Modifiable and non-modifiable risk factors for COVID-19, and comparison to risk factors for influenza and pneumonia: results from a UK Biobank prospective cohort study
et al., BMJ Open, doi:10.1136/bmjopen-2020-040402, Nov 2020
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
UK Biobank retrospective 235,928 participants using walking pace as a proxy for physical fitness, showing lower risk of COVID-19 hospitalization with an average vs. slow walking pace.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
|
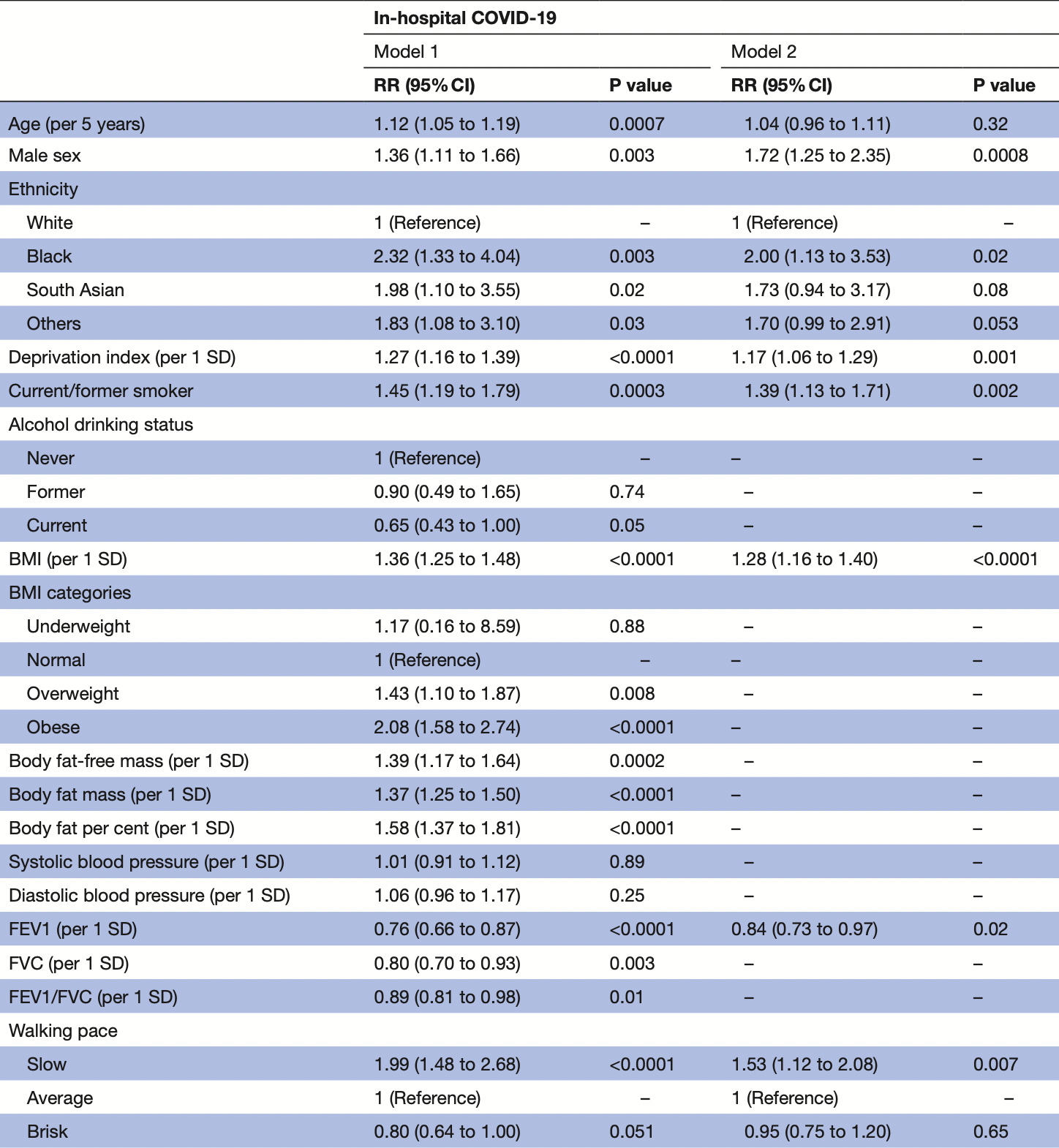
risk of hospitalization, 34.6% lower, RR 0.65, p = 0.007, high activity levels 213 of 123,588 (0.2%), low activity levels 59 of 14,887 (0.4%), adjusted per study, inverted to make RR<1 favor high activity levels, model 2, average vs. slow walking pace, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Ho et al., 19 Nov 2020, retrospective, United Kingdom, peer-reviewed, survey, 13 authors.
Modifiable and non-modifiable risk factors for COVID-19, and comparison to risk factors for influenza and pneumonia: results from a UK Biobank prospective cohort study
BMJ Open, doi:10.1136/bmjopen-2020-040402
Objectives We aimed to investigate demographic, lifestyle, socioeconomic and clinical risk factors for COVID-19, and compared them to risk factors for pneumonia and influenza in UK Biobank. Design Cohort study. Setting UK Biobank. Participants 49-83 year olds (in 2020) from a general population study. Main outcome measures Confirmed COVID-19 infection (positive SARS-CoV-2 test). Incident influenza and pneumonia were obtained from primary care data. Poisson regression was used to study the association of exposure variables with outcomes. Results Among 235 928 participants, 397 had confirmed COVID-19. After multivariable adjustment, modifiable risk factors were higher body mass index and higher glycated haemoglobin (HbA1C) (RR 1.28 and RR 1.14 per SD increase, respectively), smoking (RR 1.39), slow walking pace as a proxy for physical fitness (RR 1.53), and use of blood pressure medications as a proxy for hypertension (RR 1.33). Higher forced expiratory volume in 1 s (FEV1) and high-density lipoprotein (HDL) cholesterol were both associated with lower risk (RR 0.84 and RR 0.83 per SD increase, respectively). Non-modifiable risk factors included male sex (RR 1.72), black ethnicity (RR 2.00), socioeconomic deprivation (RR 1.17 per SD increase in Townsend Index), and high cystatin C (RR 1.13 per SD increase). The risk factors overlapped with pneumonia somewhat, less so for influenza. The associations with modifiable risk factors were generally stronger for COVID-19, than pneumonia or influenza. Conclusion These findings suggest that modification of lifestyle may help to reduce the risk of COVID-19 and could be a useful adjunct to other interventions, such as social distancing and shielding of high risk.
Ethics approval UK Biobank received ethical approval from the North West Multicentre Research Ethics Committee (REC reference: 11/NW/03820). All participants gave written informed consent before enrolment in the study, which was conducted in accordance with the principles of the Declaration of Helsinki. Direct dissemination of the results to participants is not possible/applicable. This study was performed under UK Biobank application number 7155. Provenance and peer review Not commissioned; externally peer reviewed. Data availability statement Data may be obtained from a third party and are not publicly available. UK Biobank data can be requested by bona fide researchers for approved projects, including replication, through https://www. ukbiobank. ac. uk/ Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Open access This..
References
Almirall, Serra-Prat, Bolíbar, Risk factors for communityacquired pneumonia in adults: a systematic review of observational studies, Respiration, doi:10.1159/000479089
Armstrong, Rudkin, Allen, Dynamic linkage of covid-19 test results between public health england's second generation surveillance system and uk biobank, Microb Genomics, doi:10.1099/mgen.0.000397
Banerjee, Pasea, Harris, Estimating excess 1-year mortality from COVID-19 according to underlying conditions and age in England: a rapid analysis using NHS health records in 3.8 million adults, doi:10.1101/2020.03.22.20040287
Batty, Deary, Luciano, Psychosocial factors and hospitalisations for COVID-19: prospective cohort study based on a community sample, Brain Behav Immun, doi:10.1016/j.bbi.2020.06.021
Beun, Kusadasi, Sikma, Thromboembolic events and apparent heparin resistance in patients infected with SARS-CoV-2
Bradbury, Guo, Cairns, Association between physical activity and body fat percentage, with adjustment for BMI: a large cross-sectional analysis of UK Biobank, BMJ Open, doi:10.1136/bmjopen-2016-011843
Celis-Morales, Gray, Petermann, Walking PACE is associated with lower risk of all-cause and cause-specific mortality, Med Sci Sports Exerc, doi:10.1249/MSS.0000000000001795
Celis-Morales, Welsh, Lyall, Associations of grip strength with cardiovascular, respiratory, and cancer outcomes and all cause mortality: prospective cohort study of half a million UK Biobank participants, BMJ, doi:10.1136/bmj.k1651
Collins, What makes UK Biobank special?, Lancet, doi:10.1016/S0140-6736(12)60404-8
Drummond, Dickinson, Fry, Bed rest impairs skeletal muscle amino acid transporter expression, mTORC1 signaling, and protein synthesis in response to essential amino acids in older adults, Am J Physiol Endocrinol Metab, doi:10.1152/ajpendo.00603.2011
Elliott, Peakman, Biobank, The UK Biobank sample handling and storage protocol for the collection, processing and archiving of human blood and urine, Int J Epidemiol, doi:10.1093/ije/dym276
Fk, Celis-Morales, Gray, Modifiable and nonmodifiable risk factors for COVID-19: results from UK Biobank, MedRxiv
Fry, Littlejohns, Sudlow, Comparison of sociodemographic and health-related characteristics of UK Biobank participants with those of the general population, Am J Epidemiol, doi:10.1093/aje/kwx246
Green, Popham, Interpreting mutual adjustment for multiple indicators of socioeconomic position without committing mutual adjustment fallacies, BMC Public Health, doi:10.1186/s12889-018-6364-y
Hamer, Gale, Kivimäki, Overweight, obesity, and risk of hospitalization for COVID-19: a community-based cohort study of adults in the United Kingdom, Proc Natl Acad Sci, doi:10.1073/pnas.2011086117
Keyes, Westreich, UK Biobank, big data, and the consequences of non-representativeness, Lancet, doi:10.1016/S0140-6736(18)33067-8
Klovaite, Benn, Nordestgaard, Obesity as a causal risk factor for deep venous thrombosis: a Mendelian randomization study, J Intern Med, doi:10.1111/joim.12299
Lighter, Phillips, Hochman, Obesity in patients younger than 60 years is a risk factor for Covid-19 hospital admission, Clin Infect Dis, doi:10.1093/cid/ciaa415
Mcqueenie, Foster, Jani, Multimorbidity, polypharmacy, and COVID-19 infection within the UK Biobank cohort, PLoS One, doi:10.1371/journal.pone.0238091
Mizumoto, Kagaya, Zarebski, Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the diamond Princess cruise SHIP, Euro Surveill, doi:10.2807/1560-7917.ES.2020.25.10.2000180
Olsen, Krogh-Madsen, Thomsen, Metabolic responses to reduced daily steps in healthy nonexercising men, JAMA, doi:10.1001/jama.299.11.1259
Packard, Bezlyak, Mclean, Early life socioeconomic adversity is associated in adult life with chronic inflammation, carotid atherosclerosis, poorer lung function and decreased cognitive performance: a cross-sectional, population-based study, BMC Public Health, doi:10.1186/1471-2458-11-42
Panigada, Bottino, Tagliabue, Hypercoagulability of COVID-19 patients in intensive care unit. A report of thromboelastography findings and other parameters of hemostasis, J Thromb Haemost, doi:10.1111/jth.14850
Parsons, Manor, Power, Physical activity and change in body mass index from adolescence to mid-adulthood in the 1958 British cohort, Int J Epidemiol, doi:10.1093/ije/dyi291
Petrilli, Cm, Jones, Yang, Factors associated with hospitalization and critical illness among 4,103 patients with COVID-19 disease
Razieh, Zaccardi, Davies, Body mass index and the risk of COVID-19 across ethnic groups: analysis of UK Biobank, Diabetes, Obes. Metab, doi:10.1111/dom.14125
Razzoli, Pearson, Crow, Stress, overeating, and obesity: insights from human studies and preclinical models, Neurosci Biobehav Rev, doi:10.1016/j.neubiorev.2017.01.026
Richardson, Hirsch, Narasimhan, Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area, JAMA, doi:10.1001/jama.2020.6775
Sattar, Ho, Gill, BMI and future risk for COVID-19 infection and death across sex, age and ethnicity: preliminary findings from UK Biobank, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.06.060
Simonnet, Chetboun, Poissy, High prevalence of obesity in severe acute respiratory syndrome Coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation, Obesity, doi:10.1002/oby.22831
Sudlow, Gallacher, Allen, UK Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age, PLoS Med, doi:10.1371/journal.pmed.1001779
Timpson, Nordestgaard, Harbord, C-Reactive protein levels and body mass index: elucidating direction of causation through reciprocal Mendelian randomization, Int J Obes, doi:10.1038/ijo.2010.137
Tu, Tu, Gao, The epidemiological and clinical features of COVID-19 and lessons from this global infectious public health event, J
Welsh, Polisecki, Robertson, Unraveling the directional link between adiposity and inflammation: a bidirectional Mendelian randomization approach, J Clin Endocrinol Metab, doi:10.1210/jc.2009-1064
Williamson, Walker, Bhaskaran, Factors associated with COVID-19-related death using OpenSAFELY, Nature, doi:10.1038/s41586-020-2521-4
Wood, Pya, Säfken, Smoothing parameter and model selection for general smooth models, J Am Stat Assoc, doi:10.1080/01621459.2016.1180986
Wood, Stable and efficient multiple smoothing parameter estimation for generalized additive models, J Am Stat Assoc, doi:10.1198/016214504000000980
Woolford, Angelo, Curtis, COVID-19 and associations with frailty and multimorbidity: a prospective analysis of UK Biobank participants, Aging Clin Exp Res, doi:10.1007/s40520-020-01653-6
Wu, Mcgoogan, Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases from the Chinese Center for Disease Control and Prevention, JAMA, doi:10.1001/jama.2020.2648
Zhao, Zhang, Li, Incidence, clinical characteristics and prognostic factor of patients with COVID-19: a systematic review and meta-analysis
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet, doi:10.1016/S0140-6736(20)30566-3
Zhu, Hasegawa, Ma, Obesity & genetic predisposition with COVID-19, Metabolism
Zou, A modified poisson regression approach to prospective studies with binary data, Am J Epidemiol, doi:10.1093/aje/kwh090
DOI record:
{
"DOI": "10.1136/bmjopen-2020-040402",
"ISSN": [
"2044-6055",
"2044-6055"
],
"URL": "http://dx.doi.org/10.1136/bmjopen-2020-040402",
"abstract": "<jats:sec><jats:title>Objectives</jats:title><jats:p>We aimed to investigate demographic, lifestyle, socioeconomic and clinical risk factors for COVID-19, and compared them to risk factors for pneumonia and influenza in UK Biobank.</jats:p></jats:sec><jats:sec><jats:title>Design</jats:title><jats:p>Cohort study.</jats:p></jats:sec><jats:sec><jats:title>Setting</jats:title><jats:p>UK Biobank.</jats:p></jats:sec><jats:sec><jats:title>Participants</jats:title><jats:p>49–83 year olds (in 2020) from a general population study.</jats:p></jats:sec><jats:sec><jats:title>Main outcome measures</jats:title><jats:p>Confirmed COVID-19 infection (positive SARS-CoV-2 test). Incident influenza and pneumonia were obtained from primary care data. Poisson regression was used to study the association of exposure variables with outcomes.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>Among 235 928 participants, 397 had confirmed COVID-19. After multivariable adjustment, modifiable risk factors were higher body mass index and higher glycated haemoglobin (HbA1C) (RR 1.28 and RR 1.14 per SD increase, respectively), smoking (RR 1.39), slow walking pace as a proxy for physical fitness (RR 1.53), and use of blood pressure medications as a proxy for hypertension (RR 1.33). Higher forced expiratory volume in 1 s (FEV1) and high-density lipoprotein (HDL) cholesterol were both associated with lower risk (RR 0.84 and RR 0.83 per SD increase, respectively). Non-modifiable risk factors included male sex (RR 1.72), black ethnicity (RR 2.00), socioeconomic deprivation (RR 1.17 per SD increase in Townsend Index), and high cystatin C (RR 1.13 per SD increase). The risk factors overlapped with pneumonia somewhat, less so for influenza. The associations with modifiable risk factors were generally stronger for COVID-19, than pneumonia or influenza.</jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p>These findings suggest that modification of lifestyle may help to reduce the risk of COVID-19 and could be a useful adjunct to other interventions, such as social distancing and shielding of high risk.</jats:p></jats:sec>",
"alternative-id": [
"10.1136/bmjopen-2020-040402"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-7190-9025",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ho",
"given": "Frederick K",
"sequence": "first"
},
{
"affiliation": [],
"family": "Celis-Morales",
"given": "Carlos A",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8969-9636",
"affiliation": [],
"authenticated-orcid": false,
"family": "Gray",
"given": "Stuart R",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6593-9092",
"affiliation": [],
"authenticated-orcid": false,
"family": "Katikireddi",
"given": "S Vittal",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6133-4168",
"affiliation": [],
"authenticated-orcid": false,
"family": "Niedzwiedz",
"given": "Claire L",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hastie",
"given": "Claire",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ferguson",
"given": "Lyn D",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Berry",
"given": "Colin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mackay",
"given": "Daniel F",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gill",
"given": "Jason MR",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pell",
"given": "Jill P",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1604-2593",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sattar",
"given": "Naveed",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Welsh",
"given": "Paul",
"sequence": "additional"
}
],
"container-title": "BMJ Open",
"container-title-short": "BMJ Open",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2020,
11,
20
]
],
"date-time": "2020-11-20T08:27:50Z",
"timestamp": 1605860870000
},
"deposited": {
"date-parts": [
[
2021,
4,
14
]
],
"date-time": "2021-04-14T22:30:24Z",
"timestamp": 1618439424000
},
"funder": [
{
"DOI": "10.13039/501100000274",
"award": [
"RE/18/6/34217"
],
"doi-asserted-by": "publisher",
"name": "British Heart Foundation"
},
{
"award": [
"SPHSU13"
],
"name": "Scottish Government Chief Scientist Office"
},
{
"DOI": "10.13039/501100000265",
"award": [
"MC_UU_12017/13",
"MR/R024774/1"
],
"doi-asserted-by": "publisher",
"name": "Medical Research Council"
},
{
"award": [
"SCAF/15/02"
],
"name": "NRS Senior Clinical Fellowship"
}
],
"indexed": {
"date-parts": [
[
2022,
8,
24
]
],
"date-time": "2022-08-24T23:05:53Z",
"timestamp": 1661382353772
},
"is-referenced-by-count": 57,
"issue": "11",
"issued": {
"date-parts": [
[
2020,
11
]
]
},
"journal-issue": {
"issue": "11",
"published-online": {
"date-parts": [
[
2020,
11,
19
]
]
},
"published-print": {
"date-parts": [
[
2020,
11
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "unspecified",
"delay-in-days": 18,
"start": {
"date-parts": [
[
2020,
11,
19
]
],
"date-time": "2020-11-19T00:00:00Z",
"timestamp": 1605744000000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/bmjopen-2020-040402",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "e040402",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2020,
11
]
]
},
"published-online": {
"date-parts": [
[
2020,
11,
19
]
]
},
"published-print": {
"date-parts": [
[
2020,
11
]
]
},
"publisher": "BMJ",
"reference": [
{
"DOI": "10.2807/1560-7917.ES.2020.25.10.2000180",
"article-title": "Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the diamond Princess cruise SHIP, Yokohama, Japan, 2020",
"author": "Mizumoto",
"doi-asserted-by": "crossref",
"journal-title": "Euro Surveill",
"key": "2020112000102007000_10.11.e040402.1",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.2648",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.2"
},
{
"key": "2020112000102007000_10.11.e040402.3",
"unstructured": "Coronavirus disease 2019 (COVID-19) situation Report-76 highlights"
},
{
"DOI": "10.1101/2020.04.08.20057794",
"doi-asserted-by": "crossref",
"key": "2020112000102007000_10.11.e040402.4",
"unstructured": "Petrilli CM , Jones SA , Yang J , et al . Factors associated with hospitalization and critical illness among 4,103 patients with COVID-19 disease in New York City. MedRxiv 2020;20057794."
},
{
"DOI": "10.1016/j.jinf.2020.04.011",
"doi-asserted-by": "crossref",
"key": "2020112000102007000_10.11.e040402.5",
"unstructured": "Tu H , Tu S , Gao S , et al . The epidemiological and clinical features of COVID-19 and lessons from this global infectious public health event. J Infect 2020;0."
},
{
"DOI": "10.1101/2020.03.22.20040287",
"doi-asserted-by": "crossref",
"key": "2020112000102007000_10.11.e040402.6",
"unstructured": "Banerjee A , Pasea L , Harris S , et al . Estimating excess 1- year mortality from COVID-19 according to underlying conditions and age in England: a rapid analysis using NHS health records in 3.8 million adults. MedRxiv 2020:20040287. doi:10.1101/2020.03.22.20040287"
},
{
"DOI": "10.1001/jama.2020.6775",
"doi-asserted-by": "crossref",
"key": "2020112000102007000_10.11.e040402.7",
"unstructured": "Richardson S , Hirsch JS , Narasimhan M , et al . Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. [Epub ahead of print: April 2020].doi:10.1001/jama.2020.6775"
},
{
"DOI": "10.1002/oby.22831",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.8"
},
{
"key": "2020112000102007000_10.11.e040402.9",
"unstructured": "Clinical Infectious Diseases . Obesity in patients younger than 60 years is a risk factor for Covid-19 hospital admission. Oxford Academic"
},
{
"key": "2020112000102007000_10.11.e040402.10",
"unstructured": "2 Treatment and care planning . COVID-19 rapid guideline: managing suspected or confirmed pneumonia in adults in the community. Guidance. NICE"
},
{
"DOI": "10.1159/000479089",
"article-title": "Risk factors for community-acquired pneumonia in adults: a systematic review of observational studies",
"author": "Almirall",
"doi-asserted-by": "crossref",
"first-page": "299",
"journal-title": "Respiration",
"key": "2020112000102007000_10.11.e040402.11",
"volume": "94",
"year": "2017"
},
{
"DOI": "10.1016/S0140-6736(12)60404-8",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.12"
},
{
"DOI": "10.1371/journal.pmed.1001779",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.13"
},
{
"DOI": "10.1099/mgen.0.000397",
"article-title": "Dynamic linkage of covid-19 test results between public health england’s second generation surveillance system and uk biobank",
"author": "Armstrong",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Microb Genomics",
"key": "2020112000102007000_10.11.e040402.14",
"volume": "6",
"year": "2020"
},
{
"key": "2020112000102007000_10.11.e040402.15",
"unstructured": "FK H , Celis-Morales CA , Gray SR , et al . Modifiable and non-modifiable risk factors for COVID-19: results from UK Biobank. MedRxiv 2020:20083295."
},
{
"DOI": "10.1249/MSS.0000000000001795",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.16"
},
{
"DOI": "10.1136/bmj.k1651",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.17"
},
{
"DOI": "10.1093/ije/dym276",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.18"
},
{
"DOI": "10.1093/aje/kwh090",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.19"
},
{
"DOI": "10.1198/016214504000000980",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.20"
},
{
"DOI": "10.1080/01621459.2016.1180986",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.21"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.22"
},
{
"DOI": "10.1016/j.metabol.2020.154345",
"doi-asserted-by": "crossref",
"key": "2020112000102007000_10.11.e040402.23",
"unstructured": "Zhu Z , Hasegawa K , Ma B , et al . Obesity & genetic predisposition with COVID-19. Metabolism 2020:154345."
},
{
"DOI": "10.1371/journal.pone.0238091",
"article-title": "Multimorbidity, polypharmacy, and COVID-19 infection within the UK Biobank cohort",
"author": "McQueenie",
"doi-asserted-by": "crossref",
"journal-title": "PLoS One",
"key": "2020112000102007000_10.11.e040402.24",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1007/s40520-020-01653-6",
"article-title": "COVID-19 and associations with frailty and multimorbidity: a prospective analysis of UK Biobank participants",
"author": "Woolford",
"doi-asserted-by": "crossref",
"journal-title": "Aging Clin Exp Res",
"key": "2020112000102007000_10.11.e040402.25",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.06.060",
"article-title": "BMI and future risk for COVID-19 infection and death across sex, age and ethnicity: preliminary findings from UK Biobank",
"author": "Sattar",
"doi-asserted-by": "crossref",
"first-page": "1149",
"journal-title": "Diabetes Metab Syndr",
"key": "2020112000102007000_10.11.e040402.26",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1111/dom.14125",
"doi-asserted-by": "crossref",
"key": "2020112000102007000_10.11.e040402.27",
"unstructured": "Razieh C , Zaccardi F , Davies MJ , et al . Body mass index and the risk of COVID-19 across ethnic groups: analysis of UK Biobank. Diabetes, Obes. Metab 2020.doi:10.1111/dom.14125"
},
{
"DOI": "10.1016/j.bbi.2020.06.021",
"article-title": "Psychosocial factors and hospitalisations for COVID-19: prospective cohort study based on a community sample",
"author": "Batty",
"doi-asserted-by": "crossref",
"journal-title": "Brain Behav Immun",
"key": "2020112000102007000_10.11.e040402.28",
"volume": "89",
"year": "2020"
},
{
"DOI": "10.1073/pnas.2011086117",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.29"
},
{
"DOI": "10.1001/jama.299.11.1261-a",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.30"
},
{
"DOI": "10.1152/ajpendo.00603.2011",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.31"
},
{
"DOI": "10.1136/bmjopen-2016-011843",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.32"
},
{
"DOI": "10.1093/ije/dyi291",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.33"
},
{
"DOI": "10.1016/j.neubiorev.2017.01.026",
"article-title": "Stress, overeating, and obesity: insights from human studies and preclinical models",
"author": "Razzoli",
"doi-asserted-by": "crossref",
"first-page": "154",
"journal-title": "Neurosci Biobehav Rev",
"key": "2020112000102007000_10.11.e040402.34",
"volume": "76",
"year": "2017"
},
{
"DOI": "10.1186/1471-2458-11-42",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.35"
},
{
"key": "2020112000102007000_10.11.e040402.36",
"unstructured": "Zhao X , Zhang B , Li P , et al . Incidence, clinical characteristics and prognostic factor of patients with COVID-19: a systematic review and meta-analysis. Cold Spring Harbor Laboratory Press, 2020."
},
{
"DOI": "10.1093/cid/ciaa415",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.37"
},
{
"DOI": "10.1038/ijo.2010.137",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.38"
},
{
"DOI": "10.1210/jc.2009-1064",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.39"
},
{
"DOI": "10.1111/joim.12299",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.40"
},
{
"DOI": "10.1111/ijlh.13230",
"doi-asserted-by": "crossref",
"key": "2020112000102007000_10.11.e040402.41",
"unstructured": "Beun R , Kusadasi N , Sikma M , et al . Thromboembolic events and apparent heparin resistance in patients infected with SARS-CoV-2. Int J Lab Hematol. [Epub ahead of print: April 2020].doi:10.1111/ijlh.13230"
},
{
"DOI": "10.1111/jth.14850",
"doi-asserted-by": "crossref",
"key": "2020112000102007000_10.11.e040402.42",
"unstructured": "Panigada M , Bottino N , Tagliabue P , et al . Hypercoagulability of COVID‐19 patients in intensive care unit. A report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost 2020:14850. doi:10.1111/jth.14850"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.43"
},
{
"DOI": "10.1093/aje/kwx246",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.44"
},
{
"DOI": "10.1016/s0140-6736(18)33067-8",
"doi-asserted-by": "publisher",
"key": "2020112000102007000_10.11.e040402.45"
},
{
"DOI": "10.1186/s12889-018-6364-y",
"article-title": "Interpreting mutual adjustment for multiple indicators of socioeconomic position without committing mutual adjustment fallacies",
"author": "Green",
"doi-asserted-by": "crossref",
"journal-title": "BMC Public Health",
"key": "2020112000102007000_10.11.e040402.46",
"volume": "19",
"year": "2019"
}
],
"reference-count": 46,
"references-count": 46,
"relation": {},
"resource": {
"primary": {
"URL": "https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2020-040402"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Modifiable and non-modifiable risk factors for COVID-19, and comparison to risk factors for influenza and pneumonia: results from a UK Biobank prospective cohort study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy",
"volume": "10"
}
