Risk of Underlying Diseases and Effectiveness of Drugs on COVID-19 Inpatients Assessed Using Medical Claims in Japan: Retrospective Observational Study
et al., International Journal of General Medicine, doi:10.2147/IJGM.S394413, Feb 2023
Retrospective 18,566 hospitalized patients in Japan, showing higher mortality with remdesivir treatment.
Gérard, Zhou, Wu, Kamo, Choi, Kim show increased risk of acute kidney injury, Leo, Briciu, Muntean, Petrov show increased risk of liver injury, and Negru, Cheng, Mohammed, Kwok show increased risk of cardiac disorders with remdesivir.
Standard of Care (SOC) for COVID-19 in the study country,
Japan, is very poor with very low average efficacy for approved treatments15.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 44.0% higher, OR 1.44, p < 0.01, adjusted per study, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Gérard et al., Remdesivir and Acute Renal Failure: A Potential Safety Signal From Disproportionality Analysis of the WHO Safety Database, Clinical Pharmacology & Therapeutics, doi:10.1002/cpt.2145.
2.
Zhou et al., Acute Kidney Injury and Drugs Prescribed for COVID-19 in Diabetes Patients: A Real-World Disproportionality Analysis, Frontiers in Pharmacology, doi:10.3389/fphar.2022.833679.
3.
Wu et al., Acute Kidney Injury Associated With Remdesivir: A Comprehensive Pharmacovigilance Analysis of COVID-19 Reports in FAERS, Frontiers in Pharmacology, doi:10.3389/fphar.2022.692828.
4.
Kamo et al., Association of Antiviral Drugs for the Treatment of COVID-19 With Acute Renal Failure, In Vivo, doi:10.21873/invivo.13637.
5.
Choi et al., Comparative effectiveness of combination therapy with nirmatrelvir–ritonavir and remdesivir versus monotherapy with remdesivir or nirmatrelvir–ritonavir in patients hospitalised with COVID-19: a target trial emulation study, The Lancet Infectious Diseases, doi:10.1016/S1473-3099(24)00353-0.
6.
Kim et al., Investigating the Safety Profile of Fast‐Track COVID‐19 Drugs Using the FDA Adverse Event Reporting System Database: A Comparative Observational Study, Pharmacoepidemiology and Drug Safety, doi:10.1002/pds.70043.
7.
Leo et al., Hepatocellular liver injury in hospitalized patients affected by COVID-19: Presence of different risk factors at different time points, Digestive and Liver Disease, doi:10.1016/j.dld.2021.12.014.
8.
Briciu et al., Evolving Clinical Manifestations and Outcomes in COVID-19 Patients: A Comparative Analysis of SARS-CoV-2 Variant Waves in a Romanian Hospital Setting, Pathogens, doi:10.3390/pathogens12121453.
9.
Muntean et al., Effects of COVID-19 on the Liver and Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta and Non-Delta Variants: An Analysis in a Single Centre, Pharmaceuticals, doi:10.3390/ph17010003.
10.
Petrov et al., The Effect of Potentially Hepatotoxic Medicinal Products on Alanine Transaminase Levels in COVID-19 Patients: A Case–Control Study, Safety and Risk of Pharmacotherapy, doi:10.30895/2312-7821-2025-458.
11.
Negru et al., Comparative Pharmacovigilance Analysis of Approved and Repurposed Antivirals for COVID-19: Insights from EudraVigilance Data, Biomedicines, doi:10.3390/biomedicines13061387.
12.
Cheng et al., Cardiovascular Safety of COVID-19 Treatments: A Disproportionality Analysis of Adverse Event Reports from the WHO VigiBase, Infectious Diseases and Therapy, doi:10.1007/s40121-025-01225-z.
13.
Mohammed et al., Bradycardia associated with remdesivir treatment in coronavirus disease 2019 patients: A propensity score-matched analysis, Medicine, doi:10.1097/MD.0000000000044501.
Mitsushima et al., 21 Feb 2023, retrospective, Japan, peer-reviewed, 3 authors.
Contact: mitsushi@niid.go.jp.
Risk of Underlying Diseases and Effectiveness of Drugs on COVID-19 Inpatients Assessed Using Medical Claims in Japan: Retrospective Observational Study
International Journal of General Medicine, doi:10.2147/ijgm.s394413
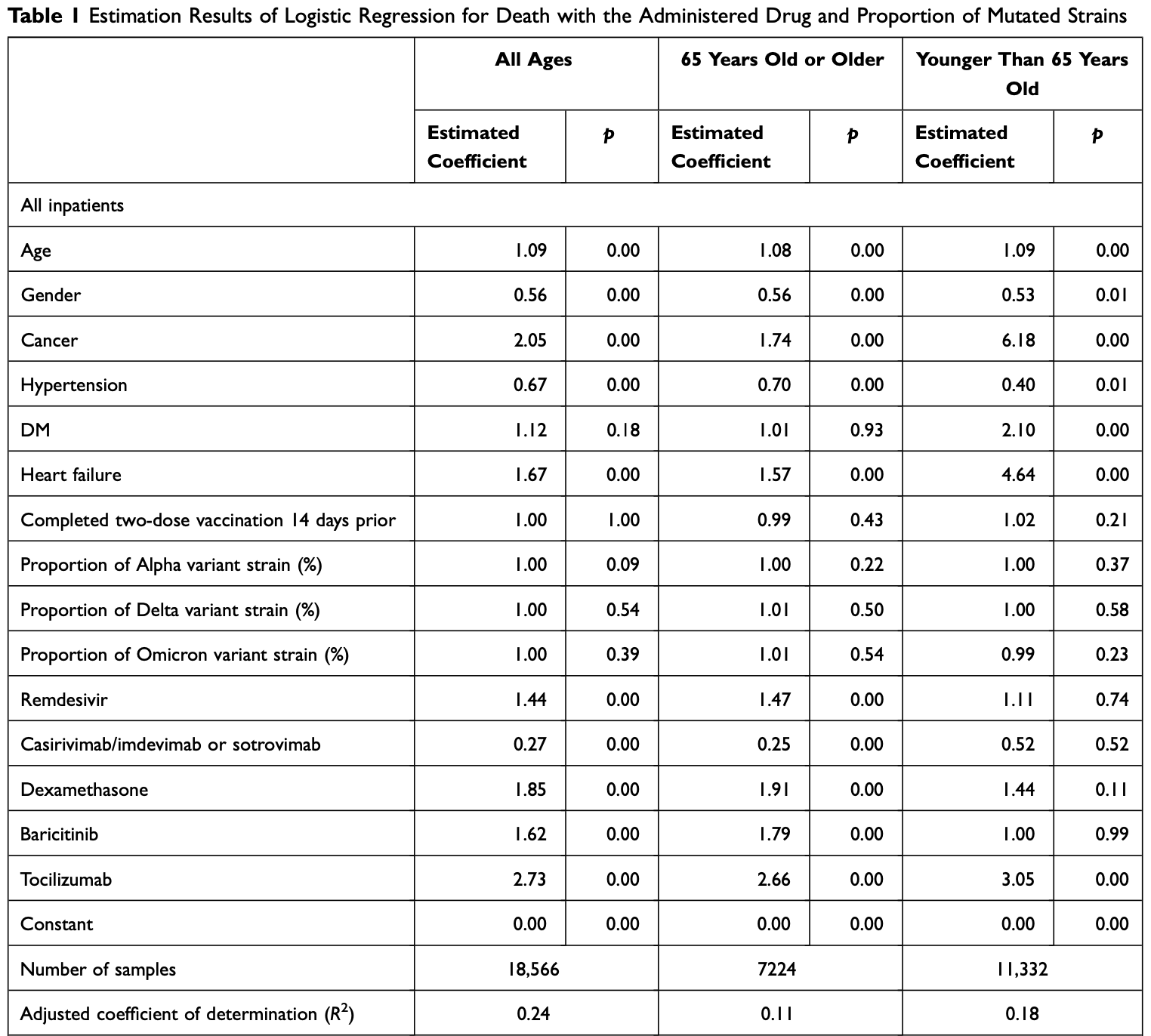
Background: Results of earlier studies have demonstrated underlying diseases such as cancer, diabetes mellitus, immunodeficiency, hypertension and heart failure to be risk factors for severe outcomes and mortality. Furthermore, clinical trials have shown that drugs such as antiviral drugs, antibody cocktails, steroids and anti-inflammatory drugs can be expected to prevent severe COVID-19 outcomes and death. Methods: This study, using inpatient records from the Medical Information Analysis Databank covering national hospital organizations in Japan, was conducted to evaluate the effects of underlying diseases and/or administered drugs on mortality. Subjects were all inpatients receiving oxygen administration and inpatients using respiratory ventilators, categorized by three age classes: all ages, patients 65 years old or older, and patients younger than 65 years old. We used logistic regression to analyze outcomes for underlying diseases, administered drugs, age, sex, the proportion of the mutated strains, and vaccine coverage. Results: Patients with hypertension, except for younger inpatients, have a lower risk of mortality (estimated coefficient 0.67 among all inpatients (p < 0.01): 0.77 among inpatients with oxygen therapy (p = 0.02) and 0.57 among inpatients with respiratory ventilation w (p = 0.01)). Except for younger inpatients, antibody cocktail (casirivimab/imdevimab or sotrovimab) administration was associated with a higher probability of survival (estimated coefficient 0.27 among all inpatients (p < 0.01)). It raised the survival probability consistently, although other drugs might have reduced the probability of survival. Conclusion: These findings suggest that antiviral drugs (remdesivir, estimated coefficient 1.44 (p < 0.01)), steroids (dexamethasone, estimated coefficient 1.85 (p < 0.01)), and anti-inflammatory drugs (baricitinib, estimated coefficient 1.62 (p < 0.01), and tocilizumab, estimated coefficient 2.73 (p < 0.01)) might not contribute to survival. These results have not been reported from earlier studies. More sophisticated estimation procedures, such as treatment effect models, are necessary to obtain conclusive results.
Ethical Considerations
Conclusion The obtained results demonstrated that patients with hypertension have a lower risk of mortality, except for younger patients, which suggests that hypertension might not pose a risk to survival. Results also show that only antibody cocktails (casirivimab/imdevimab or sotrovimab) raise the probability of survival consistently, although other drugs might reduce the probability of survival. In other words, other drugs such as antiviral drugs (remdesivir), steroids (dexamethasone), and anti-inflammatory drugs (baricitinib and tocilizumab) might not contribute to survival. These results have not been reported from any earlier study. More sophisticated estimation procedures such as treatment effect models must be used to obtain conclusive results.
Disclosure The authors report no conflicts of interest related to this work.
References
Abadie, Imbens, Bias-corrected matching estimators for average treatment effects, J Bus Econ Stat, doi:10.1198/jbes.2009.07333
Abadie, Imbens, Large sample properties of matching estimators for average treatment effects, Econometrica, doi:10.1111/j.1468-0262.2006.00655.x
Abadie, Imbens, On the failure of the bootstrap for matching estimators, Econometrica
Alhaddad, Almulaify, Alshabib, Relation between renin-angiotensin-aldosterone system inhibitors and COVID-19 severity, Cureus, doi:10.7759/cureus.22903
Bergqvist, Ahlqvist, Lundberg, HMG-CoA reductase inhibitors and COVID-19 mortality in Stockholm, Sweden: a registry-based cohort study, PLoS Med, doi:10.1371/journal.pmed.1003820
Bernal, Da Silva, Musungaie, Molnupiravir for oral treatment of Covid-19 in nonhospitalized patients, N Engl J Med, doi:10.1056/NEJMoa2116044
Cao, Wang, Wen, A trial of Lopinavir-Ritonavir in adults hospitalized with severe Covid-19, N Engl J Med, doi:10.1056/NEJMoa2001282
Capochiani, Frediani, Iervasi, Ruxolitinib rapidly reduces acute respiratory distress syndrome in COVID-19 disease. Analysis of data collection from RESPIRE protocol, Front Med, doi:10.3389/fmed.2020.00466
Chen, Yang, Gao, Influence of blood pressure control and application of renin-angiotensin-aldosterone system inhibitors on the outcomes in COVID-19 patients with hypertension, J Clin Hypertens, doi:10.1111/jch.14038
Cohen, Hanff, William, Continuation versus discontinuation of renin-angiotensin system inhibitors in patients admitted to hospital with COVID-19: a prospective, randomised, open-label trial, Lancet Respir Med, doi:10.1016/S2213-2600(20)30558-0
Del Sole, Farcomeni, Loffredo, Features of severe COVID-19: a systematic review and meta-analysis, Eur J Clin Invest, doi:10.1111/eci.13378
Duvignaud, Lhomme, Onaisi, Inhaled ciclesonide for outpatient treatment of COVID-19 in adults at risk of adverse outcomes: a randomised controlled trial (COVERAGE), Clin Microbiol Infect, doi:10.1016/j.cmi.2022.02.031
Fadini, Morieri, Longato, Avogaro, Prevalence and impact of diabetes among people infected with SARS-CoV-2, J Endocrinol Invest, doi:10.1007/s40618-020-01236-2
Fujii, Ibe, Ishigo, Early favipiravir treatment was associated with early defervescence in non-severe COVID-19 patients, J Infect Chemother, doi:10.1016/j.jiac.2021.04.013
Gordon, Mouncey, Interleukin-6 receptor antagonists in critically ill patients with Covid-19, N Engl J Med
Gunst, Staerke, Pahus, Efficacy of the TMPRSS2 inhibitor camostat mesilate in patients hospitalized with Covid-19-a double-blind randomized controlled trial, EClinicalMedicine, doi:10.1016/j.eclinm.2021.100849
Guo, Zhu, Hong, Decreased mortality of COVID-19 with renin-angiotensin-aldosterone system inhibitors therapy in patients with hypertension: a meta-analysis, Hypertension, doi:10.1161/HYPERTENSIONAHA.120.15572
Gupta, Gonzalez-Rojas, Juarez, Early treatment for Covid-19 with SARS-CoV-2 neutralizing antibody sotrovimab, N Engl J Med, doi:10.1056/NEJMoa2107934
Hammond, Leister-Tebbe, Gardner, Oral nirmatrelvir for high-risk, nonhospitalized adults with Covid-19, N Engl J Med, doi:10.1056/NEJMoa2118542
Horby, Lim, Emberson, Dexamethasone in hospitalized patients with Covid-19, N Engl J Med
Ioannidis, Infection fatality rate of COVID-19 inferred from seroprevalence data, Bull World Health Organ, doi:10.2471/BLT.20.265892
Ivashchenko, Dmitriev, Vostokova, AVIFAVIR for treatment of patients with moderate Coronavirus Disease 2019 (COVID-19): interim results of a Phase II/III multicenter randomized clinical trial, Clin Infect Dis, doi:10.1093/cid/ciaa1176
Javanmardi, Keshavarzi, Akbari, Emami, Pirbonyeh et al., Prevalence of underlying diseases in died cases of COVID-19: a systematic review and meta-analysis, PLoS One, doi:10.1371/journal.pone.0241265
Kanazawa, Tani, Imai, Horiguchi, Fushimi et al., Existing data sources for clinical epidemiology: database of the National Hospital Organization in Japan, Clin Epidemiol, doi:10.2147/CLEP.S359072
Killerby, Link-Gelles, Haight, Characteristics associated with hospitalization among patients with COVID-19 -Metropolitan Atlanta, Georgia, March, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm6925e1
Kurdi, Mueller, Weir, An umbrella review and meta-analysis of renin-angiotensin system drugs use and COVID-19 outcomes, Eur J Clin Invest, doi:10.1111/eci.13888
Kurita, Sugawara, Ohkusa, Pathogenicity of the omicron variant strain comparison with delta variant strain and seasonal influenza in Japan
Larson, Jarrett, Eckersberger, Smith, Paterson, Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012, Vaccine, doi:10.1016/j.vaccine.2014.01.081
Li, Huang, Zou, Epidemiology of COVID-19: a systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes, J Med Virol, doi:10.1002/jmv.26424
Liang, Guan, Chen, Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China, Lancet Oncol, doi:10.1016/S1470-2045(20)30096-6
López-Medina, López, Hurtado, Effect of ivermectin on time to resolution of symptoms among adults with mild COVID-19: a randomized clinical trial, JAMA, doi:10.1001/jama.2021.3071
Marconi, Ramanan, De Bono, Efficacy and safety of baricitinib for the treatment of hospitalised adults with COVID-19 (COV-BARRIER): a randomised, double-blind, parallel-group, placebo-controlled Phase 3 trial, Lancet Respir Med, doi:10.1016/S2213-2600(21)00331-3
Mozaffari, Chandak, Zhang, Remdesivir treatment in hospitalized patients with Coronavirus Disease 2019 (COVID-19): a comparative analysis of in-hospital all-cause mortality in a large multicenter observational cohort, Clin Infect Dis, doi:10.1093/cid/ciab875
Peng, He, Xue, Yang, Liu et al., Role of hypertension on the severity of COVID-19: a review, J Cardiovasc Pharmacol, doi:10.1097/FJC.0000000000001116
Pranata, Lim, Huang, Raharjo, Lukito, Hypertension is associated with increased mortality and severity of disease in COVID-19 pneumonia: a systematic review, meta-analysis and meta-regression, J Renin Angiotensin Aldosterone Syst, doi:10.1177/1470320320926899
Quinn, Gaughan, Bruce, Randomised controlled trial of intravenous nafamostat mesylate in COVID pneumonitis: phase 1b/2a experimental study to investigate safety, pharmacokinetics and pharmacodynamics, EBioMedicine, doi:10.1016/j.ebiom.2022.103856
Reynolds, Adhikari, Pulgarin, Renin-angiotensin-aldosterone system inhibitors and risk of Covid-19, N Engl J Med, doi:10.1056/NEJMoa2008975
Saini, Tagliamento, Lambertini, Mortality in patients with cancer and coronavirus disease 2019: a systematic review and pooled analysis of 52 studies, Eur J Cancer, doi:10.1016/j.ejca.2020.08.011
Salama, Han, Yau, Tocilizumab in patients hospitalized with Covid-19 pneumonia, N Engl J Med, doi:10.1056/NEJMoa2030340
Salunke, Nandy, Pathak, Impact of COVID-19 in cancer patients on severity of disease and fatal outcomes: a systematic review and meta-analysis, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.07.037
Sharafeldin, Bates, Song, Outcomes of COVID-19 in patients with cancer: report from the national COVID cohort collaborative (N3C), J Clin Oncol, doi:10.1200/JCO.21.01074
Suissa, Immortal time bias in pharmaco-epidemiology, Am J Epidemiol, doi:10.1093/aje/kwm324
Terada-Hirashima, Suzuki, Tsujimoto, Impact of inhaled ciclesonide on asymptomatic or mild COVID-19: a randomized trial, Drug Discov Ther, doi:10.5582/ddt.2022.01068
Thompson, Burgess, Naleway, Prevention and attenuation of Covid-19 with the BNT162b2 and mRNA-1273 vaccines, N Engl J Med, doi:10.1056/NEJMoa2107058
Umakanthan, Bukelo, Bukelo, Patil, Subramaniam et al., Social environmental predictors of COVID-19 vaccine hesitancy in India: a population-based survey, Vaccines, doi:10.3390/vaccines10101749
Umakanthan, Lawrence, Predictors of COVID-19 vaccine hesitancy in Germany: a cross-sectional, population-based study, Postgrad Med J, doi:10.1136/postgradmedj-2021-141365
Umakanthan, Sahu, Ranade, Origin, transmission, diagnosis and management of coronavirus disease 2019 (COVID-19), Postgrad Med J, doi:10.1136/postgradmedj-2020-138234
Umakanthan, Senthil, John, The effect of statins on clinical outcome among hospitalized patients with COVID-19: a multi-centric cohort study, Front Pharmacol, doi:10.3389/fphar.2022.742273
Venkatesulu, Chandrasekar, Girdhar, A systematic review and meta-analysis of cancer patients affected by a novel coronavirus, JNCI Cancer Spectr, doi:10.1093/jncics/pkaa102
Weinreich, Sivapalasingam, Norton, REGEN-COV antibody combination and outcomes in outpatients with Covid-19, N Engl J Med, doi:10.1056/NEJMoa2108163
Williamson, Ravani, Marginal structural models in clinical research: when and how to use them?, Nephrol Dial Transplant, doi:10.1093/ndt/gfw341
Williamson, Walker, Bhaskaran, Factors associated with COVID-19-related death using OpenSAFELY, Nature, doi:10.1038/s41586-020-2521-4
Wong, Au, Lau, Lau, Cowling et al., Real-world effectiveness of molnupiravir and nirmatrelvir plus ritonavir against mortality, hospitalisation, and in-hospital outcomes among community-dwelling, ambulatory patients with confirmed SARS-CoV-2 infection during the omicron wave in Hong Kong: an observational study, Lancet, doi:10.1016/S0140-6736(22)01586-0
Wu, Zuo, Kang, Multi-organ dysfunction in patients with COVID-19: a systematic review and meta-analysis, Aging Dis, doi:10.14336/AD.2020.0520
Zhang, Wu, Sun, Association of hypertension with the severity and fatality of SARS-CoV-2 infection: a meta-analysis, Epidemiol Infect, doi:10.1017/S095026882000117X
Zheng, Peng, Xu, Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis, J Infect, doi:10.1016/j.jinf.2020.04.021
Zhou, Yang, Chi, Comorbidities and the risk of severe or fatal outcomes associated with coronavirus disease 2019: a systematic review and meta-analysis, Int J Infect Dis, doi:10.1016/j.ijid.2020.07.029
DOI record:
{
"DOI": "10.2147/ijgm.s394413",
"ISSN": [
"1178-7074"
],
"URL": "http://dx.doi.org/10.2147/IJGM.S394413",
"author": [
{
"ORCID": "http://orcid.org/0000-0002-5827-5475",
"affiliation": [],
"authenticated-orcid": true,
"family": "Mitsushima",
"given": "Shingo",
"sequence": "first"
},
{
"affiliation": [],
"family": "Horiguchi",
"given": "Hiromasa",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4584-6168",
"affiliation": [],
"authenticated-orcid": true,
"family": "Taniguchi",
"given": "Kiyosu",
"sequence": "additional"
}
],
"container-title": "International Journal of General Medicine",
"container-title-short": "IJGM",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
2,
21
]
],
"date-time": "2023-02-21T08:03:46Z",
"timestamp": 1676966626000
},
"deposited": {
"date-parts": [
[
2023,
2,
21
]
],
"date-time": "2023-02-21T08:03:52Z",
"timestamp": 1676966632000
},
"indexed": {
"date-parts": [
[
2023,
2,
22
]
],
"date-time": "2023-02-22T05:29:47Z",
"timestamp": 1677043787035
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
2
]
]
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc/3.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
2,
1
]
],
"date-time": "2023-02-01T00:00:00Z",
"timestamp": 1675209600000
}
}
],
"link": [
{
"URL": "https://www.dovepress.com/getfile.php?fileID=87671",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.dovepress.com/getfile.php?fileID=87671",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "301",
"original-title": [],
"page": "657-672",
"prefix": "10.2147",
"published": {
"date-parts": [
[
2023,
2
]
]
},
"published-online": {
"date-parts": [
[
2023,
2
]
]
},
"publisher": "Informa UK Limited",
"reference": [
{
"DOI": "10.1136/postgradmedj-2020-138234",
"author": "Umakanthan",
"doi-asserted-by": "publisher",
"first-page": "753",
"journal-title": "Postgrad Med J",
"key": "ref1",
"volume": "96",
"year": "2020"
},
{
"DOI": "10.2471/BLT.20.265892",
"author": "Ioannidis",
"doi-asserted-by": "publisher",
"first-page": "19",
"journal-title": "Bull World Health Organ",
"key": "ref2",
"volume": "99",
"year": "2021"
},
{
"DOI": "10.1016/j.ejca.2020.08.011",
"author": "Saini",
"doi-asserted-by": "publisher",
"first-page": "43",
"journal-title": "Eur J Cancer",
"key": "ref3",
"volume": "139",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.07.029",
"author": "Zhou",
"doi-asserted-by": "publisher",
"first-page": "47",
"journal-title": "Int J Infect Dis",
"key": "ref4",
"volume": "99",
"year": "2020"
},
{
"DOI": "10.1093/jncics/pkaa102",
"author": "Venkatesulu",
"doi-asserted-by": "publisher",
"first-page": "pkaa102",
"journal-title": "JNCI Cancer Spectr",
"key": "ref5",
"volume": "5",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2020.07.037",
"author": "Salunke",
"doi-asserted-by": "publisher",
"first-page": "1431",
"journal-title": "Diabetes Metab Syndr",
"key": "ref6",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/S1470-2045(20)30096-6",
"author": "Liang",
"doi-asserted-by": "publisher",
"first-page": "335",
"journal-title": "Lancet Oncol",
"key": "ref7",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0241265",
"author": "Javanmardi",
"doi-asserted-by": "publisher",
"first-page": "e0241265",
"journal-title": "PLoS One",
"key": "ref8",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1111/eci.13378",
"author": "Del Sole",
"doi-asserted-by": "publisher",
"first-page": "e13378",
"journal-title": "Eur J Clin Invest",
"key": "ref9",
"volume": "50",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26424",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "1449",
"journal-title": "J Med Virol",
"key": "ref10",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1016/j.jinf.2020.04.021",
"author": "Zheng",
"doi-asserted-by": "publisher",
"first-page": "e16",
"journal-title": "J Infect",
"key": "ref11",
"volume": "81",
"year": "2020"
},
{
"DOI": "10.1007/s40618-020-01236-2",
"author": "Fadini",
"doi-asserted-by": "publisher",
"first-page": "867",
"journal-title": "J Endocrinol Invest",
"key": "ref12",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"author": "Williamson",
"doi-asserted-by": "publisher",
"first-page": "430",
"journal-title": "Nature",
"key": "ref13",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.15585/mmwr.mm6925e1",
"author": "Killerby",
"doi-asserted-by": "publisher",
"first-page": "790",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "ref14",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.14336/AD.2020.0520",
"author": "Wu",
"doi-asserted-by": "publisher",
"first-page": "874",
"journal-title": "Aging Dis",
"key": "ref15",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1017/S095026882000117X",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "e106",
"journal-title": "Epidemiol Infect",
"key": "ref16",
"volume": "148",
"year": "2020"
},
{
"DOI": "10.1177/1470320320926899",
"author": "Pranata",
"doi-asserted-by": "publisher",
"first-page": "1470320320926899",
"journal-title": "J Renin Angiotensin Aldosterone Syst",
"key": "ref17",
"volume": "21",
"year": "2020"
},
{
"key": "ref18",
"unstructured": "The Cabinet Secretariat. Vaccination against SARS-CoV-2. Available from: https://www.kantei.go.jp/jp/headline/kansensho/vaccine.html. Accessed January 11, 2023."
},
{
"DOI": "10.1136/postgradmedj-2021-141365",
"author": "Umakanthan",
"doi-asserted-by": "publisher",
"first-page": "756",
"journal-title": "Postgrad Med J",
"key": "ref19",
"volume": "98",
"year": "2022"
},
{
"DOI": "10.1093/cid/ciab875",
"author": "Mozaffari",
"doi-asserted-by": "publisher",
"first-page": "e450",
"journal-title": "Clin Infect Dis",
"key": "ref20",
"volume": "75",
"year": "2022"
},
{
"DOI": "10.1056/NEJMoa2108163",
"author": "Weinreich",
"doi-asserted-by": "publisher",
"first-page": "e81",
"journal-title": "N Engl J Med",
"key": "ref21",
"volume": "385",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2107934",
"author": "Gupta",
"doi-asserted-by": "publisher",
"first-page": "1941",
"journal-title": "N Engl J Med",
"key": "ref22",
"volume": "385",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2021436",
"author": "Horby",
"doi-asserted-by": "crossref",
"first-page": "693",
"journal-title": "N Engl J Med",
"key": "ref23",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1016/S2213-2600(21)00331-3",
"author": "Marconi",
"doi-asserted-by": "publisher",
"first-page": "1407",
"journal-title": "Lancet Respir Med",
"key": "ref24",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2030340",
"author": "Salama",
"doi-asserted-by": "publisher",
"first-page": "20",
"journal-title": "N Engl J Med",
"key": "ref25",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2100433",
"author": "Gordon",
"doi-asserted-by": "crossref",
"first-page": "1491",
"journal-title": "N Engl J Med",
"key": "ref26",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.3389/fphar.2022.742273",
"author": "Umakanthan",
"doi-asserted-by": "publisher",
"first-page": "742273",
"journal-title": "Front Pharmacol",
"key": "ref27",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1371/journal.pmed.1003820",
"author": "Bergqvist",
"doi-asserted-by": "publisher",
"first-page": "e1003820",
"journal-title": "PLoS Med",
"key": "ref28",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(22)01586-0",
"author": "Wong",
"doi-asserted-by": "publisher",
"first-page": "1213",
"journal-title": "Lancet",
"key": "ref29",
"volume": "400",
"year": "2022"
},
{
"DOI": "10.1056/NEJMoa2116044",
"author": "Jayk Bernal",
"doi-asserted-by": "publisher",
"first-page": "509",
"journal-title": "N Engl J Med",
"key": "ref30",
"volume": "386",
"year": "2022"
},
{
"DOI": "10.1056/NEJMoa2118542",
"author": "Hammond",
"doi-asserted-by": "publisher",
"first-page": "1397",
"journal-title": "N Engl J Med",
"key": "ref31",
"volume": "386",
"year": "2022"
},
{
"key": "ref32",
"unstructured": "Ministry of Health, Labour and Welfare. 医療施設調査 [Survey of medical institutions]. Japanese. Available from: https://www.mhlw.go.jp/toukei/saikin/hw/iryosd/20a/. Accessed June 20, 2022."
},
{
"DOI": "10.2147/CLEP.S359072",
"author": "Kanazawa",
"doi-asserted-by": "publisher",
"first-page": "689",
"journal-title": "Clin Epidemiol",
"key": "ref33",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1093/cid/ciaa1176",
"author": "Ivashchenko",
"doi-asserted-by": "publisher",
"first-page": "531",
"journal-title": "Clin Infect Dis",
"key": "ref34",
"volume": "73",
"year": "2021"
},
{
"DOI": "10.1016/j.jiac.2021.04.013",
"author": "Fujii",
"doi-asserted-by": "publisher",
"first-page": "1051",
"journal-title": "J Infect Chemother",
"key": "ref35",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.3389/fmed.2020.00466",
"author": "Capochiani",
"doi-asserted-by": "publisher",
"first-page": "466",
"journal-title": "Front Med",
"key": "ref36",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2001282",
"author": "Cao",
"doi-asserted-by": "publisher",
"first-page": "1787",
"journal-title": "N Engl J Med",
"key": "ref37",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1016/j.ebiom.2022.103856",
"author": "Quinn",
"doi-asserted-by": "publisher",
"first-page": "103856",
"journal-title": "EBioMedicine",
"key": "ref38",
"volume": "76",
"year": "2022"
},
{
"DOI": "10.1016/j.eclinm.2021.100849",
"author": "Gunst",
"doi-asserted-by": "publisher",
"first-page": "100849",
"journal-title": "EClinicalMedicine",
"key": "ref39",
"volume": "35",
"year": "2021"
},
{
"DOI": "10.1016/j.cmi.2022.02.031",
"author": "Duvignaud",
"doi-asserted-by": "publisher",
"first-page": "1010",
"journal-title": "Clin Microbiol Infect",
"key": "ref40",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.5582/ddt.2022.01068",
"author": "Terada-Hirashima",
"doi-asserted-by": "publisher",
"first-page": "225",
"journal-title": "Drug Discov Ther",
"key": "ref41",
"volume": "16",
"year": "2022"
},
{
"DOI": "10.1001/jama.2021.3071",
"author": "López-Medina",
"doi-asserted-by": "publisher",
"first-page": "1426",
"journal-title": "JAMA",
"key": "ref42",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.1111/j.1468-0262.2006.00655.x",
"author": "Abadie",
"doi-asserted-by": "publisher",
"first-page": "235",
"journal-title": "Econometrica",
"key": "ref43",
"volume": "74",
"year": "2006"
},
{
"DOI": "10.3982/ECTA6474",
"author": "Abadie",
"doi-asserted-by": "crossref",
"first-page": "1537",
"journal-title": "Econometrica",
"key": "ref44",
"volume": "76",
"year": "2008"
},
{
"DOI": "10.1198/jbes.2009.07333",
"author": "Abadie",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Bus Econ Stat",
"key": "ref45",
"volume": "29",
"year": "2011"
},
{
"DOI": "10.1016/S2213-2600(20)30558-0",
"author": "Cohen",
"doi-asserted-by": "publisher",
"first-page": "275",
"journal-title": "Lancet Respir Med",
"key": "ref46",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2008975",
"author": "Reynolds",
"doi-asserted-by": "publisher",
"first-page": "2441",
"journal-title": "N Engl J Med",
"key": "ref47",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.7759/cureus.22903",
"author": "Alhaddad",
"doi-asserted-by": "publisher",
"first-page": "e22903",
"journal-title": "Cureus",
"key": "ref48",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1111/eci.13888",
"author": "Kurdi",
"doi-asserted-by": "publisher",
"first-page": "e13888",
"journal-title": "Eur J Clin Invest",
"key": "ref49",
"volume": "53",
"year": "2023"
},
{
"DOI": "10.1161/HYPERTENSIONAHA.120.15572",
"author": "Guo",
"doi-asserted-by": "publisher",
"first-page": "e13",
"journal-title": "Hypertension",
"key": "ref50",
"volume": "76",
"year": "2020"
},
{
"DOI": "10.1097/FJC.0000000000001116",
"author": "Peng",
"doi-asserted-by": "publisher",
"first-page": "e648",
"journal-title": "J Cardiovasc Pharmacol",
"key": "ref51",
"volume": "78",
"year": "2021"
},
{
"DOI": "10.1111/jch.14038",
"author": "Chen",
"doi-asserted-by": "publisher",
"first-page": "1974",
"journal-title": "J Clin Hypertens",
"key": "ref52",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.1200/JCO.21.01074",
"author": "Sharafeldin",
"doi-asserted-by": "publisher",
"first-page": "2232",
"journal-title": "J Clin Oncol",
"key": "ref53",
"volume": "39",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2107058",
"author": "Thompson",
"doi-asserted-by": "publisher",
"first-page": "320",
"journal-title": "N Engl J Med",
"key": "ref54",
"volume": "385",
"year": "2021"
},
{
"DOI": "10.1016/j.vaccine.2014.01.081",
"author": "Larson",
"doi-asserted-by": "publisher",
"first-page": "2150",
"journal-title": "Vaccine",
"key": "ref55",
"volume": "32",
"year": "2014"
},
{
"DOI": "10.3390/vaccines10101749",
"author": "Umakanthan",
"doi-asserted-by": "publisher",
"first-page": "1749",
"journal-title": "Vaccines",
"key": "ref56",
"volume": "10",
"year": "2022"
},
{
"key": "ref57",
"unstructured": "Kurita J, Sugawara T, Ohkusa Y. Pathogenicity of the omicron variant strain comparison with delta variant strain and seasonal influenza in Japan. Available from: https://jxiv.jst.go.jp/index.php/jxiv/preprint/view/59. Accessed August 10, 2022."
},
{
"DOI": "10.1093/aje/kwm324",
"author": "Suissa",
"doi-asserted-by": "publisher",
"first-page": "492",
"journal-title": "Am J Epidemiol",
"key": "ref58",
"volume": "167",
"year": "2008"
},
{
"DOI": "10.1093/ndt/gfw341",
"author": "Williamson",
"doi-asserted-by": "publisher",
"first-page": "ii84",
"journal-title": "Nephrol Dial Transplant",
"key": "ref59",
"volume": "32",
"year": "2017"
}
],
"reference-count": 59,
"references-count": 59,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.dovepress.com/risk-of-underlying-diseases-and-effectiveness-of-drugs-on-covid-19-inp-peer-reviewed-fulltext-article-IJGM"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Risk of Underlying Diseases and Effectiveness of Drugs on COVID-19 Inpatients Assessed Using Medical Claims in Japan: Retrospective Observational Study",
"type": "journal-article",
"volume": "Volume 16"
}