Prevalence and Risk Factors of Headache Associated with COVID-19
et al., Journal of Clinical Medicine, doi:10.3390/jcm13175013, Aug 2024
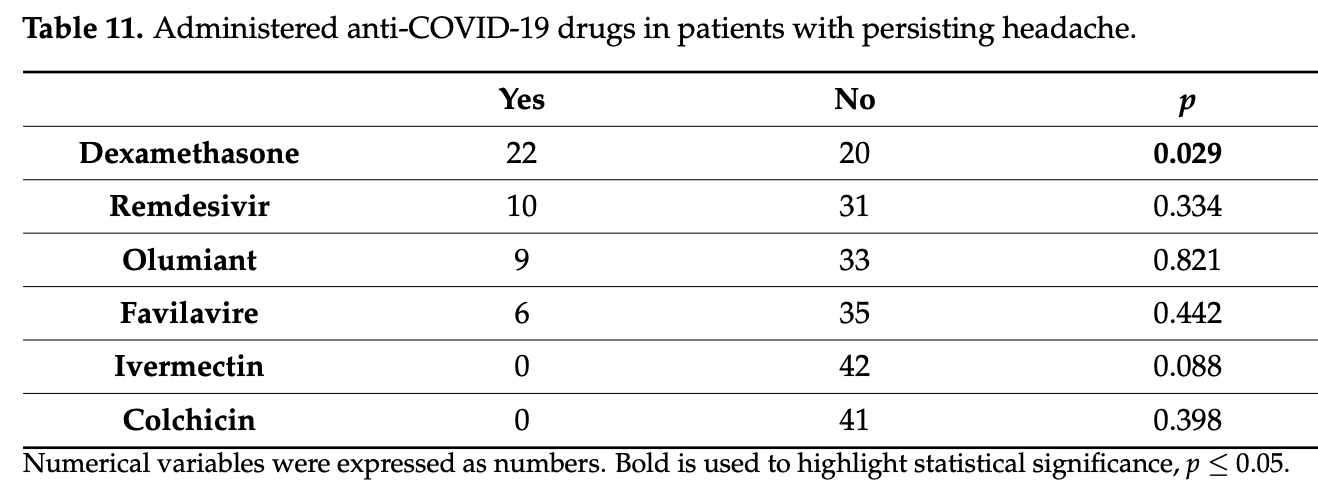
Retrospective 295 hospitalized COVID-19 patients in Slovakia showing 35% prevalence of headache, of which 41% of patients had persistent headache 12-15 months after infection. Authors' analysis of long COVID headache is only for the subgroup of 102 patients. For evaluating treatments, the risk of long COVID headache among all patients may be more relevant. Authors hypothesize that headache may be related to persistent immune system activation with biohumoral response, trigeminal system activation in genetically predisposed individuals, or structural and functional brain changes.
Potential risks of favipiravir include kidney injury1-3, liver injury2-5, cardiovascular events5,6, pulmonary toxicity6,7, and mutagenicity, carcinogenicity, teratogenicity, embryotoxicity, and the creation of dangerous variants8-14.
|
headache, 70.2% higher, RR 1.70, p = 0.24, treatment 6 of 27 (22.2%), control 35 of 268 (13.1%), persisting headache.
|
|
headache, 45.0% higher, RR 1.45, p = 0.14, treatment 13 of 27 (48.1%), control 89 of 268 (33.2%), headache during infection.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Abdulaziz et al., Clinical Features and Prognosis of Acute Kidney Injury in Hospital-Admitted Patients with COVID-19 in Egypt: A Single-Center Experience, Mansoura Medical Journal, doi:10.58775/2735-3990.1433.
2.
Ülger et al., Experimental evaluation of favipiravir (T-705)-induced liver and kidney toxicity in rats, Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115472.
3.
El-Fetouh et al., Experimental Studies on Some Drugs Used in Covid-19 Treatment (Favipiravir and Dexamethasone) in Albino Rats, Journal of Advanced Veterinary Research, 13:10, www.advetresearch.com/index.php/AVR/article/view/1635.
4.
Almutairi et al., Liver Injury in Favipiravir-Treated COVID-19 Patients: Retrospective Single-Center Cohort Study, Tropical Medicine and Infectious Disease, doi:10.3390/tropicalmed8020129.
5.
Siby et al., Temporal Trends in Serious Adverse Events Associated with Oral Antivirals During the COVID-19 Pandemic: Insights from the FAERS Database (2020–2023), Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1825.
6.
Ozhan et al., Evaluation of the cardiopulmonary effects of repurposed COVID-19 therapeutics in healthy rats, Scientific Reports, doi:10.1038/s41598-025-31048-4.
7.
Ülger (B) et al., Evaluation of the effects of favipiravir (T-705) on the lung tissue of healty rats: An experimental study, Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115235.
8.
Zhirnov et al., Favipiravir: the hidden threat of mutagenic action, Journal of microbiology, epidemiology and immunobiology, doi:10.36233/0372-9311-114.
9.
Waters et al., Human genetic risk of treatment with antiviral nucleoside analog drugs that induce lethal mutagenesis: the special case of molnupiravir, Environmental and Molecular Mutagenesis, doi:10.1002/em.22471.
10.
Hadj Hassine et al., Lethal Mutagenesis of RNA Viruses and Approved Drugs with Antiviral Mutagenic Activity, Viruses, doi:10.3390/v14040841.
11.
Shum, C., An investigational study into the drug-associated mutational signature in SARS-CoV-2 viruses, The University of Hong Kong, PhD Thesis, hub.hku.hk/handle/10722/344396.
12.
Shiraki et al., Convenient screening of the reproductive toxicity of favipiravir and antiviral drugs in Caenorhabditis elegans, Heliyon, doi:10.1016/j.heliyon.2024.e35331.
Duraníková et al., 24 Aug 2024, retrospective, Slovakia, peer-reviewed, median age 58.0, 7 authors, study period March 2020 - April 2021.
Contact: straka0105@gmail.com (corresponding author), olga.duranikova@gmail.com, simonah09@gmail.com, mmminar@gmail.com, veronika.bolekova@gmail.com, petersabaka@gmail.com, peter.valkovic@gmail.com.
Prevalence and Risk Factors of Headache Associated with COVID-19
Journal of Clinical Medicine, doi:10.3390/jcm13175013
Background: Headache is a prevalent and disabling non-respiratory symptom of COVID-19, posing a persistent challenge in post-COVID syndrome. This study aimed to determine the prevalence, phenotypes, risk factors and biomarkers associated with COVID-related headaches. Methods: A retrospective analysis of 634 hospitalized COVID-19 patients was conducted, with 295 participants being followed up 12-15 months post-discharge via telephone call. Initial laboratory workups, including complete blood count and various biochemical parameters, were compared between headache and non-headache groups. Results: One-third of hospitalized patients experienced headaches, predominantly younger individuals (p < 0.001) and women (p = 0.002). Non-dominant headaches were characterized as dull (56.9%) and holocranial (26.5%), while dominant headaches were unilateral (31.3%) with photophobia (34.3%) and nausea (56.3%). Persistent headaches were unilateral (40%) and pulsating (38%) with phonophobia (74%). Decreased CD4 T cells independently predicted COVID-associated headaches, with elevated IL-6 levels noted in the dominant-headache group (p = 0.040). Remarkably, 50% of patients reported persistent headaches 12-15 months post-infection. Dexamethasone administration significantly reduced the likelihood of long-COVID headaches (52% vs. 73%, p = 0.029). Conclusions: Headache was present in one-third of patients with heterogenous phenotypes: tension headache in the non-dominant group, and migraine in the dominant and persistent headache groups. Persistent headache remains a challenge, with dexamethasone showing potential in reducing its incidence, emphasizing the need for tailored approaches in managing long-COVID headaches.
Author Contributions: O.D.: conceptualization, data curation, investigation, project administration, formal analysis, writing-original draft; S.H.: conceptualization, data curation, investigation, formal analysis, writing-review and editing, P.S.: conceptualization, methodology, writing-review and editing, M.M.: conceptualization, methodology, writing-review and editing, supervision, V.B.: methodology, writing-review and editing, I.S.: conceptualization, methodology, writing-review and editing, supervision, P.V.: writing-review and editing, supervision. All authors have read and agreed to the published version of the manuscript. Informed Consent Statement: Participants were fully informed about the purpose of the study and potential risks of participation. Written informed consent was obtained from all participants before the enrolment and verbal informed consent during telephone survey.
Conflicts of Interest: The authors declare no conflicts of interest.
References
Al-Hashel, Ismail, Impact of Coronavirus Disease 2019 (COVID-19) Pandemic on Patients with Migraine: A Web-Based Survey Study, J. Headache Pain, doi:10.1186/s10194-020-01183-6
Aparisi, Ybarra-Falcón, Iglesias-Echeverría, García-Gómez, Marcos-Mangas et al., Cardio-Pulmonary Dysfunction Evaluation in Patients with Persistent Post-COVID-19 Headache, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph19073961
Bauer, Laksono, De Vrij, Kushner, Harschnitz et al., The Neuroinvasiveness, Neurotropism, and Neurovirulence of SARS-CoV-2, Trends Neurosci, doi:10.1016/j.tins.2022.02.006
Caronna, Pozo-Rosich, Headache as a Symptom of COVID-19: Narrative Review of 1-Year Research, Curr. Pain. Headache Rep, doi:10.1007/s11916-021-00987-8
Caronna, Van Den, Hoek, Bolay, Garcia-Azorin et al., Headache Attributed to SARS-CoV-2 Infection, Vaccination and the Impact on Primary Headache Disorders of the COVID-19 Pandemic: A Comprehensive Review, Cephalalgia, doi:10.1177/03331024221131337
Fujita, Otsuka, Sunada, Honda, Tokumasu et al., Manifestation of Headache Affecting Quality of Life in Long COVID Patients, JCM, doi:10.3390/jcm12103533
Gallardo, Shapiro, Caronna, Pozo-Rosich, The Relationship of Headache as a Symptom to COVID-19 Survival: A Systematic Review and Meta-analysis of Survival of 43,169 Inpatients with COVID-19, Headache, doi:10.1111/head.14376
Garcell, Gutiérrez, García, Ramirez Nodal, Ruiz Lozano et al., Clinical Relevance of Zika Symptoms in the Context of a Zika Dengue Epidemic, J. Infect. Public Health, doi:10.1016/j.jiph.2019.07.006
García-Azorín, Sierra, Trigo, Alberdi, Blanco et al., Frequency and Phenotype of Headache in COVID-19: A Study of 2194, Patients. Sci. Rep, doi:10.1038/s41598-021-94220-6
Gonzalez-Martinez, Fanjul, Ramos, Serrano Ballesteros, Bustamante et al., Headache during SARS-CoV-2 Infection as an Early Symptom Associated with a More Benign Course of Disease: A Case-Control Study, Eur. J. Neurol, doi:10.1111/ene.14718
Grundmann, Wu, Hardwick, Baillie, Openshaw et al., Fewer COVID-19 Neurological Complications with Dexamethasone and Remdesivir, Ann. Neurol, doi:10.1002/ana.26536
Leng, Shah, Ahmad, Premraj, Wildi et al., Pathogenesis Underlying Neurological Manifestations of Long COVID Syndrome and Potential Therapeutics, Cells, doi:10.3390/cells12050816
Mutiawati, Kusuma, Fahriani, Harapan, Syahrul et al., Headache in Post-COVID-19 Patients: Its Characteristics and Relationship with the Quality of Life, Medicina, doi:10.3390/medicina58101500
Nakano, Otsuka, Honda, Sunada, Tokumasu et al., Transitional Changes in Fatigue-Related Symptoms Due to Long COVID: A Single-Center Retrospective Observational Study in Japan, Medicina, doi:10.3390/medicina58101393
Pelayo-González, Reyes-Meza, Méndez-Balbuena, Méndez-Díaz, Trenado et al., Quantitative Electroencephalographic Analysis in Women with Migraine during the Luteal Phase, Appl. Sci, doi:10.3390/app13137443
Peng, Ouyang, Isnard, Lin, Fombuena et al., Sharing CD4+ T Cell Loss: When COVID-19 and HIV Collide on Immune System, Front. Immunol, doi:10.3389/fimmu.2020.596631
Planchuelo-Gómez, Garcia-Azorín, Aja-Fernándes, Rodríguez, Guerrero et al., White Matter Microstructural Alterations in Patients with Persistent Headache after COVID-19 Infection: An Exploratory Study. International Headache Society & European Headache Federation, doi:10.1177/03331024211034005
Planchuelo-Gómez, Trigo, De Luis-García, Guerrero, Porta-Etessam et al., Deep Phenotyping of Headache in Hospitalized COVID-19 Patients via Principal Component Analysis, Front. Neurol, doi:10.3389/fneur.2020.583870
Rakshit, Parthiban Ch Mudhavan, Adiga, Eveline, Kumar et al., Polyfunctional CD4 T-cells correlating with neutralising antibody is a hallmark of COVISHIELDTM and COVAXIN ® induced immunity in COVID-19 exposed Indians, Npj Vaccines, doi:10.1038/s41541-023-00731-w
Rocha-Filho, Torres, Ramos Montarroyos, HIV and Headache: A Cross-Sectional Study, Headache, doi:10.1111/head.13183
Rodrigues, Dias, Paranhos, Silva, Bastos et al., Headache in Long COVID as Disabling Condition: A Clinical Approach, Front. Neurol, doi:10.3389/fneur.2023.1149294
Stein, Ramelli, Grazioli, Chung, Singh et al., SARS-CoV-2 Infection and Persistence in the Human Body and Brain at Autopsy, Nature, doi:10.1038/s41586-022-05542-y
Sunada, Nakano, Otsuka, Tokumasu, Honda et al., Characteristics of Sleep Disturbance in Patients with Long COVID: A Retrospective Observational Study in Japan, JCM, doi:10.3390/jcm11247332
Swank, Senussi, Manickas-Hill, Yu, Li et al., Persistent Circulating Severe Acute Respiratory Syndrome Coronavirus 2 Spike Is Associated With Post-Acute Coronavirus Disease 2019 Sequelae, Clin. Infect. Dis, doi:10.1093/cid/ciac722
Trigo López, García-Azorín, Planchuelo-Gómez, García-Iglesias, Dueñas-Gutiérrez et al., Phenotypic Characterization of Acute Headache Attributed to SARS-CoV-2: An ICHD-3 Validation Study on 106 Hospitalized Patients, Cephalalgia, doi:10.1177/0333102420965146
Trigo, García-Azorín, Planchuelo-Gómez, Martínez-Pías, Talavera et al., Factors Associated with the Presence of Headache in Hospitalized COVID-19 Patients and Impact on Prognosis: A Retrospective Cohort Study, J. Headache Pain, doi:10.1186/s10194-020-01165-8
Trigo, García-Azorín, Sierra-Mencía, Tamayo-Velasco, Martínez-Paz et al., Cytokine and Interleukin Profile in Patients with Headache and COVID-19: A Pilot, CASE-Control, Study on 104 Patients, J. Headache Pain, doi:10.1186/s10194-021-01268-w
Wang, Yang, Mei, Zhou, Tang et al., SARS-CoV-2-Specific CD4+ T Cells Are Associated with Long-Term Persistence of Neutralizing Antibodies, Sig Transduct. Target. Ther, doi:10.1038/s41392-022-00978-0
DOI record:
{
"DOI": "10.3390/jcm13175013",
"ISSN": [
"2077-0383"
],
"URL": "http://dx.doi.org/10.3390/jcm13175013",
"abstract": "<jats:p>Background: Headache is a prevalent and disabling non-respiratory symptom of COVID-19, posing a persistent challenge in post-COVID syndrome. This study aimed to determine the prevalence, phenotypes, risk factors and biomarkers associated with COVID-related headaches. Methods: A retrospective analysis of 634 hospitalized COVID-19 patients was conducted, with 295 participants being followed up 12–15 months post-discharge via telephone call. Initial laboratory workups, including complete blood count and various biochemical parameters, were compared between headache and non-headache groups. Results: One-third of hospitalized patients experienced headaches, predominantly younger individuals (p < 0.001) and women (p = 0.002). Non-dominant headaches were characterized as dull (56.9%) and holocranial (26.5%), while dominant headaches were unilateral (31.3%) with photophobia (34.3%) and nausea (56.3%). Persistent headaches were unilateral (40%) and pulsating (38%) with phonophobia (74%). Decreased CD4 T cells independently predicted COVID-associated headaches, with elevated IL-6 levels noted in the dominant-headache group (p = 0.040). Remarkably, 50% of patients reported persistent headaches 12–15 months post-infection. Dexamethasone administration significantly reduced the likelihood of long-COVID headaches (52% vs. 73%, p = 0.029). Conclusions: Headache was present in one-third of patients with heterogenous phenotypes: tension headache in the non-dominant group, and migraine in the dominant and persistent headache groups. Persistent headache remains a challenge, with dexamethasone showing potential in reducing its incidence, emphasizing the need for tailored approaches in managing long-COVID headaches.</jats:p>",
"alternative-id": [
"jcm13175013"
],
"author": [
{
"affiliation": [
{
"name": "2nd Department of Neurology, Faculty of Medicine, Comenius University Bratislava, 813 72 Bratislava, Slovakia"
}
],
"family": "Duraníková",
"given": "Oľga",
"sequence": "first"
},
{
"affiliation": [
{
"name": "2nd Department of Neurology, Faculty of Medicine, Comenius University Bratislava, 813 72 Bratislava, Slovakia"
}
],
"family": "Horváthová",
"given": "Simona",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9337-8843",
"affiliation": [
{
"name": "Department of Infectology and Geographical Medicine, Faculty of Medicine, Comenius University Bratislava, 813 72 Bratislava, Slovakia"
}
],
"authenticated-orcid": false,
"family": "Sabaka",
"given": "Peter",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0812-2366",
"affiliation": [
{
"name": "2nd Department of Neurology, Faculty of Medicine, Comenius University Bratislava, 813 72 Bratislava, Slovakia"
}
],
"authenticated-orcid": false,
"family": "Minár",
"given": "Michal",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2076-1096",
"affiliation": [
{
"name": "2nd Department of Neurology, Faculty of Medicine, Comenius University Bratislava, 813 72 Bratislava, Slovakia"
},
{
"name": "Faculty of Psychology, Institute of Clinical Psychology, Pan-European University, 821 02 Bratislava, Slovakia"
}
],
"authenticated-orcid": false,
"family": "Boleková",
"given": "Veronika",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1134-7029",
"affiliation": [
{
"name": "2nd Department of Neurology, Faculty of Medicine, Comenius University Bratislava, 813 72 Bratislava, Slovakia"
}
],
"authenticated-orcid": false,
"family": "Straka",
"given": "Igor",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7837-8781",
"affiliation": [
{
"name": "2nd Department of Neurology, Faculty of Medicine, Comenius University Bratislava, 813 72 Bratislava, Slovakia"
},
{
"name": "Institute of Normal and Pathological Physiology, Centre of Experimental Medicine, Slovak Academy of Sciences, 813 71 Bratislava, Slovakia"
}
],
"authenticated-orcid": false,
"family": "Valkovič",
"given": "Peter",
"sequence": "additional"
}
],
"container-title": "Journal of Clinical Medicine",
"container-title-short": "JCM",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
8,
26
]
],
"date-time": "2024-08-26T07:32:01Z",
"timestamp": 1724657521000
},
"deposited": {
"date-parts": [
[
2024,
8,
26
]
],
"date-time": "2024-08-26T08:43:42Z",
"timestamp": 1724661822000
},
"funder": [
{
"award": [
"VEGA 2/0076/22"
],
"name": "Scientific Grant Agency of the Ministry of Education, Science, Research and Sport of the Slovak Republic"
}
],
"indexed": {
"date-parts": [
[
2024,
8,
27
]
],
"date-time": "2024-08-27T00:14:55Z",
"timestamp": 1724717695563
},
"is-referenced-by-count": 0,
"issue": "17",
"issued": {
"date-parts": [
[
2024,
8,
24
]
]
},
"journal-issue": {
"issue": "17",
"published-online": {
"date-parts": [
[
2024,
9
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
8,
24
]
],
"date-time": "2024-08-24T00:00:00Z",
"timestamp": 1724457600000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2077-0383/13/17/5013/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "5013",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2024,
8,
24
]
]
},
"published-online": {
"date-parts": [
[
2024,
8,
24
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1007/s11916-021-00987-8",
"article-title": "Headache as a Symptom of COVID-19: Narrative Review of 1-Year Research",
"author": "Caronna",
"doi-asserted-by": "crossref",
"first-page": "73",
"journal-title": "Curr. Pain. Headache Rep.",
"key": "ref_1",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.1016/j.tins.2022.02.006",
"article-title": "The Neuroinvasiveness, Neurotropism, and Neurovirulence of SARS-CoV-2",
"author": "Bauer",
"doi-asserted-by": "crossref",
"first-page": "358",
"journal-title": "Trends Neurosci.",
"key": "ref_2",
"volume": "45",
"year": "2022"
},
{
"DOI": "10.1186/s10194-021-01268-w",
"article-title": "Cytokine and Interleukin Profile in Patients with Headache and COVID-19: A Pilot, CASE-Control, Study on 104 Patients",
"author": "Trigo",
"doi-asserted-by": "crossref",
"first-page": "51",
"journal-title": "J. Headache Pain",
"key": "ref_3",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1111/ene.14718",
"article-title": "Headache during SARS-CoV-2 Infection as an Early Symptom Associated with a More Benign Course of Disease: A Case–Control Study",
"author": "Fanjul",
"doi-asserted-by": "crossref",
"first-page": "3426",
"journal-title": "Eur. J. Neurol.",
"key": "ref_4",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.1016/j.jiph.2019.07.006",
"article-title": "Clinical Relevance of Zika Symptoms in the Context of a Zika Dengue Epidemic",
"doi-asserted-by": "crossref",
"first-page": "173",
"journal-title": "J. Infect. Public Health",
"key": "ref_5",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1111/head.13183",
"article-title": "HIV and Headache: A Cross-Sectional Study",
"author": "Torres",
"doi-asserted-by": "crossref",
"first-page": "1545",
"journal-title": "Headache",
"key": "ref_6",
"volume": "57",
"year": "2017"
},
{
"DOI": "10.1038/s41392-022-00978-0",
"article-title": "SARS-CoV-2-Specific CD4+ T Cells Are Associated with Long-Term Persistence of Neutralizing Antibodies",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "132",
"journal-title": "Sig Transduct. Target. Ther.",
"key": "ref_7",
"volume": "7",
"year": "2022"
},
{
"DOI": "10.1186/s10194-020-01165-8",
"article-title": "Factors Associated with the Presence of Headache in Hospitalized COVID-19 Patients and Impact on Prognosis: A Retrospective Cohort Study",
"author": "Trigo",
"doi-asserted-by": "crossref",
"first-page": "94",
"journal-title": "J. Headache Pain",
"key": "ref_8",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1111/head.14376",
"article-title": "The Relationship of Headache as a Symptom to COVID-19 Survival: A Systematic Review and Meta-analysis of Survival of 43,169 Inpatients with COVID-19",
"author": "Gallardo",
"doi-asserted-by": "crossref",
"first-page": "1019",
"journal-title": "Headache",
"key": "ref_9",
"volume": "62",
"year": "2022"
},
{
"DOI": "10.3389/fimmu.2020.596631",
"doi-asserted-by": "crossref",
"key": "ref_10",
"unstructured": "Peng, X., Ouyang, J., Isnard, S., Lin, J., Fombuena, B., Zhu, B., and Routy, J.-P. (2020). Sharing CD4+ T Cell Loss: When COVID-19 and HIV Collide on Immune System. Front. Immunol., 11."
},
{
"DOI": "10.1038/s41541-023-00731-w",
"article-title": "Polyfunctional CD4 T-cells correlating with neutralising antibody is a hallmark of COVISHIELDTM and COVAXIN® induced immunity in COVID-19 exposed Indians",
"author": "Rakshit",
"doi-asserted-by": "crossref",
"first-page": "134",
"journal-title": "Npj Vaccines",
"key": "ref_11",
"volume": "8",
"year": "2023"
},
{
"DOI": "10.3390/cells12050816",
"doi-asserted-by": "crossref",
"key": "ref_12",
"unstructured": "Leng, A., Shah, M., Ahmad, S.A., Premraj, L., Wildi, K., Li Bassi, G., Pardo, C.A., Choi, A., and Cho, S.-M. (2023). Pathogenesis Underlying Neurological Manifestations of Long COVID Syndrome and Potential Therapeutics. Cells, 12."
},
{
"DOI": "10.3389/fneur.2020.583870",
"doi-asserted-by": "crossref",
"key": "ref_13",
"unstructured": "Planchuelo-Gómez, Á., Trigo, J., de Luis-García, R., Guerrero, Á.L., Porta-Etessam, J., and García-Azorín, D. (2020). Deep Phenotyping of Headache in Hospitalized COVID-19 Patients via Principal Component Analysis. Front. Neurol., 11."
},
{
"DOI": "10.1177/0333102420965146",
"article-title": "Phenotypic Characterization of Acute Headache Attributed to SARS-CoV-2: An ICHD-3 Validation Study on 106 Hospitalized Patients",
"author": "Guerrero",
"doi-asserted-by": "crossref",
"first-page": "1432",
"journal-title": "Cephalalgia",
"key": "ref_14",
"volume": "40",
"year": "2020"
},
{
"DOI": "10.3390/medicina58101500",
"doi-asserted-by": "crossref",
"key": "ref_15",
"unstructured": "Mutiawati, E., Kusuma, H.I., Fahriani, M., Harapan, H., Syahrul, S., and Musadir, N. (2022). Headache in Post-COVID-19 Patients: Its Characteristics and Relationship with the Quality of Life. Medicina, 58."
},
{
"DOI": "10.1177/03331024221131337",
"article-title": "Headache Attributed to SARS-CoV-2 Infection, Vaccination and the Impact on Primary Headache Disorders of the COVID-19 Pandemic: A Comprehensive Review",
"author": "Caronna",
"doi-asserted-by": "crossref",
"first-page": "033310242211313",
"journal-title": "Cephalalgia",
"key": "ref_16",
"volume": "43",
"year": "2023"
},
{
"DOI": "10.1038/s41598-021-94220-6",
"doi-asserted-by": "crossref",
"key": "ref_17",
"unstructured": "García-Azorín, D., Sierra, Á., Trigo, J., Alberdi, A., Blanco, M., Calcerrada, I., Cornejo, A., Cubero, M., Gil, A., and García-Iglesias, C. (2021). Frequency and Phenotype of Headache in COVID-19: A Study of 2194 Patients. Sci. Rep., 11."
},
{
"DOI": "10.3389/fneur.2023.1149294",
"doi-asserted-by": "crossref",
"key": "ref_18",
"unstructured": "Rodrigues, A.N., Dias, A.R.N., Paranhos, A.C.M., Silva, C.C., Bastos, T.D.R., Brito, B.B.D., Da Silva, N.M., De Sousa, E.D.J.S., Quaresma, J.A.S., and Falcão, L.F.M. (2023). Headache in Long COVID as Disabling Condition: A Clinical Approach. Front. Neurol., 14."
},
{
"DOI": "10.3390/jcm12103533",
"doi-asserted-by": "crossref",
"key": "ref_19",
"unstructured": "Fujita, K., Otsuka, Y., Sunada, N., Honda, H., Tokumasu, K., Nakano, Y., Sakurada, Y., Obika, M., Hagiya, H., and Otsuka, F. (2023). Manifestation of Headache Affecting Quality of Life in Long COVID Patients. JCM, 12."
},
{
"DOI": "10.3390/jcm11247332",
"doi-asserted-by": "crossref",
"key": "ref_20",
"unstructured": "Sunada, N., Nakano, Y., Otsuka, Y., Tokumasu, K., Honda, H., Sakurada, Y., Matsuda, Y., Hasegawa, T., Omura, D., and Ochi, K. (2022). Characteristics of Sleep Disturbance in Patients with Long COVID: A Retrospective Observational Study in Japan. JCM, 11."
},
{
"DOI": "10.3390/medicina58101393",
"doi-asserted-by": "crossref",
"key": "ref_21",
"unstructured": "Nakano, Y., Otsuka, Y., Honda, H., Sunada, N., Tokumasu, K., Sakurada, Y., Matsuda, Y., Hasegawa, T., Ochi, K., and Hagiya, H. (2022). Transitional Changes in Fatigue-Related Symptoms Due to Long COVID: A Single-Center Retrospective Observational Study in Japan. Medicina, 58."
},
{
"DOI": "10.3390/ijerph19073961",
"doi-asserted-by": "crossref",
"key": "ref_22",
"unstructured": "Aparisi, Á., Ybarra-Falcón, C., Iglesias-Echeverría, C., García-Gómez, M., Marcos-Mangas, M., Valle-Peñacoba, G., Carrasco-Moraleja, M., Fernández-de-las-Peñas, C., Guerrero, Á.L., and García-Azorín, D. (2022). Cardio-Pulmonary Dysfunction Evaluation in Patients with Persistent Post-COVID-19 Headache. Int. J. Environ. Res. Public Health, 19."
},
{
"DOI": "10.1093/cid/ciac722",
"article-title": "Persistent Circulating Severe Acute Respiratory Syndrome Coronavirus 2 Spike Is Associated With Post-Acute Coronavirus Disease 2019 Sequelae",
"author": "Swank",
"doi-asserted-by": "crossref",
"first-page": "e487",
"journal-title": "Clin. Infect. Dis.",
"key": "ref_23",
"volume": "76",
"year": "2023"
},
{
"DOI": "10.1038/s41586-022-05542-y",
"article-title": "SARS-CoV-2 Infection and Persistence in the Human Body and Brain at Autopsy",
"author": "Stein",
"doi-asserted-by": "crossref",
"first-page": "758",
"journal-title": "Nature",
"key": "ref_24",
"volume": "612",
"year": "2022"
},
{
"DOI": "10.1007/s00415-022-11398-z",
"doi-asserted-by": "crossref",
"key": "ref_25",
"unstructured": "Planchuelo-Gómez, Á., Garcia-Azorín, D., Aja-Fernándes, S., Rodríguez, M., Guerrero, A.L., Moro, R., and De Luis-Garcia, R. (2021, January 8–12). White Matter Microstructural Alterations in Patients with Persistent Headache after COVID-19 Infection: An Exploratory Study. International Headache Society & European Headache Federation. Proceedings of the International Headache Congress, Berlin, Germany. Available online: https://journals.sagepub.com/doi/pdf/10.1177/03331024211034005."
},
{
"DOI": "10.1002/ana.26536",
"article-title": "Fewer COVID-19 Neurological Complications with Dexamethasone and Remdesivir",
"author": "Grundmann",
"doi-asserted-by": "crossref",
"first-page": "88",
"journal-title": "Ann. Neurol.",
"key": "ref_26",
"volume": "93",
"year": "2023"
},
{
"DOI": "10.1186/s10194-020-01183-6",
"article-title": "Impact of Coronavirus Disease 2019 (COVID-19) Pandemic on Patients with Migraine: A Web-Based Survey Study",
"author": "Ismail",
"doi-asserted-by": "crossref",
"first-page": "115",
"journal-title": "J. Headache Pain",
"key": "ref_27",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.3390/app13137443",
"doi-asserted-by": "crossref",
"key": "ref_28",
"unstructured": "Pelayo-González, H.J., Reyes-Meza, V., Méndez-Balbuena, I., Méndez-Díaz, O., Trenado, C., Ruge, D., García-Aguilar, G., and López-Cortés, V.A. (2023). Quantitative Electroencephalographic Analysis in Women with Migraine during the Luteal Phase. Appl. Sci., 13."
}
],
"reference-count": 28,
"references-count": 28,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2077-0383/13/17/5013"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Prevalence and Risk Factors of Headache Associated with COVID-19",
"type": "journal-article",
"volume": "13"
}
duranikova