Role of probiotics in managing various human diseases, from oral pathology to cancer and gastrointestinal diseases
et al., Frontiers in Microbiology, doi:10.3389/fmicb.2023.1296447, Jan 2024
Probiotics for COVID-19
20th treatment shown to reduce risk in
March 2021, now with p = 0.00000044 from 29 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
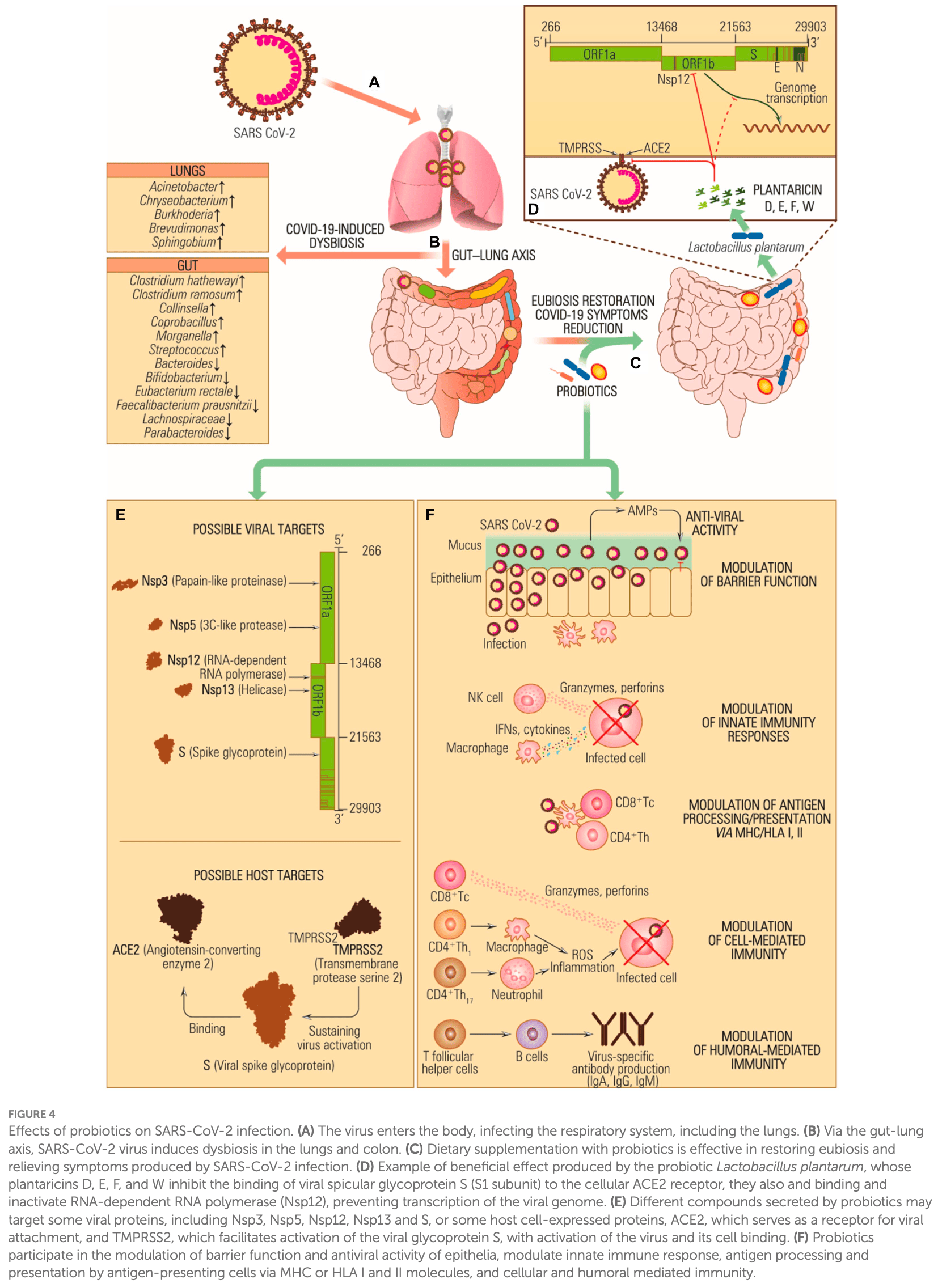
Review of the role of probiotics in managing various human diseases including potential benefits for COVID-19. Probiotics may help restore equilibrium in the gut microbiota disrupted by COVID-19. Probiotic consumption can reduce viral loads and enhance immune responses. The lung-gut axis, mediated by probiotics, might play a role in managing the disease. Meta-analyses suggest probiotics can positively impact symptoms, restore intestinal microbiota equilibrium, decrease diarrhea duration, and reduce hospitalization length. The multifactorial mechanism of action of beneficial bacteria through immunomodulatory properties, such as interferon production and cytokine storm inhibition, highlights the potential of probiotics in COVID-19 therapy.
Probiotic efficacy depends on the specific strains used. Specific microbes may decrease or increase COVID-19 risk1.
1.
Li et al., Large-scale genetic correlation studies explore the causal relationship and potential mechanism between gut microbiota and COVID-19-associated risks, BMC Microbiology, doi:10.1186/s12866-024-03423-0.
2.
Chau et al., Effectiveness of probiotics on COVID-19 prevention and treatment against mild COVID-19 in outpatient care: A systematic review, Nutrition and Health, doi:10.1177/02601060251378200.
3.
Bajić et al., Immunity's core reset: Synbiotics and gut microbiota in the COVID-19 era, Innate Immunity, doi:10.1177/17534259251362023.
4.
Bigman et al., A Comprehensive Scoping Review on Diet and Nutrition in Relation to Long COVID-19 Symptoms and Recovery, Nutrients, doi:10.3390/nu17111802.
5.
Fazli et al., Possible Link between Gut Microbiota, Diet, and COVID-19 Infection, Journal of Medical Bacteriology, 12:4, jmb.tums.ac.ir/index.php/jmb/article/view/525.
6.
Santa et al., Comparative analysis of COVID-19 responses in Japan and Africa: diet, phytochemicals, vitamin D, and gut microbiota in reducing mortality—A systematic review and meta-analysis, Frontiers in Nutrition, doi:10.3389/fnut.2024.1465324.
7.
Kaushal, A., Nutraceuticals and pharmacological to balance the transitional microbiome to extend immunity during COVID-19 and other viral infections, Journal of Translational Medicine, doi:10.1186/s12967-024-05587-9.
8.
Mu et al., Anti-inflammatory and Nutritional Interventions Against SARS-CoV-2: A Comprehensive Review, Journal of Agriculture and Food Research, doi:10.1016/j.jafr.2024.101422.
9.
Taufer et al., Lactobacilli in COVID-19: A Systematic Review Based on Next-Generation Sequencing Studies, Microorganisms, doi:10.3390/microorganisms12020284.
10.
Righi et al., Gut Microbiome Disruption Following SARS-CoV-2: A Review, Microorganisms, doi:10.3390/microorganisms12010131.
11.
Petrariu et al., Role of probiotics in managing various human diseases, from oral pathology to cancer and gastrointestinal diseases, Frontiers in Microbiology, doi:10.3389/fmicb.2023.1296447.
12.
Taufer (B) et al., The Role of Bifidobacterium in COVID-19: A Systematic Review, Life, doi:10.3390/life13091847.
13.
Di Pierro, F., A possible probiotic (S. salivarius K12) approach to improve oral and lung microbiotas and raise defenses against SARS-CoV-2, Minerva Medica, doi:10.23736/S0026-4806.20.06570-2.
14.
Kurian et al., Probiotics in Prevention and Treatment of COVID-19: Current Perspective and Future Prospects, Archives of Medical Research, doi:10.1016/j.arcmed.2021.03.002.
15.
Singh et al., Probiotics: A potential immunomodulator in COVID-19 infection management, Nutrition Research, doi:10.1016/j.nutres.2020.12.014.
16.
Stavropoulou et al., Probiotics as a Weapon in the Fight Against COVID-19, Frontiers in Nutrition, doi:10.3389/fnut.2020.614986.
Petrariu et al., 5 Jan 2024, peer-reviewed, 8 authors.
Contact: grigore.georgiana-alexandra@s.bio.unibuc.ro.
Role of probiotics in managing various human diseases, from oral pathology to cancer and gastrointestinal diseases
Frontiers in Microbiology, doi:10.3389/fmicb.2023.1296447
The imbalance of microbial composition and diversity in favor of pathogenic microorganisms combined with a loss of beneficial gut microbiota taxa results from factors such as age, diet, antimicrobial administration for different infections, other underlying medical conditions, etc. Probiotics are known for their capacity to improve health by stimulating the indigenous gut microbiota, enhancing host immunity resistance to infection, helping digestion, and carrying out various other functions. Concurrently, the metabolites produced by these microorganisms, termed postbiotics, which include compounds like bacteriocins, lactic acid, and hydrogen peroxide, contribute to inhibiting a wide range of pathogenic bacteria. This review presents an update on using probiotics in managing and treating various human diseases, including complications that may emerge during or after a COVID-19 infection.
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abikshyeet, Mishra, Bhuyan, Kumar, Mahapatra et al., Probiotics: dawn of a new era in dental caries management, J. Pharm. Bioallied Sci, doi:10.4103/jpbs.jpbs_801_21
Abruzzo, Vitali, Lombardi, Guerrini, Cinque et al., Mucoadhesive buccal films for local delivery of Lactobacillus brevis, Pharmaceutics, doi:10.3390/pharmaceutics12030241
Adiki, Perla, Saha, Katakam, Theendra, Enhancement in iron absorption on intake of chemometrically optimized ratio of probiotic strain Lactobacillus plantarum 299v with iron supplement pearl millet, Biol. Trace Elem. Res, doi:10.1007/s12011-018-1541-5
Aghamohammad, Sepehr, Miri, Najafi, Pourshafie et al., Anti-inflammatory and immunomodulatory effects of Lactobacillus spp. as a preservative and therapeutic agent for IBD control, Immun Inflamm Dis, doi:10.1002/iid3.635
Agossa, Dubar, Lemaire, Blaizot, Catteau et al., Effect of Lactobacillus reuteri on gingival inflammation and composition of the oral microbiota in patients undergoing treatment with fixed orthodontic appliances: study protocol of a randomized control trial, Pathogens, doi:10.3390/pathogens11020112
Aguilera, Manzano, Pirela, Bermúdez, Probiotics and gut microbiota in obesity: myths and realities of a new health revolution, J Pers Med, doi:10.3390/jpm12081282
Ahlawat, Asha, Sharma, Immunological co-ordination between gut and lungs in SARS-CoV-2 infection, Virus Res, doi:10.1016/j.virusres.2020.198103
Ahn, Kim, Park, Han, Kim, Effects of probiotics administration on lactose intolerance in adulthood: a meta-analysis, J. Dairy Sci, doi:10.3168/jds.2022-22762
Ahn, Kim, Yang, An aqueous extract of a Bifidobacterium species induces apoptosis and inhibits invasiveness of non-small cell lung cancer cells, J. Microbiol. Biotechnol, doi:10.4014/jmb.1912.12054
Al-Badr, Al-Shaikh, Recurrent urinary tract infections management in women: a review, Sultan Qaboos Univ. Med. J, doi:10.12816/0003256
Al-Sadi, Nighot, Nighot, Haque, Rawat et al., Lactobacillus acidophilus induces a strain-specific and toll-like receptor 2-dependent enhancement of intestinal epithelial tight junction barrier and protection against intestinal inflammation, Am. J. Pathol, doi:10.1016/j.ajpath.2021.02.003
Aleman, Moncada, Aryana, Leaky gut and the ingredients that help treat it: a review, Molecules, doi:10.3390/molecules28020619
Alkaya, Laleman, Keceli, Ozcelik, Cenk Haytac et al., Clinical effects of probiotics containing Bacillus species on gingivitis: a pilot randomized controlled trial, J. Periodontal Res, doi:10.1111/jre.12415
Amaretti, Di Nunzio, Pompei, Raimondi, Rossi et al., Antioxidant properties of potentially probiotic bacteria: in vitro and in vivo activities, Appl. Microbiol. Biotechnol, doi:10.1007/s00253-012-4241-7
Amargianitakis, Antoniadou, Rahiotis, Varzakas, Probiotics, prebiotics, synbiotics and dental caries. New perspectives, suggestions, and patient coaching approach for a cavity-free mouth, Appl. Sci, doi:10.3390/app11125472
Andolfi, Bloodworth, Papachristos, Sweis, The urinary microbiome and bladder cancer: susceptibility and immune responsiveness, Bladder Cancer, doi:10.3233/BLC-200277
Andrews, Mclean, Durum, Cytokine tuning of intestinal epithelial function, Front. Immunol, doi:10.3389/fimmu.2018.01270
Ansari, Son, Hur, Park, You et al., Lactobacillus probiotics improve vaginal dysbiosis in asymptomatic women, Nutrients, doi:10.3390/nu15081862
Armstrong, Hemmerling, Miller, Burke, Newmann et al., Sustained effect of LACTIN-V (Lactobacillus crispatus CTV-05) on genital immunology following standard bacterial vaginosis treatment: results from a randomised, placebo-controlled trial, Lancet Microbe, doi:10.1016/S2666-5247(22)00043-X
Asgari, Falak, Teimourian, Pourakbari, Ebrahimnezhad et al., Effects of oral probiotic feeding on toll-like receptor gene expression of the chicken's cecal tonsil, Rep Biochem Mol Biol
Asoudeh-Fard, Barzegari, Dehnad, Bastani, Golchin et al., Lactobacillus plantarum induces apoptosis in oral cancer KB cells through upregulation of PTEN and downregulation of MAPK signalling pathways, Bioimpacts, doi:10.15171/bi.2017.22
Atanasova, Yilmaz, Looking in the Porphyromonas gingivalis cabinet of curiosities: the microbium, the host and cancer association, Mol Oral Microbiol, doi:10.1111/omi.12047
Awasthi, Corrie, Vishwas, Gulati, Kumar et al., Gut dysbiosis and diabetic foot ulcer: role of probiotics, Pharmaceutics, doi:10.3390/pharmaceutics14112543
Aysha Jebin, Suresh, Oral microbial shift induced by probiotic Bacillus coagualans along with its clinical perspectives, J Oral Biol Craniofac Res, doi:10.1016/j.jobcr.2023.03.013
Azad, Sarker, Immunomodulatory effects of probiotics on cytokine profiles, Biomed. Res. Int, doi:10.1155/2018/8063647
Bahaddad, Almalki, Alghamdi, Sohrab, Yasir et al., Bacillus species as direct-fed microbial antibiotic alternatives for monogastric production, Probiotics Antimicrob Proteins, doi:10.1007/s12602-022-09909-5
Bai, Zhu, He, Wang, Tian et al., The impacts of probiotics in eradication therapy of Helicobacter pylori, Arch. Microbiol, doi:10.1007/s00203-022-03314-w
Ballini, Santacroce, Cantore, Bottalico, Dipalma et al., Probiotics improve urogenital health in women, Open Access Maced J Med Sci, doi:10.3889/oamjms.2018.406
Bamola, Dubey, Samanta, Kedia, Ahuja et al., Role of a probiotic strain in the modulation of gut microbiota and cytokines in inflammatory bowel disease, Anaerobe, doi:10.1016/j.anaerobe.2022.102652
Banerjee, Somasundaram, Das, Jain Manoj, Banu et al., Functional foods: a promising strategy for restoring gut microbiota diversity impacted by SARS-CoV-2 variants, Nutrients, doi:10.3390/nu15112631
Banna, Torino, Marletta, Santagati, Salemi et al., Lactobacillus rhamnosus GG: an overview to explore the rationale of its use in cancer, Front. Pharmacol, doi:10.3389/fphar.2017.00603
Barbour, Smith, Oveisi, Williams, Huang et al., Discovery of phosphorylated lantibiotics with proimmune activity that regulate the oral microbiome, Proc. Natl. Acad. Sci. U. S. A, doi:10.1073/pnas.2219392120
Barrea, Verde, Auriemma, Vetrani, Cataldi et al., Probiotics and prebiotics: any role in menopause-related diseases?, Curr Nutr Rep, doi:10.1007/s13668-023-00462-3
Baumgardner, Oral fungal microbiota: to thrush and beyond, J Patient Cent Res Rev, doi:10.17294/2330-0698.1705
Beharry, Latkowska, Valencia, Allana, Soto et al., Factors influencing neonatal gut microbiome and health with a focus on necrotizing enterocolitis, Microorganisms, doi:10.3390/microorganisms11102528
Bhattacharya, Booy, Casadevall, Dela Cruz, Fedson et al., A practical treatment for COVID-19 and the next pandemic, Pharmacol. Res. Perspect, doi:10.1002/prp2.988
Bodke, Jogdand, Role of probiotics in human health, Cureus, doi:10.7759/cureus.31313
Brahma, Naik, Lordan, Probiotics: a gut response to the COVID-19 pandemic but what does the evidence show?, Clin Nutr ESPEN, doi:10.1016/j.clnesp.2022.08.023
Brown, Charity, Adriaenssens, Ecological and functional roles of bacteriophages in contrasting environments: marine, terrestrial and human gut, Curr. Opin. Microbiol, doi:10.1016/j.mib.2022.102229
Browne, Forster, Anonye, Kumar, Neville et al., Culturing of 'unculturable' human microbiota reveals novel taxa and extensive sporulation, Nature, doi:10.1038/nature17645
Bu, Liu, Liu, Wang, Liu et al., Screening and probiotic potential evaluation of bacteriocin-producing Lactiplantibacillus plantarum in vitro, Foods, doi:10.3390/foods11111575
Butera, Gallo, Maiorani, Molino, Chiesa et al., Probiotic alternative to chlorhexidine in periodontal therapy: evaluation of clinical and microbiological parameters, Microorganisms, doi:10.3390/microorganisms9010069
Cassir, Benamar, Scola, Clostridium butyricum: from beneficial to a new emerging pathogen, Clin. Microbiol. Infect, doi:10.1016/j.cmi.2015.10.014
Chaiyasut, Sivamaruthi, Lailerd, Sirilun, Khongtan et al., Probiotics supplementation improves intestinal permeability, obesity index and metabolic biomarkers in elderly Thai subjects: a randomized controlled trial, Foods, doi:10.3390/foods11030268
Chang, Jeong, Cheng, Choi, Shin et al., Quality characteristics of yogurts fermented with short-chain fatty acid-producing probiotics and their effects on mucin production and probiotic adhesion onto human colon epithelial cells, J. Dairy Sci, doi:10.3168/jds.2020-19820
Chang, Lin, Martel, Ojcius, Lai et al., Modulation of host immune response by Bacteroides fragilis polysaccharides: a review of recent observations, J. Biomed. Lab. Sci
Chang, Lin, Tsai, Wu, Lai et al., Next generation probiotics in disease amelioration, J. Food Drug Anal, doi:10.1016/j.jfda.2018.12.011
Chen, Chen, Wang, Zhou, Hong et al., Effect of probiotic supplementation on in-hospital mortality in patients with acute myocardial infarction: a study protocol for an open-label, randomized, controlled, superiority clinical trial, Trials, doi:10.1186/s13063-023-07443-5
Chen, Hu, Yuan, Yang, Ka, Effect of early enteral nutrition combined with probiotics in patients with stroke: a meta-analysis of randomized controlled trials, Eur. J. Clin. Nutr, doi:10.1038/s41430-021-00986-3
Cristofori, Dargenio, Dargenio, Miniello, Barone et al., Anti-inflammatory and immunomodulatory effects of probiotics in gut inflammation: a door to the body, Front. Immunol, doi:10.3389/fimmu.2021.578386
Daniali, Nikfar, Abdollahi, A brief overview on the use of probiotics to treat overweight and obese patients, Expert. Rev. Endocrinol. Metab, doi:10.1080/17446651.2020.1719068
Das, Pradhan, Chakrabarti, Mondal, Ghosh, Current status of probiotic and related health benefits, Applied. Food Research, doi:10.1016/j.afres.2022.100185
De Boeck, Cauwenberghs, Spacova, Gehrmann, Eilers et al., Randomized, double-blind, placebo-controlled trial of a throat spray with selected lactobacilli in COVID-19 outpatients, Microbiol. Spectr, doi:10.1128/spectrum.01682-22
De Melo Pereira, De Oliveira Coelho, Magalhães Júnior, Thomaz-Soccol, Soccol, How to select a probiotic? A review and update of methods and criteria, Biotechnol. Adv, doi:10.1016/j.biotechadv.2018.09.003
Deandra, Ketherin, Rachmasari, Sulijaya, Takahashi, Probiotics and metabolites regulate the oral and gut microbiome composition as host modulation agents in periodontitis: a narrative review, Heliyon, doi:10.1016/j.heliyon.2023.e13475
Dempsey, Corr, Lactobacillus spp. for gastrointestinal health: current and future perspectives, Front. Immunol, doi:10.3389/fimmu.2022.840245
Deng, Shang, Zhou, Li, Guo et al., Efficacy and safety of probiotics in geriatric patients with constipation: systematic review and meta-analysis, J. Nutr. Health Aging, doi:10.1007/s12603-023-2028-4
Desai, Prickril, Rasooly, Mechanisms of phytonutrient modulation of cyclooxygenase-2 (cox-2) and inflammation related to cancer, Nutr. Cancer, doi:10.1080/01635581.2018.1446091
Di Pierro, Colombo, Giuliani, Danza, Basile et al., Effect of administration of Streptococcus salivarius K12 on the occurrence of streptococcal pharyngo-tonsillitis, scarlet fever and acute otitis media in 3 years old children, Eur. Rev. Med. Pharmacol. Sci
Djaldetti, Bessler, Probiotic strains modulate cytokine production and the immune interplay between human peripheral blood mononucear cells and colon cancer cells, FEMS Microbiol. Lett, doi:10.1093/femsle/fnx014
Dong, Wu, Zhang, Chen, Zhang et al., Effect of probiotics intake on constipation in children: an umbrella review, Front. Nutr, doi:10.3389/fnut.2023.1218909
Dou, Shang, Qiao, Wang, Li, Clostridium butyricum protects IPEC-J2 cells from ETEC K88-induced oxidative damage by activating the Nrf2/ARE signaling pathway, Oxidative Med. Cell. Longev, doi:10.1155/2021/4464002
Duan, Yu, Tian, Zhai, Fan et al., Antibiotic-induced gut dysbiosis and barrier disruption and the potential protective strategies, Crit. Rev. Food Sci. Nutr, doi:10.1080/10408398.2020.1843396
Durant, Stentz, Noble, Brooks, Gicheva et al., Bacteroides thetaiotaomicron-derived outer membrane vesicles promote regulatory dendritic cell responses in health but not in inflammatory bowel disease, Microbiome, doi:10.1186/s40168-020-00868-z
Ehrlich, Pacheco, Henrick, Taft, Xu et al., Indole-3-lactic acid associated with Bifidobacterium-dominated microbiota significantly decreases inflammation in intestinal epithelial cells, BMC Microbiol, doi:10.1186/s12866-020-02023-y
Elias, Barna, Patoni, Demeter, Veres et al., Probiotic supplementation during antibiotic treatment is unjustified in maintaining the gut microbiome diversity: a systematic review and meta-analysis, BMC Med, doi:10.1186/s12916-023-02961-0
Emara, Mohamed, Lactobacillus reuteri in management of Helicobacter pylori infection in dyspeptic patients: a double-blind placebo-controlled randomized clinical trial, Ther. Adv. Gastroenterol, doi:10.1177/1756283X13503514
Engevik, Versalovic, Biochemical features of beneficial microbes: foundations for therapeutic microbiology, doi:10.1128/microbiolspec.BAD-0012-2016
Feng, Gao, Zhao, Yang, Gao et al., Oral administration of probiotics reduces chemotherapy-induced diarrhea and oral mucositis: a systematic review and meta-analysis, Front. Nutr, doi:10.3389/fnut.2022.823288
Ferlazzo, Rizzello, Bonaccorsi, Dongarr, Fink, Role of natural killer and dendritic cell crosstalk in immunomodulation by commensal bacteria probiotics, J. Biomed. Biotechnol, doi:10.1155/2011/473097
Fernández-Ferreiro, Formigo-Couceiro, Veiga-Gutierrez, Maldonado-Lobón, Hermida-Cao et al., Effects of Loigolactobacillus coryniformis K8 CECT 5711 on the immune response of elderly subjects to COVID-19 vaccination: a randomized controlled trial, Nutrients, doi:10.3390/nu14010228
Fijan, Microorganisms with claimed probiotic properties: an overview of recent literature, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph110504745
Fijan, Probiotics and their antimicrobial effect, Microorganisms, doi:10.3390/microorganisms11020528
Fitzgerald, Patel, Eckenberger, Guillemard, Veiga et al., Improved gut microbiome recovery following drug therapy is linked to abundance and replication of probiotic strains, Gut Microbes, doi:10.1080/19490976.2022.2094664
Foditsch, Pereira, Ganda, Gomez, Marques et al., Oral administration of Faecalibacterium prausnitzii decreased the incidence of severe diarrhea and related mortality rate and increased weight gain in preweaned dairy heifers, PLoS One, doi:10.1371/journal.pone.0145485
Frey-Furtado, Magalhães, Azevedo, Sampaio-Maia, The role of biotics as a therapeutic strategy for oral mucositis -a systematic review, Probiotics Antimicrob Proteins, doi:10.1007/s12602-023-10116-z
Garcia, Knoll, Longo, Novaes, Assem et al., Effect of the probiotic Saccharomyces cerevisiae on ligature-induced periodontitis in rats, J. Periodontal Res, doi:10.1111/jre.12274
Garcia, Miessi, Da Rocha, Gomes, Nuernberg et al., The effects of Lactobacillus reuteri on the inflammation and periodontal tissue repair in rats: a pilot study, The Saudi Dental Journal, doi:10.1016/j.sdentj.2022.05.004
Gaspar, Donders, Palmeira-De-Oliveira, Queiroz, Tomaz et al., Bacteriocin production of the probiotic Lactobacillus acidophilus KS400, AMB Express, doi:10.1186/s13568-018-0679-z
Gomaa, Allam, Haridi, Eliwa, Darwish, High-protein concentrated pro-yogurt (pro-WPI) enriched with whey protein isolate improved athletic anemia and performance in a placebo-controlled study, Front. Nutr, doi:10.3389/fnut.2021.788446
Gou, Zhang, Ren, Li, Zhang, How do intestinal probiotics restore the intestinal barrier? Front, Microbiol, doi:10.3389/fmicb.2022.929346
Guallar-Garrido, Julián, Bacillus Calmette-Guérin (BCG) therapy for bladder Cancer: an update, Immunotargets Ther, doi:10.2147/ITT.S202006
Guedes, Pontes, Barreto Silva, Neves, Klein, Randomized controlled trials reporting the effects of probiotics in individuals with overweight and obesity: a critical review of the interventions and body adiposity parameters, Clin. Nutr, doi:10.1016/j.clnu.2023.03.017
Guo, Li, Xie, Zhang, Liu et al., The NAD+-dependent deacetylase, Bifidobacterium longum Sir2 in response to oxidative stress by deacetylating SigH (O H) and FOXO3a in Bifidobacterium longum and HEK293T cell respectively, Free Radic. Biol. Med
Guo, Wu, Hung, Sun, Zhao et al., Lactobacillus paracasei ET-22 suppresses dental caries by regulating microbiota of dental plaques and inhibiting biofilm formation, Nutrients, doi:10.3390/nu15153316
Gutierrez-Castrellon, Gandara-Martí, Abreu Y Abreu, Nieto-Rufino, López-Orduña et al., Probiotic improves symptomatic and viral clearance in Covid19 outpatients: a randomized, quadruple-blinded, placebocontrolled trial, Gut Microbes, doi:10.1080/19490976.2021.2018899
Hadadi, Berweiler, Wang, Trajkovski, Intestinal microbiota as a route for micronutrient bioavailability, Curr Opin Endocr Metab Res, doi:10.1016/j.coemr.2021.100285
Haghighat, Mohammadshahi, Shayanpour, Haghighizadeh, Rahmdel et al., The effect of synbiotic and probiotic supplementation on mental health parameters in patients undergoing hemodialysis: a double-blind, randomized, placebo-controlled trial, Indian J Nephrol, doi:10.4103/ijn.IJN_341_19
Hameed, Sattar Salman, Co-aggregative effect of probiotics bacteria against diarrheal causative bacteria, Arch Razi Inst, doi:10.22092/ARI.2022.359870.2494
Hampelska, Jaworska, Babalska, Karpiński, The role of oral microbiota in intra-oral halitosis, J. Clin. Med, doi:10.3390/jcm9082484
Han, Yum, Cho, Kim, Improvement of halitosis by probiotic bacterium Weissella cibaria CMU: a randomized controlled trial, Front. Microbiol, doi:10.3389/fmicb.2023.1108762
Hasan, Jang, Lee, Kim, Hur et al., Heat-killed Bacillus sp. SJ-10 probiotic acts as a growth and humoral innate immunity response enhancer in olive flounder (Paralichthys olivaceus), Fish Shellfish Immunol, doi:10.1016/j.fsi.2019.03.018
Hasanpour, Babajafari, Mazloomi, Shams, The effects of soymilk plus probiotics supplementation on cardiovascular risk factors in patients with type 2 diabetes mellitus: a randomized clinical trial, BMC Endocr. Disord, doi:10.1186/s12902-023-01290-w
Hasna, Hemida, Koula, Spînu, Ungureanu et al., In vitro and in vivo study of combined effect of some algerian medicinal plants and probiotics against Helicobacter pylori, Microorganisms, doi:10.3390/microorganisms11051242
He, Wang, Zhang, Shi, Wang et al., Evaluation of cholesterol transformation abilities and probiotic properties of Bacteroides dorei YGMCC0564, Front. Microbiol, doi:10.3389/fmicb.2023.1279996
Hemarajata, Versalovic, Effects of probiotics on gut microbiota: mechanisms of intestinal immunomodulation and neuromodulation, Ther. Adv. Gastroenterol, doi:10.1177/1756283X12459294
Hernandez, Sánchez, Llama-Palacios, Ciudad, Collado, Strategies to combat caries by maintaining the integrity of biofilm and homeostasis during the rapid phase of supragingival plaque formation, Antibiotics, doi:10.3390/antibiotics11070880
Higuchi, Furuichi, Maeda, Tsugawa, Ito, Effects of probiotics in children with acute gastroenteritis: a systematic review and meta-analysis focusing on probiotics utilized in Japan, J. Infect. Chemother. S, doi:10.1016/j.jiac.2023.11.005
Hills, Pontefract, Mishcon, Black, Sutton et al., Gut microbiome: profound implications for diet and disease, Nutrients, doi:10.3390/nu11071613
Hoffmann, Fraser, Palumbo, Ravel, Rowthorn et al., Probiotics: achieving a better regulatory fit, Food Drug Law J
Hoffmann, Kleine-Weber, Schroeder, Kruger, Herrler et al., SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor, Cells, doi:10.1016/j.cell.2020.02.052
Holdcroft, Ireland, Payne, The vaginal microbiome in health and disease -what role do common intimate hygiene practices play?, Microorganisms, doi:10.3390/microorganisms11020298
Homayouni Rad, Pourjafar, Mirzakhani, A comprehensive review of the application of probiotics and postbiotics in oral health, Front. Cell. Infect. Microbiol, doi:10.3389/fcimb.2023.1120995
Hoppe, Önning, Hulthén, Freeze-dried Lactobacillus plantarum 299v increases iron absorption in young females-double isotope sequential single-blind studies in menstruating women, PLoS One, doi:10.1371/journal.pone.0189141
Horii, Suzuki, Takano, Shibuya, Ichijima et al., Lower impact of vonoprazan-amoxicillin dual therapy on gut microbiota for Helicobacter pylori eradication, J. Gastroenterol. Hepatol, doi:10.1111/jgh.15572
Hu, Zhang, Hua, Chen, Changes in the salivary microbiota of oral leukoplakia and oral cancer, Oral Oncol, doi:10.1016/j.oraloncology.2016.03.007
Huang, Xing, Liu, Chen, Tang, Efficacy of probiotics in the treatment of acute diarrhea in children: a systematic review and metaanalysis of clinical trials, Transl. Pediatr, doi:10.21037/tp-21-511
Hurtado-Camarena, Serafín-Higuera, Chávez-Cortez, Pitones-Rubio, Lactobacillus probiotics and their impact on periodontal diseases, EAS J Dent Oral Med, doi:10.36349/easjdom.2023.v05i04.004
Hyink, Wescombe, Upton, Ragland, Burton et al., Salivaricin A2 and the novel lantibiotic salivaricin B are encoded at adjacent loci on a 190-kilobase transmissible megaplasmid in the oral probiotic strain Streptococcus salivarius K12, Appl. Environ. Microbiol, doi:10.1128/AEM.02265-06
Im, Lee, Kim, Kim, Evaluation of enterococcal probiotic usage and review of potential health benefits, safety, and risk of antibioticresistant strain emergence, Antibiotics, doi:10.3390/antibiotics12081327
Invernici, Furlaneto, Salvador, Ouwehand, Salminen et al., Bifidobacterium animalis subsp lactis HN019 presents antimicrobial potential against periodontopathogens and modulates the immunological response of oral mucosa in periodontitis patients, PLoS One, doi:10.1371/journal.pone.0238425
Ismail, Nawawi, Hsin, Hao, Mahmood et al., Probiotic containing Lactobacillus reuteri DSM 17648 as an adjunct treatment for Helicobacter pylori infection: a randomized, double-blind, placebo-controlled trial, Helicobacter, doi:10.1111/hel.13017
Ismail, Raja Ali, Wong, Muhammad Nawawi, Kok et al., IDDF2022-ABS-0107. The effect of Lactobacillus reuteri probiotic as an adjunct treatment for Helicobacter pylori infection in adults, Gut, doi:10.1136/gutjnl-2022-iddf.10
Jang, Rod-In, Monmai, Sohn, Kim et al., Anti-inflammatory potential of Lactobacillus reuteri LM1071 via eicosanoid regulation in LPS-stimulated RAW264.7 cells, J. Appl. Microbiol, doi:10.1111/jam.15331
Jansen, Abdelbary, Conrads, A concerted probiotic activity to inhibit periodontitis-associated bacteria, PLoS One, doi:10.1371/journal.pone.0248308
Javid, Amerian, Basir, Ekrami, Haghighizadeh et al., Effects of the consumption of probiotic yogurt containing Bifidobacterium lactis Bb12 on the levels of Streptococcus mutans and lactobacilli in saliva of students with initial stages of dental caries: a double-blind randomized controlled trial, Caries Res, doi:10.1159/000504164
Jia, Zou, Han, Bae, Jeon, Gut microbiome-mediated mechanisms for reducing cholesterol levels: implications for ameliorating cardiovascular disease, Trends Microbiol, doi:10.1016/j.tim.2022.08.003
Jiang, Gu, Liu, Zhao, Xia et al., Lactobacillus brevis 23017 relieves mercury toxicity in the Colon by modulation of oxidative stress and inflammation through the interplay of MAPK and NF-κB signaling cascades, Front. Microbiol, doi:10.3389/fmicb.2018.02425
Kakiuchi, Mizoe, Yamamoto, Imamura, Hashiguchi et al., Effect of probiotics during vonoprazan-containing triple therapy on gut microbiota in Helicobacter pylori infection: a randomized controlled trial, Helicobacter, doi:10.1111/hel.12690
Kang, Kim, Chung, Lee, Oh, Inhibitory effect of Weissella cibaria isolates on the production of volatile Sulphur compounds, J. Clin. Periodontol, doi:10.1111/j.1600-051X.2006.00893.x
Kany, Vollrath, Relja, Cytokines in inflammatory disease, Int. J. Mol. Sci, doi:10.3390/ijms20236008
Kawahara, Makizaki, Oikawa, Tanaka, Maeda et al., Oral administration of Bifidobacterium bifidum G9-1 alleviates rotavirus gastroenteritis through regulation of intestinal homeostasis by inducing mucosal protective factors, PLoS One, doi:10.1371/journal.pone.0173979
Kawashima, Hayashi, Kosaka, Kawashima, Igarashi et al., Lactobacillus plantarum strain YU from fermented foods activates Th1 and protective immune responses, Int. Immunopharmacol, doi:10.1016/j.intimp.2011.08.013
Keelan, Newnham, Recent advances in the prevention of preterm birth, F1000Res, doi:10.12688/f1000research.11385.1
Khan, Dwibedi, Sundh, Pradhan, Kraft et al., Synergy and oxygen adaptation for development of next-generation probiotics, Nature, doi:10.1038/s41586-023-06378-w
Khan, Mi, Gao, Hu, Gu et al., Dynamic changes of the gut microbial colonization in preterm infants with different time points after birth, Front. Microbiol, doi:10.3389/fmicb.2023.1078426
Kim, Kang, Yeu, Lee, Cho, Inhibitory effect of the probiotic bacteria, Weissella cibaria CMU on halitosis: a randomized placebo-controlled study, J. Korean Acad. Oral Health, doi:10.11149/jkaoh.2020.44.4.246
Kim, Kim, Kim, Jang, Han et al., Lactobacillus plantarum LC27 and Bifidobacterium longum LC67 simultaneously alleviate high-fat diet-induced colitis, endotoxemia, liver steatosis, and obesity in mice, Nutr. Res, doi:10.1016/j.nutres.2019.03.008
Kim, Lee, Kim, Paik, Antioxidant and angiotensinconverting enzyme (ACE) inhibitory activities of yogurt supplemented with Lactiplantibacillus plantarum NK181 and Lactobacillus delbrueckii KU200171 and sensory evaluation, Foods, doi:10.3390/foods10102324
Kitada, Ogura, Monno, Koya, Sirtuins and type 2 diabetes: role in inflammation, oxidative stress, and mitochondrial function, Front. Endocrinol, doi:10.3389/fendo.2019.00187
Knipe, Temperton, Lange, Bass, Tyler, Probiotics and competitive exclusion of pathogens in shrimp aquaculture, Rev. Aquac, doi:10.1111/raq.12477
Kora, Chapter 7 -Probiotics in the prevention and treatment of diarrheal disease
Koradia, Kapadia, Trivedi, Chanchu, Harper, Probiotic and cranberry supplementation for preventing recurrent uncomplicated urinary tract infections in premenopausal women: a controlled pilot study, Expert Rev. Anti-Infect. Ther, doi:10.1080/14787210.2019.1664287
Korcok, Tršic-Milanovic, Ivanovic, Dordevic, Development of probiotic formulation for the treatment of iron deficiency anemia, Chem. Pharm. Bull, doi:10.1248/cpb.c17-00634
Koutnikova, Genser, Monteiro-Sepulveda, Faurie, Rizkalla et al., Impact of bacterial probiotics on obesity, diabetes and nonalcoholic fatty liver disease related variables: a systematic review and meta-analysis of randomised controlled trials, BMJ Open, doi:10.1136/bmjopen-2017-017995
Lalla, Saunders, Peterson, Chemotherapy or radiationinduced oral mucositis, Dent. Clin. N. Am, doi:10.1016/j.cden.2013.12.005
Lee, Lee, Kim, Nam, Kang, Reduction of halitosis by a tablet containing Weissella cibaria CMU: a randomized, double-blind, placebo-controlled study, J. Med. Food, doi:10.1089/jmf.2019.4603
Lee, Park, Kim, Seo, Lee et al., Probiotic bacteria, B. Longum and L. acidophilus inhibit infection by rotavirus in vitro and decrease the duration of diarrhea in pediatric patients, Clin. Res. Hepatol. Gastroenterol, doi:10.1016/j.clinre.2014.09.006
Lei, Xu, Huang, Yuan, Meta-analysis of the effect of probiotics or synbiotics on the risk factors in patients with coronary artery disease, Front Cardiovasc Med, doi:10.3389/fcvm.2023.1154888
Leong, Derraik, Hofman, Cutfield, Antibiotics, gut microbiome and obesity, Clin. Endocrinol, doi:10.1111/cen.13495
Lesan, Hajifattahi, Rahbar, Mohammadi, The effect of probiotic yoghurt on the frequency of salivary Candida, J. Res. Dent. Maxillofac. Sci, doi:10.29252/jrdms.2.2.1
Li, Xu, Ye, Wu, Shi et al., Efficacy of Lactobacillus rhamnosus GG in treatment of acute pediatric diarrhea: a systematic review with meta-analysis, World J. Gastroenterol, doi:10.3748/wjg.v25.i33.4999
Liang, Wang, Hu, Luo, Li et al., Administration of Lactobacillus helveticus NS8 improves behavioral, cognitive, and biochemical aberrations caused by chronic restraint stress, Neuroscience, doi:10.1016/j.neuroscience.2015.09.033
Liu, Cao, Liu, Li, Tian et al., Effect of perioperative probiotic supplements on postoperative short-term outcomes in gastric cancer patients receiving neoadjuvant chemotherapy: a double-blind, randomized controlled trial, Nutrition, doi:10.1016/j.nut.2021.111574
Liu, Wang, Shi, Tao, Nahata, Efficacy and safety of probiotics and synbiotics for functional constipation in children: a systematic review and meta-analysis of randomized clinical trials, Clin. Nutr, doi:10.1016/j.clnu.2023.08.015
Liu, Wang, Wu, Modulation of gut microbiota and immune system by probiotics, pre-biotics, and post-biotics, Front. Nutr, doi:10.3389/fnut.2021.634897
Liu, Zhu, Song, Sohaib, Wang et al., Limosilactobacillus reuteri consumption significantly reduces the total cholesterol concentration without affecting other cardiovascular disease risk factors in adults: a systematic review and meta-analysis, Nutr. Res, doi:10.1016/j.nutres.2023.06.004
Lopez-Siles, Duncan, Garcia-Gil, Martinez-Medina, Faecalibacterium prausnitzii: from microbiology to diagnostics and prognostics, ISME J, doi:10.1038/ismej.2016.176
Louis, Duncan, Sheridan, Walker, Flint, Microbial lactate utilisation and the stability of the gut microbiome, Gut Microb, doi:10.1017/gmb.2022.3
Luise, Bosi, Raff, Amatucci, Virdis et al., Bacillus spp. probiotic strains as a potential tool for limiting the use of antibiotics, and improving the growth and health of pigs and chickens, Front. Microbiol, doi:10.3389/fmicb.2022.801827
Ma, Shen, Shi, Sakandar, Quan et al., Targeting gut microbiota and metabolism as the major probiotic mechanism -an evidence-based review, Trends Food Sci. Technol, doi:10.1016/j.tifs.2023.06.013
Madhivanan, Alleyn, Raphael, Krupp, Ravi et al., Identification of culturable vaginal Lactobacillus species among reproductive age women in Mysore, India, J. Med. Microbiol, doi:10.1099/jmm.0.000070
Maitre, Mahalli, Micheneau, Delpierre, Guerin et al., Pre and probiotics involved in the modulation of Oral bacterial species: new therapeutic leads in mental disorders?, Microorganisms, doi:10.3390/microorganisms9071450
Maldonado Galdeano, Cazorla, Lemme Dumit, Vélez, Perdigón, Beneficial effects of probiotic consumption on the immune system, Ann. Nutr. Metab, doi:10.1159/000496426
Malfertheiner, Megraud, Rokkas, Gisbert, Liou et al., Management of Helicobacter pylori infection: the Maastricht VI/Florence consensus report, Gut, doi:10.1136/gutjnl-2022-327745
Mandar, Sõerunurk, Štšepetova, Smidt, Rööp et al., Impact of Lactobacillus crispatus-containing oral and vaginal probiotics on vaginal health: a randomised double-blind placebo controlled clinical trial, Benef Microbes, doi:10.3920/BM2022.0091
Mann, Park, Johnston, Ji, Hwang et al., Oral probiotic activities and biosafety of Lactobacillus gasseri HHuMIN D, Microb. Cell Factories, doi:10.1186/s12934-021-01563-w
Martin, Chain, Miquel, Lu, Gratadoux et al., The commensal bacterium Faecalibacterium prausnitzii is protective in DNBS-induced chronic moderate and severe colitis models, Inflamm. Bowel Dis, doi:10.1097/01.MIB.0000440815.76627.64
Martinez, Balciunas, Converti, Cotter, De Souza et al., Bacteriocin production by Bifidobacterium spp. a review, Biotechnol. Adv, doi:10.1016/j.biotechadv.2013.01.010
Menezes, Zanette, Magalhães, Da Silva, Lago et al., Higher Bifidobacterium spp. fecal abundance is associated with a lower prevalence of hyperglycemia and cardiovascular risk markers among schoolchildren from Bahia, Brazil, PLoS One, doi:10.1371/journal.pone.0290813
Meng, Liu, Dong, Gu, Yang, Effects of probiotics on preventing caries in preschool children: a systematic review and meta-analysis, J. Clin. Pediatr. Dent, doi:10.22514/jocpd.2023.014
Meng, Xiao, Zhang, He, Ou et al., Renin-angiotensin system inhibitors improve the clinical outcomes of COVID-19 patients with hypertension, Emerg. Microbes. Infect, doi:10.1080/22221751.2020.1746200
Mestrovic, Matijašić, Perić, Čipčić Paljetak, Barešić et al., The role of gut, vaginal, and urinary microbiome in urinary tract infections: from bench to bedside, Diagnostics, doi:10.3390/diagnostics11010007
Momin, Khan, Kashyap, Pervaiz, Akram et al., The effects of probiotics on cholesterol levels in patients with metabolic syndrome: a systematic review, Cureus, doi:10.7759/cureus.37567
Nadeem, Siddiqui, Al-Harbi, Al-Harbi, Ahmad, TLR-7 agonist attenuates airway reactivity and inflammation through Nrf2-mediated antioxidant protection in a murine model of allergic asthma, Int. J. Biochem. Cell Biol, doi:10.1016/j.biocel.2016.02.004
Naseri, Saadati, Yari, Asbaghi, Hezaveh et al., Beneficial effects of probiotic and synbiotic supplementation on some cardiovascular risk factors among individuals with prediabetes and type 2 diabetes mellitus: a gradeassessed systematic review, meta-analysis, and meta-regression of randomized clinical trials, Pharmacol. Res, doi:10.1016/j.phrs.2022.106288
Nataraj, Ali, Behare, Yadav, Postbiotics-parabiotics: the new horizons in microbial biotherapy and functional foods, Microb. Cell Factories, doi:10.1186/s12934-020-01426-w
Nayebi, Navashenaq, Soleimani, Nachvak, Probiotic supplementation: a prospective approach in the treatment of COVID-19, Nutr. Health, doi:10.1177/02601060211049631
Nedzi-Gora, Wróblewska, Gorska, The effect of Lactobacillus salivarius SGL03 on clinical and microbiological parameters in periodontal patients, Pol. J. Microbiol, doi:10.33073/pjm-2020-047
Nguyen, Brody, Radaic, Kapila, Probiotics for periodontal health-current molecular findings, Periodontol, doi:10.1111/prd.12382
Nigam, Panwar, Singh, Orchestrating the fecal microbiota transplantation: current technological advancements and potential biomedical application, Front Med Technol, doi:10.3389/fmedt.2022.961569
O'toole, Marchesi, Hill, Next-generation probiotics: the spectrum from probiotics to live biotherapeutics, Nat. Microbiol, doi:10.1038/nmicrobiol.2017.57
Obrenovich, Leaky gut, leaky brain?, Microorganisms, doi:10.3390/microorganisms6040107
Ochoa, Castro, Bulhosa, Manso, Fernandes et al., Influence of the probiotic L. reuteri on periodontal clinical parameters after nonsurgical treatment: a systematic review, Microorganisms, doi:10.3390/microorganisms11061449
Ohtani, Yoshimoto, Hara, Obesity and cancer: a gut microbial connection, Cancer Res, doi:10.1158/0008-5472.CAN-13-3501
Okumura, Takeda, Maintenance of intestinal homeostasis by mucosal barriers, Inflamm Regener
Olaimat, Aolymat, Al-Holy, Ayyash, Ghoush et al., The potential application of probiotics and prebiotics for the prevention and treatment of COVID-19, NPJ Sci. Food, doi:10.1038/s41538-020-00078-9
Pallavi, Barik, Sahoo, Rajhans, Raut, Alleviation of dental caries by use of isolated potential probiotic and its characterization, Biotechnol. Appl. Biochem, doi:10.1002/bab.2471
Pan, Wang, Qi, Yi, Hu, Effects of Lactobacillus on the levels of the NF-N:B and inflammatory mediators in the mouse inflammation model, Chin. J. Prev. Vet. Med
Papadimitriou, Zoumpopoulou, Foligné, Alexandraki, Kazou et al., Discovering probiotic microorganisms: in vitro, in vivo, genetic and omics approaches, Front. Microbiol, doi:10.3389/fmicb.2015.00058
Park, Lee, Park, Jeong, Yun et al., Efficacy and safety of MED-01 probiotics on vaginal health: a 12-week, multicenter, randomized, double-blind, placebo-controlled clinical trial, Nutrients, doi:10.3390/nu15020331
Parkin, Christophersen, Verhasselt, Cooper, Martino, Risk factors for gut dysbiosis in early life, Microorganisms, doi:10.3390/microorganisms9102066
Patangia, Anthony Ryan, Dempsey, Paul Ross, Stanton, Impact of antibiotics on the human microbiome and consequences for host health, MicrobiologyOpen, doi:10.1002/mbo3.1260
Patch, Pearce, Cheng, Boyapati, Brenna, Bacillus Subtilis (BG01-4™) improves self-reported symptoms for constipation, indigestion, and dyspepsia: a phase 1/2A randomized controlled trial, Nutrients, doi:10.3390/nu15214490
Patil, Shetty, Padhye, Comparative evaluation of the inhibitory effect of Lactobacillus rhamnosus on halitosis-causing bacteria: an invitro microbiological study, Cureus, doi:10.7759/cureus.38568
Pavlidou, Fasoulas, Mantzorou, Giaginis, Clinical evidence on the potential beneficial effects of probiotics and prebiotics in cardiovascular disease, Int. J. Mol. Sci, doi:10.3390/ijms232415898
Penumetcha, Ahluwalia, Irfan, Khan, Reddy et al., The efficacy of probiotics in the management of Helicobacter pylori: a systematic review, Cureus, doi:10.7759/cureus.20483
Perez-Ramos, Madi-Moussa, Coucheney, Drider, Current knowledge of the mode of action and immunity mechanisms of LAB-bacteriocins, Microorganisms, doi:10.3390/microorganisms9102107
Peroni, Nuzzi, Trambusti, Di Cicco, Comberiati, Microbiome composition and its impact on the development of allergic diseases, Front. Immunol, doi:10.3389/fimmu.2020.00700
Petrova, Lievens, Malik, Imholz, Lebeer, Lactobacillus species as biomarkers and agents that can promote various aspects of vaginal health, Front. Physiol, doi:10.3389/fphys.2015.00081
Pique, Berlanga, Miñana-Galbis, Health benefits of heat-killed (tyndallized) probiotics: an overview, Int. J. Mol. Sci, doi:10.3390/ijms20102534
Pizzino, Irrera, Cucinotta, Pallio, Mannino et al., Oxidative stress: harms and benefits for human health, Oxidative Med. Cell. Longev, doi:10.1155/2017/8416763
Plaza-Diaz, Ruiz-Ojeda, Vilchez-Padial, Gil, Evidence of the anti-inflammatory effects of probiotics and synbiotics in intestinal chronic diseases, Nutrients, doi:10.3390/nu9060555
Pourrajab, Fatahi, Sohouli, Găman, Shidfar, The effects of probiotic/synbiotic supplementation compared to placebo on biomarkers of oxidative stress in adults: a systematic review and meta-analysis of randomized controlled trials, Crit. Rev. Food Sci. Nutr, doi:10.1080/10408398.2020.1821166
Prabhurajeshwar, Chandrakanth, Evaluation of antimicrobial properties and their substances against pathogenic bacteria in-vitro by probiotic lactobacilli strains isolated from commercial yoghurt, Clinical Nutrition Experimental, doi:10.1016/j.yclnex.2018.10.001
Pushpass, Alzoufairi, Mancini, Quilter, Fava et al., Chronic consumption of probiotics, oats, and apples has differential effects on postprandial bile acid profile and cardiometabolic disease risk markers compared with an isocaloric control (cornflakes): a randomized trial, Am. J. Clin. Nutr, doi:10.1016/j.ajcnut.2022.10.013
Quaranta, Guarnaccia, Fancello, Agrillo, Iannarelli et al., Fecal microbiota transplantation and other gut microbiota manipulation strategies, Microorganisms, doi:10.3390/microorganisms10122424
Rastogi, Singh, Gut microbiome and human health: exploring how the probiotic genus Lactobacillus modulate immune responses, Front. Pharmacol, doi:10.3389/fphar.2022.1042189
Rayyan, Agraib, Alkhatib, Yamani, Abu-Sneineh et al., Does probiotic supplementation improve quality of life in mildto-moderately active ulcerative colitis patients in Jordan? A secondary outcome of the randomized, double-blind, placebo-controlled study, Eur. J. Nutr, doi:10.1007/s00394-023-03207-8
Reid, Bruce, Fraser, Heinemann, Owen et al., Oral probiotics can resolve urogenital infections, FEMS Immunol. Med. Microbiol, doi:10.1111/j.1574-695X.2001.tb01549.x
Reid, Jass, Sebulsky, Mccormick, Potential uses of probiotics in clinical practice, Clin. Microbiol. Rev, doi:10.1128/CMR.16.4.658-672.2003
Riaz Rajoka, Zhao, Lu, Lian, Li et al., Anticancer potential against cervix cancer (HeLa) cell line of probiotic Lactobacillus casei and Lactobacillus paracasei strains isolated from human breast milk, Food Funct, doi:10.1039/c8fo00547h
Ribeiro, Silveira, Cândido, Cardoso, Carvalho et al., Effects of antibiotic treatment on gut microbiota and how to overcome its negative impacts on human health, ACS Infect. Dis, doi:10.1021/acsinfecdis.0c00036
Roe, Boyte, Elkins, Goldman, Heimbach et al., Considerations for determining safety of probiotics: a USP perspective, Regul. Toxicol. Pharmacol, doi:10.1016/j.yrtph.2022.105266
Rosa, Santos, Abreu, Balthazar, Rocha et al., Antiproliferative and apoptotic effects of probiotic whey dairy beverages in human prostate cell lines, Food Res. Int, doi:10.1016/j.foodres.2020.109450
Roy, Dhaneshwar, Role of prebiotics, probiotics, and synbiotics in management of inflammatory bowel disease: current perspectives, World J. Gastroenterol, doi:10.3748/wjg.v29.i14.2078
Ruiz-Tovar, Llavero, Fernandez-Contreras, Effect of Lactobacillus kefiri, in conjunction with PENS T6 and a hypocaloric diet, on weight loss, hypertension and laboratory glycemic and lipid profile, Nutrients, doi:10.3390/nu15214549
Rwubuzizi, Kim, Holzapfel, Todorov, Beneficial, safety, and antioxidant properties of lactic acid bacteria: a next step in their evaluation as potential probiotics, Heliyon, doi:10.1016/j.heliyon.2023.e15610
Sadeghpour Heravi, Hu, Bifidobacterium: host-microbiome interaction and mechanism of action in preventing common gut-microbiota-associated complications in preterm infants: a narrative review, Nutrients, doi:10.3390/nu15030709
Saiz, Taveira, Alves, Probiotics in oral health and disease: a systematic review, Appl. Sci, doi:10.3390/app11178070
Salinas-Azuceno, Martínez-Hernández, Maldonado-Noriega, Rodríguez-Hernández, Probiotic monotherapy with Lactobacillus reuteri (Prodentis) as a coadjutant to reduce subgingival dysbiosis in a patient with periodontitis, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph19137835
Sandberg, Önning, Engström, Scheers, Iron supplements containing Lactobacillus Plantarum 299v increase ferric iron and up-regulate the ferric reductase DCYTB in human Caco-2/HT29 MTX co-cultures, Nutrients, doi:10.3390/nu10121949
Santagati, Scillato, Patanè, Aiello, Stefani, Bacteriocinproducing oral streptococci and inhibition of respiratory pathogens, FEMS Immunol. Med. Microbiol, doi:10.1111/j.1574-695X.2012.00928.x
Savigamin, Samuthpongtorn, Mahakit, Nopsopon, Heath et al., Probiotic as a potential gut microbiome modifier for stroke treatment: a systematic scoping review of in vitro and in vivo studies, Nutrients, doi:10.3390/nu14173661
Seminotti, Grings, Tucci, Leipnitz, Saso, Nuclear factor erythroid-2-related factor 2 signaling in the neuropathophysiology of inherited metabolic disorders, Front. Cell. Neurosci, doi:10.3389/fncel.2021.785057
Shanahan, Ghosh, O'toole, The healthy microbiome-what is the definition of a healthy gut microbiome?, Gastroenterology, doi:10.1053/j.gastro.2020.09.057
Sharma, Tilak, Bakhshi, Raina, Kumar et al., Lactobacillus brevis CD2 lozenges prevent oral mucositis in patients undergoing high dose chemotherapy followed by haematopoietic stem cell transplantation, ESMO Open, doi:10.1136/esmoopen-2016-000138
Shen, Chen, Lei, Shen, Lv et al., Nonfood probiotic, prebiotic, and synbiotic use reduces all-cause and cardiovascular mortality risk in older adults: a population-based cohort study, J. Nutr. Health Aging, doi:10.1007/s12603-023-1921-1
Siciliano, Reale, Mazzeo, Morandi, Silvetti et al., Paraprobiotics: a new perspective for functional foods and nutraceuticals, Nutrients, doi:10.3390/nu13041225
Silva, De Cássia, Nayla De Souza, Roque, Da Silva et al., Probiotics as an alternative antimicrobial therapy: current reality and future directions, J. Funct. Foods
Singh, Rao, Probiotics: a potential immunomodulator in COVID-19 infection management, Nutr. Res, doi:10.1016/j.nutres.2020.12.014
Singh, Singh, Gaur, Probiotics as multifaceted oral vaccines against colon cancer: a review, Front. Immunol, doi:10.3389/fimmu.2022.1002674
So, Quigley, Whelan, Probiotics in irritable bowel syndrome and inflammatory bowel disease: review of mechanisms and effectiveness, Curr. Opin. Gastroenterol, doi:10.1097/MOG.0000000000000902
Srivastava, Ellepola, Venkiteswaran, Chai, Ohshima et al., Lactobacillus plantarum 108 inhibits Streptococcus mutans and Candida albicans mixed-species biofilm formation, Antibiotics, doi:10.3390/antibiotics9080478
Starosila, Rybalko, Varbanetz, Ivanskaya, Sorokulova, Antiinfluenza activity of a Bacillus subtilis probiotic strain, Antimicrob. Agents Chemother, doi:10.1128/AAC.00539-17
Storia, Di Giuseppe, Volpe, Oliviero, Villani et al., Physical properties and antimicrobial activity of bioactive film based on whey protein and lactobacillus curvatus 54M16 producer of bacteriocins, Food Hydrocoll, doi:10.1016/j.foodhyd.2020.105959
Sulijaya, Takahashi, Yamazaki, Host modulation therapy using anti-inflammatory and antioxidant agents in periodontitis: a review to a clinical translation, Arch. Oral Biol, doi:10.1016/j.archoralbio.2019.07.002
Suman, Rakshit, Ogireddy, Singh, Gupta et al., Microbiome as a key player in sustainable agriculture and human health, Front. Soil Sci, doi:10.3389/fsoil.2022.821589
Tabrizi, Ostadmohammadi, Akbari, Lankarani, Vakili et al., The effects of probiotic supplementation on clinical symptom, weight loss, glycemic control, lipid and hormonal profiles, biomarkers of inflammation, and oxidative stress in women with polycystic ovary syndrome: a systematic review and meta-analysis of randomized controlled trials, Probiotics Antimicrob Proteins, doi:10.1007/s12602-019-09559-0
Tang, Bohannon, Lew, Jensen, Jung et al., Randomised, double-blind, placebo-controlled trial of probiotics to eliminate COVID-19 transmission in exposed household contacts (PROTECT-EHC): a clinical trial protocol, BMJ Open, doi:10.1136/bmjopen-2020-047069
Telaku, Telaku, Behluli, Isjanovski, Alidema, Impact of Lactobacillus Reuteri and three other probiotics in Helicobacter pylori eradication, Macedonian. J. Med. Sci, doi:10.3889/oamjms.2022.10733
Teneva, Denev, Biologically active compounds from probiotic microorganisms and plant extracts used as biopreservatives, Microorganisms, doi:10.3390/microorganisms11081896
Thomas, Thomas, Butler-Sanchez, Dietary modification for the restoration of gut microbiome and management of symptoms in irritable bowel syndrome, Am. J. Lifestyle Med, doi:10.1177/15598276211012968
Tian, Ran, Wen, Fu, Zhou et al., Probiotics improve symptoms of patients with COVID-19 through gut-lung axis: a systematic review and meta-analysis, Front. Nutr, doi:10.3389/fnut.2023.1179432
Tiwari, Dicks, Popov, Karaseva, Ermakov et al., Probiotics at war against viruses: what is missing from the picture?, Front. Microbiol, doi:10.3389/fmicb.2020.01877
Trivedi, Jena, Tikoo, Kumar, Melatonin modulated autophagy and Nrf2 signaling pathways in mice with colitis-associated colon carcinogenesis, Mol. Carcinog, doi:10.1002/mc.22274
Tsay, Hsu, H. pylori infection and extra-gastroduodenal diseases, J. Biomed. Sci, doi:10.1186/s12929-018-0469-6
Valdez, Ximenez-Fyvie, Caiaffa, Rodrigues Dos Santos, Gonzales Cervantes et al., Antagonist effect of probiotic bifidobacteria on biofilms of pathogens associated with periodontal disease, Microb. Pathog, doi:10.1016/j.micpath.2020.104657
Van Zyl, Deane, Dicks, Molecular insights into probiotic mechanisms of action employed against intestinal pathogenic bacteria, Gut Microbes, doi:10.1080/19490976.2020.1831339
Vancamelbeke, Vermeire, The intestinal barrier: a fundamental role in health and disease, Expert Rev. Gastroenterol. Hepatol, doi:10.1080/17474124.2017.1343143
Volgenant, Van Der Waal, Brandt, Buijs, Van Der Veen et al., The evaluation of the effects of two probiotic strains on the oral ecosystem: a randomized clinical trial, Front. Oral Health, doi:10.3389/froh.2022.825017
Vonderheid, Tussing-Humphreys, Park, Pauls, Hemphill et al., A systematic review and meta-analysis on the effects of probiotic species on iron absorption and iron status, Nutrients, doi:10.3390/nu11122938
Wang, Li, Wang, Wei, Qu et al., The role of the gut microbiota and probiotics associated with microbial metabolisms in cancer prevention and therapy, Front. Pharmacol, doi:10.3389/fphar.2022.1025860
Wang, Wang, Cao, Zhu, Ma, Comparative effectiveness of different probiotics supplements for triple Helicobacter pylori eradication: a network meta-analysis, Front. Cell. Infect. Microbiol, doi:10.3389/fcimb.2023.1120789
Wang, Wu, Wang, Xu, Mei et al., Antioxidant properties of probiotic bacteria, Nutrients, doi:10.3390/nu9050521
Wang, Zhang, Zhang, Probiotics regulate gut microbiota: an effective method to improve immunity, Molecules, doi:10.3390/molecules26196076
Wang, Zheng, Kuang, Yang, Xie et al., Effects of probiotics in patients with morbid obesity undergoing bariatric surgery: a systematic review and meta-analysis, Int. J. Obes, doi:10.1038/s41366-023-01375-5
Wischmeyer, Tang, Ren, Bohannon, Ramirez et al., Daily Lactobacillus probiotic versus placebo in COVID-19-exposed household contacts (PROTECT-EHC): a randomized clinical trial, medRxiv, doi:10.1101/2022.01.04.21268275
Witkin, The vaginal microbiome, vaginal anti-microbial defence mechanisms and the clinical challenge of reducing infection-related preterm birth, BJOG, doi:10.1111/1471-0528.13115
Wu, Chiou, Potential benefits of probiotics and prebiotics for coronary heart disease and stroke, Nutrients, doi:10.3390/nu13082878
Wu, Zhang, Lv, Li, Yi et al., Beneficial impact and molecular mechanism of Bacillus coagulans on piglets' intestine, Int. J. Mol. Sci, doi:10.3390/ijms19072084
Xiao, Zhao, Microbial transmission, colonisation and succession: from pregnancy to infancy, Gut, doi:10.1136/gutjnl-2022-328970
Yadav, Kumari, Singh, Sharma, Tiwari, Probiotics, prebiotics and synbiotics: safe options for next-generation therapeutics, Appl. Microbiol. Biotechnol, doi:10.1007/s00253-021-11646-8
Yakovenko, Strokova, Ivanov, Iakovenko, Gioeva et al., The effectiveness of a probiotic containing Bifidobacterium longum BB-46 and Enterococcus faecium ENCfa-68 in the treatment of post-infectious irritable bowel syndrome. Prospective randomized comparative study, Ter. Arkh, doi:10.26442/00403660.2022.02.201368
Yang, Pan, Jia, Bai, Zhi et al., Oral administration of Lactobacillus brevis 23017 combined with ellagic acid attenuates intestinal inflammatory injury caused by Eimeria infection by activating the Nrf2/HO-1 antioxidant pathway, Vet. Res, doi:10.1186/s13567-022-01042-z
Yao, Tan, Gao, Wang, Yang et al., Effects of probiotics on toll-like receptor expression in ulcerative colitis rats induced by 2,4,6-trinitrobenzene sulfonic acid, Mol. Med. Rep, doi:10.3892/mmr.2017.6226
Yao, Zhao, Wang, Liu, Bifidobacterium longum: protection against inflammatory bowel disease, J Immunol Res, doi:10.1155/2021/8030297
Yoo, Shin, Jeon, Yang, Kim et al., The effect of probiotics on halitosis: a systematic review and Meta-analysis, Probiotics Antimicrob Proteins, doi:10.1007/s12602-017-9351-1
You, Si, Kim, Yoon, Cha et al., Bacteroides vulgatus SNUG 40005 restores Akkermansia depletion by metabolite modulation, Gastroenterology, doi:10.1053/j.gastro.2022.09.040
Zarezadeh, Musazadeh, Ghalichi, Kavyani, Nasernia et al., Effects of probiotics supplementation on blood pressure: an umbrella metaanalysis of randomized controlled trials, Nutr. Metab. Cardiovasc. Dis, doi:10.1016/j.numecd.2022.09.005
Zeng, Fadaak, Alomeir, Wu, Wu et al., Effect of probiotic Lactobacillus plantarum on Streptococcus mutans and Candida albicans clinical isolates from children with early childhood caries, Int. J. Mol. Sci, doi:10.3390/ijms24032991
Zhang, Ding, Guo, Probiotic species in the management of periodontal diseases: an overview, Front. Cell. Infect. Microbiol, doi:10.3389/fcimb.2022.806463
Zhang, Duan, Cai, Cao, Wang et al., Next-generation probiotics: microflora intervention to human diseases, Biomed. Res. Int, doi:10.1155/2022/5633403
Zhao, Wang, Liu, Liu, Ji et al., Recent perspective of Lactobacillus in reducing oxidative stress to prevent disease, Antioxidants (Basel), doi:10.3390/antiox12030769
Zheng, Ahmad, Yang, Liang, Shen et al., Lactobacillus rhamnosus CY12 enhances intestinal barrier function by regulating tight junction protein expression, oxidative stress, and inflammation response in lipopolysaccharide-induced Caco-2 cells, IJMS, doi:10.3390/ijms231911162
Zheng, Guo, Yao, Jin, Cheng et al., Lactobacillus iners is associated with vaginal Dysbiosis in healthy pregnant women: a preliminary study, Biomed. Res. Int, doi:10.1155/2019/6079734
Zheng, Xu, Zhang, Liu, Ni, Effect of a probiotic formula on gastrointestinal health, immune responses and metabolic health in adults Frontiers in Microbiology 23 frontiersin.org with functional constipation or functional diarrhea, Front. Nutr, doi:10.3389/fnut.2023.1196625
Zheng, Zhang, Tang, Wu, Zhang et al., Probiotics fortify intestinal barrier function: a systematic review and meta-analysis of randomized trials, Front. Immun, doi:10.3389/fimmu.2023.1143548
Zhu, Pitre, Ching, Zeraatkar, Gruchy, Safety and efficacy of probiotic supplements as adjunctive therapies in patients with COVID-19: a systematic review and meta-analysis, PLoS One, doi:10.1371/journal.pone.0278356
Zhu, Wang, Li, Human gut microbiome: the second genome of human body, Protein Cell, doi:10.1007/s13238-010-0093-z
Zielinska, Kolozyn-Krajewska, Food-origin lactic acid bacteria may exhibit probiotic properties: review, Biomed. Res. Int, doi:10.1155/2018/5063185
DOI record:
{
"DOI": "10.3389/fmicb.2023.1296447",
"ISSN": [
"1664-302X"
],
"URL": "http://dx.doi.org/10.3389/fmicb.2023.1296447",
"abstract": "<jats:p>The imbalance of microbial composition and diversity in favor of pathogenic microorganisms combined with a loss of beneficial gut microbiota taxa results from factors such as age, diet, antimicrobial administration for different infections, other underlying medical conditions, etc. Probiotics are known for their capacity to improve health by stimulating the indigenous gut microbiota, enhancing host immunity resistance to infection, helping digestion, and carrying out various other functions. Concurrently, the metabolites produced by these microorganisms, termed postbiotics, which include compounds like bacteriocins, lactic acid, and hydrogen peroxide, contribute to inhibiting a wide range of pathogenic bacteria. This review presents an update on using probiotics in managing and treating various human diseases, including complications that may emerge during or after a COVID-19 infection.</jats:p>",
"alternative-id": [
"10.3389/fmicb.2023.1296447"
],
"author": [
{
"affiliation": [],
"family": "Petrariu",
"given": "Oana-Alina",
"sequence": "first"
},
{
"affiliation": [],
"family": "Barbu",
"given": "Ilda Czobor",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Niculescu",
"given": "Adelina-Gabriela",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Constantin",
"given": "Marian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Grigore",
"given": "Georgiana Alexandra",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cristian",
"given": "Roxana-Elena",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mihaescu",
"given": "Grigore",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Vrancianu",
"given": "Corneliu Ovidiu",
"sequence": "additional"
}
],
"container-title": "Frontiers in Microbiology",
"container-title-short": "Front. Microbiol.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2024,
1,
5
]
],
"date-time": "2024-01-05T05:29:24Z",
"timestamp": 1704432564000
},
"deposited": {
"date-parts": [
[
2024,
1,
5
]
],
"date-time": "2024-01-05T05:29:55Z",
"timestamp": 1704432595000
},
"funder": [
{
"DOI": "10.13039/501100008530",
"doi-asserted-by": "publisher",
"name": "European Regional Development Fund"
}
],
"indexed": {
"date-parts": [
[
2024,
1,
6
]
],
"date-time": "2024-01-06T00:21:26Z",
"timestamp": 1704500486935
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2024,
1,
5
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
1,
5
]
],
"date-time": "2024-01-05T00:00:00Z",
"timestamp": 1704412800000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fmicb.2023.1296447/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2024,
1,
5
]
]
},
"published-online": {
"date-parts": [
[
2024,
1,
5
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.4103/jpbs.jpbs_801_21",
"article-title": "Probiotics: dawn of a new era in dental caries management",
"author": "Abikshyeet",
"doi-asserted-by": "publisher",
"first-page": "34",
"journal-title": "J. Pharm. Bioallied Sci.",
"key": "ref1",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.3390/pharmaceutics12030241",
"article-title": "Mucoadhesive buccal films for local delivery of Lactobacillus brevis",
"author": "Abruzzo",
"doi-asserted-by": "publisher",
"first-page": "241",
"journal-title": "Pharmaceutics",
"key": "ref2",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1007/s12011-018-1541-5",
"article-title": "Enhancement in iron absorption on intake of chemometrically optimized ratio of probiotic strain Lactobacillus plantarum 299v with iron supplement pearl millet",
"author": "Adiki",
"doi-asserted-by": "publisher",
"first-page": "150",
"journal-title": "Biol. Trace Elem. Res.",
"key": "ref3",
"volume": "190",
"year": "2019"
},
{
"DOI": "10.1002/iid3.635",
"article-title": "Anti-inflammatory and immunomodulatory effects of Lactobacillus spp. as a preservative and therapeutic agent for IBD control",
"author": "Aghamohammad",
"doi-asserted-by": "publisher",
"first-page": "e635",
"journal-title": "Immun Inflamm Dis.",
"key": "ref4",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.3390/pathogens11020112",
"article-title": "Effect of Lactobacillus reuteri on gingival inflammation and composition of the oral microbiota in patients undergoing treatment with fixed orthodontic appliances: study protocol of a randomized control trial",
"author": "Agossa",
"doi-asserted-by": "publisher",
"first-page": "112",
"journal-title": "Pathogens",
"key": "ref5",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1016/j.virusres.2020.198103",
"article-title": "Immunological co-ordination between gut and lungs in SARS-CoV-2 infection",
"author": "Ahlawat",
"doi-asserted-by": "publisher",
"first-page": "198103",
"journal-title": "Virus Res.",
"key": "ref6",
"volume": "286",
"year": "2020"
},
{
"DOI": "10.3168/jds.2022-22762",
"article-title": "Effects of probiotics administration on lactose intolerance in adulthood: a meta-analysis",
"author": "Ahn",
"doi-asserted-by": "publisher",
"first-page": "4489",
"journal-title": "J. Dairy Sci.",
"key": "ref7",
"volume": "106",
"year": "2023"
},
{
"DOI": "10.4014/jmb.1912.12054",
"article-title": "An aqueous extract of a Bifidobacterium species induces apoptosis and inhibits invasiveness of non-small cell lung cancer cells",
"author": "Ahn",
"doi-asserted-by": "publisher",
"first-page": "885",
"journal-title": "J. Microbiol. Biotechnol.",
"key": "ref8",
"volume": "30",
"year": "2020"
},
{
"DOI": "10.12816/0003256",
"article-title": "Recurrent urinary tract infections management in women: a review",
"author": "Al-Badr",
"doi-asserted-by": "publisher",
"first-page": "359",
"journal-title": "Sultan Qaboos Univ. Med. J.",
"key": "ref9",
"volume": "13",
"year": "2013"
},
{
"DOI": "10.3390/molecules28020619",
"article-title": "Leaky gut and the ingredients that help treat it: a review",
"author": "Aleman",
"doi-asserted-by": "publisher",
"first-page": "619",
"journal-title": "Molecules",
"key": "ref10",
"volume": "28",
"year": "2023"
},
{
"DOI": "10.1111/jre.12415",
"article-title": "Clinical effects of probiotics containing Bacillus species on gingivitis: a pilot randomized controlled trial",
"author": "Alkaya",
"doi-asserted-by": "publisher",
"first-page": "497",
"journal-title": "J. Periodontal Res.",
"key": "ref11",
"volume": "52",
"year": "2017"
},
{
"DOI": "10.1016/j.ajpath.2021.02.003",
"article-title": "Lactobacillus acidophilus induces a strain-specific and toll-like receptor 2-dependent enhancement of intestinal epithelial tight junction barrier and protection against intestinal inflammation",
"author": "Al-Sadi",
"doi-asserted-by": "publisher",
"first-page": "872",
"journal-title": "Am. J. Pathol.",
"key": "ref12",
"volume": "191",
"year": "2021"
},
{
"DOI": "10.1007/s00253-012-4241-7",
"article-title": "Antioxidant properties of potentially probiotic bacteria: in vitro and in vivo activities",
"author": "Amaretti",
"doi-asserted-by": "publisher",
"first-page": "809",
"journal-title": "Appl. Microbiol. Biotechnol.",
"key": "ref13",
"volume": "97",
"year": "2013"
},
{
"DOI": "10.3390/app11125472",
"article-title": "Probiotics, prebiotics, synbiotics and dental caries. New perspectives, suggestions, and patient coaching approach for a cavity-free mouth",
"author": "Amargianitakis",
"doi-asserted-by": "publisher",
"first-page": "5472",
"journal-title": "Appl. Sci.",
"key": "ref14",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.3233/BLC-200277",
"article-title": "The urinary microbiome and bladder cancer: susceptibility and immune responsiveness",
"author": "Andolfi",
"doi-asserted-by": "publisher",
"first-page": "225",
"journal-title": "Bladder Cancer",
"key": "ref15",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2018.01270",
"article-title": "Cytokine tuning of intestinal epithelial function",
"author": "Andrews",
"doi-asserted-by": "publisher",
"first-page": "1270",
"journal-title": "Front. Immunol.",
"key": "ref16",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.3390/nu15081862",
"article-title": "Lactobacillus probiotics improve vaginal dysbiosis in asymptomatic women",
"author": "Ansari",
"doi-asserted-by": "publisher",
"first-page": "1862",
"journal-title": "Nutrients",
"key": "ref17",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.1016/j.micpath.2020.104657",
"article-title": "Antagonist effect of probiotic bifidobacteria on biofilms of pathogens associated with periodontal disease",
"author": "Argandona Valdez",
"doi-asserted-by": "publisher",
"first-page": "104657",
"journal-title": "Microb. Pathog.",
"key": "ref18",
"volume": "150",
"year": "2021"
},
{
"DOI": "10.1016/S2666-5247(22)00043-X",
"article-title": "Sustained effect of LACTIN-V (Lactobacillus crispatus CTV-05) on genital immunology following standard bacterial vaginosis treatment: results from a randomised, placebo-controlled trial",
"author": "Armstrong",
"doi-asserted-by": "publisher",
"first-page": "e435",
"journal-title": "Lancet Microbe",
"key": "ref19",
"volume": "3",
"year": "2022"
},
{
"article-title": "Effects of oral probiotic feeding on toll-like receptor gene expression of the chicken’s cecal tonsil",
"author": "Asgari",
"first-page": "151",
"journal-title": "Rep Biochem Mol Biol.",
"key": "ref20",
"volume": "6",
"year": "2018"
},
{
"DOI": "10.15171/bi.2017.22",
"article-title": "Lactobacillus plantarum induces apoptosis in oral cancer KB cells through upregulation of PTEN and downregulation of MAPK signalling pathways",
"author": "Asoudeh-Fard",
"doi-asserted-by": "publisher",
"first-page": "193",
"journal-title": "Bioimpacts",
"key": "ref21",
"volume": "7",
"year": "2017"
},
{
"DOI": "10.1111/omi.12047",
"article-title": "Looking in the Porphyromonas gingivalis cabinet of curiosities: the microbium, the host and cancer association",
"author": "Atanasova",
"doi-asserted-by": "publisher",
"first-page": "55",
"journal-title": "Mol Oral Microbiol",
"key": "ref22",
"volume": "29",
"year": "2014"
},
{
"DOI": "10.3390/pharmaceutics14112543",
"article-title": "Gut dysbiosis and diabetic foot ulcer: role of probiotics",
"author": "Awasthi",
"doi-asserted-by": "publisher",
"first-page": "2543",
"journal-title": "Pharmaceutics",
"key": "ref23",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1016/j.jobcr.2023.03.013",
"article-title": "Oral microbial shift induced by probiotic Bacillus coagualans along with its clinical perspectives",
"author": "Aysha Jebin",
"doi-asserted-by": "publisher",
"first-page": "398",
"journal-title": "J Oral Biol Craniofac Res.",
"key": "ref24",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1155/2018/8063647",
"article-title": "Immunomodulatory effects of probiotics on cytokine profiles",
"author": "Azad",
"doi-asserted-by": "publisher",
"first-page": "8063647",
"journal-title": "Biomed. Res. Int.",
"key": "ref25",
"volume": "2018",
"year": "2018"
},
{
"DOI": "10.1007/s12602-022-09909-5",
"article-title": "Bacillus species as direct-fed microbial antibiotic alternatives for monogastric production",
"author": "Bahaddad",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Probiotics Antimicrob Proteins",
"key": "ref26",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.1007/s00203-022-03314-w",
"article-title": "The impacts of probiotics in eradication therapy of Helicobacter pylori",
"author": "Bai",
"doi-asserted-by": "publisher",
"first-page": "692",
"journal-title": "Arch. Microbiol.",
"key": "ref27",
"volume": "204",
"year": "2022"
},
{
"DOI": "10.3889/oamjms.2018.406",
"article-title": "Probiotics improve urogenital health in women",
"author": "Ballini",
"doi-asserted-by": "publisher",
"first-page": "1845",
"journal-title": "Open Access Maced J Med Sci.",
"key": "ref28",
"volume": "6",
"year": "2018"
},
{
"DOI": "10.1016/j.anaerobe.2022.102652",
"article-title": "Role of a probiotic strain in the modulation of gut microbiota and cytokines in inflammatory bowel disease",
"author": "Bamola",
"doi-asserted-by": "publisher",
"first-page": "102652",
"journal-title": "Anaerobe",
"key": "ref29",
"volume": "78",
"year": "2022"
},
{
"DOI": "10.3390/nu15112631",
"article-title": "Functional foods: a promising strategy for restoring gut microbiota diversity impacted by SARS-CoV-2 variants",
"author": "Banerjee",
"doi-asserted-by": "publisher",
"first-page": "2631",
"journal-title": "Nutrients",
"key": "ref30",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.3389/fphar.2017.00603",
"article-title": "Lactobacillus rhamnosus GG: an overview to explore the rationale of its use in cancer",
"author": "Banna",
"doi-asserted-by": "publisher",
"first-page": "603",
"journal-title": "Front. Pharmacol.",
"key": "ref31",
"volume": "8",
"year": "2017"
},
{
"DOI": "10.1073/pnas.2219392120",
"article-title": "Discovery of phosphorylated lantibiotics with proimmune activity that regulate the oral microbiome",
"author": "Barbour",
"doi-asserted-by": "publisher",
"first-page": "e2219392120",
"journal-title": "Proc. Natl. Acad. Sci. U. S. A.",
"key": "ref32",
"volume": "120",
"year": "2023"
},
{
"DOI": "10.1007/s13668-023-00462-3",
"article-title": "Probiotics and prebiotics: any role in menopause-related diseases?",
"author": "Barrea",
"doi-asserted-by": "publisher",
"first-page": "83",
"journal-title": "Curr Nutr Rep.",
"key": "ref33",
"volume": "12",
"year": "2023"
},
{
"DOI": "10.17294/2330-0698.1705",
"article-title": "Oral fungal microbiota: to thrush and beyond",
"author": "Baumgardner",
"doi-asserted-by": "publisher",
"first-page": "252",
"journal-title": "J Patient Cent Res Rev.",
"key": "ref34",
"volume": "6",
"year": "2019"
},
{
"DOI": "10.3390/microorganisms11102528",
"article-title": "Factors influencing neonatal gut microbiome and health with a focus on necrotizing enterocolitis",
"author": "Beharry",
"doi-asserted-by": "publisher",
"first-page": "2528",
"journal-title": "Microorganisms",
"key": "ref35",
"volume": "11",
"year": "2023"
},
{
"DOI": "10.1002/prp2.988",
"article-title": "A practical treatment for COVID-19 and the next pandemic",
"author": "Bhattacharya",
"doi-asserted-by": "publisher",
"first-page": "e00988",
"journal-title": "Pharmacol. Res. Perspect.",
"key": "ref36",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.7759/cureus.31313",
"article-title": "Role of probiotics in human health",
"author": "Bodke",
"doi-asserted-by": "publisher",
"first-page": "e31313",
"journal-title": "Cureus",
"key": "ref37",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1016/j.clnesp.2022.08.023",
"article-title": "Probiotics: a gut response to the COVID-19 pandemic but what does the evidence show?",
"author": "Brahma",
"doi-asserted-by": "publisher",
"first-page": "17",
"journal-title": "Clin Nutr ESPEN.",
"key": "ref38",
"volume": "51",
"year": "2022"
},
{
"DOI": "10.1016/j.mib.2022.102229",
"article-title": "Ecological and functional roles of bacteriophages in contrasting environments: marine, terrestrial and human gut",
"author": "Brown",
"doi-asserted-by": "publisher",
"first-page": "102229",
"journal-title": "Curr. Opin. Microbiol.",
"key": "ref39",
"volume": "70",
"year": "2022"
},
{
"DOI": "10.1038/nature17645",
"article-title": "Culturing of ‘unculturable’ human microbiota reveals novel taxa and extensive sporulation",
"author": "Browne",
"doi-asserted-by": "publisher",
"first-page": "543",
"journal-title": "Nature",
"key": "ref40",
"volume": "533",
"year": "2016"
},
{
"DOI": "10.3390/foods11111575",
"article-title": "Screening and probiotic potential evaluation of bacteriocin-producing Lactiplantibacillus plantarum in vitro",
"author": "Bu",
"doi-asserted-by": "publisher",
"first-page": "1575",
"journal-title": "Foods.",
"key": "ref41",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.3390/microorganisms9010069",
"article-title": "Probiotic alternative to chlorhexidine in periodontal therapy: evaluation of clinical and microbiological parameters",
"author": "Butera",
"doi-asserted-by": "publisher",
"first-page": "69",
"journal-title": "Microorganisms",
"key": "ref42",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1016/j.cmi.2015.10.014",
"article-title": "Clostridium butyricum: from beneficial to a new emerging pathogen",
"author": "Cassir",
"doi-asserted-by": "publisher",
"first-page": "37",
"journal-title": "Clin. Microbiol. Infect.",
"key": "ref43",
"volume": "22",
"year": "2016"
},
{
"DOI": "10.3390/foods11030268",
"article-title": "Probiotics supplementation improves intestinal permeability, obesity index and metabolic biomarkers in elderly Thai subjects: a randomized controlled trial",
"author": "Chaiyasut",
"doi-asserted-by": "publisher",
"first-page": "268",
"journal-title": "Foods",
"key": "ref44",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.3168/jds.2020-19820",
"article-title": "Quality characteristics of yogurts fermented with short-chain fatty acid-producing probiotics and their effects on mucin production and probiotic adhesion onto human colon epithelial cells",
"author": "Chang",
"doi-asserted-by": "publisher",
"first-page": "7415",
"journal-title": "J. Dairy Sci.",
"key": "ref45",
"volume": "104",
"year": "2021"
},
{
"article-title": "Modulation of host immune response by Bacteroides fragilis polysaccharides: a review of recent observations",
"author": "Chang",
"first-page": "1",
"journal-title": "J. Biomed. Lab. Sci.",
"key": "ref46",
"volume": "28",
"year": "2016"
},
{
"DOI": "10.1016/j.jfda.2018.12.011",
"article-title": "Next generation probiotics in disease amelioration",
"author": "Chang",
"doi-asserted-by": "publisher",
"first-page": "615",
"journal-title": "J. Food Drug Anal.",
"key": "ref47",
"volume": "27",
"year": "2019"
},
{
"DOI": "10.1186/s13063-023-07443-5",
"article-title": "Effect of probiotic supplementation on in-hospital mortality in patients with acute myocardial infarction: a study protocol for an open-label, randomized, controlled, superiority clinical trial",
"author": "Chen",
"doi-asserted-by": "publisher",
"first-page": "429",
"journal-title": "Trials",
"key": "ref48",
"volume": "24",
"year": "2023"
},
{
"DOI": "10.1038/s41430-021-00986-3",
"article-title": "Effect of early enteral nutrition combined with probiotics in patients with stroke: a meta-analysis of randomized controlled trials",
"author": "Chen",
"doi-asserted-by": "publisher",
"first-page": "592",
"journal-title": "Eur. J. Clin. Nutr.",
"key": "ref49",
"volume": "76",
"year": "2022"
},
{
"DOI": "10.3389/fimmu.2021.578386",
"article-title": "Anti-inflammatory and immunomodulatory effects of probiotics in gut inflammation: a door to the body",
"author": "Cristofori",
"doi-asserted-by": "publisher",
"first-page": "578386",
"journal-title": "Front. Immunol.",
"key": "ref50",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1080/17446651.2020.1719068",
"article-title": "A brief overview on the use of probiotics to treat overweight and obese patients",
"author": "Daniali",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Expert. Rev. Endocrinol. Metab.",
"key": "ref51",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1016/j.afres.2022.100185",
"article-title": "Current status of probiotic and related health benefits",
"author": "Das",
"doi-asserted-by": "publisher",
"first-page": "100185",
"journal-title": "Applied. Food Research",
"key": "ref52",
"volume": "2",
"year": "2022"
},
{
"DOI": "10.1128/spectrum.01682-22",
"article-title": "Randomized, double-blind, placebo-controlled trial of a throat spray with selected lactobacilli in COVID-19 outpatients",
"author": "De Boeck",
"doi-asserted-by": "publisher",
"first-page": "e0168222",
"journal-title": "Microbiol. Spectr.",
"key": "ref53",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1016/j.biotechadv.2018.09.003",
"article-title": "How to select a probiotic? A review and update of methods and criteria",
"author": "de Melo Pereira",
"doi-asserted-by": "publisher",
"first-page": "2060",
"journal-title": "Biotechnol. Adv.",
"key": "ref54",
"volume": "36",
"year": "2018"
},
{
"DOI": "10.1016/j.heliyon.2023.e13475",
"article-title": "Probiotics and metabolites regulate the oral and gut microbiome composition as host modulation agents in periodontitis: a narrative review",
"author": "Deandra",
"doi-asserted-by": "publisher",
"first-page": "e13475",
"journal-title": "Heliyon",
"key": "ref55",
"volume": "9",
"year": "2023"
},
{
"DOI": "10.3389/fimmu.2022.840245",
"article-title": "Lactobacillus spp. for gastrointestinal health: current and future perspectives",
"author": "Dempsey",
"doi-asserted-by": "publisher",
"first-page": "840245",
"journal-title": "Front. Immunol.",
"key": "ref56",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1007/s12603-023-2028-4",
"article-title": "Efficacy and safety of probiotics in geriatric patients with constipation: systematic review and meta-analysis",
"author": "Deng",
"doi-asserted-by": "publisher",
"first-page": "1140",
"journal-title": "J. Nutr. Health Aging",
"key": "ref57",
"volume": "27",
"year": "2023"
},
{
"DOI": "10.1080/01635581.2018.1446091",
"article-title": "Mechanisms of phytonutrient modulation of cyclooxygenase-2 (cox-2) and inflammation related to cancer",
"author": "Desai",
"doi-asserted-by": "publisher",
"first-page": "350",
"journal-title": "Nutr. Cancer",
"key": "ref58",
"volume": "70",
"year": "2018"
},
{
"article-title": "Effect of administration of Streptococcus salivarius K12 on the occurrence of streptococcal pharyngo-tonsillitis, scarlet fever and acute otitis media in 3 years old children",
"author": "Di Pierro",
"first-page": "4601",
"journal-title": "Eur. Rev. Med. Pharmacol. Sci.",
"key": "ref59",
"volume": "20",
"year": "2016"
},
{
"DOI": "10.1093/femsle/fnx014",
"article-title": "Probiotic strains modulate cytokine production and the immune interplay between human peripheral blood mononucear cells and colon cancer cells",
"author": "Djaldetti",
"doi-asserted-by": "publisher",
"journal-title": "FEMS Microbiol. Lett.",
"key": "ref60",
"volume": "364",
"year": "2017"
},
{
"DOI": "10.3389/fnut.2023.1218909",
"article-title": "Effect of probiotics intake on constipation in children: an umbrella review",
"author": "Dong",
"doi-asserted-by": "publisher",
"first-page": "1218909",
"journal-title": "Front. Nutr.",
"key": "ref61",
"volume": "10",
"year": "2023"
},
{
"DOI": "10.1155/2021/4464002",
"article-title": "Clostridium butyricum protects IPEC-J2 cells from ETEC K88-induced oxidative damage by activating the Nrf2/ARE signaling pathway",
"author": "Dou",
"doi-asserted-by": "publisher",
"first-page": "4464002",
"journal-title": "Oxidative Med. Cell. Longev.",
"key": "ref62",
"volume": "2021",
"year": "2021"
},
{
"DOI": "10.1080/10408398.2020.1843396",
"article-title": "Antibiotic-induced gut dysbiosis and barrier disruption and the potential protective strategies",
"author": "Duan",
"doi-asserted-by": "publisher",
"first-page": "1427",
"journal-title": "Crit. Rev. Food Sci. Nutr.",
"key": "ref63",
"volume": "62",
"year": "2022"
},
{
"DOI": "10.1186/s40168-020-00868-z",
"article-title": "Bacteroides thetaiotaomicron-derived outer membrane vesicles promote regulatory dendritic cell responses in health but not in inflammatory bowel disease",
"author": "Durant",
"doi-asserted-by": "publisher",
"first-page": "88",
"journal-title": "Microbiome",
"key": "ref64",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1186/s12866-020-02023-y",
"article-title": "Indole-3-lactic acid associated with Bifidobacterium-dominated microbiota significantly decreases inflammation in intestinal epithelial cells",
"author": "Ehrlich",
"doi-asserted-by": "publisher",
"first-page": "357",
"journal-title": "BMC Microbiol.",
"key": "ref65",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1186/s12916-023-02961-0",
"article-title": "Probiotic supplementation during antibiotic treatment is unjustified in maintaining the gut microbiome diversity: a systematic review and meta-analysis",
"author": "Elias",
"doi-asserted-by": "publisher",
"first-page": "262",
"journal-title": "BMC Med.",
"key": "ref66",
"volume": "21",
"year": "2023"
},
{
"DOI": "10.1177/1756283X13503514",
"article-title": "Lactobacillus reuteri in management of Helicobacter pylori infection in dyspeptic patients: a double-blind placebo-controlled randomized clinical trial",
"author": "Emara",
"doi-asserted-by": "publisher",
"first-page": "4",
"journal-title": "Ther. Adv. Gastroenterol.",
"key": "ref67",
"volume": "7",
"year": "2014"
},
{
"DOI": "10.1128/microbiolspec.BAD-0012-2016",
"article-title": "Biochemical features of beneficial microbes: foundations for therapeutic microbiology",
"author": "Engevik",
"doi-asserted-by": "publisher",
"journal-title": "Microbiol Spectr.",
"key": "ref68",
"volume": "5",
"year": "2017"
},
{
"first-page": "1",
"key": "ref69",
"volume-title": "Guidelines for the Evaluation of Probiotics in Food",
"year": "2002"
},
{
"DOI": "10.3389/fnut.2022.823288",
"article-title": "Oral administration of probiotics reduces chemotherapy-induced diarrhea and oral mucositis: a systematic review and meta-analysis",
"author": "Feng",
"doi-asserted-by": "publisher",
"first-page": "823288",
"journal-title": "Front. Nutr.",
"key": "ref70",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.1155/2011/473097",
"article-title": "Role of natural killer and dendritic cell crosstalk in immunomodulation by commensal bacteria probiotics",
"author": "Ferlazzo",
"doi-asserted-by": "publisher",
"first-page": "473097",
"journal-title": "J. Biomed. Biotechnol.",
"key": "ref71",
"volume": "2011",
"year": "2011"
},
{
"DOI": "10.3390/nu14010228",
"article-title": "Effects of Loigolactobacillus coryniformis K8 CECT 5711 on the immune response of elderly subjects to COVID-19 vaccination: a randomized controlled trial",
"author": "Fernández-Ferreiro",
"doi-asserted-by": "publisher",
"first-page": "228",
"journal-title": "Nutrients",
"key": "ref72",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.3390/ijerph110504745",
"article-title": "Microorganisms with claimed probiotic properties: an overview of recent literature",
"author": "Fijan",
"doi-asserted-by": "publisher",
"first-page": "4745",
"journal-title": "Int. J. Environ. Res. Public Health",
"key": "ref73",
"volume": "11",
"year": "2014"
},
{
"DOI": "10.3390/microorganisms11020528",
"article-title": "Probiotics and their antimicrobial effect",
"author": "Fijan",
"doi-asserted-by": "publisher",
"first-page": "528",
"journal-title": "Microorganisms",
"key": "ref74",
"volume": "11",
"year": "2023"
},
{
"DOI": "10.1080/19490976.2022.2094664",
"article-title": "Improved gut microbiome recovery following drug therapy is linked to abundance and replication of probiotic strains",
"author": "FitzGerald",
"doi-asserted-by": "publisher",
"first-page": "2094664",
"journal-title": "Gut Microbes",
"key": "ref75",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1371/journal.pone.0145485",
"article-title": "Oral administration of Faecalibacterium prausnitzii decreased the incidence of severe diarrhea and related mortality rate and increased weight gain in preweaned dairy heifers",
"author": "Foditsch",
"doi-asserted-by": "publisher",
"first-page": "e0145485",
"journal-title": "PLoS One",
"key": "ref76",
"volume": "10",
"year": "2015"
},
{
"DOI": "10.1007/s12602-023-10116-z",
"article-title": "The role of biotics as a therapeutic strategy for oral mucositis – a systematic review",
"author": "Frey-Furtado",
"doi-asserted-by": "publisher",
"journal-title": "Probiotics Antimicrob Proteins",
"key": "ref77",
"volume": "30",
"year": "2023"
},
{
"DOI": "10.1111/jre.12274",
"article-title": "Effect of the probiotic Saccharomyces cerevisiae on ligature-induced periodontitis in rats",
"author": "Garcia",
"doi-asserted-by": "publisher",
"first-page": "26",
"journal-title": "J. Periodontal Res.",
"key": "ref78",
"volume": "51",
"year": "2016"
},
{
"DOI": "10.1016/j.sdentj.2022.05.004",
"article-title": "The effects of Lactobacillus reuteri on the inflammation and periodontal tissue repair in rats: a pilot study",
"author": "Garcia",
"doi-asserted-by": "publisher",
"first-page": "516",
"journal-title": "The Saudi Dental Journal",
"key": "ref79",
"volume": "34",
"year": "2022"
},
{
"DOI": "10.1186/s13568-018-0679-z",
"article-title": "Bacteriocin production of the probiotic Lactobacillus acidophilus KS400",
"author": "Gaspar",
"doi-asserted-by": "publisher",
"first-page": "153",
"journal-title": "AMB Express",
"key": "ref80",
"volume": "8",
"year": "2018"
},
{
"DOI": "10.3389/fnut.2021.788446",
"article-title": "High-protein concentrated pro-yogurt (pro-WPI) enriched with whey protein isolate improved athletic anemia and performance in a placebo-controlled study",
"author": "Gomaa",
"doi-asserted-by": "publisher",
"first-page": "788446",
"journal-title": "Front. Nutr.",
"key": "ref81",
"volume": "8",
"year": "2022"
},
{
"DOI": "10.3389/fmicb.2022.929346",
"article-title": "How do intestinal probiotics restore the intestinal barrier?",
"author": "Gou",
"doi-asserted-by": "publisher",
"first-page": "929346",
"journal-title": "Front. Microbiol.",
"key": "ref82",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.2147/ITT.S202006",
"article-title": "Bacillus Calmette-Guérin (BCG) therapy for bladder Cancer: an update",
"author": "Guallar-Garrido",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Immunotargets Ther.",
"key": "ref83",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1016/j.clnu.2023.03.017",
"article-title": "Randomized controlled trials reporting the effects of probiotics in individuals with overweight and obesity: a critical review of the interventions and body adiposity parameters",
"author": "Guedes",
"doi-asserted-by": "publisher",
"first-page": "835",
"journal-title": "Clin. Nutr.",
"key": "ref84",
"volume": "42",
"year": "2023"
},
{
"DOI": "10.1016/j.freeradbiomed.2017.05.012",
"article-title": "The NAD+-dependent deacetylase, Bifidobacterium longum Sir2 in response to oxidative stress by deacetylating SigH (O H) and FOXO3a in Bifidobacterium longum and HEK293T cell respectively",
"author": "Guo",
"doi-asserted-by": "publisher",
"first-page": "929",
"journal-title": "Free Radic. Biol. Med.",
"key": "ref85",
"volume": "108",
"year": "2017"
},
{
"DOI": "10.3390/nu15153316",
"article-title": "Lactobacillus paracasei ET-22 suppresses dental caries by regulating microbiota of dental plaques and inhibiting biofilm formation",
"author": "Guo",
"doi-asserted-by": "publisher",
"first-page": "3316",
"journal-title": "Nutrients",
"key": "ref86",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.1080/19490976.2021.2018899",
"article-title": "Probiotic improves symptomatic and viral clearance in Covid19 outpatients: a randomized, quadruple-blinded, placebo-controlled trial",
"author": "Gutierrez-Castrellon",
"doi-asserted-by": "publisher",
"first-page": "2018899",
"journal-title": "Gut Microbes",
"key": "ref87",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1016/j.coemr.2021.100285",
"article-title": "Intestinal microbiota as a route for micronutrient bioavailability",
"author": "Hadadi",
"doi-asserted-by": "publisher",
"first-page": "100285",
"journal-title": "Curr Opin Endocr Metab Res.",
"key": "ref88",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.4103/ijn.IJN_341_19",
"article-title": "The effect of synbiotic and probiotic supplementation on mental health parameters in patients undergoing hemodialysis: a double-blind, randomized, placebo-controlled trial",
"author": "Haghighat",
"doi-asserted-by": "publisher",
"first-page": "149",
"journal-title": "Indian J Nephrol.",
"key": "ref89",
"volume": "31",
"year": "2021"
},
{
"DOI": "10.3390/jcm9082484",
"article-title": "The role of oral microbiota in intra-oral halitosis",
"author": "Hampelska",
"doi-asserted-by": "publisher",
"first-page": "2484",
"journal-title": "J. Clin. Med.",
"key": "ref90",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.3389/fmicb.2023.1108762",
"article-title": "Improvement of halitosis by probiotic bacterium Weissella cibaria CMU: a randomized controlled trial",
"author": "Han",
"doi-asserted-by": "publisher",
"first-page": "1108762",
"journal-title": "Front. Microbiol.",
"key": "ref91",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.1016/j.fsi.2019.03.018",
"article-title": "Heat-killed Bacillus sp. SJ-10 probiotic acts as a growth and humoral innate immunity response enhancer in olive flounder (Paralichthys olivaceus)",
"author": "Hasan",
"doi-asserted-by": "publisher",
"first-page": "424",
"journal-title": "Fish Shellfish Immunol.",
"key": "ref92",
"volume": "88",
"year": "2019"
},
{
"DOI": "10.1186/s12902-023-01290-w",
"article-title": "The effects of soymilk plus probiotics supplementation on cardiovascular risk factors in patients with type 2 diabetes mellitus: a randomized clinical trial",
"author": "Hasanpour",
"doi-asserted-by": "publisher",
"first-page": "36",
"journal-title": "BMC Endocr. Disord.",
"key": "ref93",
"volume": "23",
"year": "2023"
},
{
"DOI": "10.3390/microorganisms11051242",
"article-title": "In vitro and in vivo study of combined effect of some algerian medicinal plants and probiotics against Helicobacter pylori",
"author": "Hasna",
"doi-asserted-by": "publisher",
"first-page": "1242",
"journal-title": "Microorganisms",
"key": "ref94",
"volume": "11",
"year": "2023"
},
{
"DOI": "10.3389/fmicb.2023.1279996",
"article-title": "Evaluation of cholesterol transformation abilities and probiotic properties of Bacteroides dorei YGMCC0564",
"author": "He",
"doi-asserted-by": "publisher",
"first-page": "1279996",
"journal-title": "Front. Microbiol.",
"key": "ref95",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.1177/1756283X12459294",
"article-title": "Effects of probiotics on gut microbiota: mechanisms of intestinal immunomodulation and neuromodulation",
"author": "Hemarajata",
"doi-asserted-by": "publisher",
"first-page": "39",
"journal-title": "Ther. Adv. Gastroenterol.",
"key": "ref96",
"volume": "6",
"year": "2013"
},
{
"DOI": "10.3390/antibiotics11070880",
"article-title": "Strategies to combat caries by maintaining the integrity of biofilm and homeostasis during the rapid phase of supragingival plaque formation",
"author": "Hernandez",
"doi-asserted-by": "publisher",
"first-page": "880",
"journal-title": "Antibiotics (Basel)",
"key": "ref97",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1016/j.jiac.2023.11.005",
"article-title": "Effects of probiotics in children with acute gastroenteritis: a systematic review and meta-analysis focusing on probiotics utilized in Japan",
"author": "Higuchi",
"doi-asserted-by": "publisher",
"journal-title": "J. Infect. Chemother.",
"key": "ref98",
"year": "2023"
},
{
"DOI": "10.3390/nu11071613",
"article-title": "Gut microbiome: profound implications for diet and disease",
"author": "Hills",
"doi-asserted-by": "publisher",
"first-page": "1613",
"journal-title": "Nutrients",
"key": "ref99",
"volume": "11",
"year": "2019"
},
{
"article-title": "Probiotics: achieving a better regulatory fit",
"author": "Hoffmann",
"first-page": "237",
"journal-title": "Food Drug Law J.",
"key": "ref100",
"volume": "69",
"year": "2014"
},
{
"DOI": "10.1016/j.cell.2020.02.052",
"article-title": "SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor",
"author": "Hoffmann",
"doi-asserted-by": "publisher",
"first-page": "271",
"journal-title": "Cells",
"key": "ref101",
"volume": "181",
"year": "2020"
},
{
"DOI": "10.3390/microorganisms11020298",
"article-title": "The vaginal microbiome in health and disease – what role do common intimate hygiene practices play?",
"author": "Holdcroft",
"doi-asserted-by": "publisher",
"first-page": "298",
"journal-title": "Microorganisms",
"key": "ref102",
"volume": "11",
"year": "2023"
},
{
"DOI": "10.3389/fcimb.2023.1120995",
"article-title": "A comprehensive review of the application of probiotics and postbiotics in oral health",
"author": "Homayouni Rad",
"doi-asserted-by": "publisher",
"first-page": "1120995",
"journal-title": "Front. Cell. Infect. Microbiol.",
"key": "ref103",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1371/journal.pone.0189141",
"article-title": "Freeze-dried Lactobacillus plantarum 299v increases iron absorption in young females-double isotope sequential single-blind studies in menstruating women",
"author": "Hoppe",
"doi-asserted-by": "publisher",
"first-page": "e0189141",
"journal-title": "PLoS One",
"key": "ref104",
"volume": "12",
"year": "2017"
},
{
"DOI": "10.1111/jgh.15572",
"article-title": "Lower impact of vonoprazan-amoxicillin dual therapy on gut microbiota for Helicobacter pylori eradication",
"author": "Horii",
"doi-asserted-by": "publisher",
"first-page": "3314",
"journal-title": "J. Gastroenterol. Hepatol.",
"key": "ref105",
"volume": "36",
"year": "2021"
},
{
"DOI": "10.1016/j.oraloncology.2016.03.007",
"article-title": "Changes in the salivary microbiota of oral leukoplakia and oral cancer",
"author": "Hu",
"doi-asserted-by": "publisher",
"first-page": "e6",
"journal-title": "Oral Oncol.",
"key": "ref106",
"volume": "56",
"year": "2016"
},
{
"DOI": "10.21037/tp-21-511",
"article-title": "Efficacy of probiotics in the treatment of acute diarrhea in children: a systematic review and meta-analysis of clinical trials",
"author": "Huang",
"doi-asserted-by": "publisher",
"first-page": "3248",
"journal-title": "Transl. Pediatr.",
"key": "ref107",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.36349/easjdom.2023.v05i04.004",
"article-title": "Lactobacillus probiotics and their impact on periodontal diseases",
"author": "Hurtado-Camarena",
"doi-asserted-by": "publisher",
"first-page": "111",
"journal-title": "EAS J Dent Oral Med",
"key": "ref108",
"volume": "5",
"year": "2023"
},
{
"DOI": "10.1128/AEM.02265-06",
"article-title": "Salivaricin A2 and the novel lantibiotic salivaricin B are encoded at adjacent loci on a 190-kilobase transmissible megaplasmid in the oral probiotic strain Streptococcus salivarius K12",
"author": "Hyink",
"doi-asserted-by": "publisher",
"first-page": "1107",
"journal-title": "Appl. Environ. Microbiol.",
"key": "ref109",
"volume": "73",
"year": "2007"
},
{
"DOI": "10.3390/antibiotics12081327",
"article-title": "Evaluation of enterococcal probiotic usage and review of potential health benefits, safety, and risk of antibiotic-resistant strain emergence",
"author": "Im",
"doi-asserted-by": "publisher",
"first-page": "1327",
"journal-title": "Antibiotics (Basel)",
"key": "ref110",
"volume": "12",
"year": "2023"
},
{
"DOI": "10.1371/journal.pone.0238425",
"article-title": "Bifidobacterium animalis subsp lactis HN019 presents antimicrobial potential against periodontopathogens and modulates the immunological response of oral mucosa in periodontitis patients",
"author": "Invernici",
"doi-asserted-by": "publisher",
"first-page": "e0238425",
"journal-title": "PLoS One",
"key": "ref111",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1111/hel.13017",
"article-title": "Probiotic containing Lactobacillus reuteri DSM 17648 as an adjunct treatment for Helicobacter pylori infection: a randomized, double-blind, placebo-controlled trial",
"author": "Ismail",
"doi-asserted-by": "publisher",
"first-page": "e13017",
"journal-title": "Helicobacter",
"key": "ref112",
"volume": "28",
"year": "2023"
},
{
"DOI": "10.1136/gutjnl-2022-iddf.10",
"article-title": "IDDF2022-ABS-0107. The effect of Lactobacillus reuteri probiotic as an adjunct treatment for Helicobacter pylori infection in adults",
"author": "Ismail",
"doi-asserted-by": "publisher",
"first-page": "A9",
"journal-title": "Gut",
"key": "ref113",
"volume": "71",
"year": "2022"
},
{
"DOI": "10.1111/jam.15331",
"article-title": "Anti-inflammatory potential of Lactobacillus reuteri LM1071 via eicosanoid regulation in LPS-stimulated RAW264.7 cells",
"author": "Jang",
"doi-asserted-by": "publisher",
"first-page": "67",
"journal-title": "J. Appl. Microbiol.",
"key": "ref114",
"volume": "133",
"year": "2022"
},
{
"DOI": "10.1371/journal.pone.0248308",
"article-title": "A concerted probiotic activity to inhibit periodontitis-associated bacteria",
"author": "Jansen",
"doi-asserted-by": "publisher",
"first-page": "e0248308",
"journal-title": "PLoS One",
"key": "ref115",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1016/j.tim.2022.08.003",
"article-title": "Gut microbiome-mediated mechanisms for reducing cholesterol levels: implications for ameliorating cardiovascular disease",
"author": "Jia",
"doi-asserted-by": "publisher",
"first-page": "76",
"journal-title": "Trends Microbiol.",
"key": "ref116",
"volume": "31",
"year": "2023"
},
{
"DOI": "10.3389/fmicb.2018.02425",
"article-title": "Lactobacillus brevis 23017 relieves mercury toxicity in the Colon by modulation of oxidative stress and inflammation through the interplay of MAPK and NF-κB signaling cascades",
"author": "Jiang",
"doi-asserted-by": "publisher",
"first-page": "2425",
"journal-title": "Front. Microbiol.",
"key": "ref117",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.1111/hel.12690",
"article-title": "Effect of probiotics during vonoprazan-containing triple therapy on gut microbiota in Helicobacter pylori infection: a randomized controlled trial",
"author": "Kakiuchi",
"doi-asserted-by": "publisher",
"first-page": "e12690",
"journal-title": "Helicobacter",
"key": "ref118",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.1111/j.1600-051X.2006.00893.x",
"article-title": "Inhibitory effect of Weissella cibaria isolates on the production of volatile Sulphur compounds",
"author": "Kang",
"doi-asserted-by": "publisher",
"first-page": "226",
"journal-title": "J. Clin. Periodontol.",
"key": "ref119",
"volume": "33",
"year": "2006"
},
{
"DOI": "10.3390/ijms20236008",
"article-title": "Cytokines in inflammatory disease",
"author": "Kany",
"doi-asserted-by": "publisher",
"first-page": "6008",
"journal-title": "Int. J. Mol. Sci.",
"key": "ref120",
"volume": "20",
"year": "2019"
},
{
"DOI": "10.1371/journal.pone.0173979",
"article-title": "Oral administration of Bifidobacterium bifidum G9-1 alleviates rotavirus gastroenteritis through regulation of intestinal homeostasis by inducing mucosal protective factors",
"author": "Kawahara",
"doi-asserted-by": "publisher",
"first-page": "e0173979",
"journal-title": "PLoS One",
"key": "ref121",
"volume": "12",
"year": "2017"
},
{
"DOI": "10.1016/j.intimp.2011.08.013",
"article-title": "Lactobacillus plantarum strain YU from fermented foods activates Th1 and protective immune responses",
"author": "Kawashima",
"doi-asserted-by": "publisher",
"first-page": "2017",
"journal-title": "Int. Immunopharmacol.",
"key": "ref122",
"volume": "11",
"year": "2011"
},
{
"DOI": "10.12688/f1000research.11385.1",
"article-title": "Recent advances in the prevention of preterm birth",
"author": "Keelan",
"doi-asserted-by": "publisher",
"journal-title": "F1000Res",
"key": "ref123",
"volume": "6",
"year": "2017"
},
{
"DOI": "10.1038/s41586-023-06378-w",
"article-title": "Synergy and oxygen adaptation for development of next-generation probiotics",
"author": "Khan",
"doi-asserted-by": "publisher",
"first-page": "381",
"journal-title": "Nature",
"key": "ref124",
"volume": "620",
"year": "2023"
},
{
"DOI": "10.3389/fmicb.2023.1078426",
"article-title": "Dynamic changes of the gut microbial colonization in preterm infants with different time points after birth",
"author": "Khan",
"doi-asserted-by": "publisher",
"first-page": "1078426",
"journal-title": "Front. Microbiol.",
"key": "ref125",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.11149/jkaoh.2020.44.4.246",
"article-title": "Inhibitory effect of the probiotic bacteria, Weissella cibaria CMU on halitosis: a randomized placebo-controlled study",
"author": "Kim",
"doi-asserted-by": "publisher",
"first-page": "246",
"journal-title": "J. Korean Acad. Oral Health",
"key": "ref126",
"volume": "44",
"year": "2020"
},
{
"DOI": "10.1016/j.nutres.2019.03.008",
"article-title": "Lactobacillus plantarum LC27 and Bifidobacterium longum LC67 simultaneously alleviate high-fat diet-induced colitis, endotoxemia, liver steatosis, and obesity in mice",
"author": "Kim",
"doi-asserted-by": "publisher",
"first-page": "78",
"journal-title": "Nutr. Res.",
"key": "ref127",
"volume": "67",
"year": "2019"
},
{
"DOI": "10.3390/foods10102324",
"article-title": "Antioxidant and angiotensin-converting enzyme (ACE) inhibitory activities of yogurt supplemented with Lactiplantibacillus plantarum NK181 and Lactobacillus delbrueckii KU200171 and sensory evaluation",
"author": "Kim",
"doi-asserted-by": "publisher",
"first-page": "2324",
"journal-title": "Foods.",
"key": "ref128",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.3389/fendo.2019.00187",
"article-title": "Sirtuins and type 2 diabetes: role in inflammation, oxidative stress, and mitochondrial function",
"author": "Kitada",
"doi-asserted-by": "publisher",
"first-page": "187",
"journal-title": "Front. Endocrinol.",
"key": "ref129",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1111/raq.12477",
"article-title": "Probiotics and competitive exclusion of pathogens in shrimp aquaculture",
"author": "Knipe",
"doi-asserted-by": "publisher",
"first-page": "324",
"journal-title": "Rev. Aquac.",
"key": "ref130",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1016/B978-0-12-823733-5.00011-8",
"article-title": "Chapter 7 – Probiotics in the prevention and treatment of diarrheal disease",
"author": "Kora",
"doi-asserted-by": "crossref",
"first-page": "107",
"key": "ref131",
"volume-title": "Probiotics in the Prevention and Management of Human Disease",
"year": "2022"
},
{
"DOI": "10.1080/14787210.2019.1664287",
"article-title": "Probiotic and cranberry supplementation for preventing recurrent uncomplicated urinary tract infections in premenopausal women: a controlled pilot study",
"author": "Koradia",
"doi-asserted-by": "publisher",
"first-page": "733",
"journal-title": "Expert Rev. Anti-Infect. Ther.",
"key": "ref132",
"volume": "17",
"year": "2019"
},
{
"DOI": "10.1248/cpb.c17-00634",
"article-title": "Development of probiotic formulation for the treatment of iron deficiency anemia",
"author": "Korcok",
"doi-asserted-by": "publisher",
"first-page": "347",
"journal-title": "Chem. Pharm. Bull.",
"key": "ref133",
"volume": "66",
"year": "2018"
},
{
"DOI": "10.1136/bmjopen-2017-017995",
"article-title": "Impact of bacterial probiotics on obesity, diabetes and non-alcoholic fatty liver disease related variables: a systematic review and meta-analysis of randomised controlled trials",
"author": "Koutnikova",
"doi-asserted-by": "publisher",
"first-page": "e017995",
"journal-title": "BMJ Open",
"key": "ref134",
"volume": "9",
"year": "2019"
},
{
"DOI": "10.1016/j.foodhyd.2020.105959",
"article-title": "Physical properties and antimicrobial activity of bioactive film based on whey protein and lactobacillus curvatus 54M16 producer of bacteriocins",
"author": "La Storia",
"doi-asserted-by": "publisher",
"first-page": "105959",
"journal-title": "Food Hydrocoll.",
"key": "ref135",
"volume": "108",
"year": "2020"
},
{
"DOI": "10.1016/j.cden.2013.12.005",
"article-title": "Chemotherapy or radiation-induced oral mucositis",
"author": "Lalla",
"doi-asserted-by": "publisher",
"first-page": "341",
"journal-title": "Dent. Clin. N. Am.",
"key": "ref136",
"volume": "58",
"year": "2014"
},
{
"DOI": "10.1089/jmf.2019.4603",
"article-title": "Reduction of halitosis by a tablet containing Weissella cibaria CMU: a randomized, double-blind, placebo-controlled study",
"author": "Lee",
"doi-asserted-by": "publisher",
"first-page": "649",
"journal-title": "J. Med. Food",
"key": "ref137",
"volume": "23",
"year": "2020"
},
{
"DOI": "10.1016/j.clinre.2014.09.006",
"article-title": "Probiotic bacteria, B. Longum and L. acidophilus inhibit infection by rotavirus in vitro and decrease the duration of diarrhea in pediatric patients",
"author": "Lee",
"doi-asserted-by": "publisher",
"first-page": "237",
"journal-title": "Clin. Res. Hepatol. Gastroenterol.",
"key": "ref138",
"volume": "39",
"year": "2015"
},
{
"DOI": "10.3389/fcvm.2023.1154888",
"article-title": "Meta-analysis of the effect of probiotics or synbiotics on the risk factors in patients with coronary artery disease",
"author": "Lei",
"doi-asserted-by": "publisher",
"first-page": "1154888",
"journal-title": "Front Cardiovasc Med.",
"key": "ref139",
"volume": "10",
"year": "2023"
},
{
"DOI": "10.3390/jpm12081282",
"article-title": "Probiotics and gut microbiota in obesity: myths and realities of a new health revolution",
"author": "Leon Aguilera",
"doi-asserted-by": "publisher",
"first-page": "1282",
"journal-title": "J Pers Med.",
"key": "ref140",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1111/cen.13495",
"article-title": "Antibiotics, gut microbiome and obesity",
"author": "Leong",
"doi-asserted-by": "publisher",
"first-page": "185",
"journal-title": "Clin. Endocrinol.",
"key": "ref141",
"volume": "88",
"year": "2018"
},
{
"DOI": "10.29252/jrdms.2.2.1",
"article-title": "The effect of probiotic yoghurt on the frequency of salivary Candida",
"author": "Lesan",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J. Res. Dent. Maxillofac. Sci.",
"key": "ref142",
"volume": "2",
"year": "2017"
},
{
"DOI": "10.3748/wjg.v25.i33.4999",
"article-title": "Efficacy of Lactobacillus rhamnosus GG in treatment of acute pediatric diarrhea: a systematic review with meta-analysis",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "4999",
"journal-title": "World J. Gastroenterol.",
"key": "ref143",
"volume": "25",
"year": "2019"
},
{
"DOI": "10.1016/j.neuroscience.2015.09.033",
"article-title": "Administration of Lactobacillus helveticus NS8 improves behavioral, cognitive, and biochemical aberrations caused by chronic restraint stress",
"author": "Liang",
"doi-asserted-by": "publisher",
"first-page": "561",
"journal-title": "Neuroscience",
"key": "ref144",
"volume": "310",
"year": "2015"
},
{
"DOI": "10.1016/j.nut.2021.111574",
"article-title": "Effect of perioperative probiotic supplements on postoperative short-term outcomes in gastric cancer patients receiving neoadjuvant chemotherapy: a double-blind, randomized controlled trial",
"author": "Liu",
"doi-asserted-by": "publisher",
"first-page": "111574",
"journal-title": "Nutrition",
"key": "ref145",
"volume": "96",
"year": "2022"
},
{
"DOI": "10.1016/j.clnu.2023.08.015",
"article-title": "Efficacy and safety of probiotics and synbiotics for functional constipation in children: a systematic review and meta-analysis of randomized clinical trials",
"author": "Liu",
"doi-asserted-by": "publisher",
"first-page": "1817",
"journal-title": "Clin. Nutr.",
"key": "ref146",
"volume": "42",
"year": "2023"
},
{
"DOI": "10.3389/fnut.2021.634897",
"article-title": "Modulation of gut microbiota and immune system by probiotics, pre-biotics, and post-biotics",
"author": "Liu",
"doi-asserted-by": "publisher",
"first-page": "634897",
"journal-title": "Front. Nutr.",
"key": "ref147",
"volume": "8",
"year": "2022"
},
{
"DOI": "10.1016/j.nutres.2023.06.004",
"article-title": "Limosilactobacillus reuteri consumption significantly reduces the total cholesterol concentration without affecting other cardiovascular disease risk factors in adults: a systematic review and meta-analysis",
"author": "Liu",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Nutr. Res.",
"key": "ref148",
"volume": "117",
"year": "2023"
},
{
"DOI": "10.1038/ismej.2016.176",
"article-title": "Faecalibacterium prausnitzii: from microbiology to diagnostics and prognostics",
"author": "Lopez-Siles",
"doi-asserted-by": "publisher",
"first-page": "841",
"journal-title": "ISME J.",
"key": "ref149",
"volume": "11",
"year": "2017"
},
{
"DOI": "10.1017/gmb.2022.3",
"article-title": "Microbial lactate utilisation and the stability of the gut microbiome",
"author": "Louis",
"doi-asserted-by": "publisher",
"first-page": "e3",
"journal-title": "Gut Microb.",
"key": "ref150",
"volume": "3",
"year": "2022"
},
{
"DOI": "10.3389/fmicb.2022.801827",
"article-title": "Bacillus spp. probiotic strains as a potential tool for limiting the use of antibiotics, and improving the growth and health of pigs and chickens",
"author": "Luise",
"doi-asserted-by": "publisher",
"first-page": "801827",
"journal-title": "Front. Microbiol.",
"key": "ref151",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1016/j.tifs.2023.06.013",
"article-title": "Targeting gut microbiota and metabolism as the major probiotic mechanism – an evidence-based review",
"author": "Ma",
"doi-asserted-by": "publisher",
"first-page": "178",
"journal-title": "Trends Food Sci. Technol.",
"key": "ref152",
"volume": "138",
"year": "2023"
},
{
"DOI": "10.1099/jmm.0.000070",
"article-title": "Identification of culturable vaginal Lactobacillus species among reproductive age women in Mysore, India",
"author": "Madhivanan",
"doi-asserted-by": "publisher",
"first-page": "636",
"journal-title": "J. Med. Microbiol.",
"key": "ref153",
"volume": "64",
"year": "2015"
},
{
"DOI": "10.3390/microorganisms9071450",
"article-title": "Pre and probiotics involved in the modulation of Oral bacterial species: new therapeutic leads in mental disorders?",
"author": "Maitre",
"doi-asserted-by": "publisher",
"first-page": "1450",
"journal-title": "Microorganisms.",
"key": "ref154",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1159/000496426",
"article-title": "Beneficial effects of probiotic consumption on the immune system",
"author": "Maldonado Galdeano",
"doi-asserted-by": "publisher",
"first-page": "115",
"journal-title": "Ann. Nutr. Metab.",
"key": "ref155",
"volume": "74",
"year": "2019"
},
{
"DOI": "10.1136/gutjnl-2022-327745",
"article-title": "Management of Helicobacter pylori infection: the Maastricht VI/Florence consensus report",
"author": "Malfertheiner",
"doi-asserted-by": "publisher",
"journal-title": "Gut",
"key": "ref156",
"year": "2022"
},
{
"DOI": "10.3920/BM2022.0091",
"article-title": "Impact of Lactobacillus crispatus-containing oral and vaginal probiotics on vaginal health: a randomised double-blind placebo controlled clinical trial",
"author": "Mandar",
"doi-asserted-by": "publisher",
"first-page": "143",
"journal-title": "Benef Microbes.",
"key": "ref157",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.1186/s12934-021-01563-w",
"article-title": "Oral probiotic activities and biosafety of Lactobacillus gasseri HHuMIN D",
"author": "Mann",
"doi-asserted-by": "publisher",
"first-page": "75",
"journal-title": "Microb. Cell Factories",
"key": "ref158",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.1097/01.MIB.0000440815.76627.64",
"article-title": "The commensal bacterium Faecalibacterium prausnitzii is protective in DNBS-induced chronic moderate and severe colitis models",
"author": "Martin",
"doi-asserted-by": "publisher",
"first-page": "417",
"journal-title": "Inflamm. Bowel Dis.",
"key": "ref159",
"volume": "20",
"year": "2014"
},
{
"DOI": "10.1016/j.biotechadv.2013.01.010",
"article-title": "Bacteriocin production by Bifidobacterium spp. a review",
"author": "Martinez",
"doi-asserted-by": "publisher",
"first-page": "482",
"journal-title": "Biotechnol. Adv.",
"key": "ref160",
"volume": "31",
"year": "2013"
},
{
"DOI": "10.1371/journal.pone.0290813",
"article-title": "Higher Bifidobacterium spp. fecal abundance is associated with a lower prevalence of hyperglycemia and cardiovascular risk markers among schoolchildren from Bahia, Brazil",
"author": "Menezes",
"doi-asserted-by": "publisher",
"first-page": "e0290813",
"journal-title": "PLoS One",
"key": "ref161",
"volume": "18",
"year": "2023"
},
{
"DOI": "10.22514/jocpd.2023.014",
"article-title": "Effects of probiotics on preventing caries in preschool children: a systematic review and meta-analysis",
"author": "Meng",
"doi-asserted-by": "publisher",
"first-page": "85",
"journal-title": "J. Clin. Pediatr. Dent.",
"key": "ref162",
"volume": "47",
"year": "2023"
},
{
"DOI": "10.1080/22221751.2020.1746200",
"article-title": "Renin-angiotensin system inhibitors improve the clinical outcomes of COVID-19 patients with hypertension",
"author": "Meng",
"doi-asserted-by": "publisher",
"first-page": "757",
"journal-title": "Emerg. Microbes. Infect.",
"key": "ref163",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.3390/diagnostics11010007",
"article-title": "The role of gut, vaginal, and urinary microbiome in urinary tract infections: from bench to bedside",
"author": "Mestrovic",
"doi-asserted-by": "publisher",
"first-page": "7",
"journal-title": "Diagnostics",
"key": "ref164",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.7759/cureus.37567",
"article-title": "The effects of probiotics on cholesterol levels in patients with metabolic syndrome: a systematic review",
"author": "Momin",
"doi-asserted-by": "publisher",
"first-page": "e37567",
"journal-title": "Cureus.",
"key": "ref165",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.1016/j.biocel.2016.02.004",
"article-title": "TLR-7 agonist attenuates airway reactivity and inflammation through Nrf2-mediated antioxidant protection in a murine model of allergic asthma",
"author": "Nadeem",
"doi-asserted-by": "publisher",
"first-page": "53",
"journal-title": "Int. J. Biochem. Cell Biol.",
"key": "ref166",
"volume": "73",
"year": "2016"
},
{
"DOI": "10.1016/j.phrs.2022.106288",
"article-title": "Beneficial effects of probiotic and synbiotic supplementation on some cardiovascular risk factors among individuals with prediabetes and type 2 diabetes mellitus: a grade-assessed systematic review, meta-analysis, and meta-regression of randomized clinical trials",
"author": "Naseri",
"doi-asserted-by": "publisher",
"first-page": "106288",
"journal-title": "Pharmacol. Res.",
"key": "ref167",
"volume": "182",
"year": "2022"
},
{
"DOI": "10.1186/s12934-020-01426-w",
"article-title": "Postbiotics-parabiotics: the new horizons in microbial biotherapy and functional foods",
"author": "Nataraj",
"doi-asserted-by": "publisher",
"first-page": "168",
"journal-title": "Microb. Cell Factories",
"key": "ref168",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1177/02601060211049631",
"article-title": "Probiotic supplementation: a prospective approach in the treatment of COVID-19",
"author": "Nayebi",
"doi-asserted-by": "publisher",
"first-page": "163",
"journal-title": "Nutr. Health",
"key": "ref169",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.33073/pjm-2020-047",
"article-title": "The effect of Lactobacillus salivarius SGL03 on clinical and microbiological parameters in periodontal patients",
"author": "Nedzi-Gora",
"doi-asserted-by": "publisher",
"first-page": "441",
"journal-title": "Pol. J. Microbiol.",
"key": "ref170",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1111/prd.12382",
"article-title": "Probiotics for periodontal health—current molecular findings",
"author": "Nguyen",
"doi-asserted-by": "publisher",
"first-page": "254",
"journal-title": "Periodontol.",
"key": "ref171",
"volume": "87",
"year": "2021"
},
{
"DOI": "10.3389/fmedt.2022.961569",
"article-title": "Orchestrating the fecal microbiota transplantation: current technological advancements and potential biomedical application",
"author": "Nigam",
"doi-asserted-by": "publisher",
"first-page": "961569",
"journal-title": "Front Med Technol.",
"key": "ref172",
"volume": "4",
"year": "2022"
},
{
"DOI": "10.3390/microorganisms6040107",
"article-title": "Leaky gut, leaky brain?",
"author": "Obrenovich",
"doi-asserted-by": "publisher",
"first-page": "107",
"journal-title": "Microorganisms",
"key": "ref173",
"volume": "6",
"year": "2018"
},
{
"DOI": "10.3390/microorganisms11061449",
"article-title": "Influence of the probiotic L. reuteri on periodontal clinical parameters after nonsurgical treatment: a systematic review",
"author": "Ochoa",
"doi-asserted-by": "publisher",
"first-page": "1449",
"journal-title": "Microorganisms.",
"key": "ref174",
"volume": "11",
"year": "2023"
},
{
"DOI": "10.1158/0008-5472.CAN-13-3501",
"article-title": "Obesity and cancer: a gut microbial connection",
"author": "Ohtani",
"doi-asserted-by": "publisher",
"first-page": "1885",
"journal-title": "Cancer Res.",
"key": "ref175",
"volume": "74",
"year": "2014"
},
{
"DOI": "10.1186/s41232-018-0063-z",
"article-title": "Maintenance of intestinal homeostasis by mucosal barriers",
"author": "Okumura",
"doi-asserted-by": "publisher",
"first-page": "5",
"journal-title": "Inflamm Regener.",
"key": "ref176",
"volume": "38",
"year": "2018"
},
{
"DOI": "10.1038/s41538-020-00078-9",
"article-title": "The potential application of probiotics and prebiotics for the prevention and treatment of COVID-19",
"author": "Olaimat",
"doi-asserted-by": "publisher",
"first-page": "17",
"journal-title": "NPJ Sci. Food",
"key": "ref177",
"volume": "4",
"year": "2020"
},
{
"DOI": "10.1038/nmicrobiol.2017.57",
"article-title": "Next-generation probiotics: the spectrum from probiotics to live biotherapeutics",
"author": "O’Toole",
"doi-asserted-by": "publisher",
"first-page": "17057",
"journal-title": "Nat. Microbiol.",
"key": "ref178",
"volume": "2",
"year": "2017"
},
{
"DOI": "10.1002/bab.2471",
"article-title": "Alleviation of dental caries by use of isolated potential probiotic and its characterization",
"author": "Pallavi",
"doi-asserted-by": "publisher",
"first-page": "1518",
"journal-title": "Biotechnol. Appl. Biochem.",
"key": "ref179",
"volume": "70",
"year": "2023"
},
{
"article-title": "Effects of Lactobacillus on the levels of the NF-N:B and inflammatory mediators in the mouse inflammation model",
"author": "Pan",
"first-page": "686",
"journal-title": "Chin. J. Prev. Vet. Med.",
"key": "ref180",
"volume": "38",
"year": "2016"
},
{
"DOI": "10.3389/fmicb.2015.00058",
"article-title": "Discovering probiotic microorganisms: in vitro, in vivo, genetic and omics approaches",
"author": "Papadimitriou",
"doi-asserted-by": "publisher",
"first-page": "58",
"journal-title": "Front. Microbiol.",
"key": "ref181",
"volume": "6",
"year": "2015"
},
{
"DOI": "10.3390/nu15020331",
"article-title": "Efficacy and safety of MED-01 probiotics on vaginal health: a 12-week, multicenter, randomized, double-blind, placebo-controlled clinical trial",
"author": "Park",
"doi-asserted-by": "publisher",
"first-page": "331",
"journal-title": "Nutrients",
"key": "ref182",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.3390/microorganisms9102066",
"article-title": "Risk factors for gut dysbiosis in early life",
"author": "Parkin",
"doi-asserted-by": "publisher",
"first-page": "2066",
"journal-title": "Microorganisms",
"key": "ref183",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1002/mbo3.1260",
"article-title": "Impact of antibiotics on the human microbiome and consequences for host health",
"author": "Patangia",
"doi-asserted-by": "publisher",
"first-page": "e1260",
"journal-title": "MicrobiologyOpen",
"key": "ref184",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.3390/nu15214490",
"article-title": "Bacillus Subtilis (BG01-4™) improves self-reported symptoms for constipation, indigestion, and dyspepsia: a phase 1/2A randomized controlled trial",
"author": "Patch",
"doi-asserted-by": "publisher",
"first-page": "4490",
"journal-title": "Nutrients",
"key": "ref185",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.7759/cureus.38568",
"article-title": "Comparative evaluation of the inhibitory effect of Lactobacillus rhamnosus on halitosis-causing bacteria: an invitro microbiological study",
"author": "Patil",
"doi-asserted-by": "publisher",
"first-page": "e38568",
"journal-title": "Cureus",
"key": "ref186",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.3390/ijms232415898",
"article-title": "Clinical evidence on the potential beneficial effects of probiotics and prebiotics in cardiovascular disease",
"author": "Pavlidou",
"doi-asserted-by": "publisher",
"first-page": "15898",
"journal-title": "Int. J. Mol. Sci.",
"key": "ref187",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.7759/cureus.20483",
"article-title": "The efficacy of probiotics in the management of Helicobacter pylori: a systematic review",
"author": "Penumetcha",
"doi-asserted-by": "publisher",
"first-page": "e20483",
"journal-title": "Cureus",
"key": "ref188",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.3390/microorganisms9102107",
"article-title": "Current knowledge of the mode of action and immunity mechanisms of LAB-bacteriocins",
"author": "Perez-Ramos",
"doi-asserted-by": "publisher",
"first-page": "2107",
"journal-title": "Microorganisms",
"key": "ref189",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2020.00700",
"article-title": "Microbiome composition and its impact on the development of allergic diseases",
"author": "Peroni",
"doi-asserted-by": "publisher",
"first-page": "700",
"journal-title": "Front. Immunol.",
"key": "ref190",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.3389/fphys.2015.00081",
"article-title": "Lactobacillus species as biomarkers and agents that can promote various aspects of vaginal health",
"author": "Petrova",
"doi-asserted-by": "publisher",
"first-page": "81",
"journal-title": "Front. Physiol.",
"key": "ref191",
"volume": "6",
"year": "2015"
},
{
"DOI": "10.3390/ijms20102534",
"article-title": "Health benefits of heat-killed (tyndallized) probiotics: an overview",
"author": "Pique",
"doi-asserted-by": "publisher",
"first-page": "2534",
"journal-title": "Int. J. Mol. Sci.",
"key": "ref192",
"volume": "20",
"year": "2019"
},
{
"DOI": "10.1155/2017/8416763",
"article-title": "Oxidative stress: harms and benefits for human health",
"author": "Pizzino",
"doi-asserted-by": "publisher",
"first-page": "8416763",
"journal-title": "Oxidative Med. Cell. Longev.",
"key": "ref193",
"volume": "2017",
"year": "2017"
},
{
"DOI": "10.3390/nu9060555",
"article-title": "Evidence of the anti-inflammatory effects of probiotics and synbiotics in intestinal chronic diseases",
"author": "Plaza-Diaz",
"doi-asserted-by": "publisher",
"first-page": "555",
"journal-title": "Nutrients",
"key": "ref194",
"volume": "9",
"year": "2017"
},
{
"DOI": "10.1080/10408398.2020.1821166",
"article-title": "The effects of probiotic/synbiotic supplementation compared to placebo on biomarkers of oxidative stress in adults: a systematic review and meta-analysis of randomized controlled trials",
"author": "Pourrajab",
"doi-asserted-by": "publisher",
"first-page": "490",
"journal-title": "Crit. Rev. Food Sci. Nutr.",
"key": "ref195",
"volume": "62",
"year": "2022"
},
{
"DOI": "10.1016/j.yclnex.2018.10.001",
"article-title": "Evaluation of antimicrobial properties and their substances against pathogenic bacteria in-vitro by probiotic lactobacilli strains isolated from commercial yoghurt",
"author": "Prabhurajeshwar",
"doi-asserted-by": "publisher",
"first-page": "97",
"journal-title": "Clinical Nutrition Experimental",
"key": "ref196",
"volume": "23",
"year": "2019"
},
{
"DOI": "10.1016/j.ajcnut.2022.10.013",
"article-title": "Chronic consumption of probiotics, oats, and apples has differential effects on postprandial bile acid profile and cardiometabolic disease risk markers compared with an isocaloric control (cornflakes): a randomized trial",
"author": "Pushpass",
"doi-asserted-by": "publisher",
"first-page": "252",
"journal-title": "Am. J. Clin. Nutr.",
"key": "ref197",
"volume": "117",
"year": "2023"
},
{
"DOI": "10.3390/microorganisms10122424",
"article-title": "Fecal microbiota transplantation and other gut microbiota manipulation strategies",
"author": "Quaranta",
"doi-asserted-by": "publisher",
"first-page": "2424",
"journal-title": "Microorganisms",
"key": "ref198",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.22092/ARI.2022.359870.2494",
"article-title": "Co-aggregative effect of probiotics bacteria against diarrheal causative bacteria",
"author": "Rashad Hameed",
"doi-asserted-by": "publisher",
"first-page": "831",
"journal-title": "Arch Razi Inst.",
"key": "ref199",
"volume": "78",
"year": "2023"
},
{
"DOI": "10.3389/fphar.2022.1042189",
"article-title": "Gut microbiome and human health: exploring how the probiotic genus Lactobacillus modulate immune responses",
"author": "Rastogi",
"doi-asserted-by": "publisher",
"first-page": "1042189",
"journal-title": "Front. Pharmacol.",
"key": "ref200",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1007/s00394-023-03207-8",
"article-title": "Does probiotic supplementation improve quality of life in mild-to-moderately active ulcerative colitis patients in Jordan? A secondary outcome of the randomized, double-blind, placebo-controlled study",
"author": "Rayyan",
"doi-asserted-by": "publisher",
"first-page": "3069",
"journal-title": "Eur. J. Nutr.",
"key": "ref201",
"volume": "62",
"year": "2023"
},
{
"DOI": "10.1111/j.1574-695X.2001.tb01549.x",
"article-title": "Oral probiotics can resolve urogenital infections",
"author": "Reid",
"doi-asserted-by": "publisher",
"first-page": "49",
"journal-title": "FEMS Immunol. Med. Microbiol.",
"key": "ref202",
"volume": "30",
"year": "2001"
},
{
"DOI": "10.1128/CMR.16.4.658-672.2003",
"article-title": "Potential uses of probiotics in clinical practice",
"author": "Reid",
"doi-asserted-by": "publisher",
"first-page": "658",
"journal-title": "Clin. Microbiol. Rev.",
"key": "ref203",
"volume": "16",
"year": "2003"
},
{
"DOI": "10.1039/c8fo00547h",
"article-title": "Anticancer potential against cervix cancer (HeLa) cell line of probiotic Lactobacillus casei and Lactobacillus paracasei strains isolated from human breast milk",
"author": "Riaz Rajoka",
"doi-asserted-by": "publisher",
"first-page": "2705",
"journal-title": "Food Funct.",
"key": "ref204",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.1021/acsinfecdis.0c00036",
"article-title": "Effects of antibiotic treatment on gut microbiota and how to overcome its negative impacts on human health",
"author": "Ribeiro",
"doi-asserted-by": "publisher",
"first-page": "2544",
"journal-title": "ACS Infect. Dis.",
"key": "ref205",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.1016/j.yrtph.2022.105266",
"article-title": "Considerations for determining safety of probiotics: a USP perspective",
"author": "Roe",
"doi-asserted-by": "publisher",
"first-page": "105266",
"journal-title": "Regul. Toxicol. Pharmacol.",
"key": "ref206",
"volume": "136",
"year": "2022"
},
{
"DOI": "10.1016/j.foodres.2020.109450",
"article-title": "Antiproliferative and apoptotic effects of probiotic whey dairy beverages in human prostate cell lines",
"author": "Rosa",
"doi-asserted-by": "publisher",
"first-page": "109450",
"journal-title": "Food Res. Int.",
"key": "ref207",
"volume": "137",
"year": "2020"
},
{
"DOI": "10.3748/wjg.v29.i14.2078",
"article-title": "Role of prebiotics, probiotics, and synbiotics in management of inflammatory bowel disease: current perspectives",
"author": "Roy",
"doi-asserted-by": "publisher",
"first-page": "2078",
"journal-title": "World J. Gastroenterol.",
"key": "ref208",
"volume": "29",
"year": "2023"
},
{
"DOI": "10.3390/nu15214549",
"article-title": "Effect of Lactobacillus kefiri, in conjunction with PENS T6 and a hypocaloric diet, on weight loss, hypertension and laboratory glycemic and lipid profile",
"author": "Ruiz-Tovar",
"doi-asserted-by": "publisher",
"first-page": "4549",
"journal-title": "Nutrients",
"key": "ref209",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.1016/j.heliyon.2023.e15610",
"article-title": "Beneficial, safety, and antioxidant properties of lactic acid bacteria: a next step in their evaluation as potential probiotics",
"author": "Rwubuzizi",
"doi-asserted-by": "publisher",
"first-page": "e15610",
"journal-title": "Heliyon",
"key": "ref210",
"volume": "9",
"year": "2023"
},
{
"DOI": "10.3390/nu15030709",
"article-title": "Bifidobacterium: host-microbiome interaction and mechanism of action in preventing common gut-microbiota-associated complications in preterm infants: a narrative review",
"author": "Sadeghpour Heravi",
"doi-asserted-by": "publisher",
"first-page": "709",
"journal-title": "Nutrients",
"key": "ref211",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.3390/app11178070",
"article-title": "Probiotics in oral health and disease: a systematic review",
"author": "Saiz",
"doi-asserted-by": "publisher",
"first-page": "8070",
"journal-title": "Appl. Sci.",
"key": "ref212",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.3390/ijerph19137835",
"article-title": "Probiotic monotherapy with Lactobacillus reuteri (Prodentis) as a coadjutant to reduce subgingival dysbiosis in a patient with periodontitis",
"author": "Salinas-Azuceno",
"doi-asserted-by": "publisher",
"first-page": "7835",
"journal-title": "Int. J. Environ. Res. Public Health",
"key": "ref213",
"volume": "19",
"year": "2022"
},
{
"DOI": "10.3390/nu10121949",
"article-title": "Iron supplements containing Lactobacillus Plantarum 299v increase ferric iron and up-regulate the ferric reductase DCYTB in human Caco-2/HT29 MTX co-cultures",
"author": "Sandberg",
"doi-asserted-by": "publisher",
"first-page": "1949",
"journal-title": "Nutrients",
"key": "ref214",
"volume": "10",
"year": "2018"
},
{
"DOI": "10.1111/j.1574-695X.2012.00928.x",
"article-title": "Bacteriocin-producing oral streptococci and inhibition of respiratory pathogens",
"author": "Santagati",
"doi-asserted-by": "publisher",
"first-page": "23",
"journal-title": "FEMS Immunol. Med. Microbiol.",
"key": "ref215",
"volume": "65",
"year": "2012"
},
{
"DOI": "10.3390/nu14173661",
"article-title": "Probiotic as a potential gut microbiome modifier for stroke treatment: a systematic scoping review of in vitro and in vivo studies",
"author": "Savigamin",
"doi-asserted-by": "publisher",
"first-page": "3661",
"journal-title": "Nutrients",
"key": "ref216",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.3389/fncel.2021.785057",
"article-title": "Nuclear factor erythroid-2-related factor 2 signaling in the neuropathophysiology of inherited metabolic disorders",
"author": "Seminotti",
"doi-asserted-by": "publisher",
"first-page": "785057",
"journal-title": "Front. Cell. Neurosci.",
"key": "ref217",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1053/j.gastro.2020.09.057",
"article-title": "The healthy microbiome—what is the definition of a healthy gut microbiome?",
"author": "Shanahan",
"doi-asserted-by": "publisher",
"first-page": "483",
"journal-title": "Gastroenterology",
"key": "ref218",
"volume": "160",
"year": "2021"
},
{
"DOI": "10.1136/esmoopen-2016-000138",
"article-title": "Lactobacillus brevis CD2 lozenges prevent oral mucositis in patients undergoing high dose chemotherapy followed by haematopoietic stem cell transplantation",
"author": "Sharma",
"doi-asserted-by": "publisher",
"first-page": "e000138",
"journal-title": "ESMO Open.",
"key": "ref219",
"volume": "1",
"year": "2017"
},
{
"DOI": "10.1007/s12603-023-1921-1",
"article-title": "Nonfood probiotic, prebiotic, and synbiotic use reduces all-cause and cardiovascular mortality risk in older adults: a population-based cohort study",
"author": "Shen",
"doi-asserted-by": "publisher",
"first-page": "391",
"journal-title": "J. Nutr. Health Aging",
"key": "ref220",
"volume": "27",
"year": "2023"
},
{
"DOI": "10.3390/nu13041225",
"article-title": "Paraprobiotics: a new perspective for functional foods and nutraceuticals",
"author": "Siciliano",
"doi-asserted-by": "publisher",
"first-page": "1225",
"journal-title": "Nutrients",
"key": "ref221",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1016/j.jff.2020.104080",
"article-title": "Probiotics as an alternative antimicrobial therapy: current reality and future directions",
"author": "Silva",
"doi-asserted-by": "publisher",
"first-page": "104080",
"journal-title": "J. Funct. Foods",
"key": "ref222",
"volume": "73",
"year": "2020"
},
{
"DOI": "10.1016/j.nutres.2020.12.014",
"article-title": "Probiotics: a potential immunomodulator in COVID-19 infection management",
"author": "Singh",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Nutr. Res.",
"key": "ref223",
"volume": "87",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2022.1002674",
"article-title": "Probiotics as multifaceted oral vaccines against colon cancer: a review",
"author": "Singh",
"doi-asserted-by": "publisher",
"first-page": "1002674",
"journal-title": "Front. Immunol.",
"key": "ref224",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1097/MOG.0000000000000902",
"article-title": "Probiotics in irritable bowel syndrome and inflammatory bowel disease: review of mechanisms and effectiveness",
"author": "So",
"doi-asserted-by": "publisher",
"first-page": "103",
"journal-title": "Curr. Opin. Gastroenterol.",
"key": "ref225",
"volume": "39",
"year": "2023"
},
{
"DOI": "10.3390/antibiotics9080478",
"article-title": "Lactobacillus plantarum 108 inhibits Streptococcus mutans and Candida albicans mixed-species biofilm formation",
"author": "Srivastava",
"doi-asserted-by": "publisher",
"first-page": "478",
"journal-title": "Antibiotics",
"key": "ref226",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1128/AAC.00539-17",
"article-title": "Anti-influenza activity of a Bacillus subtilis probiotic strain",
"author": "Starosila",
"doi-asserted-by": "publisher",
"first-page": "e00539",
"journal-title": "Antimicrob. Agents Chemother.",
"key": "ref227",
"volume": "61",
"year": "2017"
},
{
"DOI": "10.1016/j.archoralbio.2019.07.002",
"article-title": "Host modulation therapy using anti-inflammatory and antioxidant agents in periodontitis: a review to a clinical translation",
"author": "Sulijaya",
"doi-asserted-by": "publisher",
"first-page": "72",
"journal-title": "Arch. Oral Biol.",
"key": "ref228",
"volume": "105",
"year": "2019"
},
{
"DOI": "10.3389/fsoil.2022.821589",
"article-title": "Microbiome as a key player in sustainable agriculture and human health",
"author": "Suman",
"doi-asserted-by": "publisher",
"first-page": "821589",
"journal-title": "Front. Soil Sci.",
"key": "ref229",
"volume": "2",
"year": "2022"
},
{
"DOI": "10.1007/s12602-019-09559-0",
"article-title": "The effects of probiotic supplementation on clinical symptom, weight loss, glycemic control, lipid and hormonal profiles, biomarkers of inflammation, and oxidative stress in women with polycystic ovary syndrome: a systematic review and meta-analysis of randomized controlled trials",
"author": "Tabrizi",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Probiotics Antimicrob Proteins.",
"key": "ref230",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1136/bmjopen-2020-047069",
"article-title": "Randomised, double-blind, placebo-controlled trial of probiotics to eliminate COVID-19 transmission in exposed household contacts (PROTECT-EHC): a clinical trial protocol",
"author": "Tang",
"doi-asserted-by": "publisher",
"first-page": "e047069",
"journal-title": "BMJ Open",
"key": "ref231",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.3889/oamjms.2022.10733",
"article-title": "Impact of Lactobacillus Reuteri and three other probiotics in Helicobacter pylori eradication. Macedonian",
"author": "Telaku",
"doi-asserted-by": "publisher",
"first-page": "2215",
"journal-title": "J. Med. Sci.",
"key": "ref232",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.3390/microorganisms11081896",
"article-title": "Biologically active compounds from probiotic microorganisms and plant extracts used as biopreservatives",
"author": "Teneva",
"doi-asserted-by": "publisher",
"first-page": "1896",
"journal-title": "Microorganisms",
"key": "ref233",
"volume": "11",
"year": "2023"
},
{
"DOI": "10.1177/15598276211012968",
"article-title": "Dietary modification for the restoration of gut microbiome and management of symptoms in irritable bowel syndrome",
"author": "Thomas",
"doi-asserted-by": "publisher",
"first-page": "608",
"journal-title": "Am. J. Lifestyle Med.",
"key": "ref234",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.3389/fnut.2023.1179432",
"article-title": "Probiotics improve symptoms of patients with COVID-19 through gut-lung axis: a systematic review and meta-analysis",
"author": "Tian",
"doi-asserted-by": "publisher",
"first-page": "1179432",
"journal-title": "Front. Nutr.",
"key": "ref235",
"volume": "10",
"year": "2023"
},
{
"DOI": "10.3389/fmicb.2020.01877",
"article-title": "Probiotics at war against viruses: what is missing from the picture?",
"author": "Tiwari",
"doi-asserted-by": "publisher",
"first-page": "1877",
"journal-title": "Front. Microbiol.",
"key": "ref236",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1002/mc.22274",
"article-title": "Melatonin modulated autophagy and Nrf2 signaling pathways in mice with colitis-associated colon carcinogenesis",
"author": "Trivedi",
"doi-asserted-by": "publisher",
"first-page": "255",
"journal-title": "Mol. Carcinog.",
"key": "ref237",
"volume": "55",
"year": "2016"
},
{
"DOI": "10.1186/s12929-018-0469-6",
"article-title": "H. pylori infection and extra-gastroduodenal diseases",
"author": "Tsay",
"doi-asserted-by": "publisher",
"first-page": "65",
"journal-title": "J. Biomed. Sci.",
"key": "ref238",
"volume": "25",
"year": "2018"
},
{
"DOI": "10.1080/19490976.2020.1831339",
"article-title": "Molecular insights into probiotic mechanisms of action employed against intestinal pathogenic bacteria",
"author": "Van Zyl",
"doi-asserted-by": "publisher",
"first-page": "1831339",
"journal-title": "Gut Microbes",
"key": "ref239",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1080/17474124.2017.1343143",
"article-title": "The intestinal barrier: a fundamental role in health and disease",
"author": "Vancamelbeke",
"doi-asserted-by": "publisher",
"first-page": "821",
"journal-title": "Expert Rev. Gastroenterol. Hepatol.",
"key": "ref240",
"volume": "11",
"year": "2017"
},
{
"DOI": "10.3389/froh.2022.825017",
"article-title": "The evaluation of the effects of two probiotic strains on the oral ecosystem: a randomized clinical trial",
"author": "Volgenant",
"doi-asserted-by": "publisher",
"first-page": "825017",
"journal-title": "Front. Oral Health",
"key": "ref241",
"volume": "3",
"year": "2022"
},
{
"DOI": "10.3390/nu11122938",
"article-title": "A systematic review and meta-analysis on the effects of probiotic species on iron absorption and iron status",
"author": "Vonderheid",
"doi-asserted-by": "publisher",
"first-page": "2938",
"journal-title": "Nutrients",
"key": "ref242",
"volume": "11",
"year": "2019"
},
{
"DOI": "10.3389/fphar.2022.1025860",
"article-title": "The role of the gut microbiota and probiotics associated with microbial metabolisms in cancer prevention and therapy",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "1025860",
"journal-title": "Front. Pharmacol.",
"key": "ref243",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.3389/fcimb.2023.1120789",
"article-title": "Comparative effectiveness of different probiotics supplements for triple Helicobacter pylori eradication: a network meta-analysis",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "1120789",
"journal-title": "Front. Cell. Infect. Microbiol.",
"key": "ref244",
"volume": "13",
"year": ""
},
{
"DOI": "10.3390/nu9050521",
"article-title": "Antioxidant properties of probiotic bacteria",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "521",
"journal-title": "Nutrients",
"key": "ref245",
"volume": "9",
"year": "2017"
},
{
"DOI": "10.3390/molecules26196076",
"article-title": "Probiotics regulate gut microbiota: an effective method to improve immunity",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "6076",
"journal-title": "Molecules",
"key": "ref246",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.1038/s41366-023-01375-5",
"article-title": "Effects of probiotics in patients with morbid obesity undergoing bariatric surgery: a systematic review and meta-analysis",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "1029",
"journal-title": "Int. J. Obes.",
"key": "ref247",
"volume": "47",
"year": ""
},
{
"DOI": "10.1101/2022.01.04.21268275",
"article-title": "Daily Lactobacillus probiotic versus placebo in COVID-19-exposed household contacts (PROTECT-EHC): a randomized clinical trial",
"author": "Wischmeyer",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv",
"key": "ref248",
"year": "2022"
},
{
"DOI": "10.1111/1471-0528.13115",
"article-title": "The vaginal microbiome, vaginal anti-microbial defence mechanisms and the clinical challenge of reducing infection-related preterm birth",
"author": "Witkin",
"doi-asserted-by": "publisher",
"first-page": "213",
"journal-title": "BJOG",
"key": "ref249",
"volume": "122",
"year": "2015"
},
{
"DOI": "10.3390/nu13082878",
"article-title": "Potential benefits of probiotics and prebiotics for coronary heart disease and stroke",
"author": "Wu",
"doi-asserted-by": "publisher",
"first-page": "2878",
"journal-title": "Nutrients",
"key": "ref250",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.3390/ijms19072084",
"article-title": "Beneficial impact and molecular mechanism of Bacillus coagulans on piglets’ intestine",
"author": "Wu",
"doi-asserted-by": "publisher",
"first-page": "2084",
"journal-title": "Int. J. Mol. Sci.",
"key": "ref251",
"volume": "19",
"year": "2018"
},
{
"DOI": "10.1136/gutjnl-2022-328970",
"article-title": "Microbial transmission, colonisation and succession: from pregnancy to infancy",
"author": "Xiao",
"doi-asserted-by": "publisher",
"first-page": "772",
"journal-title": "Gut",
"key": "ref252",
"volume": "72",
"year": "2023"
},
{
"DOI": "10.1007/s00253-021-11646-8",
"article-title": "Probiotics, prebiotics and synbiotics: safe options for next-generation therapeutics",
"author": "Yadav",
"doi-asserted-by": "publisher",
"first-page": "505",
"journal-title": "Appl. Microbiol. Biotechnol.",
"key": "ref253",
"volume": "106",
"year": "2022"
},
{
"DOI": "10.26442/00403660.2022.02.201368",
"article-title": "The effectiveness of a probiotic containing Bifidobacterium longum BB-46 and Enterococcus faecium ENCfa-68 in the treatment of post-infectious irritable bowel syndrome. Prospective randomized comparative study",
"author": "Yakovenko",
"doi-asserted-by": "publisher",
"first-page": "180",
"journal-title": "Ter. Arkh.",
"key": "ref254",
"volume": "94",
"year": "2022"
},
{
"DOI": "10.1186/s13567-022-01042-z",
"article-title": "Oral administration of Lactobacillus brevis 23017 combined with ellagic acid attenuates intestinal inflammatory injury caused by Eimeria infection by activating the Nrf2/HO-1 antioxidant pathway",
"author": "Yang",
"doi-asserted-by": "publisher",
"first-page": "21",
"journal-title": "Vet. Res.",
"key": "ref255",
"volume": "53",
"year": "2022"
},
{
"DOI": "10.3892/mmr.2017.6226",
"article-title": "Effects of probiotics on toll-like receptor expression in ulcerative colitis rats induced by 2,4,6-trinitro-benzene sulfonic acid",
"author": "Yao",
"doi-asserted-by": "publisher",
"first-page": "1973",
"journal-title": "Mol. Med. Rep.",
"key": "ref256",
"volume": "15",
"year": "2017"
},
{
"DOI": "10.1155/2021/8030297",
"article-title": "Bifidobacterium longum: protection against inflammatory bowel disease",
"author": "Yao",
"doi-asserted-by": "publisher",
"first-page": "8030297",
"journal-title": "J Immunol Res",
"key": "ref257",
"volume": "2021",
"year": "2021"
},
{
"DOI": "10.1007/s12602-017-9351-1",
"article-title": "The effect of probiotics on halitosis: a systematic review and Meta-analysis",
"author": "Yoo",
"doi-asserted-by": "publisher",
"first-page": "150",
"journal-title": "Probiotics Antimicrob Proteins.",
"key": "ref258",
"volume": "11",
"year": "2019"
},
{
"DOI": "10.1053/j.gastro.2022.09.040",
"article-title": "Bacteroides vulgatus SNUG 40005 restores Akkermansia depletion by metabolite modulation",
"author": "You",
"doi-asserted-by": "publisher",
"first-page": "103",
"journal-title": "Gastroenterology",
"key": "ref259",
"volume": "164",
"year": "2023"
},
{
"DOI": "10.1159/000504164",
"article-title": "Effects of the consumption of probiotic yogurt containing Bifidobacterium lactis Bb12 on the levels of Streptococcus mutans and lactobacilli in saliva of students with initial stages of dental caries: a double-blind randomized controlled trial",
"author": "Zare Javid",
"doi-asserted-by": "publisher",
"first-page": "68",
"journal-title": "Caries Res.",
"key": "ref260",
"volume": "54",
"year": "2020"
},
{
"DOI": "10.1016/j.numecd.2022.09.005",
"article-title": "Effects of probiotics supplementation on blood pressure: an umbrella meta-analysis of randomized controlled trials",
"author": "Zarezadeh",
"doi-asserted-by": "publisher",
"first-page": "275",
"journal-title": "Nutr. Metab. Cardiovasc. Dis.",
"key": "ref261",
"volume": "33",
"year": "2023"
},
{
"DOI": "10.3390/ijms24032991",
"article-title": "Effect of probiotic Lactobacillus plantarum on Streptococcus mutans and Candida albicans clinical isolates from children with early childhood caries",
"author": "Zeng",
"doi-asserted-by": "publisher",
"first-page": "2991",
"journal-title": "Int. J. Mol. Sci.",
"key": "ref262",
"volume": "24",
"year": "2023"
},
{
"DOI": "10.3389/fcimb.2022.806463",
"article-title": "Probiotic species in the management of periodontal diseases: an overview",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "806463",
"journal-title": "Front. Cell. Infect. Microbiol.",
"key": "ref263",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1155/2022/5633403",
"article-title": "Next-generation probiotics: microflora intervention to human diseases",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "5633403",
"journal-title": "Biomed. Res. Int.",
"key": "ref264",
"volume": "2022",
"year": "2022"
},
{
"DOI": "10.3390/antiox12030769",
"article-title": "Recent perspective of Lactobacillus in reducing oxidative stress to prevent disease",
"author": "Zhao",
"doi-asserted-by": "publisher",
"first-page": "769",
"journal-title": "Antioxidants (Basel).",
"key": "ref265",
"volume": "12",
"year": "2023"
},
{
"DOI": "10.3390/ijms231911162",
"article-title": "Lactobacillus rhamnosus CY12 enhances intestinal barrier function by regulating tight junction protein expression, oxidative stress, and inflammation response in lipopolysaccharide-induced Caco-2 cells",
"author": "Zheng",
"doi-asserted-by": "publisher",
"first-page": "11162",
"journal-title": "IJMS",
"key": "ref266",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.1155/2019/6079734",
"article-title": "Lactobacillus iners is associated with vaginal Dysbiosis in healthy pregnant women: a preliminary study",
"author": "Zheng",
"doi-asserted-by": "publisher",
"first-page": "6079734",
"journal-title": "Biomed. Res. Int.",
"key": "ref267",
"volume": "2019",
"year": "2019"
},
{
"DOI": "10.3389/fnut.2023.1196625",
"article-title": "Effect of a probiotic formula on gastrointestinal health, immune responses and metabolic health in adults with functional constipation or functional diarrhea",
"author": "Zheng",
"doi-asserted-by": "publisher",
"first-page": "1196625",
"journal-title": "Front. Nutr.",
"key": "ref268",
"volume": "10",
"year": ""
},
{
"DOI": "10.3389/fimmu.2023.1143548",
"article-title": "Probiotics fortify intestinal barrier function: a systematic review and meta-analysis of randomized trials",
"author": "Zheng",
"doi-asserted-by": "publisher",
"first-page": "1143548",
"journal-title": "Front. Immun.",
"key": "ref269",
"volume": "14",
"year": ""
},
{
"DOI": "10.1371/journal.pone.0278356",
"article-title": "Safety and efficacy of probiotic supplements as adjunctive therapies in patients with COVID-19: a systematic review and meta-analysis",
"author": "Zhu",
"doi-asserted-by": "publisher",
"first-page": "e0278356",
"journal-title": "PLoS One",
"key": "ref270",
"volume": "18",
"year": "2023"
},
{
"DOI": "10.1007/s13238-010-0093-z",
"article-title": "Human gut microbiome: the second genome of human body",
"author": "Zhu",
"doi-asserted-by": "publisher",
"first-page": "718",
"journal-title": "Protein Cell",
"key": "ref271",
"volume": "1",
"year": "2010"
},
{
"DOI": "10.1155/2018/5063185",
"article-title": "Food-origin lactic acid bacteria may exhibit probiotic properties: review",
"author": "Zielinska",
"doi-asserted-by": "publisher",
"first-page": "5063185",
"journal-title": "Biomed. Res. Int.",
"key": "ref272",
"volume": "2018",
"year": "2018"
}
],
"reference-count": 272,
"references-count": 272,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fmicb.2023.1296447/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Microbiology (medical)",
"Microbiology"
],
"subtitle": [],
"title": "Role of probiotics in managing various human diseases, from oral pathology to cancer and gastrointestinal diseases",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "14"
}
