T07:26:40Z",
"timestamp": 1641194800324
},
"is-referenced-by-count": 1,
"issn-type": [
{
"type": "print",
"value": "0040-6376"
},
{
"type": "electronic",
"value": "1468-3296"
}
],
"issued": {
"date-parts": [
[
2021,
11,
30
]
]
},
"language": "en",
"license": [
{
"URL": "https://bmj.com/coronavirus/usage",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
11,
30
]
],
"date-time": "2021-11-30T00:00:00Z",
"timestamp": 1638230400000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/thoraxjnl-2021-217487",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "thoraxjnl-2021-217487",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2021,
11,
30
]
]
},
"published-online": {
"date-parts": [
[
2021,
11,
30
]
]
},
"publisher": "BMJ",
"reference": [
{
"DOI": "10.1136/jech-2020-215505",
"doi-asserted-by": "publisher",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.1"
},
{
"DOI": "10.1038/s41591-020-0952-y",
"article-title": "Disease and healthcare burden of COVID-19 in the United States",
"author": "Miller",
"doi-asserted-by": "crossref",
"first-page": "1212",
"journal-title": "Nat Med",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.2",
"volume": "26",
"year": "2020"
},
{
"article-title": "Years of life lost to COVID-19 in 81 countries",
"author": "Pifarré I Arolas",
"journal-title": "Sci Rep",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.3",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1136/bmj.m3731",
"doi-asserted-by": "publisher",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.4"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"doi-asserted-by": "publisher",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.5"
},
{
"DOI": "10.1016/S2213-2600(20)30461-6",
"article-title": "The changing demographics of COVID-19",
"author": "Venkatesan",
"doi-asserted-by": "crossref",
"journal-title": "Lancet Respir Med",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.6",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1101/2020.08.12.20173690",
"doi-asserted-by": "crossref",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.7",
"unstructured": "Ward H , Atchison C , Whitaker M . Antibody prevalence for SARS-CoV-2 following the peak of the pandemic in England: REACT2 study in 100,000 adults. MedRxiv 2020."
},
{
"DOI": "10.1016/S0140-6736(20)31304-0",
"doi-asserted-by": "publisher",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.8"
},
{
"DOI": "10.1016/S0140-6736(20)31102-8",
"doi-asserted-by": "publisher",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.9"
},
{
"DOI": "10.1016/S2213-8587(20)30268-0",
"article-title": "Vitamin D for COVID-19: a case to answer?",
"author": "Martineau",
"doi-asserted-by": "crossref",
"first-page": "735",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.10",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/j.bbi.2020.05.059",
"doi-asserted-by": "publisher",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.11"
},
{
"DOI": "10.1038/s41591-020-0916-2",
"doi-asserted-by": "publisher",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.12"
},
{
"DOI": "10.1038/s41467-020-19478-2",
"doi-asserted-by": "publisher",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.13"
},
{
"DOI": "10.1097/00001648-199001000-00010",
"doi-asserted-by": "publisher",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.14"
},
{
"DOI": "10.1097/EDE.0000000000000457",
"doi-asserted-by": "publisher",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.15"
},
{
"DOI": "10.1177/1536867X20909696",
"article-title": "Conducting sensitivity analysis for unmeasured confounding in observational studies using E-values: the evalue package",
"author": "Linden",
"doi-asserted-by": "crossref",
"first-page": "162",
"journal-title": "Stata J",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.16",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1016/j.jaci.2020.04.009",
"article-title": "Association of respiratory allergy, asthma, and expression of the SARS-CoV-2 receptor ACE2",
"author": "Jackson",
"doi-asserted-by": "crossref",
"first-page": "203",
"journal-title": "J Allergy Clin Immunol",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.17",
"volume": "146",
"year": "2020"
},
{
"key": "2021113017051049000_thoraxjnl-2021-217487v1.18",
"unstructured": "Mathur R , Rentsch CT , The OpenSAFELY Collaborative . Ethnic differences in COVID-19 infection, hospitalisation, and mortality: an OpenSAFELY analysis of 17 million adults in England. MedRxiv 2020."
},
{
"DOI": "10.1111/obr.13128",
"article-title": "Individuals with obesity and COVID-19: a global perspective on the epidemiology and biological relationships",
"author": "Popkin",
"doi-asserted-by": "crossref",
"journal-title": "Obes Rev",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.19",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1136/bmjopen-2020-040402",
"doi-asserted-by": "publisher",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.20"
},
{
"DOI": "10.1016/S1473-3099(20)30371-6",
"doi-asserted-by": "publisher",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.21"
},
{
"DOI": "10.1093/ajcn/nqaa381",
"article-title": "Habitual use of vitamin D supplements and risk of coronavirus disease 2019 (COVID-19) infection: a prospective study in UK Biobank",
"author": "Ma",
"doi-asserted-by": "crossref",
"first-page": "1275",
"journal-title": "Am J Clin Nutr",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.22",
"volume": "113",
"year": "2021"
},
{
"DOI": "10.1136/bmjnph-2021-000250",
"article-title": "Modest effects of dietary supplements during the COVID-19 pandemic: insights from 445 850 users of the COVID-19 symptom study APP",
"author": "Louca",
"doi-asserted-by": "crossref",
"first-page": "149",
"journal-title": "BMJ Nutr Prev Health",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.23",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1136/bmj.1.5396.1460",
"doi-asserted-by": "publisher",
"key": "2021113017051049000_thoraxjnl-2021-217487v1.24"
}
],
"reference-count": 24,
"references-count": 24,
"relation": {},
"score": 1,
"short-container-title": [
"Thorax"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Pulmonary and Respiratory Medicine"
],
"subtitle": [],
"title": [
"Risk factors for developing COVID-19: a population-based longitudinal study (COVIDENCE UK)"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy"
}
holt