Glucose-lowering drugs and outcome from COVID-19 among patients with type 2 diabetes mellitus: a population-wide analysis in Hong Kong
et al., BMJ Open, doi:10.1136/bmjopen-2021-052310, Oct 2021
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
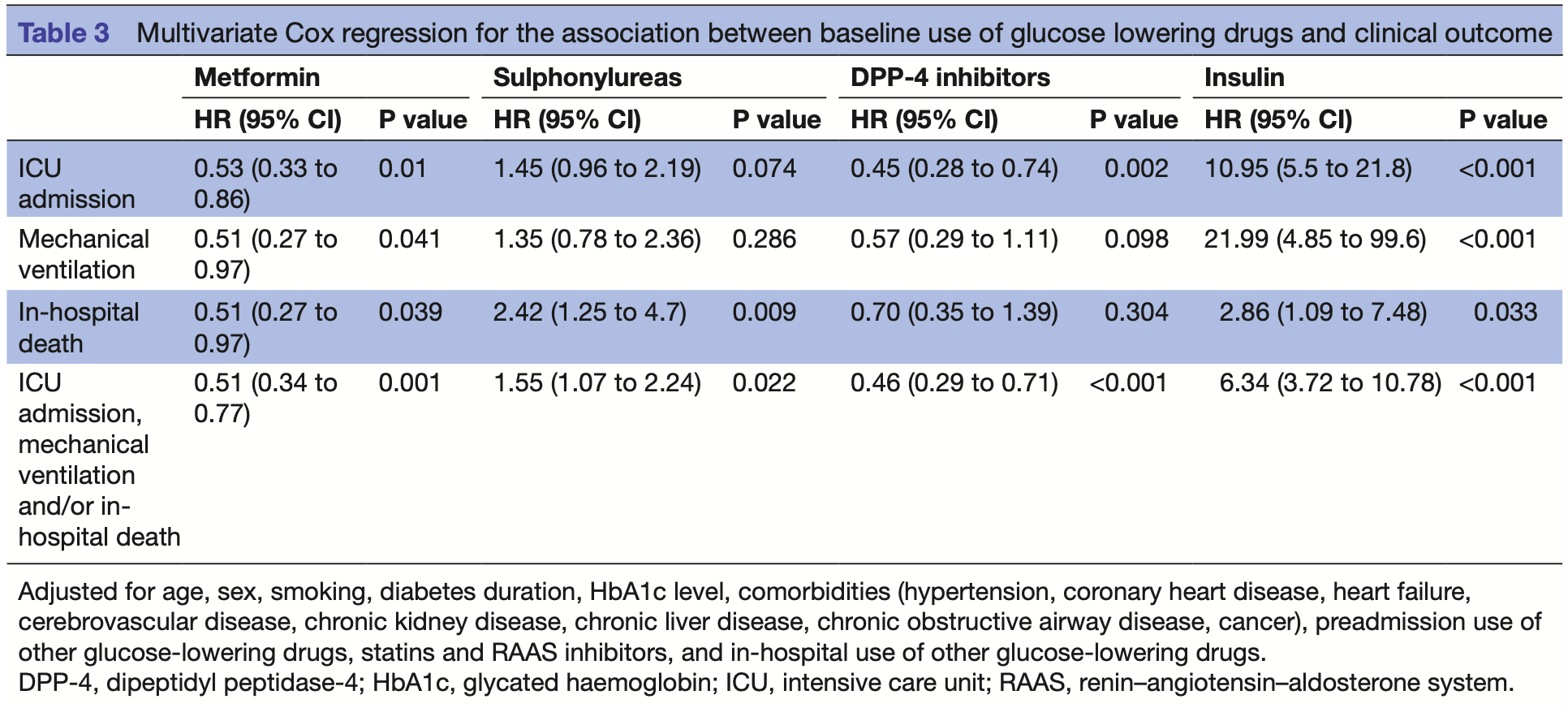
Retrospective 1,220 hospitalized COVID-19 patients with type 2 diabetes in Hong Kong showing reduced risk of ICU admission, mechanical ventilation, and death with metformin and DPP-4 inhibitors, but increased risk with insulin and sulphonylureas.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments1.
|
risk of death, 49.0% lower, HR 0.51, p = 0.04, treatment 737, control 254.
|
|
risk of mechanical ventilation, 49.0% lower, HR 0.51, p = 0.04, treatment 737, control 254.
|
|
risk of ICU admission, 47.0% lower, HR 0.53, p = 0.01, treatment 737, control 254.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Luk et al., 20 Oct 2021, retrospective, China, peer-reviewed, median age 65.3, 7 authors, study period January 2020 - February 2021.
Contact: wonglaihung@cuhk.edu.hk.
Glucose-lowering drugs and outcome from COVID-19 among patients with type 2 diabetes mellitus: a population-wide analysis in Hong Kong
BMJ Open, doi:10.1136/bmjopen-2021-052310
Objectives To investigate the association between baseline use of glucose-lowering drugs and serious clinical outcome among patients with type 2 diabetes. Design Territory-wide retrospective cohort of confirmed cases of COVID-19 between January 2020 and February 2021. Setting All public health facilities in Hong Kong. Participants 1220 patients with diabetes who were admitted for confirmed COVID-19. Primary and secondary outcome measures Composite clinical endpoint of intensive care unit admission, requirement of invasive mechanical ventilation and/or inhospital death. Results In this cohort (median age 65.3 years, 54.3% men), 737 (60.4%) patients were treated with metformin, 385 (31.6%) with sulphonylureas, 199 (16.3%) with dipeptidyl peptidase-4 (DPP-4) inhibitors and 273 (22.4%) with insulin prior to admission. In multivariate Cox regression, use of metformin and DPP-4 inhibitors was associated with reduced incidence of the composite endpoint relative to non-use, with respective HRs of 0.51 (95% CI 0.34 to 0.77, p=0.001) and 0.46 (95% CI 0.29 to 0.71, p<0.001), adjusted for age, sex, diabetes duration, glycated haemoglobin (HbA1c), smoking, comorbidities and drugs. Use of sulphonylureas (HR 1.55, 95% CI 1.07 to 2.24, p=0.022) and insulin (HR 6.34, 95% CI 3.72 to 10.78, p<0.001) were both associated with increased hazards of the composite endpoint. Conclusions Users of metformin and DPP-4 inhibitors had fewer adverse outcomes from COVID-19 compared with non-users, whereas insulin and sulphonylurea might predict a worse prognosis.
Competing interests AOYL has served as a member of advisory panel for Amgen, AstraZeneca, Boehringer Ingelheim and Sanofi and received research support from Amgen, Asia Diabetes Foundation, Bayer, Boehringer Ingelheim, Lee's Pharmaceutical, MSD, Novo Nordisk, Roche, Sanofi, Sugardown, Takeda. TCFY has served as an advisory committee member and a speaker for Gilead Sciences. APSK has received research grants and/or speaker honoraria from Abbott, Astra Zeneca, Bayer, Boehringer Ingelheim, Eli-Lilly, Merck Serono, Nestle, Novo Nordisk, Pfizer and Sanofi. VW-SW has served as an advisory committee member for 3V-BIO, AbbVie, Allergan, Boehringer Ingelheim, Echosens, Gilead Sciences, Intercept, Janssen, Novartis, Novo Nordisk, Perspectum Diagnostics, Pfizer, TARGET-NASH and Terns; and a speaker for Bristol-Myers Squibb, Echosens, Gilead Sciences and Merck. He has also received a research grant from Gilead Sciences. RCWM has received research funding from AstraZeneca, Bayer, Merck Sharp & Dohme, Novo Nordisk, Pfizer and Tricida Inc. for carrying out clinical trials, and has received speaker honorarium or consultancy in advisory boards from AstraZeneca, Bayer and Boehringer Ingelheim. All proceeds have been donated to the Chinese University of Hong Kong to support diabetes research. GL-HW has served as an advisory committee member for Gilead Sciences and Janssen, as a speaker for Abbott, Abbvie, Bristol-Myers Squibb, Echosens, Furui, Gilead Sciences, Janssen and Roche, and..
References
Agarwal, Schechter, Southern, Preadmission diabetes-specific risk factors for mortality in hospitalized patients with diabetes and coronavirus disease 2019, Diabetes Care, doi:10.2337/dc20-1543
Assiri, Al-Tawfiq, Aa, Epidemiological, demographic, and clinical characteristics of 47 cases of middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study, Lancet Infect Dis, doi:10.1016/S1473-3099(13)70204-4
Barron, Bakhai, Kar, Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a wholepopulation study, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30272-2
Bramante, Ingraham, Murray, Observational study of metformin and risk of mortality in patients hospitalized with Covid-19, medRxiv, doi:10.1101/2020.06.19.20135095
Cameron, Morrison, Levin, Anti-inflammatory effects of metformin irrespective of diabetes status, Circ Res, doi:10.1161/CIRCRESAHA.116.308445
Cariou, Hadjadj, Wargny, Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study, Diabetologia, doi:10.1007/s00125-020-05180-x
Chen, Yang, Cheng, Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication, Diabetes Care, doi:10.2337/dc20-0660
Crouse, Grimes, Li, Metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes, medRxiv, doi:10.1101/2020.07.29.20164020
Cummings, Baldwin, Abrams, Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study, Lancet, doi:10.1016/S0140-6736(20)31189-2
Do, Kim, Park, Is there an association between metformin use and clinical outcomes in diabetes patients with COVID-19?, Diabetes Metab, doi:10.1016/j.diabet.2020.10.006
Fadini, Morieri, Longato, Exposure to dipeptidylpeptidase-4 inhibitors and COVID-19 among people with type 2 diabetes: a case-control study, Diabetes Obes Metab, doi:10.1111/dom.14097
Foretz, Guigas, Bertrand, Metformin: from mechanisms of action to therapies, Cell Metab, doi:10.1016/j.cmet.2014.09.018
Gao, Piernas, Astbury, Associations between bodymass index and COVID-19 severity in 6•9 million people in England: a prospective, community-based, cohort study, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(21)00089-9
Grasselli, Greco, Zanella, Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy, JAMA Intern Med, doi:10.1001/jamainternmed.2020.3539
Guan, Ni, Hu, Clinical characteristics of coronavirus disease 2019 in China, N Engl J Med, doi:10.1056/NEJMoa2002032
Hariyanto, Kurniawan, Dipeptidyl peptidase 4 (DPP4) inhibitor and outcome from coronavirus disease 2019 (COVID-19) in diabetic patients: a systematic review, meta-analysis, and meta-regression, J Diabetes Metab Disord, doi:10.1007/s40200-021-00777-4
Hendren, De Lemos, Ayers, Association of body mass index and age with morbidity and mortality in patients hospitalized with COVID-19: results from the American heart association COVID-19 cardiovascular disease registry, Circulation, doi:10.1161/CIRCULATIONAHA.120.051936
Holman, Knighton, Kar, Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30271-0
Khunti, Knighton, Zaccardi, Prescription of glucoselowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(21)00050-4
Koh, Maude, Schreiber, Glyburide is antiinflammatory and associated with reduced mortality in melioidosis, Clin Infect Dis, doi:10.1093/cid/ciq192
Kong, census and statistics department
Kow, Hasan, Mortality risk with preadmission metformin use in patients with COVID-19 and diabetes: a meta-analysis, J Med Virol, doi:10.1002/jmv.26498
Lally, Tsoukas, Halladay, Metformin is associated with decreased 30-day mortality among nursing home residents infected with SARS-CoV2, J Am Med Dir Assoc, doi:10.1016/j.jamda.2020.10.031
Li, Thomas, Li, Addressing extreme propensity scores via the overlap weights, Am J Epidemiol, doi:10.1093/aje/kwy201
Liang, Ding, Li, Association of preadmission metformin use and mortality in patients with sepsis and diabetes mellitus: a systematic review and meta-analysis of cohort studies, Crit Care, doi:10.1186/s13054-019-2346-4
Lui, Yip, Wong, Significantly lower casefatality ratio of coronavirus disease 2019 (COVID-19) than severe acute respiratory syndrome (SARS) in Hong Kong-A Territory-Wide cohort study, Clin Infect Dis, doi:10.1093/cid/ciaa1187
Lukito, Pranata, Henrina, The effect of metformin consumption on mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.11.006
Mirani, Favacchio, Carrone, Impact of comorbidities and glycemia at admission and dipeptidyl peptidase 4 inhibitors in patients with type 2 diabetes with COVID-19: a case series from an academic hospital in Lombardy, Italy, Diabetes Care, doi:10.2337/dc20-1340
Pernicova, Kelly, Ajodha, Metformin to reduce metabolic complications and inflammation in patients on systemic glucocorticoid therapy: a randomised, double-blind, placebocontrolled, proof-of-concept, phase 2 trial, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30021-8
Pérez-Belmonte, Torres-Peña, Md, Mortality and other adverse outcomes in patients with type 2 diabetes mellitus admitted for COVID-19 in association with glucoselowering drugs: a nationwide cohort study, BMC Med, doi:10.1186/s12916-020-01832-2
Raj, Mou, Smits, Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC, Nature, doi:10.1038/nature12005
Shao, Xu, Yu, Dipeptidyl peptidase 4 inhibitors and their potential immune modulatory functions, Pharmacol Ther, doi:10.1016/j.pharmthera.2020.107503
Solerte, 'addio, Trevisan, Sitagliptin treatment at the time of hospitalization was associated with reduced mortality in patients with type 2 diabetes and COVID-19: a multicenter, case-control, retrospective, observational study, Diabetes Care, doi:10.2337/dc20-1521
Strollo, Pozzilli, Dpp4 inhibition: preventing SARS-CoV-2 infection and/or progression of COVID-19?, Diabetes Metab Res Rev, doi:10.1002/dmrr.3330
Wong, Chan, Tse, Statins reduce the risk of liver decompensation and death in chronic viral hepatitis: a propensity score weighted landmark analysis, Aliment Pharmacol Ther, doi:10.1111/apt.14341
Wong, Wong, Thompson, Management of patients with liver derangement during the COVID-19 pandemic: an Asia-Pacific position statement, Lancet Gastroenterol Hepatol, doi:10.1016/S2468-1253(20)30190-4
Wu, Zhang, Sun, Influence of diabetes mellitus on the severity and fatality of SARS-CoV-2 (COVID-19) infection, Diabetes Obes Metab, doi:10.1111/dom.14105
Yan, Yang, Wang, Clinical characteristics and outcomes of patients with severe covid-19 with diabetes, BMJ Open Diabetes Res Care, doi:10.1136/bmjdrc-2020-001343
Yang, Feng, Yuan, Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS, Diabet Med, doi:10.1111/j.1464-5491.2006.01861.x
Yip, Lui, Wong, Liver injury is independently associated with adverse clinical outcomes in patients with COVID-19, Gut, doi:10.1136/gutjnl-2020-321726
Zhang, Dong, Martin, Amp-Activated protein kinase phosphorylation of angiotensin-converting enzyme 2 in endothelium mitigates pulmonary hypertension, Am J Respir Crit Care Med, doi:10.1164/rccm.201712-2570OC
Zhang, He, Impacts of metformin on tuberculosis incidence and clinical outcomes in patients with diabetes: a systematic review and meta-analysis, Eur J Clin Pharmacol, doi:10.1007/s00228-019-02786-y
DOI record:
{
"DOI": "10.1136/bmjopen-2021-052310",
"ISSN": [
"2044-6055",
"2044-6055"
],
"URL": "http://dx.doi.org/10.1136/bmjopen-2021-052310",
"abstract": "<jats:sec>\n <jats:title>Objectives</jats:title>\n <jats:p>To investigate the association between baseline use of glucose-lowering drugs and serious clinical outcome among patients with type 2 diabetes.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Design</jats:title>\n <jats:p>Territory-wide retrospective cohort of confirmed cases of COVID-19 between January 2020 and February 2021.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Setting</jats:title>\n <jats:p>All public health facilities in Hong Kong.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Participants</jats:title>\n <jats:p>1220 patients with diabetes who were admitted for confirmed COVID-19.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Primary and secondary outcome measures</jats:title>\n <jats:p>Composite clinical endpoint of intensive care unit admission, requirement of invasive mechanical ventilation and/or in-hospital death.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>In this cohort (median age 65.3 years, 54.3% men), 737 (60.4%) patients were treated with metformin, 385 (31.6%) with sulphonylureas, 199 (16.3%) with dipeptidyl peptidase-4 (DPP-4) inhibitors and 273 (22.4%) with insulin prior to admission. In multivariate Cox regression, use of metformin and DPP-4 inhibitors was associated with reduced incidence of the composite endpoint relative to non-use, with respective HRs of 0.51 (95% CI 0.34 to 0.77, p=0.001) and 0.46 (95% CI 0.29 to 0.71, p<0.001), adjusted for age, sex, diabetes duration, glycated haemoglobin (HbA1c), smoking, comorbidities and drugs. Use of sulphonylureas (HR 1.55, 95% CI 1.07 to 2.24, p=0.022) and insulin (HR 6.34, 95% CI 3.72 to 10.78, p<0.001) were both associated with increased hazards of the composite endpoint.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Conclusions</jats:title>\n <jats:p>Users of metformin and DPP-4 inhibitors had fewer adverse outcomes from COVID-19 compared with non-users, whereas insulin and sulphonylurea might predict a worse prognosis.</jats:p>\n </jats:sec>",
"accepted": {
"date-parts": [
[
2021,
10,
4
]
]
},
"alternative-id": [
"10.1136/bmjopen-2021-052310"
],
"author": [
{
"affiliation": [
{
"name": "Department of Medicine and Therapeutics, The Chinese University of Hong Kong Faculty of Medicine, Hong Kong Special Administrative Region, People’s Republic of China"
},
{
"name": "Hong Kong Institute of Diabetes and Obesity, The Chinese University of Hong Kong, Hong Kong Special Administrative Region, People’s Republic of China"
}
],
"family": "Luk",
"given": "Andrea On Yan",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Medicine and Therapeutics, The Chinese University of Hong Kong Faculty of Medicine, Hong Kong Special Administrative Region, People’s Republic of China"
}
],
"family": "Yip",
"given": "Terry C F",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine and Therapeutics, The Chinese University of Hong Kong Faculty of Medicine, Hong Kong Special Administrative Region, People’s Republic of China"
}
],
"family": "Zhang",
"given": "Xinge",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine and Therapeutics, The Chinese University of Hong Kong Faculty of Medicine, Hong Kong Special Administrative Region, People’s Republic of China"
},
{
"name": "Hong Kong Institute of Diabetes and Obesity, The Chinese University of Hong Kong, Hong Kong Special Administrative Region, People’s Republic of China"
}
],
"family": "Kong",
"given": "Alice Pik Shan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine and Therapeutics, The Chinese University of Hong Kong Faculty of Medicine, Hong Kong Special Administrative Region, People’s Republic of China"
}
],
"family": "Wong",
"given": "Vincent Wai-Sun",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine and Therapeutics, The Chinese University of Hong Kong Faculty of Medicine, Hong Kong Special Administrative Region, People’s Republic of China"
},
{
"name": "Hong Kong Institute of Diabetes and Obesity, The Chinese University of Hong Kong, Hong Kong Special Administrative Region, People’s Republic of China"
}
],
"family": "Ma",
"given": "Ronald Ching Wan",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0002-2863-9389",
"affiliation": [
{
"name": "Department of Medicine and Therapeutics, The Chinese University of Hong Kong Faculty of Medicine, Hong Kong Special Administrative Region, People’s Republic of China"
}
],
"authenticated-orcid": false,
"family": "Wong",
"given": "Grace Lai-Hung",
"sequence": "additional"
}
],
"container-title": "BMJ Open",
"container-title-short": "BMJ Open",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2021,
10,
20
]
],
"date-time": "2021-10-20T14:27:00Z",
"timestamp": 1634740020000
},
"deposited": {
"date-parts": [
[
2025,
12,
16
]
],
"date-time": "2025-12-16T11:16:03Z",
"timestamp": 1765883763000
},
"funder": [
{
"DOI": "10.13039/501100005847",
"award": [
"COVID1903002"
],
"award-info": [
{
"award-number": [
"COVID1903002"
]
}
],
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/501100005847",
"id-type": "DOI"
}
],
"name": "Health and Medical Research Fund"
}
],
"indexed": {
"date-parts": [
[
2025,
12,
16
]
],
"date-time": "2025-12-16T11:20:03Z",
"timestamp": 1765884003492,
"version": "3.48.0"
},
"is-referenced-by-count": 18,
"issue": "10",
"issued": {
"date-parts": [
[
2021,
10
]
]
},
"journal-issue": {
"issue": "10",
"published-online": {
"date-parts": [
[
2021,
10,
20
]
]
},
"published-print": {
"date-parts": [
[
2021,
10
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "unspecified",
"delay-in-days": 18,
"start": {
"date-parts": [
[
2021,
10,
19
]
],
"date-time": "2021-10-19T00:00:00Z",
"timestamp": 1634601600000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/bmjopen-2021-052310",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "e052310",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2021,
10
]
]
},
"published-online": {
"date-parts": [
[
2021,
10,
20
]
]
},
"published-print": {
"date-parts": [
[
2021,
10
]
]
},
"publisher": "BMJ",
"reference": [
{
"DOI": "10.1016/S1473-3099(13)70204-4",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.1"
},
{
"DOI": "10.1111/j.1464-5491.2006.01861.x",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.2"
},
{
"DOI": "10.1056/NEJMoa2002032",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.3"
},
{
"DOI": "10.1111/dom.14105",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.4"
},
{
"DOI": "10.1001/jamainternmed.2020.3539",
"article-title": "Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy",
"author": "Grasselli",
"doi-asserted-by": "crossref",
"first-page": "1345",
"journal-title": "JAMA Intern Med",
"key": "2025121603155268000_11.10.e052310.5",
"volume": "180",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30272-2",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.6"
},
{
"DOI": "10.1007/s00125-020-05180-x",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.7"
},
{
"DOI": "10.2337/dc20-1543",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.8"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.051936",
"article-title": "Association of body mass index and age with morbidity and mortality in patients hospitalized with COVID-19: results from the American heart association COVID-19 cardiovascular disease registry",
"author": "Hendren",
"doi-asserted-by": "crossref",
"first-page": "135",
"journal-title": "Circulation",
"key": "2025121603155268000_11.10.e052310.9",
"volume": "143",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(20)31189-2",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.10"
},
{
"DOI": "10.2337/dbi19-0023",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.11"
},
{
"DOI": "10.1136/bmjdrc-2020-001343",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.12"
},
{
"DOI": "10.1016/j.cmet.2014.09.018",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.13"
},
{
"DOI": "10.1161/CIRCRESAHA.116.308445",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.14"
},
{
"DOI": "10.1164/rccm.201712-2570OC",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.15"
},
{
"DOI": "10.1186/s13054-019-2346-4",
"article-title": "Association of preadmission metformin use and mortality in patients with sepsis and diabetes mellitus: a systematic review and meta-analysis of cohort studies",
"author": "Liang",
"doi-asserted-by": "crossref",
"first-page": "50",
"journal-title": "Crit Care",
"key": "2025121603155268000_11.10.e052310.16",
"volume": "23",
"year": "2019"
},
{
"DOI": "10.1007/s00228-019-02786-y",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.17"
},
{
"DOI": "10.1016/j.pharmthera.2020.107503",
"article-title": "Dipeptidyl peptidase 4 inhibitors and their potential immune modulatory functions",
"author": "Shao",
"doi-asserted-by": "crossref",
"first-page": "107503",
"journal-title": "Pharmacol Ther",
"key": "2025121603155268000_11.10.e052310.18",
"volume": "209",
"year": "2020"
},
{
"DOI": "10.2337/dc20-1521",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.19"
},
{
"DOI": "10.1186/s12916-020-01832-2",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.20"
},
{
"DOI": "10.1111/dom.14097",
"article-title": "Exposure to dipeptidyl-peptidase-4 inhibitors and COVID-19 among people with type 2 diabetes: a case-control study",
"author": "Fadini",
"doi-asserted-by": "crossref",
"first-page": "1946",
"journal-title": "Diabetes Obes Metab",
"key": "2025121603155268000_11.10.e052310.21",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(21)00050-4",
"article-title": "Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England",
"author": "Khunti",
"doi-asserted-by": "crossref",
"first-page": "293",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2025121603155268000_11.10.e052310.22",
"volume": "9",
"year": "2021"
},
{
"key": "2025121603155268000_11.10.e052310.23",
"unstructured": "Census and Statistic Department . Thematic household survey report No. 50. Hong Kong SAR: census and statistics department, 2013. Available: https://www.statistics.gov.hk/pub/B11302502013XXXXB0100.pdf [Accessed 03 Feb 2021]."
},
{
"DOI": "10.1136/gutjnl-2020-321726",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.24"
},
{
"DOI": "10.1093/cid/ciaa1187",
"article-title": "Significantly lower case-fatality ratio of coronavirus disease 2019 (COVID-19) than severe acute respiratory syndrome (SARS) in Hong Kong-A Territory-Wide cohort study",
"author": "Lui",
"doi-asserted-by": "crossref",
"first-page": "e466",
"journal-title": "Clin Infect Dis",
"key": "2025121603155268000_11.10.e052310.25",
"volume": "72",
"year": "2021"
},
{
"DOI": "10.1111/apt.14341",
"article-title": "Statins reduce the risk of liver decompensation and death in chronic viral hepatitis: a propensity score weighted landmark analysis",
"author": "Wong",
"doi-asserted-by": "crossref",
"first-page": "1001",
"journal-title": "Aliment Pharmacol Ther",
"key": "2025121603155268000_11.10.e052310.26",
"volume": "46",
"year": "2017"
},
{
"DOI": "10.1093/aje/kwy201",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.27"
},
{
"article-title": "Observational study of metformin and risk of mortality in patients hospitalized with Covid-19",
"author": "Bramante",
"first-page": "2020.06.19.20135095",
"journal-title": "medRxiv",
"key": "2025121603155268000_11.10.e052310.28",
"year": "2020"
},
{
"DOI": "10.1016/j.jamda.2020.10.031",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.29"
},
{
"article-title": "Metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes",
"author": "Crouse",
"first-page": "2020.07.29.20164020",
"journal-title": "medRxiv",
"key": "2025121603155268000_11.10.e052310.30",
"year": "2020"
},
{
"DOI": "10.1016/j.diabet.2020.10.006",
"article-title": "Is there an association between metformin use and clinical outcomes in diabetes patients with COVID-19?",
"author": "Do",
"doi-asserted-by": "crossref",
"first-page": "S1262",
"journal-title": "Diabetes Metab",
"key": "2025121603155268000_11.10.e052310.31",
"volume": "47",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2020.11.006",
"article-title": "The effect of metformin consumption on mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis",
"author": "Lukito",
"doi-asserted-by": "crossref",
"first-page": "2177",
"journal-title": "Diabetes Metab Syndr",
"key": "2025121603155268000_11.10.e052310.32",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26498",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.33"
},
{
"DOI": "10.1016/S2213-8587(21)00089-9",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.34"
},
{
"DOI": "10.1016/S2213-8587(20)30271-0",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.35"
},
{
"DOI": "10.1016/S2468-1253(20)30190-4",
"article-title": "Management of patients with liver derangement during the COVID-19 pandemic: an Asia-Pacific position statement",
"author": "Wong",
"doi-asserted-by": "crossref",
"first-page": "776",
"journal-title": "Lancet Gastroenterol Hepatol",
"key": "2025121603155268000_11.10.e052310.36",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30021-8",
"article-title": "Metformin to reduce metabolic complications and inflammation in patients on systemic glucocorticoid therapy: a randomised, double-blind, placebo-controlled, proof-of-concept, phase 2 trial",
"author": "Pernicova",
"doi-asserted-by": "crossref",
"first-page": "278",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2025121603155268000_11.10.e052310.37",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1038/nature12005",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.38"
},
{
"DOI": "10.1002/dmrr.3330",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.39"
},
{
"DOI": "10.2337/dc20-1340",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.40"
},
{
"DOI": "10.1007/s40200-021-00777-4",
"article-title": "Dipeptidyl peptidase 4 (DPP4) inhibitor and outcome from coronavirus disease 2019 (COVID-19) in diabetic patients: a systematic review, meta-analysis, and meta-regression",
"author": "Hariyanto",
"doi-asserted-by": "crossref",
"first-page": "543",
"journal-title": "J Diabetes Metab Disord",
"key": "2025121603155268000_11.10.e052310.41",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.2337/dc20-0660",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.42"
},
{
"DOI": "10.1093/cid/ciq192",
"doi-asserted-by": "publisher",
"key": "2025121603155268000_11.10.e052310.43"
}
],
"reference-count": 43,
"references-count": 43,
"relation": {},
"resource": {
"primary": {
"URL": "https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2021-052310"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Glucose-lowering drugs and outcome from COVID-19 among patients with type 2 diabetes mellitus: a population-wide analysis in Hong Kong",
"type": "journal-article",
"update-policy": "https://doi.org/10.1136/crossmarkpolicy",
"volume": "11"
}
