Fluoxetine and Sertraline Potently Neutralize the Replication of Distinct SARS-CoV-2 Variants
et al., Viruses, doi:10.3390/v16040545, Mar 2024
31st treatment shown to reduce risk in
November 2021, now with p = 0.00014 from 21 studies, recognized in 2 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
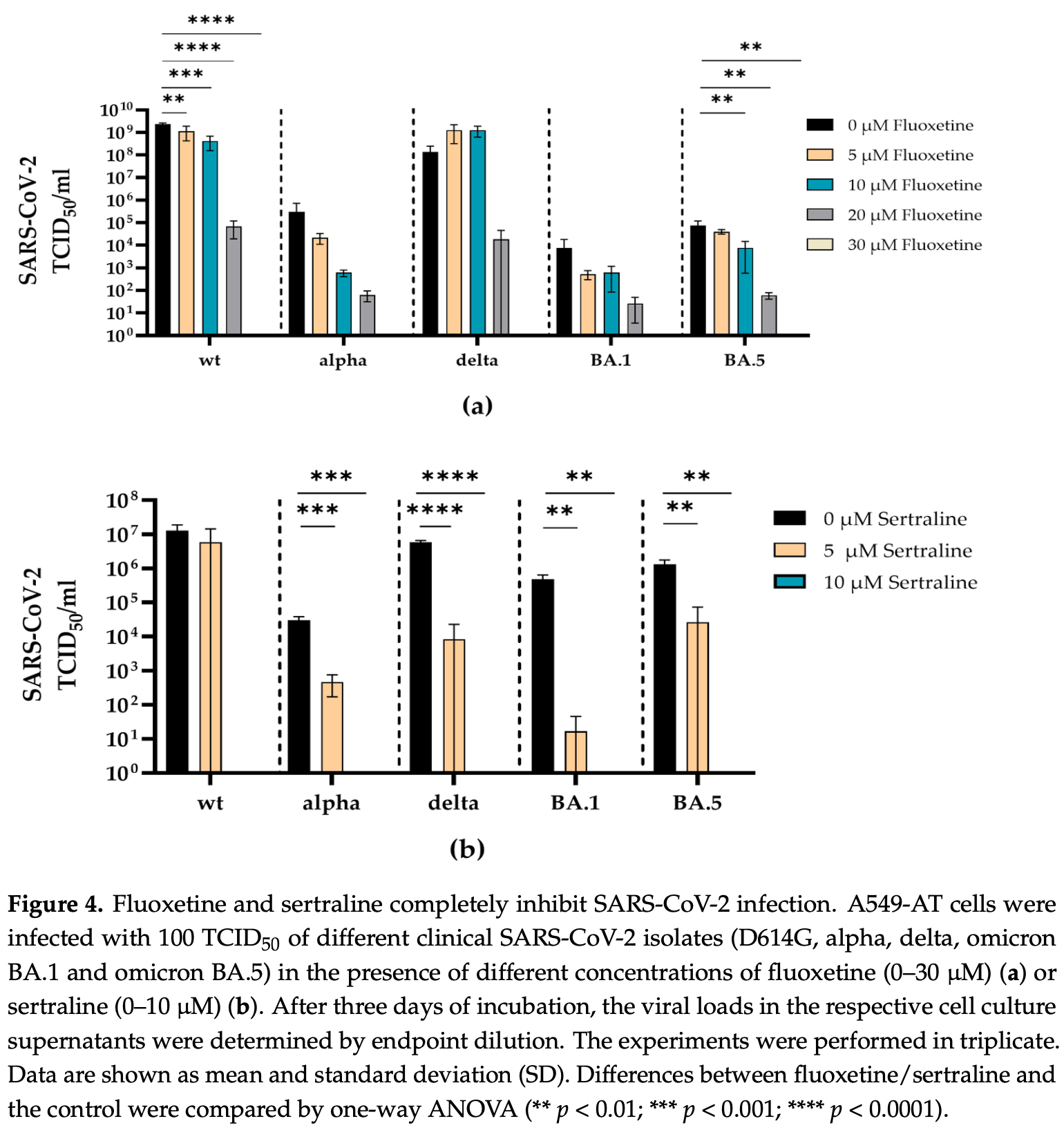
In vitro study showing that fluoxetine and sertraline potently neutralize the replication of distinct SARS-CoV-2 variants at subtoxic concentrations. Authors demonstrate that fluoxetine and sertraline inhibit infection with pseudotyped virus-like particles and clinical isolates of SARS-CoV-2 variants D614G, alpha, delta, omicron BA.1, and omicron BA.5 in A549 lung cells overexpressing ACE2 and TMPRSS2. Complete inhibition was achieved at 30μM fluoxetine or 10μM sertraline. The inhibitory effects were validated by RT-qPCR quantification of SARS-CoV-2 M- and N-gene RNA levels. No substantial cytotoxicity was observed at the effective concentrations. As fluvoxamine is a closely related, it may also provide similar inhibition.
5 preclinical studies support the efficacy of fluvoxamine for COVID-19:
Fluvoxamine may inhibit SARS-CoV-2 cell entry by preventing the formation of ceramide platforms that facilitates viral uptake1, may help restore autophagic processes disrupted by NSP6, thereby reducing SARS-CoV-2 replication and improving host cellular defenses3, and may reduce COVID-19 thrombotic complications by inhibiting serotonin reuptake and decreasing platelet activation4.
1.
Alkafaas et al., Molecular docking as a tool for the discovery of novel insight about the role of acid sphingomyelinase inhibitors in SARS- CoV-2 infectivity, BMC Public Health, doi:10.1186/s12889-024-17747-z.
2.
Abatematteo et al., A conformational rearrangement of the SARS-CoV-2 host protein sigma-1 is required for antiviral activity: insights from a combined in-silico/in-vitro approach, Scientific Reports, doi:10.1038/s41598-023-39662-w.
Thümmler et al., 30 Mar 2024, peer-reviewed, 21 authors.
Contact: adalbert.krawczyk@uk-essen.de (corresponding author), laura.thuemmler@uk-essen.de, peer.brass@uk-essen.de, maren.bormann@uk-essen.de, leonie.brochhagen@uk-essen.de, oliver.witzke@uk-essen.de, monika.lindemann@uk-essen.de, peter.horn@uk-essen.de, carolin.sehl@uk-essen.de, matthias.soddemann@uk-essen.de, stephanie.kadow@uk-essen.de, erich.gulbins@uk-essen.de, katrin.becker-flegler@uni-due.de, carina.elsner@uk-essen.de, ulf.dittmer@uk-essen.de, nicolas.hoertel@aphp.fr, celine.cougoule@ipbs.fr, sandra.ciesek@ukffm.de, marek.widera@ukffm.de, markus.kamler@uk-essen.de.
In vitro studies are an important part of preclinical research, however results may be very different in vivo.
Fluoxetine and Sertraline Potently Neutralize the Replication of Distinct SARS-CoV-2 Variants
Viruses, doi:10.3390/v16040545
The pandemic caused by SARS-CoV-2 is still a major health problem. Newly emerging variants and long-COVID-19 represent a challenge for the global health system. In particular, individuals in developing countries with insufficient health care need easily accessible, affordable and effective treatments of COVID-19. Previous studies have demonstrated the efficacy of functional inhibitors of acid sphingomyelinase against infections with various viruses, including early variants of SARS-CoV-2. This work investigated whether the acid sphingomyelinase inhibitors fluoxetine and sertraline, usually used as antidepressant molecules in clinical practice, can inhibit the replication of the former and recently emerged SARS-CoV-2 variants in vitro. Fluoxetine and sertraline potently inhibited the infection with pseudotyped virus-like particles and SARS-CoV-2 variants D614G, alpha, delta, omicron BA.1 and omicron BA.5. These results highlight fluoxetine and sertraline as priority candidates for large-scale phase 3 clinical trials at different stages of SARS-CoV-2 infections, either alone or in combination with other medications.
spike protein. This is an interesting finding, as fluoxetine and sertraline were described to interfere with SARS-CoV-2 entry, and at least sertraline directly targeted the SARS-CoV-2 spike protein [7] . In addition to targeting the spike protein, fluoxetine and sertraline were described as functional inhibitors of the acid sphingomyelinase (ASM), which plays an important role during SARS-CoV-2 entry into the host cell [38, 39] . ASM is a glycoprotein that catalyzes sphingomyelin degradation to phosphorylcholine and ceramide, which is known to facilitate viral entry into the host cell [40] [41] [42] . SARS-CoV-2 activates the ASM/ceramide system, resulting in the formation of ceramide-enriched membrane domains that cluster ACE2 and thereby facilitate viral entry and infection [39, 40, 43] . Thus, inhibiting ASM represents a SARS-CoV-2 spike mutation-independent mechanism to interfere with viral entry and infection. In the context of other viral infections, our data indicate that FIASMAs are effective not only against, for example, rhinoviruses [44] or ebolaviruses [45] , but also against SARS-CoV-2. In line with prior studies, our findings suggest that fluoxetine and sertraline use in early-stage SARS-CoV-2 infections with recent variants may reduce the risk of a severe course of COVID-19 or death [46] . However, we have demonstrated the antiviral efficacy of fluoxetine and sertraline against the respective SARS-CoV-2 variants in cell culture. Nonetheless, deriving..
References
Albouz, Boutry, Dubois, Bourdon, Hauw et al., Lipid and lysosomal enzymes in human fibroblasts cultured with perhexiline maleate, Naunyn-Schmiedebergs Arch. Pharmacol, doi:10.1007/BF00500076
Becker, Carpinteiro, Hoffmann, Pöhlmann, Kornhuber et al., Ex vivo assay to evaluate the efficacy of drugs targeting sphingolipids in preventing SARS-CoV-2 infection of nasal epithelial cells, STAR Protoc, doi:10.1016/j.xpro.2021.100356
Beckmann, Becker, Ceramide and Related Molecules in Viral Infections, Int. J. Mol. Sci, doi:10.3390/ijms22115676
Berger Rentsch, Zimmer, A vesicular stomatitis virus replicon-based bioassay for the rapid and sensitive determination of multi-species type I interferon, PLoS ONE, doi:10.1371/journal.pone.0025858
Bergwerk, Gonen, Lustig, Amit, Lipsitch et al., Covid-19 Breakthrough Infections in Vaccinated Health Care Workers, N. Engl. J. Med, doi:10.1056/NEJMoa2109072
Bormann, Brochhagen, Alt, Otte, Thümmler et al., Immune responses in COVID-19 patients during breakthrough infection with SARS-CoV-2 variants Delta, Omicron-BA.1 and Omicron-BA.5, Front. Immunol, doi:10.3389/fimmu.2023.1150667
Calusic, Marcec, Luksa, Jurkovic, Kovac et al., Safety and efficacy of fluvoxamine in COVID-19 ICU patients: An open label, prospective cohort trial with matched controls, Br. J. Clin. Pharmacol, doi:10.1111/bcp.15126
Carpinteiro, Edwards, Hoffmann, Kochs, Gripp et al., Pharmacological Inhibition of Acid Sphingomyelinase Prevents Uptake of SARS-CoV-2 by Epithelial Cells, Cell Rep. Med, doi:10.1016/j.xcrm.2020.100142
Carpinteiro, Gripp, Hoffmann, Pöhlmann, Hoertel et al., Inhibition of acid sphingomyelinase by ambroxol prevents SARS-CoV-2 entry into epithelial cells, J. Biol. Chem, doi:10.1016/j.jbc.2021.100701
Chen, Wu, Chen, Zhan, Wu et al., Sertraline Is an Effective SARS-CoV-2 Entry Inhibitor Targeting the Spike Protein, J. Virol, doi:10.1128/jvi.01245-22
Dash, Barqawi, Obaideen, Al Chame, Samara et al., COVID-19 Breakthrough Infection Among Vaccinated Population in the United Arab Emirates, J. Epidemiol. Glob. Health, doi:10.1007/s44197-023-00090-8
Fred, Kuivanen, Ugurlu, Casarotto, Levanov et al., Antidepressant and Antipsychotic Drugs Reduce Viral Infection by SARS-CoV-2 and Fluoxetine Shows Antiviral Activity Against the Novel Variants in vitro, Front. Pharmacol, doi:10.3389/fphar.2021.755600
Geiger, Kersting, Schlegel, Stelz, Fähr et al., The Acid Ceramidase Is a SARS-CoV-2 Host Factor, Cells, doi:10.3390/cells11162532
Grassme, Riehle, Wilker, Gulbins, Rhinoviruses infect human epithelial cells via ceramide-enriched membrane platforms, J. Biol. Chem, doi:10.1074/jbc.M500835200
Hashimoto, Suzuki, Hashimoto, Mechanisms of action of fluvoxamine for COVID-19: A historical review, Mol. Psychiatry, doi:10.1038/s41380-021-01432-3
Heilingloh, Aufderhorst, Schipper, Dittmer, Witzke et al., Susceptibility of SARS-CoV-2 to UV irradiation, Am. J. Infect. Control, doi:10.1016/j.ajic.2020.07.031
Herring, Oda, Wagoner, Kirchmeier, O'connor et al., Inhibition of Arenaviruses by Combinations of Orally Available Approved Drugs, Antimicrob. Agents Chemother, doi:10.1128/AAC.01146-20
Hoertel, Do the Selective Serotonin Reuptake Inhibitor Antidepressants Fluoxetine and Fluvoxamine Reduce Mortality among Patients with COVID-19?, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2021.36510
Hoertel, Rezaei, Sánchez-Rico, Delgado-Álvarez, Kornhuber et al., Medications Modulating the Acid Sphingomyelinase/Ceramide System and 28-Day Mortality among Patients with SARS-CoV-2: An Observational Study, Pharmaceuticals, doi:10.3390/ph16081107
Hoertel, Sánchez-Rico, Cougoule, Gulbins, Kornhuber et al., Repurposing antidepressants inhibiting the sphingomyelinase acid/ceramide system against COVID-19: Current evidence and potential mechanisms, Mol. Psychiatry, doi:10.1038/s41380-021-01254-3
Hoffmann, Hofmann-Winkler, Krüger, Kempf, Nehlmeier et al., SARS-CoV-2 variant B.1.617 is resistant to bamlanivimab and evades antibodies induced by infection and vaccination, Cell Rep, doi:10.1016/j.celrep.2021.109415
Hoffmann, Kleine-Weber, Schroeder, Krüger, Herrler et al., SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor, Cell, doi:10.1016/j.cell.2020.02.052
Hurwitz, Ferlinz, Sandhoff, The Tricyclic Antidepressant Desipramine Causes Proteolytic Degradation of Lysosomal Sphingomyelinase in Human Fibroblasts, Biol. Chem. Hoppe-Seyler, doi:10.1515/bchm3.1994.375.7.447
Jittamala, Boyd, Schilling, Watson, Ngamprasertchai et al., Antiviral efficacy of fluoxetine in early symptomatic COVID-19: An open-label, randomised, controlled, adaptive platform trial (PLATCOV), doi:10.1101/2024.01.16.24301337
Kornhuber, Hoertel, Gulbins, The acid sphingomyelinase/ceramide system in COVID-19, Mol. Psychiatry, doi:10.1038/s41380-021-01309-5
Kornhuber, Tripal, Reichel, Mühle, Rhein et al., Functional Inhibitors of Acid Sphingomyelinase (FIASMAs): A novel pharmacological group of drugs with broad clinical applications, Cell Physiol. Biochem, doi:10.1159/000315101
Kutkat, Moatasim, Al-Karmalawy, Abulkhair, Gomaa et al., Robust antiviral activity of commonly prescribed antidepressants against emerging coronaviruses: In vitro and in silico drug repurposing studies, Sci. Rep, doi:10.1038/s41598-022-17082-6
Lenze, Mattar, Zorumski, Stevens, Schweiger et al., Fluvoxamine vs Placebo and Clinical Deterioration in Outpatients with Symptomatic COVID-19: A Randomized Clinical Trial, JAMA, doi:10.1001/jama.2020.22760
Manganaro, Zonsics, Bauer, Lopez, Donselaar et al., Synthesis and antiviral effect of novel fluoxetine analogues as enterovirus 2C inhibitors, Antivir. Res, doi:10.1016/j.antiviral.2020.104781
Messacar, Sillau, Hopkins, Otten, Wilson-Murphy et al., Safety, tolerability, and efficacy of fluoxetine as an antiviral for acute flaccid myelitis, Neurology, doi:10.1212/WNL.0000000000006670
Miller, Adhikary, Kolokoltsov, Davey, Ebolavirus requires acid sphingomyelinase activity and plasma membrane sphingomyelin for infection, J. Virol, doi:10.1128/JVI.00136-12
Oskotsky, Maric, Tang, Oskotsky, Wong et al., Mortality Risk Among Patients with COVID-19 Prescribed Selective Serotonin Reuptake Inhibitor Antidepressants, JAMA Netw Open
Panneer, Kantamaneni, Akkayasamy, Susairaj, Panda et al., The Great Lockdown in the Wake of COVID-19 and Its Implications: Lessons for Low and Middle-Income Countries, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph19010610
Patel, Lim, Cheng, Lawitz, Tillmann et al., Open-label Phase 1b pilot study to assess the antiviral efficacy of simvastatin combined with sertraline in chronic hepatitis C patients, Antivir. Ther, doi:10.3851/IMP1898
Péricat, Leon-Icaza, Sanchez Rico, Mühle, Zoicas et al., Antiviral and Anti-Inflammatory Activities of Fluoxetine in a SARS-CoV-2 Infection Mouse Model, Int. J. Mol. Sci, doi:10.3390/ijms232113623
Reis, Dos, Moreira-Silva, Silva, Thabane et al., Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with COVID-19: The TOGETHER randomised, platform clinical trial, Lancet Glob. Health, doi:10.1016/S2214-109X(21)00448-4
Reis, Dos, Silva, Medeiros Silva, Thabane et al., Oral Fluvoxamine with Inhaled Budesonide for Treatment of Early-Onset COVID-19: A Randomized Platform Trial, Ann. Intern. Med, doi:10.7326/M22-3305
Reis, Silva, Silva, Thabane, Milagres et al., Effect of Early Treatment with Ivermectin among Patients with COVID-19, N. Engl. J. Med, doi:10.1056/NEJMoa2115869
Schloer, Brunotte, Goretzko, Mecate-Zambrano, Korthals et al., Targeting the endolysosomal host-SARS-CoV-2 interface by clinically licensed functional inhibitors of acid sphingomyelinase (FIASMA) including the antidepressant fluoxetine, Emerg. Microbes Infect, doi:10.1080/22221751.2020.1829082
Seftel, Boulware, Prospective Cohort of Fluvoxamine for Early Treatment of Coronavirus Disease 19, Open Forum. Infect. Dis, doi:10.1093/ofid/ofab050
Stamm, Partheymüller, Mosor, Ritschl, Kritzinger et al., Determinants of COVID-19 vaccine fatigue, Nat. Med, doi:10.1038/s41591-023-02282-y
Thümmler, Gäckler, Bormann, Ciesek, Widera et al., Cellular and Humoral Immunity against Different SARS-CoV-2 Variants Is Detectable but Reduced in Vaccinated Kidney Transplant Patients, Vaccines, doi:10.3390/vaccines10081348
Tseng, Hsu, Ling, Lu, Lin et al., Antidepressant Sertraline Is a Broad-Spectrum Inhibitor of Enteroviruses Targeting Viral Entry through Neutralization of Endolysosomal Acidification, Viruses, doi:10.3390/v14010109
Törnquist, Asghar, Srinivasan, Korhonen, Lindholm, Sphingolipids as Modulators of SARS-CoV-2 Infection, Front. Cell Dev. Biol, doi:10.3389/fcell.2021.689854
Wang, Wei, Hung, Jiang, Li et al., Relationship between antidepressants and severity of SARS-CoV-2 Omicron infection: A retrospective cohort study using real-world data, Lancet Reg. Health West. Pac, doi:10.1016/j.lanwpc.2023.100716
Who, None
Widera, Wilhelm, Toptan, Raffel, Kowarz et al., Generation of a Sleeping Beauty Transposon-Based Cellular System for Rapid and Sensitive Screening for Compounds and Cellular Factors Limiting SARS-CoV-2 Replication, Front. Microbiol, doi:10.3389/fmicb.2021.701198
Worldometers, None
Zettl, Meister, Vollmer, Fischer, Steinmann et al., Rapid Quantification of SARS-CoV-2-Neutralizing Antibodies Using Propagation-Defective Vesicular Stomatitis Virus Pseudotypes, Vaccines, doi:10.3390/vaccines8030386
Zimniak, Kirschner, Hilpert, Geiger, Danov et al., The serotonin reuptake inhibitor Fluoxetine inhibits SARS-CoV-2 in human lung tissue, Sci. Rep, doi:10.1038/s41598-021-85049-0
Zuo, Quinn, Kye, Cooper, Damoiseaux et al., Fluoxetine Is a Potent Inhibitor of Coxsackievirus Replication, Antimicrob. Agents Chemother, doi:10.1128/AAC.00983-12
DOI record:
{
"DOI": "10.3390/v16040545",
"ISSN": [
"1999-4915"
],
"URL": "http://dx.doi.org/10.3390/v16040545",
"abstract": "<jats:p>The pandemic caused by SARS-CoV-2 is still a major health problem. Newly emerging variants and long-COVID-19 represent a challenge for the global health system. In particular, individuals in developing countries with insufficient health care need easily accessible, affordable and effective treatments of COVID-19. Previous studies have demonstrated the efficacy of functional inhibitors of acid sphingomyelinase against infections with various viruses, including early variants of SARS-CoV-2. This work investigated whether the acid sphingomyelinase inhibitors fluoxetine and sertraline, usually used as antidepressant molecules in clinical practice, can inhibit the replication of the former and recently emerged SARS-CoV-2 variants in vitro. Fluoxetine and sertraline potently inhibited the infection with pseudotyped virus-like particles and SARS-CoV-2 variants D614G, alpha, delta, omicron BA.1 and omicron BA.5. These results highlight fluoxetine and sertraline as priority candidates for large-scale phase 3 clinical trials at different stages of SARS-CoV-2 infections, either alone or in combination with other medications.</jats:p>",
"alternative-id": [
"v16040545"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-2034-6255",
"affiliation": [
{
"name": "Department of Infectious Diseases, West German Centre of Infectious Diseases, University Medicine Essen, University Hospital Essen, University Duisburg-Essen, 45147 Essen, Germany"
},
{
"name": "Institute for Transfusion Medicine, University Hospital Essen, University Duisburg-Essen, 45147 Essen, Germany"
}
],
"authenticated-orcid": false,
"family": "Thümmler",
"given": "Laura",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Institute of Molecular Biology, University Hospital Essen, University of Duisburg-Essen, 45147 Essen, Germany"
}
],
"family": "Beckmann",
"given": "Nadine",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Institute of Molecular Biology, University Hospital Essen, University of Duisburg-Essen, 45147 Essen, Germany"
}
],
"family": "Sehl",
"given": "Carolin",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Institute of Molecular Biology, University Hospital Essen, University of Duisburg-Essen, 45147 Essen, Germany"
}
],
"family": "Soddemann",
"given": "Matthias",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3169-9515",
"affiliation": [
{
"name": "Department of Infectious Diseases, West German Centre of Infectious Diseases, University Medicine Essen, University Hospital Essen, University Duisburg-Essen, 45147 Essen, Germany"
}
],
"authenticated-orcid": false,
"family": "Braß",
"given": "Peer",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0955-1453",
"affiliation": [
{
"name": "Department of Infectious Diseases, West German Centre of Infectious Diseases, University Medicine Essen, University Hospital Essen, University Duisburg-Essen, 45147 Essen, Germany"
}
],
"authenticated-orcid": false,
"family": "Bormann",
"given": "Maren",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Infectious Diseases, West German Centre of Infectious Diseases, University Medicine Essen, University Hospital Essen, University Duisburg-Essen, 45147 Essen, Germany"
}
],
"family": "Brochhagen",
"given": "Leonie",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Institute for Virology, University Hospital Essen, University Duisburg-Essen, 45147 Essen, Germany"
}
],
"family": "Elsner",
"given": "Carina",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Institute Psychiatry and Neuroscience de Paris, INSERM U1266, Paris Cité University, 75014 Paris, France"
},
{
"name": "Psychiatry and Addiction Department Corentin-Celton Hospital (AP-HP), 92130 Paris, France"
}
],
"family": "Hoertel",
"given": "Nicolas",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6795-5448",
"affiliation": [
{
"name": "Institute of Pharmacology and Structural Biology (IPBS), CNRS, University of Toulouse, UPS, 31000 Toulouse, France"
}
],
"authenticated-orcid": false,
"family": "Cougoule",
"given": "Céline",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Institute of Medical Virology, University Hospital Frankfurt, 60590 Frankfurt am Main, Germany"
},
{
"name": "Institute of Pharmaceutical Biology, Goethe-University, 60323 Frankfurt am Main, Germany"
},
{
"name": "Fraunhofer Institute for Molecular Biology and Applied Ecology (IME), Branch Translational Medicine and Pharmacology, 60311 Frankfurt am Main, Germany"
}
],
"family": "Ciesek",
"given": "Sandra",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Institute of Medical Virology, University Hospital Frankfurt, 60590 Frankfurt am Main, Germany"
}
],
"family": "Widera",
"given": "Marek",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Institute for Virology, University Hospital Essen, University Duisburg-Essen, 45147 Essen, Germany"
}
],
"family": "Dittmer",
"given": "Ulf",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6708-4390",
"affiliation": [
{
"name": "Institute for Transfusion Medicine, University Hospital Essen, University Duisburg-Essen, 45147 Essen, Germany"
}
],
"authenticated-orcid": false,
"family": "Lindemann",
"given": "Monika",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Institute for Transfusion Medicine, University Hospital Essen, University Duisburg-Essen, 45147 Essen, Germany"
}
],
"family": "Horn",
"given": "Peter A.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Infectious Diseases, West German Centre of Infectious Diseases, University Medicine Essen, University Hospital Essen, University Duisburg-Essen, 45147 Essen, Germany"
}
],
"family": "Witzke",
"given": "Oliver",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6430-1230",
"affiliation": [
{
"name": "Institute of Molecular Biology, University Hospital Essen, University of Duisburg-Essen, 45147 Essen, Germany"
}
],
"authenticated-orcid": false,
"family": "Kadow",
"given": "Stephanie",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6608-8496",
"affiliation": [
{
"name": "Department of Thoracic and Cardiovascular Surgery, West German Heart Center, University Hospital Essen, 45147 Essen, Germany"
}
],
"authenticated-orcid": false,
"family": "Kamler",
"given": "Markus",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Institute of Molecular Biology, University Hospital Essen, University of Duisburg-Essen, 45147 Essen, Germany"
}
],
"family": "Gulbins",
"given": "Erich",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6317-7298",
"affiliation": [
{
"name": "Institute of Molecular Biology, University Hospital Essen, University of Duisburg-Essen, 45147 Essen, Germany"
}
],
"authenticated-orcid": false,
"family": "Becker",
"given": "Katrin Anne",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9502-9903",
"affiliation": [
{
"name": "Department of Infectious Diseases, West German Centre of Infectious Diseases, University Medicine Essen, University Hospital Essen, University Duisburg-Essen, 45147 Essen, Germany"
},
{
"name": "Institute for Virology, University Hospital Essen, University Duisburg-Essen, 45147 Essen, Germany"
}
],
"authenticated-orcid": false,
"family": "Krawczyk",
"given": "Adalbert",
"sequence": "additional"
}
],
"container-title": "Viruses",
"container-title-short": "Viruses",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
3,
31
]
],
"date-time": "2024-03-31T17:44:52Z",
"timestamp": 1711907092000
},
"deposited": {
"date-parts": [
[
2024,
4,
2
]
],
"date-time": "2024-04-02T04:37:42Z",
"timestamp": 1712032662000
},
"indexed": {
"date-parts": [
[
2024,
4,
3
]
],
"date-time": "2024-04-03T01:25:35Z",
"timestamp": 1712107535605
},
"is-referenced-by-count": 0,
"issue": "4",
"issued": {
"date-parts": [
[
2024,
3,
30
]
]
},
"journal-issue": {
"issue": "4",
"published-online": {
"date-parts": [
[
2024,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
3,
30
]
],
"date-time": "2024-03-30T00:00:00Z",
"timestamp": 1711756800000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/1999-4915/16/4/545/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "545",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2024,
3,
30
]
]
},
"published-online": {
"date-parts": [
[
2024,
3,
30
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"key": "ref_1",
"unstructured": "(2024, January 08). Worldometers. Available online: https://www.worldometers.info/coronavirus/."
},
{
"DOI": "10.3390/ijerph19010610",
"doi-asserted-by": "crossref",
"key": "ref_2",
"unstructured": "Panneer, S., Kantamaneni, K., Akkayasamy, V.S., Susairaj, A.X., Panda, P.K., Acharya, S.S., Rice, L., Liyanage, C., and Pushparaj, R.R.B. (2022). The Great Lockdown in the Wake of COVID-19 and Its Implications: Lessons for Low and Middle-Income Countries. Int. J. Environ. Res. Public Health, 19."
},
{
"DOI": "10.1038/s41591-023-02282-y",
"article-title": "Determinants of COVID-19 vaccine fatigue",
"author": "Stamm",
"doi-asserted-by": "crossref",
"first-page": "1164",
"journal-title": "Nat. Med.",
"key": "ref_3",
"volume": "29",
"year": "2023"
},
{
"DOI": "10.3389/fimmu.2023.1150667",
"article-title": "Immune responses in COVID-19 patients during breakthrough infection with SARS-CoV-2 variants Delta, Omicron-BA.1 and Omicron-BA.5",
"author": "Bormann",
"doi-asserted-by": "crossref",
"first-page": "1150667",
"journal-title": "Front. Immunol.",
"key": "ref_4",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.1056/NEJMoa2109072",
"article-title": "Covid-19 Breakthrough Infections in Vaccinated Health Care Workers",
"author": "Bergwerk",
"doi-asserted-by": "crossref",
"first-page": "1474",
"journal-title": "N. Engl. J. Med.",
"key": "ref_5",
"volume": "385",
"year": "2021"
},
{
"DOI": "10.1007/s44197-023-00090-8",
"article-title": "COVID-19 Breakthrough Infection Among Vaccinated Population in the United Arab Emirates",
"author": "Dash",
"doi-asserted-by": "crossref",
"first-page": "67",
"journal-title": "J. Epidemiol. Glob. Health",
"key": "ref_6",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1128/jvi.01245-22",
"article-title": "Sertraline Is an Effective SARS-CoV-2 Entry Inhibitor Targeting the Spike Protein",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "e01245-22",
"journal-title": "J. Virol.",
"key": "ref_7",
"volume": "96",
"year": "2022"
},
{
"DOI": "10.1016/j.antiviral.2020.104781",
"article-title": "Synthesis and antiviral effect of novel fluoxetine analogues as enterovirus 2C inhibitors",
"author": "Manganaro",
"doi-asserted-by": "crossref",
"first-page": "104781",
"journal-title": "Antivir. Res.",
"key": "ref_8",
"volume": "178",
"year": "2020"
},
{
"DOI": "10.1212/WNL.0000000000006670",
"article-title": "Safety, tolerability, and efficacy of fluoxetine as an antiviral for acute flaccid myelitis",
"author": "Messacar",
"doi-asserted-by": "crossref",
"first-page": "E2118",
"journal-title": "Neurology",
"key": "ref_9",
"volume": "92",
"year": "2019"
},
{
"DOI": "10.3390/v14010109",
"doi-asserted-by": "crossref",
"key": "ref_10",
"unstructured": "Tseng, K.C., Hsu, B.Y., Ling, P., Lu, W.W., Lin, C.W., and Kung, S.H. (2022). Antidepressant Sertraline Is a Broad-Spectrum Inhibitor of Enteroviruses Targeting Viral Entry through Neutralization of Endolysosomal Acidification. Viruses, 14."
},
{
"DOI": "10.1128/AAC.00983-12",
"article-title": "Fluoxetine Is a Potent Inhibitor of Coxsackievirus Replication",
"author": "Zuo",
"doi-asserted-by": "crossref",
"first-page": "4838",
"journal-title": "Antimicrob. Agents Chemother.",
"key": "ref_11",
"volume": "56",
"year": "2012"
},
{
"DOI": "10.3851/IMP1898",
"article-title": "Open-label Phase 1b pilot study to assess the antiviral efficacy of simvastatin combined with sertraline in chronic hepatitis C patients",
"author": "Patel",
"doi-asserted-by": "crossref",
"first-page": "1341",
"journal-title": "Antivir. Ther.",
"key": "ref_12",
"volume": "16",
"year": "2011"
},
{
"DOI": "10.1128/AAC.01146-20",
"article-title": "Inhibition of Arenaviruses by Combinations of Orally Available Approved Drugs",
"author": "Herring",
"doi-asserted-by": "crossref",
"first-page": "e01146-20",
"journal-title": "Antimicrob. Agents Chemother.",
"key": "ref_13",
"volume": "65",
"year": "2021"
},
{
"DOI": "10.1007/BF00500076",
"article-title": "Lipid and lysosomal enzymes in human fibroblasts cultured with perhexiline maleate",
"author": "Albouz",
"doi-asserted-by": "crossref",
"first-page": "173",
"journal-title": "Naunyn-Schmiedebergs Arch. Pharmacol.",
"key": "ref_14",
"volume": "317",
"year": "1981"
},
{
"DOI": "10.1515/bchm3.1994.375.7.447",
"article-title": "The Tricyclic Antidepressant Desipramine Causes Proteolytic Degradation of Lysosomal Sphingomyelinase in Human Fibroblasts",
"author": "Hurwitz",
"doi-asserted-by": "crossref",
"first-page": "447",
"journal-title": "Biol. Chem. Hoppe-Seyler",
"key": "ref_15",
"volume": "375",
"year": "1994"
},
{
"DOI": "10.1159/000315101",
"article-title": "Functional Inhibitors of Acid Sphingomyelinase (FIASMAs): A novel pharmacological group of drugs with broad clinical applications",
"author": "Kornhuber",
"doi-asserted-by": "crossref",
"first-page": "9",
"journal-title": "Cell Physiol. Biochem.",
"key": "ref_16",
"volume": "26",
"year": "2010"
},
{
"DOI": "10.1038/s41598-021-85049-0",
"article-title": "The serotonin reuptake inhibitor Fluoxetine inhibits SARS-CoV-2 in human lung tissue",
"author": "Zimniak",
"doi-asserted-by": "crossref",
"first-page": "5890",
"journal-title": "Sci. Rep.",
"key": "ref_17",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1038/s41598-022-17082-6",
"article-title": "Robust antiviral activity of commonly prescribed antidepressants against emerging coronaviruses: In vitro and in silico drug repurposing studies",
"author": "Kutkat",
"doi-asserted-by": "crossref",
"first-page": "12920",
"journal-title": "Sci. Rep.",
"key": "ref_18",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.3390/ijms232113623",
"doi-asserted-by": "crossref",
"key": "ref_19",
"unstructured": "Péricat, D., Leon-Icaza, S.A., Sanchez Rico, M., Mühle, C., Zoicas, I., Schumacher, F., Planès, R., Mazars, R., Gros, G., and Carpinteiro, A. (2022). Antiviral and Anti-Inflammatory Activities of Fluoxetine in a SARS-CoV-2 Infection Mouse Model. Int. J. Mol. Sci., 23."
},
{
"DOI": "10.1001/jama.2020.22760",
"article-title": "Fluvoxamine vs Placebo and Clinical Deterioration in Outpatients with Symptomatic COVID-19: A Randomized Clinical Trial",
"author": "Lenze",
"doi-asserted-by": "crossref",
"first-page": "2292",
"journal-title": "JAMA",
"key": "ref_20",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1111/bcp.15126",
"article-title": "Safety and efficacy of fluvoxamine in COVID-19 ICU patients: An open label, prospective cohort trial with matched controls",
"author": "Calusic",
"doi-asserted-by": "crossref",
"first-page": "2065",
"journal-title": "Br. J. Clin. Pharmacol.",
"key": "ref_21",
"volume": "88",
"year": "2022"
},
{
"DOI": "10.1093/ofid/ofab050",
"article-title": "Prospective Cohort of Fluvoxamine for Early Treatment of Coronavirus Disease 19",
"author": "Seftel",
"doi-asserted-by": "crossref",
"first-page": "ofab050",
"journal-title": "Open Forum. Infect. Dis.",
"key": "ref_22",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2115869",
"article-title": "Effect of Early Treatment with Ivermectin among Patients with COVID-19",
"author": "Reis",
"doi-asserted-by": "crossref",
"first-page": "1721",
"journal-title": "N. Engl. J. Med.",
"key": "ref_23",
"volume": "386",
"year": "2022"
},
{
"DOI": "10.1016/j.xcrm.2020.100142",
"article-title": "Pharmacological Inhibition of Acid Sphingomyelinase Prevents Uptake of SARS-CoV-2 by Epithelial Cells",
"author": "Carpinteiro",
"doi-asserted-by": "crossref",
"first-page": "100142",
"journal-title": "Cell Rep. Med.",
"key": "ref_24",
"volume": "1",
"year": "2020"
},
{
"DOI": "10.1016/j.jbc.2021.100701",
"doi-asserted-by": "crossref",
"key": "ref_25",
"unstructured": "Carpinteiro, A., Gripp, B., Hoffmann, M., Pöhlmann, S., Hoertel, N., Edwards, M.J., Kamler, M., Kornhuber, J., Becker, K.A., and Gulbins, E. (2021). Inhibition of acid sphingomyelinase by ambroxol prevents SARS-CoV-2 entry into epithelial cells. J. Biol. Chem., 296."
},
{
"DOI": "10.1001/jamanetworkopen.2021.36510",
"article-title": "Do the Selective Serotonin Reuptake Inhibitor Antidepressants Fluoxetine and Fluvoxamine Reduce Mortality among Patients with COVID-19?",
"author": "Hoertel",
"doi-asserted-by": "crossref",
"first-page": "e2136510",
"journal-title": "JAMA Netw. Open",
"key": "ref_26",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1038/s41380-021-01254-3",
"article-title": "Repurposing antidepressants inhibiting the sphingomyelinase acid/ceramide system against COVID-19: Current evidence and potential mechanisms",
"author": "Hoertel",
"doi-asserted-by": "crossref",
"first-page": "7098",
"journal-title": "Mol. Psychiatry",
"key": "ref_27",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.3389/fmicb.2021.701198",
"doi-asserted-by": "crossref",
"key": "ref_28",
"unstructured": "Widera, M., Wilhelm, A., Toptan, T., Raffel, J.M., Kowarz, E., Roesmann, F., Grozinger, F., Siemund, A.L., Luciano, V., and Kulp, M. (2021). Generation of a Sleeping Beauty Transposon-Based Cellular System for Rapid and Sensitive Screening for Compounds and Cellular Factors Limiting SARS-CoV-2 Replication. Front. Microbiol., 12."
},
{
"DOI": "10.3390/vaccines10081348",
"doi-asserted-by": "crossref",
"key": "ref_29",
"unstructured": "Thümmler, L., Gäckler, A., Bormann, M., Ciesek, S., Widera, M., Rohn, H., Fisenkci, N., Otte, M., Alt, M., and Dittmer, U. (2022). Cellular and Humoral Immunity against Different SARS-CoV-2 Variants Is Detectable but Reduced in Vaccinated Kidney Transplant Patients. Vaccines, 10."
},
{
"key": "ref_30",
"unstructured": "(2024, January 09). WHO. Available online: https://www.who.int/activities/tracking-SARS-CoV-2-variants."
},
{
"DOI": "10.1016/j.ajic.2020.07.031",
"article-title": "Susceptibility of SARS-CoV-2 to UV irradiation",
"author": "Heilingloh",
"doi-asserted-by": "crossref",
"first-page": "1273",
"journal-title": "Am. J. Infect. Control",
"key": "ref_31",
"volume": "48",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2020.02.052",
"article-title": "SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor",
"author": "Hoffmann",
"doi-asserted-by": "crossref",
"first-page": "271",
"journal-title": "Cell",
"key": "ref_32",
"volume": "181",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0025858",
"doi-asserted-by": "crossref",
"key": "ref_33",
"unstructured": "Berger Rentsch, M., and Zimmer, G. (2011). A vesicular stomatitis virus replicon-based bioassay for the rapid and sensitive determination of multi-species type I interferon. PLoS ONE, 6."
},
{
"DOI": "10.1016/j.xpro.2021.100356",
"article-title": "Ex vivo assay to evaluate the efficacy of drugs targeting sphingolipids in preventing SARS-CoV-2 infection of nasal epithelial cells",
"author": "Becker",
"doi-asserted-by": "crossref",
"first-page": "100356",
"journal-title": "STAR Protoc.",
"key": "ref_34",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.3390/vaccines8030386",
"doi-asserted-by": "crossref",
"key": "ref_35",
"unstructured": "Zettl, F., Meister, T.L., Vollmer, T., Fischer, B., Steinmann, J., Krawczyk, A., V’kovski, P., Todt, D., Steinmann, E., and Pfaender, S. (2020). Rapid Quantification of SARS-CoV-2-Neutralizing Antibodies Using Propagation-Defective Vesicular Stomatitis Virus Pseudotypes. Vaccines, 8."
},
{
"DOI": "10.1016/j.celrep.2021.109415",
"article-title": "SARS-CoV-2 variant B.1.617 is resistant to bamlanivimab and evades antibodies induced by infection and vaccination",
"author": "Hoffmann",
"doi-asserted-by": "crossref",
"first-page": "109415",
"journal-title": "Cell Rep.",
"key": "ref_36",
"volume": "36",
"year": "2021"
},
{
"DOI": "10.3389/fphar.2021.755600",
"article-title": "Antidepressant and Antipsychotic Drugs Reduce Viral Infection by SARS-CoV-2 and Fluoxetine Shows Antiviral Activity Against the Novel Variants in vitro",
"author": "Fred",
"doi-asserted-by": "crossref",
"first-page": "755600",
"journal-title": "Front. Pharmacol.",
"key": "ref_37",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.3390/cells11162532",
"doi-asserted-by": "crossref",
"key": "ref_38",
"unstructured": "Geiger, N., Kersting, L., Schlegel, J., Stelz, L., Fähr, S., Diesendorf, V., Roll, V., Sostmann, M., König, E.-M., and Reinhard, S. (2022). The Acid Ceramidase Is a SARS-CoV-2 Host Factor. Cells, 11."
},
{
"DOI": "10.1080/22221751.2020.1829082",
"article-title": "Targeting the endolysosomal host-SARS-CoV-2 interface by clinically licensed functional inhibitors of acid sphingomyelinase (FIASMA) including the antidepressant fluoxetine",
"author": "Schloer",
"doi-asserted-by": "crossref",
"first-page": "2245",
"journal-title": "Emerg. Microbes Infect.",
"key": "ref_39",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1038/s41380-021-01309-5",
"article-title": "The acid sphingomyelinase/ceramide system in COVID-19",
"author": "Kornhuber",
"doi-asserted-by": "crossref",
"first-page": "307",
"journal-title": "Mol. Psychiatry",
"key": "ref_40",
"volume": "27",
"year": "2022"
},
{
"DOI": "10.3389/fcell.2021.689854",
"doi-asserted-by": "crossref",
"key": "ref_41",
"unstructured": "Törnquist, K., Asghar, M.Y., Srinivasan, V., Korhonen, L., and Lindholm, D. (2021). Sphingolipids as Modulators of SARS-CoV-2 Infection. Front. Cell Dev. Biol., 9."
},
{
"DOI": "10.3390/ijms22115676",
"doi-asserted-by": "crossref",
"key": "ref_42",
"unstructured": "Beckmann, N., and Becker, K.A. (2021). Ceramide and Related Molecules in Viral Infections. Int. J. Mol. Sci., 22."
},
{
"DOI": "10.1038/s41380-021-01432-3",
"article-title": "Mechanisms of action of fluvoxamine for COVID-19: A historical review",
"author": "Hashimoto",
"doi-asserted-by": "crossref",
"first-page": "1898",
"journal-title": "Mol. Psychiatry",
"key": "ref_43",
"volume": "27",
"year": "2022"
},
{
"DOI": "10.1074/jbc.M500835200",
"article-title": "Rhinoviruses infect human epithelial cells via ceramide-enriched membrane platforms",
"author": "Grassme",
"doi-asserted-by": "crossref",
"first-page": "26256",
"journal-title": "J. Biol. Chem.",
"key": "ref_44",
"volume": "280",
"year": "2005"
},
{
"DOI": "10.1128/JVI.00136-12",
"article-title": "Ebolavirus requires acid sphingomyelinase activity and plasma membrane sphingomyelin for infection",
"author": "Miller",
"doi-asserted-by": "crossref",
"first-page": "7473",
"journal-title": "J. Virol.",
"key": "ref_45",
"volume": "86",
"year": "2012"
},
{
"DOI": "10.3390/ph16081107",
"doi-asserted-by": "crossref",
"key": "ref_46",
"unstructured": "Hoertel, N., Rezaei, K., Sánchez-Rico, M., Delgado-Álvarez, A., Kornhuber, J., Gulbins, E., Olfson, M., Ouazana-Vedrines, C., Carpinteiro, A., and Cougoule, C. (2023). Medications Modulating the Acid Sphingomyelinase/Ceramide System and 28-Day Mortality among Patients with SARS-CoV-2: An Observational Study. Pharmaceuticals, 16."
},
{
"DOI": "10.7326/M22-3305",
"article-title": "Oral Fluvoxamine with Inhaled Budesonide for Treatment of Early-Onset COVID-19: A Randomized Platform Trial",
"author": "Reis",
"doi-asserted-by": "crossref",
"first-page": "667",
"journal-title": "Ann. Intern. Med.",
"key": "ref_47",
"volume": "176",
"year": "2023"
},
{
"DOI": "10.1016/j.lanwpc.2023.100716",
"article-title": "Relationship between antidepressants and severity of SARS-CoV-2 Omicron infection: A retrospective cohort study using real-world data",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "100716",
"journal-title": "Lancet Reg. Health West. Pac.",
"key": "ref_48",
"volume": "34",
"year": "2023"
},
{
"DOI": "10.1101/2024.01.16.24301337",
"doi-asserted-by": "crossref",
"key": "ref_49",
"unstructured": "Jittamala, P., Boyd, S., Schilling, W.H., Watson, J.A., Ngamprasertchai, T., Siripoon, T., Luvira, V., Batty, E.M., Wongnak, P., and Esper, L.M. (2024). Antiviral efficacy of fluoxetine in early symptomatic COVID-19: An open-label, randomised, controlled, adaptive platform trial (PLATCOV). medRxiv."
},
{
"DOI": "10.1016/S2214-109X(21)00448-4",
"article-title": "Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with COVID-19: The TOGETHER randomised, platform clinical trial",
"author": "Reis",
"doi-asserted-by": "crossref",
"first-page": "e42",
"journal-title": "Lancet Glob. Health",
"key": "ref_50",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1001/jamanetworkopen.2021.33090",
"article-title": "Mortality Risk Among Patients with COVID-19 Prescribed Selective Serotonin Reuptake Inhibitor Antidepressants",
"author": "Oskotsky",
"doi-asserted-by": "crossref",
"first-page": "e2133090",
"journal-title": "JAMA Netw Open",
"key": "ref_51",
"volume": "4",
"year": "2021"
}
],
"reference-count": 51,
"references-count": 51,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/1999-4915/16/4/545"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Virology",
"Infectious Diseases"
],
"subtitle": [],
"title": "Fluoxetine and Sertraline Potently Neutralize the Replication of Distinct SARS-CoV-2 Variants",
"type": "journal-article",
"volume": "16"
}
