COVID-19 and Lactoferrin: A Systematic Review and Meta-Analysis
et al., COVID, doi:10.3390/covid5100176, Oct 2025
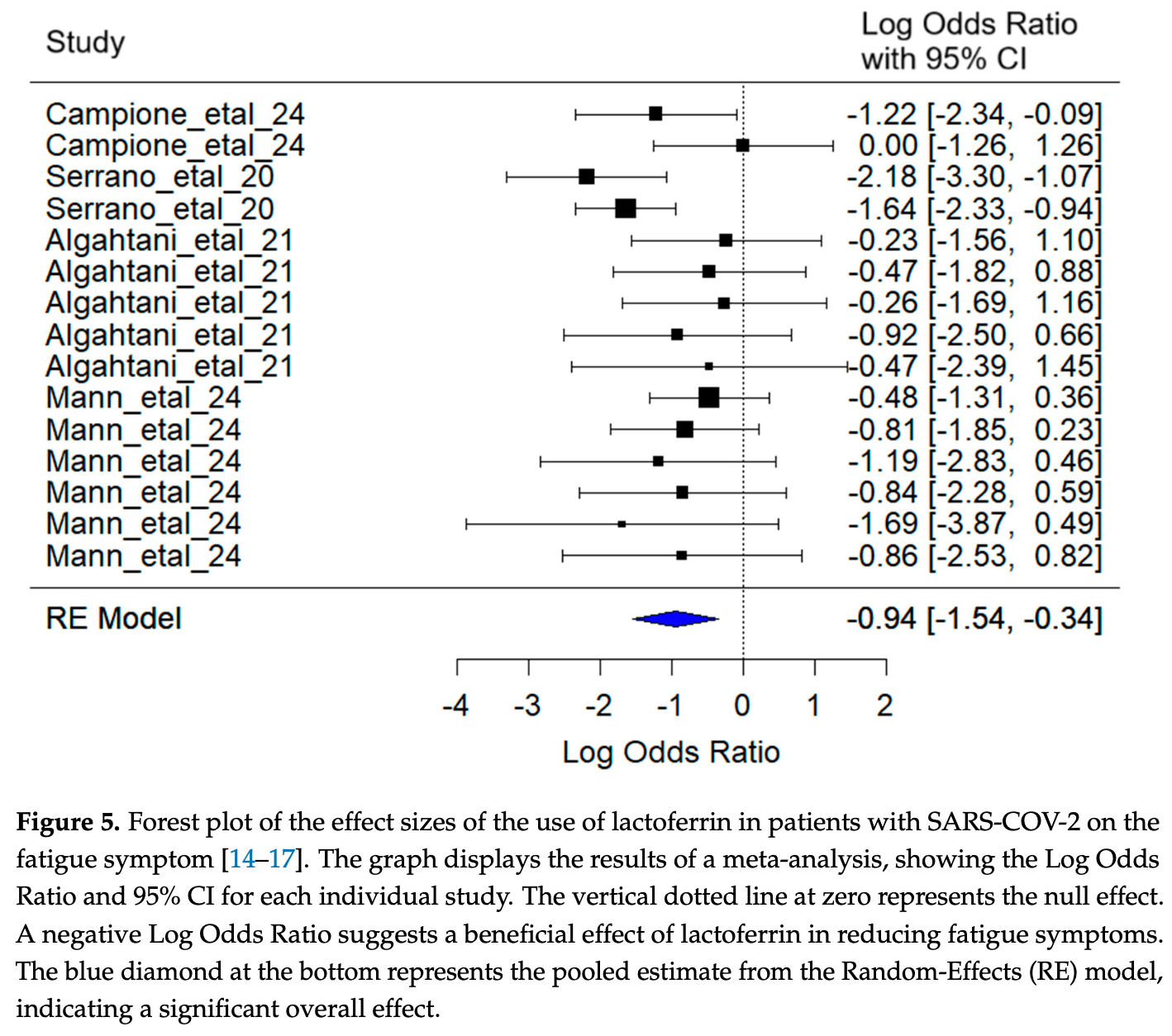
Systematic review and meta-analysis of lactoferrin studies for COVID-19. Authors found that lactoferrin demonstrated a significant effect in reducing fatigue among COVID-19 patients. While trends toward improvement were observed for other symptoms including headache and anosmia/ageusia, these did not reach statistical significance.
Currently there are 8 lactoferrin studies and meta-analysis shows:
| Outcome | Improvement |
|---|---|
| Mortality | 17% lower [-161‑73%] |
| Ventilation | 45% higher [-35‑220%] |
| Hospitalization | 61% lower [-164‑94%] |
| Cases | 36% more [-42‑218%] |
1.
Palacios-Rosas et al., COVID-19 and Lactoferrin: A Systematic Review and Meta-Analysis, COVID, doi:10.3390/covid5100176.
2.
Eker et al., The potential of lactoferrin as antiviral and immune-modulating agent in viral infectious diseases, Frontiers in Immunology, doi:10.3389/fimmu.2024.1402135.
3.
Manzoni et al., Lactoferrin Supplementation in Preventing and Protecting from SARS-CoV-2 Infection: Is There Any Role in General and Special Populations? An Updated Review of Literature, International Journal of Molecular Sciences, doi:10.3390/ijms251910248.
4.
Rosa et al., An overview on in vitro and in vivo antiviral activity of lactoferrin: its efficacy against SARS-CoV-2 infection, BioMetals, doi:10.1007/s10534-022-00427-z.
5.
Mattar et al., Natural resources to control COVID-19: could lactoferrin amend SARS-CoV-2 infectivity?, PeerJ, doi:10.7717/peerj.11303.
Palacios-Rosas et al., 16 Oct 2025, peer-reviewed, 7 authors.
Contact: adriana.palacios@udlap.mx (corresponding author), erika.palacios@udlap.mx, zabdi.perezua@udlap.mx, eduardo.lopezlz@udlap.mx, anas.garciamo@udlap.mx, talmughanam@kfu.edu.sa, mcuautle2004@gmail.com.
COVID-19 and Lactoferrin: A Systematic Review and Meta-Analysis
COVID, doi:10.3390/covid5100176
To analyze the relationship between lactoferrin and COVID-19, a systematic review and meta-analysis of works published between 2020 and 2025 was carried out. The search strategy consisted of compiling research and review articles with the keywords COVID-19 and lactoferrin, COVID-19 and lactoferrin, SARS-COV-2 and lactoferrin, and SARS-COV-2 and lactoferrin in the databases of the search engines Elsevier, PubMed, and Google Scholar. In addition, these were classified depending on the type of study (e.g., in vivo, in vitro, both, or neither). PRISMA was used to perform a systematic review and meta-analysis. A total of 1531 articles were found, of which any duplicates were discarded, leaving 1234. A second database was created for strictly research and in vivo type articles, obtaining only 69 articles. Lactoferrin demonstrated a significant effect in reducing fatigue among COVID-19 patients, contributing to improved recovery and functional status-particularly in individuals with post-acute COVID-19 syndrome. However, its impact on other symptoms did not reach statistical significance.
Abbreviations The
References
Algahtani, Elabbasy, Samak, Adeboye, Yusuf et al., The Prospect of Lactoferrin Use as Adjunctive Agent in Management of SARS-CoV-2 Patients: A Randomized Pilot Study, Medicina, doi:10.3390/medicina57080842
Ali, Hasan, Kow, Merchant, Lactoferrin Reduces the Risk of Respiratory Tract Infections: A Meta-Analysis of Randomized Controlled Trials, Clin. Nutr. ESPEN, doi:10.1016/j.clnesp.2021.08.019
Andreu, Ripa, Bello-Morales, López-Guerrero, Liposomal Lactoferrin Exerts Antiviral Activity against HCoV-229E and SARS-CoV-2 Pseudoviruses In Vitro, Viruses, doi:10.3390/v15040972
Berthon, Williams, Williams, Wood, Effect of Lactoferrin Supplementation on Inflammation, Immune Function, and Prevention of Respiratory Tract Infections in Humans: A Systematic Review and Meta-Analysis, Adv. Nutr, doi:10.1093/advances/nmac047
Bhandari, Phatak, Pawar, Khobarkar, Nakanekar, Add On Effect of Indian Breed A2 Cow Milk Colostrum Tablet (Gopiyush) in Management of COVID-19: An Observational Study (Case Series), Ann. Ayurvedic Med, doi:10.5455/AAM.3770
Campione, Lanna, Cosio, Rosa, Conte et al., Lactoferrin as Antiviral Treatment in COVID-19 Management: Preliminary Evidence, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph182010985
Cao, Ren, Lu, Wang, Wu et al., Lactoferrin: A Glycoprotein That Plays an Active Role in Human Health, Front. Nutr, doi:10.3389/fnut.2022.1018336
Carfì, Bernabei, Landi, for the Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients after Acute COVID-19, JAMA, doi:10.1001/jama.2020.12603
Coccolini, Berselli, Blanco-Llamero, Fathi, Oliveira et al., Biomedical and nutritional applications of lactoferrin, Int. J. Pept. Res. Ther, doi:10.1007/s10989-023-10541-2
Cutone, Rosa, Lepanto, Scotti, Berlutti et al., Lactoferrin Efficiently Counteracts the Inflammation-Induced Changes of the Iron Homeostasis System in Macrophages, Front. Immunol, doi:10.3389/fimmu.2017.00705
Fijałkowski, Pomastowski, Van Eldik, Rafi Ńska, Multifunctional role of Lactoferrin in metal ion interactions and biomedical applications: A review, Int. J. Biol. Macromol, doi:10.1016/j.ijbiomac.2025.146531
Kowalczyk, Kaczy Ńska, Kleczkowska, Bukowska-Ośko, Kramkowski et al., The Lactoferrin Phenomenon-A Miracle Molecule, Molecules, doi:10.3390/molecules27092941
Legrand, Elass, Carpentier, Mazurier, Interactions of Lactoferrin with Cells Involved in Immune Function, Biochem. Cell Biol, doi:10.1139/o06-045
Lepanto, Rosa, Paesano, Valenti, Cutone, Lactoferrin in Aseptic and Septic Inflammation, Molecules, doi:10.3390/molecules24071323
Mann, Reddy, Van Der Stok, Ngubane, Mulaudzi et al., Hen Egg White Bovine Colostrum Supplement Reduces Symptoms of Mild/Moderate COVID-19: A Randomized Control Trial, Future Sci, doi:10.2144/fsoa-2023-0024
Mariani, Rainaldi, Dall'ara, De Rose, Morello et al., Persisting Gastrointestinal Symptoms in Children with SARS-CoV-2: Temporal Evolution over 18 Months and Possible Role of Lactoferrin, Children, doi:10.3390/children11010105
Matino, Tavella, Rizzi, Avanzi, Azzolina et al., Effect of Lactoferrin on Clinical Outcomes of Hospitalized Patients with COVID-19: The LAC Randomized Clinical Trial, Nutrients, doi:10.3390/nu15051285
Mitra, Zhang, Expression of human lactoferrin cDNA in tobacco cells produces antibacterial protein(s), Plant Physiol, doi:10.1104/pp.106.3.977
Nalbandian, Sehgal, Gupta, Madhavan, Mcgroder et al., Post-Acute COVID-19 Syndrome, Nat. Med, doi:10.1038/s41591-021-01283-z
Paesano, Berlutti, Pietropaoli, Pantanella, Pacifici et al., Lactoferrin Efficacy versus Ferrous Sulfate in Curing Iron Deficiency and Iron Deficiency Anemia in Pregnant Women, Biometals, doi:10.1007/s10534-010-9335-z
Proal, Vanelzakker, Long COVID or Post-Acute Sequelae of COVID-19 (PASC): An Overview of Biological Factors That May Contribute to Persistent Symptoms, Front. Microbiol, doi:10.3389/fmicb.2021.698169
Redel, Miry, Hellemons, Oswald, Braunstahl, Effect of lactoferrin treatment on symptoms and physical performance in long COVID patients: A randomised, double-blind, placebo-controlled trial, ERJ Open Res, doi:10.1183/23120541.00031-2024
Rodwal, Shinwari, Naizi, Sherzad, Marappan, Lactoferrin: Structure, biological functions as functional food and maintaining health, Funct. Food Sci.-Online, doi:10.31989/ffs.v4i12.1407
Rosa, Tripepi, Naldi, Aimati, Santangeli et al., Ambulatory COVID-19 Patients Treated with Lactoferrin as a Supplementary Antiviral Agent: A Preliminary Study, J. Clin. Med, doi:10.3390/jcm10184276
Rümke, Visser, Kwa, Hart, Radio-immuno assay of lactoferrin in blood plasma of breast cancer patients, lactating and normal women; prevention of false high levels caused by leakage from neutrophile leucocytes in vitro, Folia Medica Neerl
Serrano, Kochergina, Albors, Díaz, Liposomal Lactoferrin as Potential Preventative and Cure for COVID-19, Int. J. Res. Health Sci, doi:10.5530/ijrhs.8.1.3
Townsend, Dyer, Jones, Dunne, Mooney et al., Persistent Fatigue Following SARS-CoV-2 Infection Is Common and Independent of Severity of Initial Infection, PLoS ONE, doi:10.1371/journal.pone.0240784
Uesaki, Imanaka, Suido, Suwa, Effects of lactoferrin supplementation on sleep quality, mood states, and enteric environment in poor sleepers: Randomized, placebo-controlled, double-blind study, Jpn. Pharmacol. Ther
Valenti, Antonini, Lactoferrin: An Important Host Defence against Microbial and Viral Attack, Cell. Mol. Life Sci, doi:10.1007/s00018-005-5372-0
Van Berkel, Welling, Geerts, Van Veen, Ravensbergen et al., Large scale production of recombinant human lactoferrin in the milk of transgenic cows, Nat. Biotechnol, doi:10.1038/nbt0502-484
Vélez-Santamaría, Fernández-Solana, Méndez-López, Domínguez-García, González-Bernal et al., Functionality, Physical Activity, Fatigue and Quality of Life in Patients with Acute COVID-19 and Long COVID Infection, Sci. Rep, doi:10.1038/s41598-023-47218-1
Walker, Goodfellow, Pookarnjanamorakot, Murray, Bindman et al., Impact of Fatigue as the Primary Determinant of Functional Limitations among Patients with Post-COVID-19 Syndrome: A Cross-Sectional Observational Study, BMJ Open, doi:10.1136/bmjopen-2022-069217
DOI record:
{
"DOI": "10.3390/covid5100176",
"ISSN": [
"2673-8112"
],
"URL": "http://dx.doi.org/10.3390/covid5100176",
"abstract": "<jats:p>To analyze the relationship between lactoferrin and COVID-19, a systematic review and meta-analysis of works published between 2020 and 2025 was carried out. The search strategy consisted of compiling research and review articles with the keywords COVID-19 and lactoferrin, COVID-19 and lactoferrin, SARS-COV-2 and lactoferrin, and SARS-COV-2 and lactoferrin in the databases of the search engines Elsevier, PubMed, and Google Scholar. In addition, these were classified depending on the type of study (e.g., in vivo, in vitro, both, or neither). PRISMA was used to perform a systematic review and meta-analysis. A total of 1531 articles were found, of which any duplicates were discarded, leaving 1234. A second database was created for strictly research and in vivo type articles, obtaining only 69 articles. Lactoferrin demonstrated a significant effect in reducing fatigue among COVID-19 patients, contributing to improved recovery and functional status—particularly in individuals with post-acute COVID-19 syndrome. However, its impact on other symptoms did not reach statistical significance.</jats:p>",
"alternative-id": [
"covid5100176"
],
"author": [
{
"ORCID": "https://orcid.org/0000-0001-8983-5781",
"affiliation": [
{
"name": "Health Sciences Department, Universidad de las Américas Puebla, Puebla 72810, Mexico"
}
],
"authenticated-orcid": false,
"family": "Palacios-Rosas",
"given": "Erika",
"sequence": "first"
},
{
"ORCID": "https://orcid.org/0000-0002-6972-5988",
"affiliation": [
{
"name": "Chemical, Food, and Environmental Engineering Department, Universidad de las Américas Puebla, Puebla 72810, Mexico"
}
],
"authenticated-orcid": false,
"family": "Palacios",
"given": "Adriana",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Biological Sciences Research Center, Universidad Autónoma de Tlaxcala, Tlaxcala 90120, Mexico"
}
],
"family": "Cuautle",
"given": "Mariana",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Mechanical Engineering, College of Engineering, King Faisal University, Al-Ahsa 31982, Saudi Arabia"
}
],
"family": "Abdulaziz-Almughanam",
"given": "Tawfiq",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Chemical, Food, and Environmental Engineering Department, Universidad de las Américas Puebla, Puebla 72810, Mexico"
}
],
"family": "Pérez-Urquieta",
"given": "Zabdi Paulina",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Chemical, Food, and Environmental Engineering Department, Universidad de las Américas Puebla, Puebla 72810, Mexico"
}
],
"family": "López-López",
"given": "Eduardo Alejandro",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Chemical, Food, and Environmental Engineering Department, Universidad de las Américas Puebla, Puebla 72810, Mexico"
}
],
"family": "García-Montejano",
"given": "Ana Sofía",
"sequence": "additional"
}
],
"container-title": "COVID",
"container-title-short": "COVID",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2025,
10,
16
]
],
"date-time": "2025-10-16T16:33:22Z",
"timestamp": 1760632402000
},
"deposited": {
"date-parts": [
[
2025,
10,
18
]
],
"date-time": "2025-10-18T04:27:36Z",
"timestamp": 1760761656000
},
"funder": [
{
"award": [
"KFU250157"
],
"name": "King Faisal University"
}
],
"indexed": {
"date-parts": [
[
2025,
10,
18
]
],
"date-time": "2025-10-18T04:41:34Z",
"timestamp": 1760762494678,
"version": "build-2065373602"
},
"is-referenced-by-count": 0,
"issue": "10",
"issued": {
"date-parts": [
[
2025,
10,
16
]
]
},
"journal-issue": {
"issue": "10",
"published-online": {
"date-parts": [
[
2025,
10
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
10,
16
]
],
"date-time": "2025-10-16T00:00:00Z",
"timestamp": 1760572800000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2673-8112/5/10/176/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "176",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2025,
10,
16
]
]
},
"published-online": {
"date-parts": [
[
2025,
10,
16
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.3390/molecules27092941",
"doi-asserted-by": "crossref",
"key": "ref_1",
"unstructured": "Kowalczyk, P., Kaczyńska, K., Kleczkowska, P., Bukowska-Ośko, I., Kramkowski, K., and Sulejczak, D. (2022). The Lactoferrin Phenomenon-A Miracle Molecule. Molecules, 27."
},
{
"DOI": "10.1007/s10989-023-10541-2",
"article-title": "Biomedical and nutritional applications of lactoferrin",
"author": "Coccolini",
"doi-asserted-by": "crossref",
"first-page": "71",
"journal-title": "Int. J. Pept. Res. Ther.",
"key": "ref_2",
"volume": "29",
"year": "2023"
},
{
"DOI": "10.1016/j.ijbiomac.2025.146531",
"doi-asserted-by": "crossref",
"key": "ref_3",
"unstructured": "Fijałkowski, P., Pomastowski, P., van Eldik, R., and Rafińska, K. (2025). Multifunctional role of Lactoferrin in metal ion interactions and biomedical applications: A review. Int. J. Biol. Macromol., 321."
},
{
"article-title": "Lactoferrin: Structure, biological functions as functional food and maintaining health",
"author": "Rodwal",
"first-page": "495",
"journal-title": "Funct. Food Sci.-Online",
"key": "ref_4",
"volume": "4",
"year": "2024"
},
{
"DOI": "10.3389/fnut.2022.1018336",
"doi-asserted-by": "crossref",
"key": "ref_5",
"unstructured": "Cao, X., Ren, Y., Lu, Q., Wang, K., Wu, Y., Wang, Y., Zhang, Y., Cui, X., Yang, Z., and Chen, Z. (2023). Lactoferrin: A Glycoprotein That Plays an Active Role in Human Health. Front. Nutr., 9."
},
{
"article-title": "Radio-immuno assay of lactoferrin in blood plasma of breast cancer patients, lactating and normal women; prevention of false high levels caused by leakage from neutrophile leucocytes in vitro",
"author": "Visser",
"first-page": "156",
"journal-title": "Folia Medica Neerl.",
"key": "ref_6",
"volume": "14",
"year": "1971"
},
{
"DOI": "10.1104/pp.106.3.977",
"article-title": "Expression of human lactoferrin cDNA in tobacco cells produces antibacterial protein(s)",
"author": "Mitra",
"doi-asserted-by": "crossref",
"first-page": "977",
"journal-title": "Plant Physiol.",
"key": "ref_7",
"volume": "106",
"year": "1994"
},
{
"DOI": "10.1038/nbt0502-484",
"article-title": "Large scale production of recombinant human lactoferrin in the milk of transgenic cows",
"author": "Welling",
"doi-asserted-by": "crossref",
"first-page": "484",
"journal-title": "Nat. Biotechnol.",
"key": "ref_8",
"volume": "20",
"year": "2002"
},
{
"key": "ref_9",
"unstructured": "Johns Hopkins University of Medicine (2025, January 13). COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Coronavirus Resource Center. Available online: https://coronavirus.jhu.edu/map.html."
},
{
"DOI": "10.3390/v15040972",
"doi-asserted-by": "crossref",
"key": "ref_10",
"unstructured": "Andreu, S., Ripa, I., Bello-Morales, R., and López-Guerrero, J.A. (2023). Liposomal Lactoferrin Exerts Antiviral Activity against HCoV-229E and SARS-CoV-2 Pseudoviruses In Vitro. Viruses, 15."
},
{
"DOI": "10.1016/j.clnesp.2021.08.019",
"article-title": "Lactoferrin Reduces the Risk of Respiratory Tract Infections: A Meta-Analysis of Randomized Controlled Trials",
"author": "Ali",
"doi-asserted-by": "crossref",
"first-page": "26",
"journal-title": "Clin. Nutr. ESPEN.",
"key": "ref_11",
"volume": "45",
"year": "2021"
},
{
"DOI": "10.1093/advances/nmac047",
"article-title": "Effect of Lactoferrin Supplementation on Inflammation, Immune Function, and Prevention of Respiratory Tract Infections in Humans: A Systematic Review and Meta-Analysis",
"author": "Berthon",
"doi-asserted-by": "crossref",
"first-page": "1799",
"journal-title": "Adv. Nutr.",
"key": "ref_12",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.3390/nu15051285",
"doi-asserted-by": "crossref",
"key": "ref_13",
"unstructured": "Matino, E., Tavella, E., Rizzi, M., Avanzi, G., Azzolina, D., Battaglia, A., Becco, P., Bellan, M., Bertinieri, G., and Bertoletti, M. (2023). Effect of Lactoferrin on Clinical Outcomes of Hospitalized Patients with COVID-19: The LAC Randomized Clinical Trial. Nutrients, 15."
},
{
"DOI": "10.3390/ijerph182010985",
"doi-asserted-by": "crossref",
"key": "ref_14",
"unstructured": "Campione, E., Lanna, C., Cosio, T., Rosa, L., Conte, M.P., Iacovelli, F., Romeo, A., Falconi, M., Del Vecchio, C., and Franchin, E. (2021). Lactoferrin as Antiviral Treatment in COVID-19 Management: Preliminary Evidence. Int. J. Environ. Res. Public Health, 18."
},
{
"article-title": "Liposomal Lactoferrin as Potential Preventative and Cure for COVID-19",
"author": "Serrano",
"first-page": "8",
"journal-title": "Int. J. Res. Health Sci.",
"key": "ref_15",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.3390/medicina57080842",
"doi-asserted-by": "crossref",
"key": "ref_16",
"unstructured": "Algahtani, F.D., Elabbasy, M.T., Samak, M.A., Adeboye, A.A., Yusuf, R.A., and Ghoniem, M.E. (2021). The Prospect of Lactoferrin Use as Adjunctive Agent in Management of SARS-CoV-2 Patients: A Randomized Pilot Study. Medicina, 57."
},
{
"DOI": "10.2144/fsoa-2023-0024",
"article-title": "Hen Egg White Bovine Colostrum Supplement Reduces Symptoms of Mild/Moderate COVID-19: A Randomized Control Trial",
"author": "Mann",
"doi-asserted-by": "crossref",
"first-page": "FSO882",
"journal-title": "Future Sci. OA",
"key": "ref_17",
"volume": "9",
"year": "2023"
},
{
"article-title": "Add On Effect of Indian Breed A2 Cow Milk Colostrum Tablet (Gopiyush) in Management of COVID-19: An Observational Study (Case Series)",
"author": "Bhandari",
"first-page": "80",
"journal-title": "Ann. Ayurvedic Med.",
"key": "ref_18",
"volume": "12",
"year": "2023"
},
{
"DOI": "10.3390/children11010105",
"doi-asserted-by": "crossref",
"key": "ref_19",
"unstructured": "Mariani, F., Rainaldi, S., Dall’Ara, G., De Rose, C., Morello, R., and Buonsenso, D. (2024). Persisting Gastrointestinal Symptoms in Children with SARS-CoV-2: Temporal Evolution over 18 Months and Possible Role of Lactoferrin. Children, 11."
},
{
"DOI": "10.3390/jcm10184276",
"doi-asserted-by": "crossref",
"key": "ref_20",
"unstructured": "Rosa, L., Tripepi, G., Naldi, E., Aimati, M., Santangeli, S., Venditto, F., Caldarelli, M., and Valenti, P. (2021). Ambulatory COVID-19 Patients Treated with Lactoferrin as a Supplementary Antiviral Agent: A Preliminary Study. J. Clin. Med., 10."
},
{
"DOI": "10.1183/23120541.00031-2024",
"article-title": "Effect of lactoferrin treatment on symptoms and physical performance in long COVID patients: A randomised, double-blind, placebo-controlled trial",
"author": "Redel",
"doi-asserted-by": "crossref",
"first-page": "00031",
"journal-title": "ERJ Open Res.",
"key": "ref_21",
"volume": "10",
"year": "2024"
},
{
"DOI": "10.1007/s10534-010-9335-z",
"article-title": "Lactoferrin Efficacy versus Ferrous Sulfate in Curing Iron Deficiency and Iron Deficiency Anemia in Pregnant Women",
"author": "Paesano",
"doi-asserted-by": "crossref",
"first-page": "411",
"journal-title": "Biometals",
"key": "ref_22",
"volume": "23",
"year": "2010"
},
{
"DOI": "10.3390/molecules24071323",
"doi-asserted-by": "crossref",
"key": "ref_23",
"unstructured": "Lepanto, M.S., Rosa, L., Paesano, R., Valenti, P., and Cutone, A. (2017). Lactoferrin in Aseptic and Septic Inflammation. Molecules, 24."
},
{
"DOI": "10.1038/s41591-021-01283-z",
"article-title": "Post-Acute COVID-19 Syndrome",
"author": "Nalbandian",
"doi-asserted-by": "crossref",
"first-page": "601",
"journal-title": "Nat. Med.",
"key": "ref_24",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.3389/fmicb.2021.698169",
"doi-asserted-by": "crossref",
"key": "ref_25",
"unstructured": "Proal, A., and VanElzakker, M. (2021). Long COVID or Post-Acute Sequelae of COVID-19 (PASC): An Overview of Biological Factors That May Contribute to Persistent Symptoms. Front. Microbiol., 12."
},
{
"DOI": "10.1001/jama.2020.12603",
"article-title": "for the Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients after Acute COVID-19",
"author": "Bernabei",
"doi-asserted-by": "crossref",
"first-page": "603",
"journal-title": "JAMA",
"key": "ref_26",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1139/o06-045",
"article-title": "Interactions of Lactoferrin with Cells Involved in Immune Function",
"author": "Legrand",
"doi-asserted-by": "crossref",
"first-page": "282",
"journal-title": "Biochem. Cell Biol.",
"key": "ref_27",
"volume": "84",
"year": "2006"
},
{
"DOI": "10.1007/s00018-005-5372-0",
"article-title": "Lactoferrin: An Important Host Defence against Microbial and Viral Attack",
"author": "Valenti",
"doi-asserted-by": "crossref",
"first-page": "2576",
"journal-title": "Cell. Mol. Life Sci.",
"key": "ref_28",
"volume": "62",
"year": "2005"
},
{
"DOI": "10.3389/fimmu.2017.00705",
"doi-asserted-by": "crossref",
"key": "ref_29",
"unstructured": "Cutone, A., Rosa, L., Lepanto, M.S., Scotti, M.J., Berlutti, F., Bonaccorsi di Patti, M.C., Musci, G., and Valenti, P. (2019). Lactoferrin Efficiently Counteracts the Inflammation-Induced Changes of the Iron Homeostasis System in Macrophages. Front. Immunol., 8."
},
{
"DOI": "10.1101/2020.07.29.20164293",
"doi-asserted-by": "crossref",
"key": "ref_30",
"unstructured": "Townsend, L., Dyer, A.H., Jones, K., Dunne, J., Mooney, A., Gaffney, F., O’Connor, L., Leavy, D., O’Brien, K., and Dowds, J. (2020). Persistent Fatigue Following SARS-CoV-2 Infection Is Common and Independent of Severity of Initial Infection. PLoS ONE, 15."
},
{
"DOI": "10.1136/bmjopen-2022-069217",
"article-title": "Impact of Fatigue as the Primary Determinant of Functional Limitations among Patients with Post-COVID-19 Syndrome: A Cross-Sectional Observational Study",
"author": "Walker",
"doi-asserted-by": "crossref",
"first-page": "e069217",
"journal-title": "BMJ Open",
"key": "ref_31",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1038/s41598-023-47218-1",
"doi-asserted-by": "crossref",
"key": "ref_32",
"unstructured": "Vélez-Santamaría, R., Fernández-Solana, J., Méndez-López, F., Domínguez-García, M., González-Bernal, J.J., Magallón-Botaya, R., Oliván-Blázquez, B., González-Santos, J., and Santamaría-Peláez, M. (2023). Functionality, Physical Activity, Fatigue and Quality of Life in Patients with Acute COVID—19 and Long COVID Infection. Sci. Rep., 13."
},
{
"article-title": "Effects of lactoferrin supplementation on sleep quality, mood states, and enteric environment in poor sleepers: Randomized, placebo-controlled, double-blind study",
"author": "Uesaki",
"first-page": "43",
"journal-title": "Jpn. Pharmacol. Ther.",
"key": "ref_33",
"volume": "46",
"year": "2018"
}
],
"reference-count": 33,
"references-count": 33,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2673-8112/5/10/176"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "COVID-19 and Lactoferrin: A Systematic Review and Meta-Analysis",
"type": "journal-article",
"update-policy": "https://doi.org/10.3390/mdpi_crossmark_policy",
"volume": "5"
}