Vitamin D Deficiency and Comorbidities as Risk Factors of COVID-19 Infection: A Systematic Review and Meta-analysis
et al., Journal of Preventive Medicine and Public Health, doi:10.3961/jpmph.21.640, Jul 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Systematic review and meta analysis showing low vitamin D levels associated with COVID-19 cases.
20 meta-analyses show significant improvements with vitamin D treatment for mortality1-14,
mechanical ventilation1,5,6,11,15-17 ,
ICU admission1,3,5,6,9,11,13,15-19 ,
hospitalization11,
severity2,4,5,10,20 , and
cases7,19,20 .
Currently there are 136 vitamin D treatment for COVID-19 studies, showing 39% lower mortality [31‑45%], 17% lower ventilation [-5‑35%], 45% lower ICU admission [28‑57%], 22% lower hospitalization [13‑30%], and 17% fewer cases [9‑25%].
1.
Shah et al., Does vitamin D supplementation reduce COVID-19 severity? - a systematic review, QJM: An International Journal of Medicine, doi:10.1093/qjmed/hcac040.
2.
Nikniaz et al., The impact of vitamin D supplementation on mortality rate and clinical outcomes of COVID-19 patients: A systematic review and meta-analysis, Pharmaceutical Sciences, doi:10.34172/PS.2021.13.
3.
Hosseini et al., Effects of Vitamin D Supplementation on COVID-19 Related Outcomes: A Systematic Review and Meta-Analysis, Nutrients, doi:10.3390/nu14102134.
4.
D’Ecclesiis et al., Vitamin D and SARS-CoV2 infection, severity and mortality: A systematic review and meta-analysis, PLOS ONE, doi:10.1371/journal.pone.0268396.
5.
Xie et al., Micronutrient perspective on COVID-19: Umbrella review and reanalysis of meta-analyses, Critical Reviews in Food Science and Nutrition, doi:10.1080/10408398.2023.2174948.
6.
Hariyanto et al., Vitamin D supplementation and Covid‐19 outcomes: A systematic review, meta‐analysis and meta‐regression, Reviews in Medical Virology, doi:10.1002/rmv.2269.
7.
Begum et al., The Role of Vitamin D in COVID-19 Survival and Prevention: A Meta-analysis, Sudan Journal of Medical Sciences, doi:10.18502/sjms.v19i1.15776.
8.
Jamilian et al., The role of vitamin D in outcomes of critical care in COVID-19 patients: Evidence from an umbrella meta-analysis of interventional and observational studies, Public Health Nutrition, doi:10.1017/S1368980024000934.
9.
Sobczak et al., Effect of Vitamin D3 Supplementation on Severe COVID-19: A Meta-Analysis of Randomized Clinical Trials, Nutrients, doi:10.3390/nu16101402.
10.
Petrelli et al., Therapeutic and prognostic role of vitamin D for COVID-19 infection: A systematic review and meta-analysis of 43 observational studies, The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2021.105883.
11.
Asla et al., Vitamin D on COVID-19 Patients During the Pandemic, 2022. A Systematic Review and Meta-Analysis, Current Research in Nutrition and Food Science Journal, doi:10.12944/CRNFSJ.11.1.3.
12.
Kow et al., The impact of vitamin D administration on mortality in COVID-19 patients: a systematic review and meta-analysis of randomized controlled trials, Inflammopharmacology, doi:10.1007/s10787-024-01564-2.
13.
Zhang et al., The impact of supplementing vitamin D through different methods on the prognosis of COVID-19 patients: a systematic review and meta-analysis, Frontiers in Nutrition, doi:10.3389/fnut.2024.1441847.
14.
Doustmohammadian et al., Impact of vitamin D supplementation on COVID-19 mortality: A systematic review and meta-analysis, Nutrition Clinique et Métabolisme, doi:10.1016/j.nupar.2025.12.001.
15.
Meng et al., The role of vitamin D in the prevention and treatment of SARS-CoV-2 infection: A meta-analysis of randomized controlled trials, Clinical Nutrition, doi:10.1016/j.clnu.2023.09.008.
16.
Yang et al., Therapeutic effects of vitamin D supplementation on COVID-19 aggravation: a systematic review and meta-analysis of randomized controlled trials, Frontiers in Pharmacology, doi:10.3389/fphar.2024.1367686.
17.
Szarpak et al., Vitamin D supplementation to treat SARS-CoV-2 positive patients. Evidence from meta-analysis, Cardiology Journal, doi:10.5603/CJ.a2021.0122.
18.
Tentolouris et al., The effect of vitamin D supplementation on mortality and intensive care unit admission of COVID-19 patients. A systematic review, meta-analysis and meta-regression, Diabetes/Metabolism Research and Reviews, doi:10.1002/dmrr.3517.
Mishra et al., 31 Jul 2022, peer-reviewed, 4 authors.
Contact: nidhi.bharal@gmail.com.
Vitamin D Deficiency and Comorbidities as Risk Factors of COVID-19 Infection: A Systematic Review and Meta-analysis
Journal of Preventive Medicine and Public Health, doi:10.3961/jpmph.21.640
Objectives: Extensive evidence links low vitamin D status and comorbidities with coronavirus disease 2019 outcomes, but the results of published studies are contradictory. Therefore, we investigated the association of lower levels of vitamin D and comorbidities with the risk of COVID-19 infection.
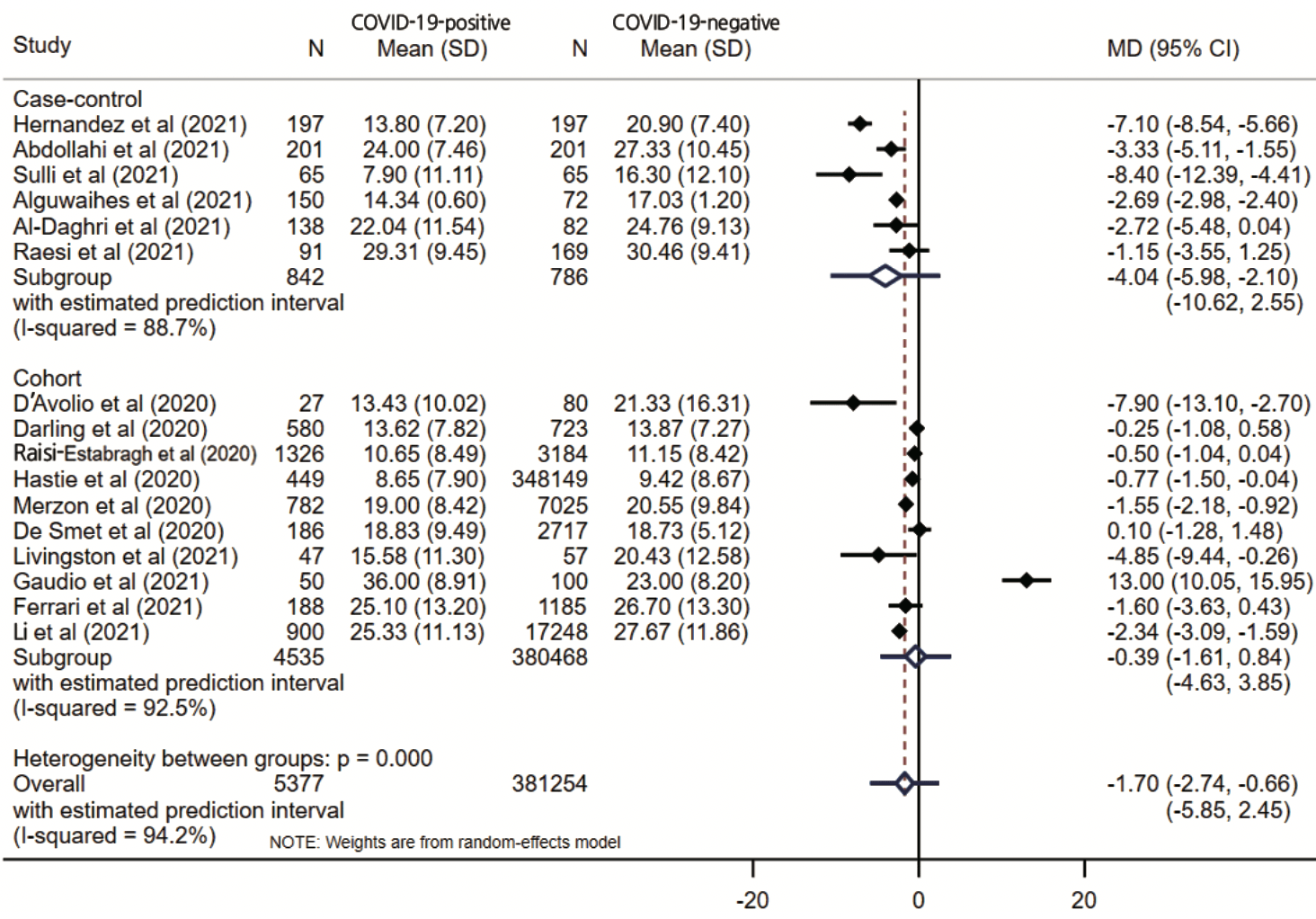
Methods: We searched MEDLINE (via PubMed), Cochrane Central Register of Controlled Trials, and ClinicalTrials.gov for articles published until August 20, 2021. Sixteen eligible studies were identified (386 631 patients, of whom 181 114 were male). We included observational cohort and case-control studies that evaluated serum levels of vitamin D in COVID-19-positive and COVID-19-negative patients. Mean differences (MDs) with 95% confidence intervals (CIs) were calculated. Results: Significantly lower vitamin D levels were found in COVID-19-positive patients (MD, -1.70; 95% CI, -2.74 to -0.66; p=0.001), but with variation by study design (case-control: -4.04; 95% CI, -5.98 to -2.10; p<0.001; cohort: -0.39; 95% CI, -1.62 to 0.84; p=0.538). This relationship was more prominent in female patients (MD, -2.18; 95% CI, -4.08 to -0.28; p=0.024) than in male patients (MD, -1.74; 95% CI, -3.79 to 0.31; p=0.096). Male patients showed higher odds of having low vitamin D levels (odds ratio [OR], 2.09; 95% CI, 1.38 to 3.17; p<0.001) than female patients (OR, 1.17; 95% CI, 0.74 to 1.86; p=0.477). Comorbidities showed inconsistent, but generally nonsignificant, associations with COVID-19 infection. Conclusions: Low serum vitamin-D levels were significantly associated with the risk of COVID-19 infection. This relationship was stronger in female than in male COVID-19 patients. Limited evidence was found for the relationships between comorbidities and COVID-19 infection, warranting large population-based studies to clarify these associations.
CONFLICT OF INTEREST The authors have no conflicts of interest associated with the material presented in this paper.
FUNDING None.
AUTHOR CONTRIBUTIONS Conceptualization: Mishra P, Parveen R. Data curation: Mishra P, Parveen R. Formal analysis: Mishra P, Bajpai R. Funding acquisition: None. Methodology: Mishra P, Bajpai R. Project administration: Agarwal N, Mishra P. Visualization: Mishra P, Parveen R. Writing -original draft: Mishra P, Parveen R, Agarwal N, Bajpai R. Writing -review & editing: Bajpai R, Agarwal N.
References
Abdollahi, Sarvestani, Rafat, Ghaderkhani, Mahmoudi-Aliabadi et al., The association between the level of serum 25(OH) vitamin D, obesity, and underlying diseases with the risk of developing COVID-19 infection: a case-control study of hospitalized patients in Tehran, Iran, J Med Virol
Al-Daghri, Saleh, Aljohani, Sulimani, Al-Othman et al., Vitamin D status correction in Saudi Arabia: an experts' consensus under the auspices of the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis, and Musculoskeletal Diseases (ESCEO), Arch Osteoporos
Alguwaihes, Sabico, Hasanato, Megdad, Albader, Severe vitamin D deficiency is not related to SARS-CoV-2 infection but may increase mortality risk in hospitalized adults: a retrospective case-control study in an Arab Gulf country, Aging Clin Exp Res
Amer, Alotaibi, Aldisi, Enani, Sheshah, Vitamin D status of Arab Gulf residents screened for SARS-CoV-2 and its association with COVID-19 infection: a multi-centre case-control study, J Transl Med
Baktash, Hosack, Patel, Shah, Kandiah et al., Vitamin D status and outcomes for hospitalised older patients with COVID-19, Postgrad Med J
Bassatne, Basbous, Chakhtoura, El Zein, Rahme et al., The link between COVID-19 and vItamin D (VIVID): a systematic review and meta-analysis, Metabolism
Berry, Hesketh, Power, Hyppönen, Vitamin D status has a linear association with seasonal infections and lung function in British adults, Br J Nutr
Bouillon, Marcocci, Carmeliet, Bikle, White et al., Skeletal and extraskeletal actions of vitamin D: current evidence and outstanding questions, Endocr Rev
Cai, Sex difference and smoking predisposition in patients with COVID-19, Lancet Respir Med
Campi, Gennari, Merlotti, Mingiano, Frosali et al., Vitamin D and COVID-19 severity and related mortality: a prospective study in Italy, BMC Infect Dis
Cannell, Vieth, Umhau, Holick, Grant et al., Epidemic influenza and vitamin D, Epidemiol Infect
Cannell, Zasloff, Garland, Scragg, Giovannucci, On the epidemiology of influenza, Virol J
Clinical, Group, Treatment of vitamin D deficiency in adults
Crafa, Cannarella, Condorelli, Mongioì, Barbagallo et al., Influence of 25-hydroxy-cholecalciferol levels on SARS-CoV-2 infection and COVID-19 severity: a systematic review and meta-analysis, EClinicalMedicine
Cutolo, Paolino, Smith, Evidences for a protective role of vitamin D in COVID-19, RMD Open
D'avolio, Avataneo, Manca, Cusato, Nicolò et al., 25-Hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2, Nutrients
Daneshkhah, Agrawal, Eshein, Subramanian, Roy et al., The possible role of vitamin D in suppressing cytokine storm and associated mortality in COVID-19 patients, doi:10.1101/2020.04.08.20058578
Dankers, Colin, Van Hamburg, Lubberts, Vitamin D in autoimmunity: molecular mechanisms and therapeutic potential, Front Immunol
Darling, Ahmadi, Ward, Harvey, Alves et al., Vitamin D status, body, doi:10.1101/2020.04.29.20084277
Duval, Tweedie, Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in metaanalysis, Biometrics
Ebadi, Montano-Loza, Perspective: improving vitamin D status in the management of COVID-19, Eur J Clin Nutr
Ferrari, Locatelli, Faraldi, Lombardi, Changes in 25-(OH) vitamin D levels during the SARS-CoV-2 outbreak: lockdown-related effects and first-to-second wave difference-an observational study from northern Italy, Biology
Gaudio, Murabito, Agodi, Montineri, Castellino et al., Vitamin D levels are reduced at the time of hospital admission in Sicilian SARS-CoV-2-positive patients, Int J Environ Res Public Health
Ghasemian, Shamshirian, Heydari, Malekan, Alizadeh-Navaei et al., The role of vitamin D in the age of COVID-19: a systematic review and meta-analysis, Int J Clin Pract
Ginde, Liu, Camargo, Demographic differences and trends of vitamin D insufficiency in the US population, 1988-2004, Arch Intern Med
Gombart, Pierre, Maggini, A review of micronutrients and the immune system-working in harmony to reduce the risk of infection, Nutrients
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths, Nutrients
Guan, Liang, Zhao, Liang, Chen et al., Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis, Eur Respir J
Hastie, Mackay, Ho, Celis-Morales, Katikireddi et al., Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metab Syndr
Hernández, Nan, Fernandez-Ayala, García-Unzueta, Hernández-Hernández et al., Vitamin D status in hospitalized patients with SARS-CoV-2 infection, J Clin Endocrinol Metab
Higgins, Green, Cochrane handbook for systematic reviews of interventions
Ho, Fernando, Chan, Sia, Obesity in COVID-19: a systematic review and meta-analysis, Ann Acad Med Singap
Holick, The vitamin D deficiency pandemic: approaches for diagnosis, treatment and prevention, Rev Endocr Metab Disord
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin Exp Res
Infante, Ricordi, Sanchez, Salzler, Padilla et al., Influence of vitamin D on islet autoimmunity and beta-cell function in type 1 diabetes, Nutrients
Inthout, Ioannidis, Rovers, Goeman, Plea for routinely presenting prediction intervals in meta-analysis, BMJ Open
Kralj, Jakovac, Vitamin D and COVID-19 in an immunocompromised patient with multiple comorbidities-a case report, Clin Case Rep
Kweder, Eidi, Vitamin D deficiency in elderly: risk factors and drugs impact on vitamin D status, Avicenna J Med
Lau, Majumder, Torabi, Saeg, Hoffman et al., Vitamin D insufficiency is prevalent in severe COVID-19, doi:10.1101/2020.04.24.20075838
Li, Li, Zhang, Liu, Sunlight and vitamin D in the prevention of coronavirus disease (COVID-19) infection and mortality in the United States, Res Sq, doi:10.21203/rs.3.rs-32499/v1
Li, Tong, Bare, Devlin, Assessment of the association of vitamin D level with SARS-CoV-2 seropositivity among working-age adults, JAMA Netw Open
Lips, Cashman, Lamberg-Allardt, Bischoff-Ferrari, Obermayer-Pietsch et al., Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency: a position statement of the European Calcified Tissue Society, Eur J Endocrinol
Liu, Sun, Wang, Zhang, Zhao et al., Low vitamin D status is associated with coronavirus disease 2019 outcomes: a systematic review and meta-analysis, Int J Infect Dis
Livingston, Plant, Dunmore, Hartland, Jones et al., Detectable respiratory SARS-CoV-2 RNA is associated with low vitamin D levels and high social deprivation, Int J Clin Pract
Mamelund, Shelley-Egan, Rogeberg, The association between socioeconomic status and pandemic influenza: systematic review and meta-analysis, PLoS One
Meltzer, Best, Zhang, Vokes, Arora et al., Association of vitamin D deficiency and treatment with COVID-19 incidence, doi:10.1101/2020.05.08.20095893
Merzon, Tworowski, Gorohovski, Vinker, Cohen et al., Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli populationbased study, FEBS J
Mishra, Parveen, Agarwal, Role of vitamin D in risk reduction of COVID-19: a narrative review, Ann Natl Acad Med Sci
Munshi, Hussein, Toraih, Elshazli, Jardak et al., Vitamin D insufficiency as a potential culprit in critical COVID-19 patients, J Med Virol
Murdaca, Pioggia, Negrini, Vitamin D and Covid-19: an update on evidence and potential therapeutic implications, Clin Mol Allergy
Muscogiuri, Barrea, Somma, Laudisio, Salzano et al., Sex differences of vitamin D status across BMI classes: an observational prospective cohort study, Nutrients
Pagano, Peruzzu, Ruggieri, Ortona, Gagliardi, Vitamin D and sex differences in COVID-19, Front Endocrinol
Page, Mckenzie, Bossuyt, Boutron, Hoffmann et al., The PRISMA 2020 statement: an updated guideline for reporting systematic reviews, BMJ
Panagiotou, Tee, Ihsan, Athar, Marchitelli et al., Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalized with COVID-19 are associated with greater disease severity, Clin Endocrinol (Oxf)
Parveen, Sehar, Bajpai, Agarwal, Association of diabetes and hypertension with disease severity in covid-19 patients: a systematic literature review and exploratory metaanalysis, Diabetes Res Clin Pract
Pereira, Damascena, Azevedo, De Almeida Oliveira, Da et al., Vitamin D deficiency aggravates COVID-19: systematic review and meta-analysis, Crit Rev Food Sci Nutr
Raesi, Dezaki, Moosapour, Saeidifard, Habibi et al., Hypocalcemia in Covid-19: a prognostic marker for severe disease, Iran J Pathol
Raisi-Estabragh, Mccracken, Bethell, Cooper, Cooper et al., Greater risk of severe COVID-19 in Black, Asian and Minority Ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25(OH)-vitamin D status: study of 1326 cases from the UK Biobank, J Public Health (Oxf)
Sanghera, Sapkota, Aston, Blackett, Vitamin D status, gender differences, and cardiometabolic health disparities, Ann Nutr Metab
Shah, Saxena, Mavalankar, Vitamin D supplementation, COVID-19 and disease severity: a meta-analysis, QJM
Smet, Smet, Herroelen, Gryspeerdt, Martens, Vitamin D deficiency as risk factor for severe COVID-19: a convergence of two pandemics, doi:10.1101/2020.05.01.20079376
Stroup, Berlin, Morton, Olkin, Williamson et al., Meta-analysis of observational studies in epidemi-Pinki Mishra, JAMA
Sulli, Gotelli, Casabella, Paolino, Pizzorni et al., Vitamin D and lung outcomes in elderly COVID-19 patients, Nutrients
Szarpak, Rafique, Gasecka, Chirico, Gawel et al., A systematic review and meta-analysis of effect of vitamin D levels on the incidence of COVID-19, Cardiol J
Teshome, Adane, Girma, Mekonnen, The impact of vitamin D level on COVID-19 infection: systematic review and meta-analysis, Front Public Health
Wang, Dabbas, Laperriere, Bitton, Soualhine et al., Direct and indirect induction by 1,25-dihydroxyvitamin D3 of the NOD2/CARD15-defensin beta2 innate immune pathway defective in Crohn disease, J Biol Chem
Wang, Hu, Hu, Zhu, Liu et al., Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China, JAMA
Wei, Christakos, Mechanisms underlying the regulation of innate and adaptive immunity by vitamin D, Nutrients
Wenham, Smith, Morgan, Gender and COVID-19 Working Group. COVID-19: the gendered impacts of the outbreak, Lancet
Yang, Zheng, Gou, Pu, Chen et al., Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis, Int J Infect Dis
Ye, Tang, Liao, Shaw, Deng et al., Does serum vitamin D level affect COVID-19 infection and its severity?-A case-control study, J Am Coll Nutr
Zhou, Luo, Qin, The association between vitamin D deficiency and community-acquired pneumonia: a meta-analysis of observational studies, Medicine
DOI record:
{
"DOI": "10.3961/jpmph.21.640",
"ISSN": [
"1975-8375",
"2233-4521"
],
"URL": "http://dx.doi.org/10.3961/jpmph.21.640",
"abstract": "<jats:p>Objectives: Extensive evidence links low vitamin D status and comorbidities with coronavirus disease 2019 (COVID-19) outcomes, but the results of published studies are contradictory. Therefore, we investigated the association of lower levels of vitamin D and comorbidities with the risk of COVID-19 infection.Methods: We searched MEDLINE (via PubMed), Cochrane Central Register of Controlled Trials, and ClinicalTrials.gov for articles published until August 20, 2021. Sixteen eligible studies were identified (386 631 patients, of whom 181 114 were male). We included observational cohort and case-control studies that evaluated serum levels of vitamin D in COVID-19-positive and COVID-19-negative patients. Mean differences (MDs) with 95% confidence intervals (CIs) were calculated.Results: Significantly lower vitamin D levels were found in COVID-19-positive patients (MD, -1.70; 95% CI, -2.74 to -0.66; p=0.001), but with variation by study design (case-control: -4.04; 95% CI, -5.98 to -2.10; p<0.001; cohort: -0.39; 95% CI, -1.62 to 0.84; p=0.538). This relationship was more prominent in female patients (MD, -2.18; 95% CI, -4.08 to -0.28; p=0.024) than in male patients (MD, -1.74; 95% CI, -3.79 to 0.31; p=0.096). Male patients showed higher odds of having low vitamin D levels (odds ratio [OR], 2.09; 95% CI, 1.38 to 3.17; p<0.001) than female patients (OR, 1.17; 95% CI, 0.74 to 1.86; p=0.477). Comorbidities showed inconsistent, but generally non-significant, associations with COVID-19 infection.Conclusions: Low serum vitamin-D levels were significantly associated with the risk of COVID-19 infection. This relationship was stronger in female than in male COVID-19 patients. Limited evidence was found for the relationships between comorbidities and COVID-19 infection, warranting large population-based studies to clarify these associations.</jats:p>",
"assertion": [
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2021-12-18"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 1,
"value": "2022-05-09"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published online",
"name": "published",
"order": 2,
"value": "2022-06-13"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Print publication",
"name": "published",
"order": 3,
"value": "2022-07-31"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-5326-0522",
"affiliation": [],
"authenticated-orcid": true,
"family": "Mishra",
"given": "Pinki",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-3506-7497",
"affiliation": [],
"authenticated-orcid": true,
"family": "Parveen",
"given": "Rizwana",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1227-2703",
"affiliation": [],
"authenticated-orcid": true,
"family": "Bajpai",
"given": "Ram",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2509-3026",
"affiliation": [],
"authenticated-orcid": true,
"family": "Agarwal",
"given": "Nidhi",
"sequence": "additional"
}
],
"container-title": "Journal of Preventive Medicine and Public Health",
"container-title-short": "J Prev Med Public Health",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"jpmph.org"
]
},
"created": {
"date-parts": [
[
2022,
6,
13
]
],
"date-time": "2022-06-13T04:29:05Z",
"timestamp": 1655094545000
},
"deposited": {
"date-parts": [
[
2022,
8,
7
]
],
"date-time": "2022-08-07T23:59:30Z",
"timestamp": 1659916770000
},
"indexed": {
"date-parts": [
[
2022,
8,
8
]
],
"date-time": "2022-08-08T00:40:44Z",
"timestamp": 1659919244521
},
"is-referenced-by-count": 0,
"issue": "4",
"issued": {
"date-parts": [
[
2022,
7,
31
]
]
},
"journal-issue": {
"issue": "4",
"published-print": {
"date-parts": [
[
2022,
7
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
6,
13
]
],
"date-time": "2022-06-13T00:00:00Z",
"timestamp": 1655078400000
}
}
],
"link": [
{
"URL": "http://jpmph.org/upload/pdf/jpmph-21-640.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://jpmph.org/journal/view.php?doi=10.3961/jpmph.21.640",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://jpmph.org/upload/pdf/jpmph-21-640.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "2350",
"original-title": [],
"page": "321-333",
"prefix": "10.3961",
"published": {
"date-parts": [
[
2022,
7,
31
]
]
},
"published-print": {
"date-parts": [
[
2022,
7,
31
]
]
},
"publisher": "Korean Society for Preventive Medicine",
"reference": [
{
"DOI": "10.3390/nu12040988",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.1093/qjmed/hcab009",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1038/s41430-020-0661-0",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.3390/nu7105392",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1007/s11154-017-9424-1",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.3389/fimmu.2016.00697",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.3390/nu11092185",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1210/er.2018-00126",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.1017/s0950268806007175",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1186/1743-422x-5-29",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1001/archinternmed.2008.604",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.3390/nu12010236",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"author": "Wang",
"first-page": "2227",
"key": "ref13",
"volume-title": "Direct and indirect induction by 1,25-dihydroxyvitamin D3 of the NOD2/CARD15-defensin beta2 innate immune pathway defective in Crohn disease",
"year": "2010"
},
{
"DOI": "10.1111/cen.14276",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1017/s0007114511001991",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1002/ccr3.4010",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.1016/j.diabres.2020.108295",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1055/s-0041-1724460",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1101/2020.05.08.20095893",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.3390/nu12051359",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1016/j.dsx.2020.04.050",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"author": "Zhou",
"first-page": "e17252",
"key": "ref22",
"volume-title": "The association between vitamin D deficiency and community-acquired pneumonia: a meta-analysis of observational studies",
"year": "2019"
},
{
"DOI": "10.1136/rmdopen-2020-001454",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1101/2020.04.08.20058578",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1101/2020.04.29.20084277",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1101/2020.05.01.20079376",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1007/s40520-020-01570-8",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1101/2020.04.24.20075838",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.21203/rs.3.rs-32499/v1",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.3389/fpubh.2021.624559",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1016/j.eclinm.2021.100967",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.1136/bmj.n71",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1001/jama.283.15.2008",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"key": "ref34",
"volume-title": ""
},
{
"DOI": "10.1002/jmv.26726",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1007/s40520-021-01831-0",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.1186/s12967-021-02838-x",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.1210/clinem/dgaa733",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.3390/biology10030237",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.1001/jamanetworkopen.2021.11634",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.3390/nu13030717",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.1007/s11657-016-0295-y",
"doi-asserted-by": "publisher",
"key": "ref42"
},
{
"DOI": "10.1530/eje-18-0736",
"doi-asserted-by": "publisher",
"key": "ref43"
},
{
"author": "Gaudio",
"first-page": "3491",
"key": "ref44",
"volume-title": "D O CoV Research, Vitamin D levels are reduced at the time of hospital admission in Sicilian SARS-CoV-2-positive patients",
"year": "2021"
},
{
"DOI": "10.1111/ijcp.14166",
"doi-asserted-by": "publisher",
"key": "ref45"
},
{
"DOI": "10.1111/febs.15495",
"doi-asserted-by": "publisher",
"key": "ref46"
},
{
"key": "ref47",
"volume-title": "",
"year": "2020"
},
{
"author": "Higgins",
"key": "ref48",
"volume-title": "",
"year": "2011"
},
{
"DOI": "10.1111/j.0006-341x.2000.00455.x",
"doi-asserted-by": "publisher",
"key": "ref49"
},
{
"DOI": "10.1136/bmjopen-2015-010247",
"doi-asserted-by": "publisher",
"key": "ref50"
},
{
"DOI": "10.1093/pubmed/fdaa095",
"doi-asserted-by": "publisher",
"key": "ref51"
},
{
"DOI": "10.30699/ijp.2020.130491.2442",
"doi-asserted-by": "publisher",
"key": "ref52"
},
{
"DOI": "10.5603/cj.a2021.0072",
"doi-asserted-by": "publisher",
"key": "ref53"
},
{
"DOI": "10.1016/j.metabol.2021.154753",
"doi-asserted-by": "publisher",
"key": "ref54"
},
{
"DOI": "10.1016/j.ijid.2020.12.077",
"doi-asserted-by": "publisher",
"key": "ref55"
},
{
"DOI": "10.1080/10408398.2020.1841090",
"doi-asserted-by": "publisher",
"key": "ref56"
},
{
"DOI": "10.1111/ijcp.14675",
"doi-asserted-by": "publisher",
"key": "ref57"
},
{
"DOI": "10.1002/jmv.26360",
"doi-asserted-by": "publisher",
"key": "ref58"
},
{
"DOI": "10.1016/s2213-2600(20)30117-x",
"doi-asserted-by": "publisher",
"key": "ref59"
},
{
"DOI": "10.1016/s0140-6736(20)30526-2",
"doi-asserted-by": "publisher",
"key": "ref60"
},
{
"DOI": "10.3390/nu11123034",
"doi-asserted-by": "publisher",
"key": "ref61"
},
{
"DOI": "10.1159/000458765",
"doi-asserted-by": "publisher",
"key": "ref62"
},
{
"DOI": "10.3389/fendo.2020.567824",
"doi-asserted-by": "publisher",
"key": "ref63"
},
{
"DOI": "10.1080/07315724.2020.1826005",
"doi-asserted-by": "publisher",
"key": "ref64"
},
{
"DOI": "10.1186/s12948-020-00139-0",
"doi-asserted-by": "publisher",
"key": "ref65"
},
{
"DOI": "10.1136/postgradmedj-2020-138712",
"doi-asserted-by": "publisher",
"key": "ref66"
},
{
"DOI": "10.1186/s12879-021-06281-7",
"doi-asserted-by": "publisher",
"key": "ref67"
},
{
"DOI": "10.4103/ajm.ajm_20_18",
"doi-asserted-by": "publisher",
"key": "ref68"
},
{
"DOI": "10.1183/13993003.00547-2020",
"doi-asserted-by": "publisher",
"key": "ref69"
},
{
"DOI": "10.1001/jama.2020.1585",
"doi-asserted-by": "publisher",
"key": "ref70"
},
{
"DOI": "10.47102/annals-acadmedsg.2020299",
"doi-asserted-by": "publisher",
"key": "ref71"
},
{
"DOI": "10.1371/journal.pone.0244346",
"doi-asserted-by": "publisher",
"key": "ref72"
},
{
"DOI": "10.1016/j.ijid.2020.03.017",
"doi-asserted-by": "publisher",
"key": "ref73"
}
],
"reference-count": 73,
"references-count": 73,
"relation": {},
"resource": {
"primary": {
"URL": "http://jpmph.org/journal/view.php?doi=10.3961/jpmph.21.640"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Public Health, Environmental and Occupational Health"
],
"subtitle": [],
"title": "Vitamin D Deficiency and Comorbidities as Risk Factors of COVID-19 Infection: A Systematic Review and Meta-analysis",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3961/crossmark_policy",
"volume": "55"
}
